Sir,
Congenital simple hamartoma of the retinal pigment epithelium (CSHRPE) is an uncommon benign tumor with characteristic clinical and imaging features. Owing to its benign nature, histopathological evaluation of tissue specimens is rare, and consequently, the histopathological features are not well-described. We report a case of CSHRPE with foveal involvement and secondary epiretinal membrane formation that underwent surgical excision, allowing for a detailed histopathological examination of the lesion.
Case report
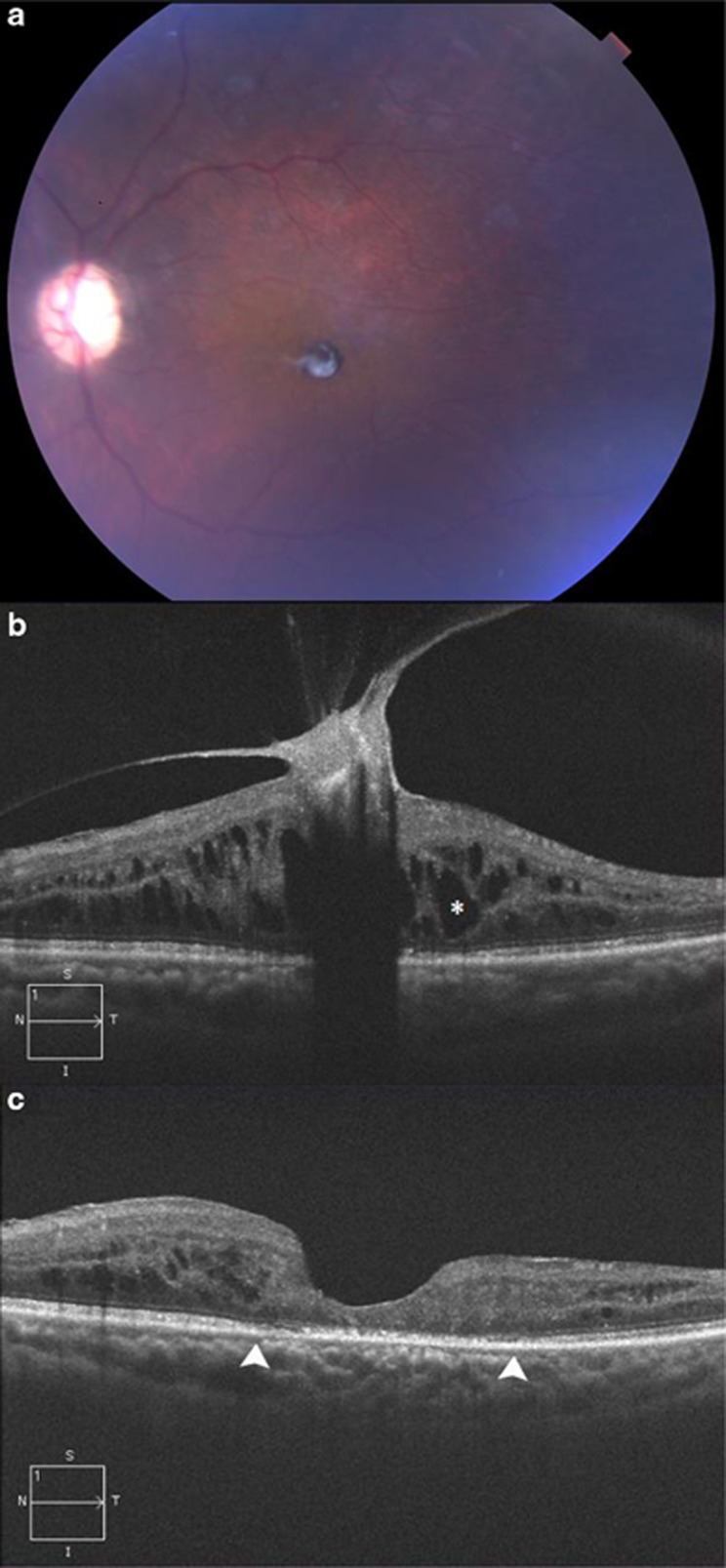
A 66-year-old Hispanic female presented with long-standing, decreased visual acuity in the left eye to the level of counting fingers. Fundus examination revealed a small, darkly pigmented, circumscribed, minimally elevated preretinal lesion involving the fovea (Figure 1a). Optical coherence tomography (OCT) showed involvement of the preretinal surface and significant vitreomacular traction (VMT) with secondary retinal thickening (Figure 1b). The lesion's surface was hyperreflective and demonstrated distinct borders with significant underlying shadowing, consistent with the clinical diagnosis of CSHRPE.
