Abstract
Background
To evaluate and compare the ability of two Fourier-domain optical coherence tomography (OCT) devices to detect retinal and retinal nerve fibre layer (RNFL) atrophy in patients with Alzheimer's disease (AD) compared with healthy subjects; to test the intra-session reliability of two OCT devices in AD patients and healthy subjects.
Methods
AD patients (n=75) and age-matched healthy subjects (n=75) underwent three Macular Cube 200 × 200 protocols using the Cirrus and Spectralis OCT devices and three 360° circular scans centred on the optic disc using the Cirrus OCT device, the classic glaucoma application, and the new Nsite Axonal Analytics application of the Spectralis OCT instrument. Differences between healthy and AD eyes were compared, and measurements provided by each OCT protocol were compared. Reliability was measured using intraclass correlation coefficients and coefficients of variation. Correlations between OCT measurements and disease duration and severity were also analysed.
Results
Retinal thinning was observed in AD eyes in all areas except the fovea using both OCT devices. RNFL atrophy was detected in AD eyes with all three protocols, but the Nsite Axonal application was the most sensitive. Measurements by the two OCT devices were correlated, but differed significantly. Reliability was good using all protocols, but better with the glaucoma application of Spectralis. Mean RNFL thickness provided by the Nsite Axonal application correlated with disease duration.
Conclusions
Fourier-domain OCT is a valid and reliable technique for detecting subclinical RNFL and retinal atrophy in AD, especially using the Nsite Axonal application. RNFL thickness decreased with disease duration.
Introduction
Alzheimer's disease (AD) is a common cause of dementia in the elderly. The worldwide prevalence, estimated to be 35.6 million in 2010, is expected to double every 20 years, increasing to 115.4 million in 2050. AD is typically characterized by a progressive loss of memory and other cognitive functions and has a substantial impact on the patient, as well as the patient's family and society.1 AD affects both behaviour and functional ability and is a leading cause of disability in older people living in developed countries.2 Biomarkers and tools are needed to detect the disease in early phases, especially in high-risk families, and to monitor disease progression.
Visual impairment is often one of the earliest complaints of patients with AD.3 Although the symptoms of AD have historically been attributed to cerebral cortex damage,4, 5 recent studies have revealed degenerative changes in optic nerve fibres, causing retinal nerve fibre layer (RNFL) thinning in AD patients6, 7 with mild cognitive impairment.8 The RNFL comprises axons originating in retinal ganglion cells and can be measured using ocular imaging technologies such as optical coherence tomography (OCT),9 which provide non-invasive, rapid, objective, and reliable measurements. Numerous studies have analysed the ability of OCT to detect RNFL thickness abnormalities and changes in the macula of patients with neurodegenerative diseases.10, 11 Retrograde loss of nerve fibres in the retina and optic nerve may be an early biomarker of neurodegeneration in AD, even before hippocampal damage, which leads to memory impairment.12
Recent studies have revealed the value of RNFL and macular measurements provided by OCT for detecting neurodegenerative disease progression and facilitating the diagnosis of diseases such as multiple sclerosis10, 13, 14 and Parkinson's disease.15, 16 Therefore, in the present study we evaluated the reliability of retinal and RNFL applications of the two most commonly available FD-OCT devices, the Cirrus (Carl Zeiss Meditec Inc., Dublin, CA, USA) and Spectralis (Heidelberg Engineering, Inc., Heidelberg, Germany), for detecting retinal thinning and RNFL atrophy in patients with AD. We compared the measurements obtained using each device as well as the new software for neuro-ophthalmology evaluations of the Spectralis OCT (Nsite Axonal Analytics) and the classic software (glaucoma application). In addition, we analysed the correlations between retinal and RNFL measurements, and disease duration and severity measured with the Mini Mental State Examination (MMSE) for individuals with dementia.
Materials and methods
Seventy-five patients with AD and 75 sex- and age-matched healthy subjects were included in this cross-sectional study and underwent neuro-ophthalmologic and neurologic examinations.
Diagnosis of AD was determined by neurologists according to the National Institute of Neurologic and Communicative Disorders and Stroke-Alzheimer's Disease and Related Disorders Association17 and the Diagnostic and Statistical Manual of Mental Disorders (DSM IV) criteria.18 Patients with severe dementia were not included because of the inability to complete an ophthalmologic examination and to provide reliable test results.
Inclusion criteria were confirmed AD diagnosis; best-corrected visual acuity (BCVA) of 0.1 or higher (using a Snellen chart) in each eye to allow for performance of the protocol; and intraocular pressure less than 21 mm Hg to exclude the possibility of RNFL thinning due to other processes, such as open angle chronic glaucoma.19 Exclusion criteria were presence of significant refractive errors (>5 dioptres of spherical equivalent refraction or 3 diopters of astigmatism); systemic conditions that could affect the visual system; history of ocular trauma or concomitant ocular diseases, including a previous history of retinal pathology, glaucoma, or laser therapy; and ocular pathologies affecting the cornea, lens, retina, or optic nerve. Healthy controls had no evidence of disease of any nature, including neurologic disorders. All procedures adhered to the tenets of the Declaration of Helsinki, and the experimental protocol was approved by the local ethics committee. All subjects provided informed consent to participate in the study and underwent measurement of disease duration since diagnosis; MMSE evaluation, pupillary, anterior segment, and fundoscopic examinations, assessment of BCVA relative to the Snellen scale, and a visual field test. Three scan repetitions were performed using retinal and RNFL analysis protocols of Cirrus and Spectralis OCT. Each eye was considered separately, and only one eye of each subject was randomly selected to be included in the analyses, except when one of the eyes was excluded.
The visual field was assessed using a Humphrey Field Analyser (Carl Zeiss Meditec). A Swedish Interactive Threshold Algorithm Standard strategy (program 30-2) recorded mean deviation (MD, dB), pattern standard deviation (PSD), and pattern of defect.
OCT evaluation
The OCT tests measured retinal and peripapillary RNFL thickness using the Cirrus and Spectralis OCT devices, which were used in random order to prevent fatigue bias. All scans were performed by the same experienced operator. Between scan acquisitions, there was a time delay, and subject position and focus were randomly disrupted, meaning that alignment parameters were newly adjusted at the start of each image acquisition. No manual correction was applied to the OCT output. An internal fixation target was used because it provides the highest reproducibility.9 Images with quality a score of at least 7 in Cirrus OCT and 25 in Spectralis OCT were analysed. Three series of good-quality scans were obtained for each device. Two patients were excluded because a centred scan could not be acquired due to poor fixation. Sixteen images with artefacts, missing parts, or seemingly distorted anatomy were excluded.20 To obtain good quality, centred images, eight eyes were rescanned using the Cirrus OCT and seven eyes were rescanned using the Spectralis OCT.
Three repetitions of Cirrus Macular Cube 200 × 200 scans were performed in each eye. This protocol provides thickness measurements for each of the nine subfields defined by the Early Treatment Diabetic Retinopathy Study (ETDRS).21 Three concentric circles defined nine macular sectors. The mean of all points within the inner circle (1-mm radius) was defined as the central foveal subfield thickness. The intermediate (inner) and outer rings were each subdivided into superior, nasal, inferior, and temporal areas. The nine areas were analysed using Cirrus software, version 6.0.
Three optic disc cube 200 × 200 scans in each eye were performed using the Cirrus OCT. Each scan analysed mean RNFL thickness and quadrant RNFL thickness (superior, inferior, temporal, and nasal).
All subjects underwent three image acquisition protocols using the Spectralis OCT (three acquisitions with the Spectralis Fast Retinal protocol, three with the RNFL protocol of the classic glaucoma application, and three with the RNFL-N protocol of Nsite Axonal Analytics application) with a TruTrack eye-tracking technology. The mean number of scans to produce each circular B-scan was nine. The Spectralis Fast Retinal protocol uses an internal fixation source and centres on the patient's fovea. The operator independently monitored the stability of fixation with the built-in infrared camera. The axial and transverse resolutions of the images were 7 and 10 μm, respectively. The retinal thickness map analysis protocol represents the nine subfields as defined by the ETDRS, similar to the Cirrus OCT.21
Both RNFL protocols of the Spectralis OCT generate a thickness map with mean thickness, thickness of the four quadrants (superior, nasal, inferior, and temporal), and thickness of the six sectors (superonasal, nasal, inferonasal, inferotemporal, temporal, and superotemporal in the clockwise direction for the right eye and counterclockwise for the left eye). Defects in the RNFL are identified by comparing measurements from each patient with the normative database of each instrument. In the Nsite Axonal Analytics system, the FoDi fovea-to-disc technology correctly orients the anatomy to insure papillomacular bundle (PMB) measurement accuracy and minimize variability due to patient head orientation. The RNFL-N system places the temporal region of the scan in the centre of the viewing window for better analysis of axonal loss in the PMB, as observed in patients with neurologic diseases. The RNFL thickness graph displays the scan results in the order of nasal, inferior, temporal, superior, and nasal sectors. This protocol also provides two new neuro-ophthalmologic parameters: the PMB thickness and the nasal/temporal (N/T) ratio. Spectralis software version 5.4b was used.