Figure 1.
(a) Color photograph shows a small, darkly pigmented, well-circumscribed lesion involving the central macula with an overlying membrane. (b) OCT shows a hyperreflective preretinal lesion in the fovea with associated VMT distorting the macular architecture. The retinal features underlying the lesion cannot be ascertained owing to severe shadowing artifact. Cystoid macular edema (*) and retinal thickening are also evident. The increased reflectivity of the lesion's anterior surface and deep underlying shadowing are characteristic of congenital simple hamartoma of the retinal pigment epithelium. (c) Optical coherence tomography shows restored foveal anatomy and resolved VMT following pars plana vitrectomy and tumor excision. There is focal disruption of the photoreceptors and retinal pigment epithelium (between arrowheads).
Pars plana vitrectomy was performed to release the VMT with the aim of improving visual acuity by restoring a more natural anatomical configuration. At the time of vitrectomy, the posterior vitreous gel was firmly attached to the anterior portion of the lesion. The traction was segmented with the vitreous cutter, and the suspected CSHRPE was successfully separated from the retina in total using a bimanual approach with forceps and curved scissors. The patient's vision improved slightly postoperatively (CF at 1 ft to CF at 6 ft). Postoperative OCT revealed no full-thickness retinal defect and near normal foveal contour with photoreceptor and RPE atrophy (Figure 1c).
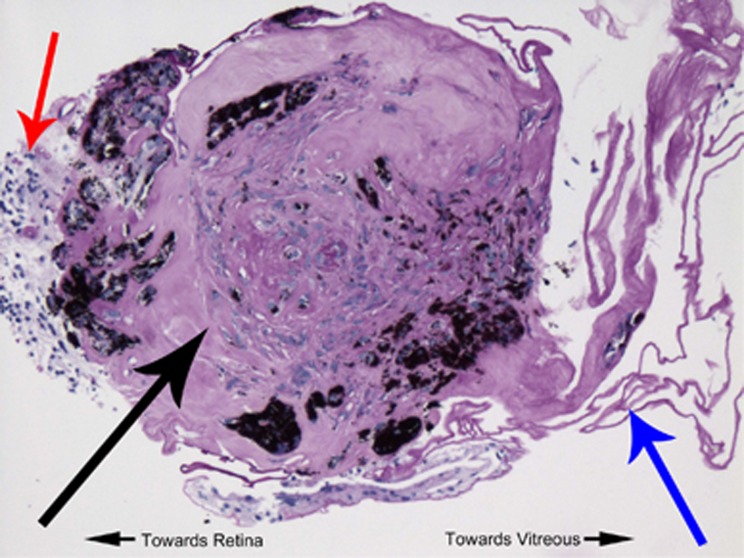
Histopathological examination of the lesion confirmed the clinical diagnosis of CSHRPE (Figure 2). The lesion showed a nodular proliferation of hyperplastic RPE cells with attached gliotic retina and internal limiting membrane (ILM). The RPE cells showed fibrous metaplasia with immunoreactivity to CD68, a histiocytic cell marker. Glial fibrillary acidic protein immunostaining exhibited peripheral staining of gliotic retinal tissue. There was no evidence of axons (neurofilament immunostain) or vascular spaces present (CD31 immunostain).
Figure 2.
Formalin-fixed, paraffin-embedded, periodic acid–Schiff (PAS) stained slide of the hyperreflective lesion depicted in Figure 1a. There is a central, nodular proliferation of hyperplastic RPE that has undergone fibrous metaplasia (black arrow). Gliotic retinal elements are attached to one surface (red arrow), whereas epiretinal membrane or posterior hyaloid is attached to the other surface of the lesion (blue arrow).