Neurologic evaluation
The stage and severity of AD were determined by the MMSE scale. The items of the MMSE include tests of orientation, registration, recall, calculation, attention, naming, repetition, comprehension, reading, writing, and drawing. A score of 30 indicates 100% correct. The mean score for a community-dwelling population over 65 years old is about 27.22 AD patients lose 3 to 4 points per year of illness after the onset of memory disturbance, although there is wide variability.23 The MMSE scale was performed by one trained neurologist who was blind to the OCT results. Severity was determined by MMSE score as mild (18–24), moderate (10–18), or severe (≤9).
Disease duration was also recorded, setting the appearance of the first symptoms as the onset time of the disease.
Statistical analysis
All variables were recorded in a database created with File Maker Pro, version 8.5. Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS 20.0, SPSS Inc., Chicago, IL, USA). The Kolmogorov–Smirnov test was used to assess sample distribution. Retinal and RNFL thicknesses were compared between patients and healthy controls using Student's t-test. A P-value of less than 0.05 was considered statistically significant.
For each parameter, the coefficient of variation (COV) was calculated as the SD divided by the mean of the measurement value and expressed as a percentage. Devices with a COV less than 10% are considered highly reliable, while a COV less than 5% indicates very high reliability.24 To assess the reliability of the repeated measurements, the intraclass correlation coefficients for absolute agreement were calculated. These are used to measure the concordance for continuous variables and correct correlations for systematic bias. The intraclass correlation coefficient interpretations that we used were ‘slight reliability' (values between 0 and 0.2), ‘fair reliability' (values between 0.21 and 0.4), ‘moderate reliability' (values between 0.41 and 0.6), ‘substantial reliability' (values between 0.61 and 0.8), and ‘almost perfect reliability' (values of 0.81 and higher). Bland–Altman plots were used to assess agreement.
Relationships between measurements obtained using each OCT protocol in AD patients were evaluated. Correlation analysis was performed to evaluate the association between retinal and RNFL thicknesses and neurologic characteristics (disease duration and severity) using the Pearson correlation analysis test. Logistical regression analysis was performed to determine which OCT measurements provided better sensitivity for detecting disease severity in AD patients (measured by MMSE).
All subjects provided detailed consent to participate in this study, which was conducted in accordance with the guidelines established by the Ethics Committee of the Miguel Servet Hospital and based on the principles of the Declaration of Helsinki.
Results
One hundred and fifty eyes were evaluated: 75 eyes from AD patients and 75 eyes from healthy subjects (Table 1). Mean age was 74.15±9.15 years in the AD group and 73.98±9.05 years in the control group. Epidemiologic and disease characteristics are shown in Table 1. Age, sex, and intraocular pressure were not significantly different between AD and healthy groups. AD duration ranged from 8 months to 7 years with a median of 3.80 years since diagnosis. Mean MMSE was 15.96±7.3. Thirty patients presented mild cognitive impairment (40%), 32 patients had moderate score (42.7%), and 13 patients presented severe affectation (17.3%).
Table 1. Epidemiologic and disease characteristics of 70 patients with Alzheimer's disease and 70 healthy subjects, and statistical significance (P).
| Alzheimer's disease eyes | Healthy eyes | P-value | |
|---|---|---|---|
| Number (n) | 70 | 70 | − |
| Age (years) (range) | 74.15 (65–90) | 73.98 (65-90) | 0.602 |
| Male:female (% women) | 30:40 (57.1%) | 30:40 (57.1%) | 0.889 |
| Intraocular pressure | 14.06 (2.2) | 14.31 (1.9) | 0.305 |
| BCVA (Snellen scale) (mean (SD)) | 0.71 (0.2) | 0.94 (0.1) | <0.001 |
| MD visual field (dB) (mean (SD)) | −6.31 (3.9) | −0.6 (1.6) | <0.001 |
| PSD visual field (dB) (mean (SD)) | 4.5 (2.2) | 2.0 (0.2) | <0.001 |
| Disease duration (years) (mean (SD)) | 3.80 (1.9) | − | − |
| MMSE score (mean (range)) | 15.96 (2–28) | − | − |
Abbreviations: BCVA, best-corrected visual acuity; MMSE, Mini Mental State Examination; MSD, mean deviation of visual field; n, number of eyes; PSD, pattern standard deviation of visual field.
Visual function parameters, BCVA, mean deviation, and SD of visual field differed significantly (P<0.001) between AD patients and healthy controls.
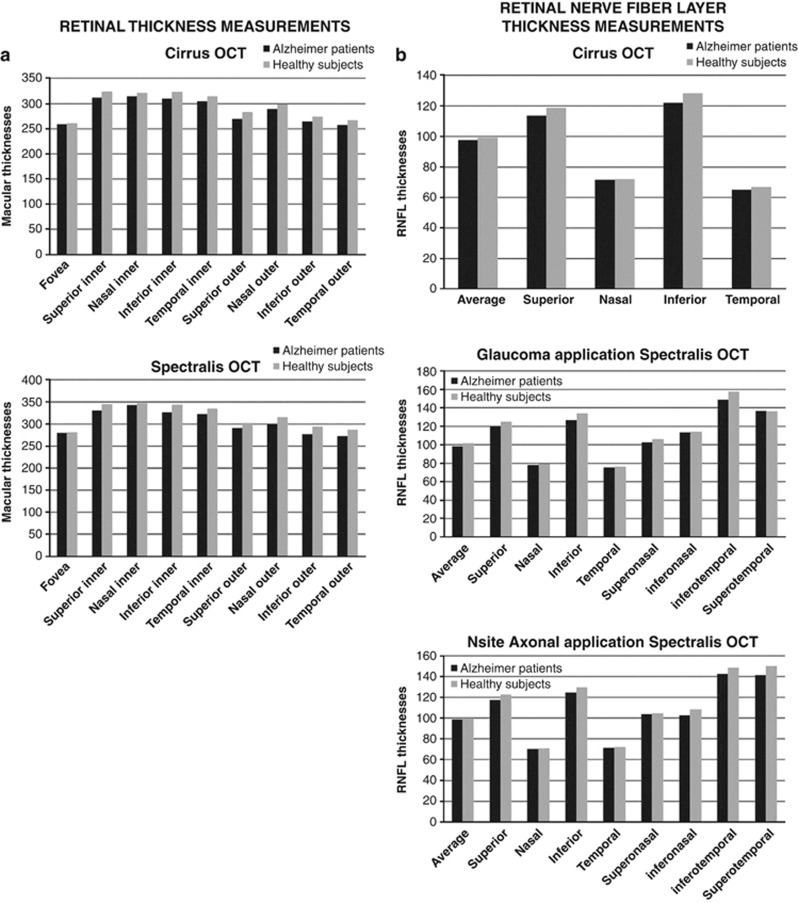
Retinal and RNFL thickness comparisons between AD and healthy eyes
Both OCT devices revealed a significant reduction in all retinal ETDRS sectors except for foveal thickness in AD patients compared with healthy subjects and reduction in RNFL thickness of AD patients (Table 2, Figure 1). The three RNFL applications used (optic disc cube 200 × 200 scan of the Cirrus OCT, the RNFL protocol of the classic glaucoma application of the Spectralis OCT, and the RNFL-N protocol of the Nsite Axonal Analytics application of the Spectralis OCT) revealed significant differences in the superior and inferior quadrants. The Spectralis OCT also revealed significant RNFL thinning in AD patients in the mean thickness and thickness of the inferotemporal and inferonasal RNFL sectors using the glaucoma application, and in the mean thickness and thickness of the inferotemporal, inferonasal, and superotemporal RNFL sectors using the Nsite Axonal Analytics application. The Nsite Axonal Analytics application also detected significant papillomacular bundle (PMB) thinning and a significant increase in the nasal/temporal (N/T) index (Table 2).