Comment
Congenital simple hamartoma of the RPE (CSHRPE) was first recognized in 1981 by Laqua1 and later characterized and named in 1989 by Gass2, who reported ten cases of the entity. In 2003, Shields3 documented the largest subsequent case series, consisting of five patients. Only 1 in 15 patients from the Shields' and Gass' cohorts presented with poor visual acuity, and the remainder of cases were discovered as incidental findings.2, 3 Though these lesions are congenital, they often are not identified until adulthood owing to their typically asymptomatic presentation (eg, two of the five patients in the Shields' case series were >60 years of age).3 An observational approach to treatment for CSHRPE is generally recommended, given its benign character and typically asymptomatic presentation.3 Mild VMT in the setting of CSHRPE has been reported,4 but the case reported herein is unique in the degree of visual impairment, owing to severe VMT with cystoid macular edema.
Most previous case reports of CSHRPE lacked histopathological confirmation of the diagnosis. Given the presumed RPE pathogenesis of the tumors, previous authors hypothesized that the lesions must involve the full-thickness of the retina.1, 2 OCT descriptions of the deeper layers of the retina underlying CSHRPE are limited by severe shadowing effect of the highly pigmented anterior aspects of the tumors,5 which prevents detailed analysis of the tissue lying below the surface of the lesion. One previous report provides a brief histopathological description of a biphasic tumor with angiomatous features and hyperplasia of the RPE but was obtained from a free-floating intravitreous lesion that was presumed CSHRPE.6 In contrast, histopathologic examination of the specimen in this case, showed a predominance of hyperplastic and metaplastic RPE cells lacking any significant angiomatous component, demonstrated by the negative CD31 immunostain. It is possible that a hyalinized vascular component was present in this case, suggested by central PAS staining that could represent basement membrane material or embedded ILM. Given the preretinal location of the CSHRPE in our case, we presume a single or a group of RPE cells migrated to the retinal surface during embryogenesis and then proliferated into a hamartomatous lesion that did not involve the entire retinal thickness. Another possibility includes RPE cell migration, secondary to traction created by this lesion. Though the identity of this tumor is difficult to prove, the age of presentation, the clinical course and imaging characteristics are most consistent with CSHRPE. In conclusion, this report provides a complete histopathological description of CSHRPE along with clinical and OCT correlation.
Acknowledgments
This work was supported in part by both a Research to Prevent Blindness Unrestricted Grant and the Massachusetts Lions Eye Research Fund to the New England Eye Center/Department of Ophthalmology, Tufts University School of Medicine.
The authors declare no conflict of interest.
References
- Laqua H. Tumors and tumor-like lesions of the retinal pigment epithelium. Ophthalmologica. 1981;183 (1:34–38. doi: 10.1159/000309131. [DOI] [PubMed] [Google Scholar]
- Gass JD. Focal congenital anomalies of the retinal pigment epithelium. Eye (Lond) 1989;3:1–18. doi: 10.1038/eye.1989.2. [DOI] [PubMed] [Google Scholar]
- Shields CL, Shields JA, Marr BP, Sperber DE, Gass JD. Congenital simple hamartoma of the retinal pigment epithelium: a study of five cases. Ophthalmology. 2003;110:1005–1011. doi: 10.1016/S0161-6420(03)00087-3. [DOI] [PubMed] [Google Scholar]
- Shukla D, Ambatkar S, Jethani J, Kim R. Optical coherence tomography in presumed congenital simple hamartoma of retinal pigment epithelium. Am J Ophthalmol. 2005;139:945–947. doi: 10.1016/j.ajo.2004.11.037. [DOI] [PubMed] [Google Scholar]
- Shields CL, Materin MA, Karatza EC, Shields JA. Optical coherence tomography of congenital simple hamartoma of the retinal pigment epithelium. Retina. 2004;24:327–328. doi: 10.1097/00006982-200404000-00031. [DOI] [PubMed] [Google Scholar]
- Holz FG, Alexandridis E, Volker HE, Dithmar S, Grossniklaus HE. Spontaneous incomplete avulsion of juxtafoveal retinal pigment epithelial hamartoma. Arch Ophthalmol. 2001;119 (6:903–907. [PubMed] [Google Scholar]