Table 2. Mean and SD of retinal and RNFL measurements of Alzheimer's disease patients and healthy subjects using Cirrus and Spectralis OCT, and statistical significance (P).
| Alzheimer patients | Healthy subjects | P-value | |
|---|---|---|---|
| Retinal measurements with Cirrus OCT | |||
| Fovea | 258.96 (25.8) | 260.41 (22.5) | 0.115 |
| Superior inner | 311.58 (24.7) | 324.00 (19.8) | <0.001 |
| Nasal inner | 314.21 (21.5) | 320.58 (16.9) | 0.004 |
| Inferior inner | 309.52 (24.9) | 322.45 (20.3) | <0.001 |
| Temporal inner | 304.11 (22.7) | 313.67 (21.5) | 0.009 |
| Superior outer | 269.74 (27.4) | 283.11 (19.6) | 0.003 |
| Nasal outer | 288.88 (20.7) | 297.95 (17.9) | <0.001 |
| Inferior outer | 263.77 (23.4) | 274.21 (20.6) | 0.016 |
| Temporal outer | 256.79 (23.6) | 267.01(21.1) | 0.001 |
| Retinal measurements with Spectralis OCT | |||
| Fovea | 278.89 (25.8) | 280.25 (18.2) | 0.096 |
| Superior inner | 330.22 (17.6) | 344.59 (13.8) | <0.001 |
| Nasal inner | 342.50 (17.8) | 346.98 (15.1) | 0.005 |
| Inferior inner | 325.69 (20.5) | 343.41 (13.6) | <0.001 |
| Temporal inner | 322.54 (17.5) | 334.69 (14.8) | 0.001 |
| Superior outer | 290.33 (19.6) | 301.25 (10.0) | <0.001 |
| Nasal outer | 298.97 (20.1) | 314.89 (13.5) | 0.002 |
| Inferior outer | 276.08 (21.5) | 293.33 (19.7) | <0.001 |
| Temporal outer | 272.88 (21.9) | 286.55 (14.8) | 0.009 |
| RNFL measurements with Cirrus OCT | |||
| Mean thickness | 97.40 (11.2) | 99.21 (9.9) | 0.106 |
| Superior thickness | 113.59 (14.5) | 118.58 (10.8) | 0.006 |
| Nasal thickness | 71.61 (15.0) | 72.12 (14.5) | 0.425 |
| Inferior thickness | 121.96 (16.9) | 127.97 (15.9) | 0.018 |
| Temporal thickness | 65.00 (10.2) | 66.96 (9.2) | 0.096 |
| Macular volume (mm3) | 9.75 (0.83) | 9.95 (0.71) | 0.111 |
| RNFL measurements with Glaucoma application of Spectralis OCT | |||
| Mean thickness | 98.11 (10.7) | 101.57 (9.5) | 0.021 |
| Superior thickness | 119.96 (13.5) | 124.87 (11.8) | 0.001 |
| Inferior thickness | 126.33 (14.6) | 133.86 (14.2) | 0.002 |
| Superonasal thickness | 102.25 (16.9) | 105.78 (16.9) | 0.201 |
| Nasal thickness | 77.88 (19.8) | 79.01 (15.7) | 0.109 |
| Inferonasal thickness | 112.95 (15.1) | 113.78 (14.4) | 0.034 |
| Inferotemporal thickness | 148.69 (14.9) | 157.00 (15.6) | 0.004 |
| Temporal thickness | 75.44 (11.9) | 76.39 (17.1) | 0.435 |
| Superotemporal thickness | 136.60 (17.6) | 143.67 (15.1) | 0.156 |
| RNFL measurements with Axonal Nsite application of Spectralis OCT | |||
| Mean thickness | 98.50 (12.4) | 99.61 (9.0) | 0.034 |
| Superior thickness | 117.10 (10.6) | 122.41 (9.1) | <0.001 |
| Inferior thickness | 124.45 (15.1) | 129.69 (13.8) | <0.001 |
| Superonasal thickness | 103.77 (15.6) | 104.42 (13.6) | 0.059 |
| Nasal thickness | 70.09 (11.5) | 70.89 (9.8) | 0.097 |
| Inferonasal thickness | 102.54 (10.6) | 108.11 (9.2) | 0.025 |
| Inferotemporal thickness | 142.36 (16.6) | 148.54 (11.3) | 0.043 |
| Temporal thickness | 71.25 (14.6) | 72.00 (14.7) | 0.088 |
| Superotemporal thickness | 141.11 (18.7) | 150.11 (15.8) | 0.028 |
| PMB sector | 51.58 (14.6) | 56.79 (10.0) | 0.012 |
| N/T index | 1.10 (0.4) | 1.01 (0.3) | 0.040 |
Abbreviations: N/T, nasal/temporal index; OCT, optical coherence tomography; PMB, papillomacular bundle; RNFL, retinal nerve fibre layer. Measurements are in microns (μm).
Significant differences are shown in bold italic font.
Figure 1.
Box plots comparing optical coherence tomography (OCT) results in eyes from Alzheimer's disease patients (n=75) and healthy subjects (n=75). (a) Retinal measurements using the Cirrus optical coherence tomography (OCT) device (top) and the Spectralis OCT device (bottom). (b) Retinal nerve fibre layer (RNFL) measurements using the Cirrus OCT device (top), the RNFL glaucoma analytic application of the Spectralis OCT device (middle), and the Nsite RNFL (RNFL-N) Axonal Analytic application of the Spectralis OCT device (bottom).
Other structural areas showed a clear tendency towards thinning in AD patients (Figure 1), but the differences were not statistically significant (Table 2).
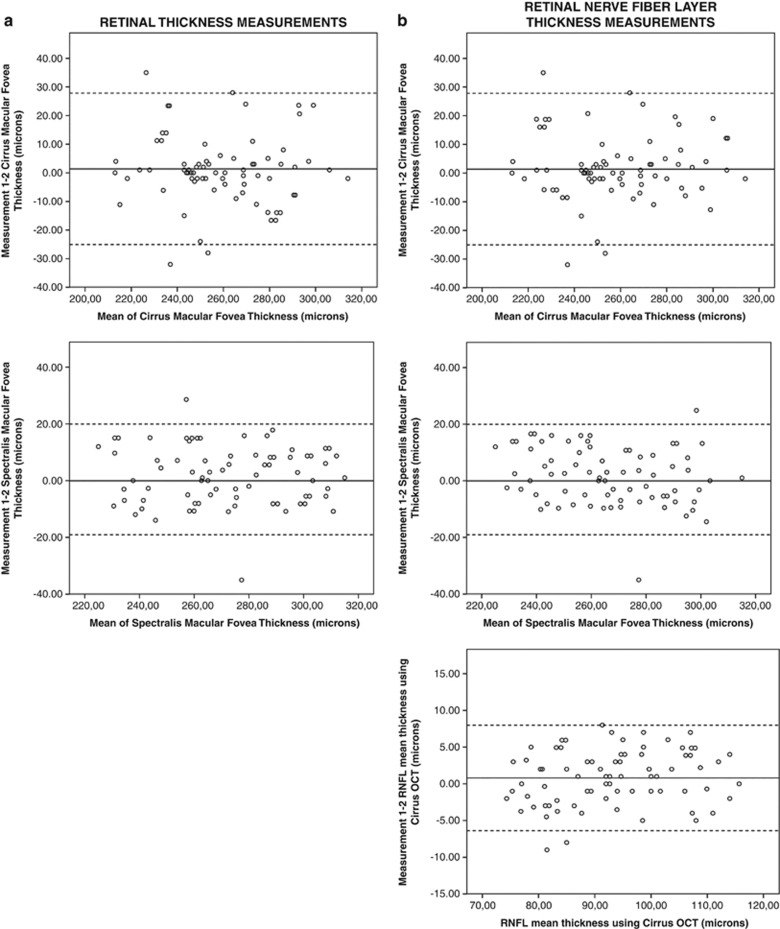
Reliability of Cirrus and Spectralis OCT measurements in AD and healthy eyes
Retina and RNFL thickness measurements showed good COV and intraclass correlation coefficients in AD patients (Table 3).
Table 3. Coefficients of variation and intraclass coefficients for repeated retinal and retinal nerve fibre layer thickness measurements in Alzheimer's disease patients and healthy controls.
| Alzheimer's disease eyes | Healthy eyes | |||
|---|---|---|---|---|
| |
COV |
ICC |
COV |
ICC |
| Macular protocol of Cirrus OCT | ||||
| Fovea | 2.50 | 0.974 | 1.78 | 0.980 |
| Superior inner | 4.70 | 0.965 | 3.62 | 0.972 |
| Nasal inner | 5.90 | 0.931 | 4.17 | 0.940 |
| Inferior inner | 6.11 | 0.905 | 4.86 | 0.955 |
| Temporal inner | 6.32 | 0.897 | 5.22 | 0.943 |
| Superior outer | 5.03 | 0.959 | 3.78 | 0.970 |
| Nasal outer | 4.99 | 0.962 | 3.77 | 0.972 |
| Inferior outer | 6.23 | 0.900 | 4.54 | 0.958 |
| Temporal outer | 6.24 | 0.909 | 4.29 | 0.949 |
| Macular protocol of Spectralis OCT | ||||
| Fovea | 2.15 | 0.980 | 1.35 | 0.989 |
| Superior inner | 4.25 | 0.969 | 3.25 | 0.958 |
| Nasal inner | 5.10 | 0.935 | 3.29 | 0.965 |
| Inferior inner | 5.26 | 0.939 | 3.39 | 0.959 |
| Temporal inner | 4.95 | 0.943 | 2.98 | 0.985 |
| Superior outer | 5.12 | 0.940 | 3.45 | 0.971 |
| Nasal outer | 5.69 | 0.905 | 4.25 | 0.963 |
| Inferior outer | 5.45 | 0.911 | 3.68 | 0.978 |
| Temporal outer | 5.11 | 0.923 | 3.44 | 0.946 |
| RNFL protocol Cirrus OCT | ||||
| Mean thickness | 2.42 | 0.959 | 1.81 | 0.979 |
| Superior quadrant | 4.03 | 0.932 | 3.00 | 0.963 |
| Nasal quadrant | 5.21 | 0.939 | 4.20 | 0.963 |
| Inferior quadrant | 3.45 | 0.964 | 3.09 | 0.955 |
| Temporal quadrant | 5.11 | 0.891 | 3.12 | 0.960 |
| Glaucoma RNFL protocol of Spectralis OCT | ||||
| Mean thickness | 2.02 | 0.985 | 1.10 | 0.991 |
| Superior area | 2.67 | 0.973 | 1.62 | 0.989 |
| Inferior area | 2.12 | 0.975 | 1.70 | 0.988 |
| Superonasal area | 3.12 | 0.970 | 2.25 | 0.986 |
| Nasal area | 3.00 | 0.974 | 2.53 | 0.985 |
| Inferonasal area | 2.89 | 0.977 | 2.50 | 0.987 |
| Inferotemporal area | 3.23 | 0.969 | 1.89 | 0.987 |
| Temporal area | 2.65 | 0.971 | 2.19 | 0.985 |
| Superotemporal area | 2.77 | 0.975 | 2.10 | 0.986 |
| Axonal RNFL-N protocol of Spectralis OCT | ||||
| Mean thickness | 2.21 | 0.959 | 1.69 | 0.989 |
| Superior area | 3.26 | 0.949 | 1.60 | 0.990 |
| Inferior area | 5.46 | 0.887 | 2.79 | 0.980 |
| Superonasal area | 4.21 | 0.959 | 3.22 | 0.973 |
| Nasal area | 6.23 | 0.896 | 5.68 | 0.877 |
| Inferonasal area | 7.11 | 0.812 | 4.41 | 0.911 |
| Inferotemporal area | 4.00 | 0.955 | 2.50 | 0.947 |
| Temporal area | 4.67 | 0.932 | 2.31 | 0.954 |
| Superotemporal area | 3.78 | 0.947 | 2.23 | 0.966 |
| PMB sector | 5.45 | 0.896 | 2.44 | 0.968 |
| N/T index | 7.30 | 0.959 | 6.02 | 0.895 |
Abbreviations: COV, coefficients of variation (in %); ICC, intraclass coefficients; N/T, nasal/temporal index; OCT, optical coherence tomography; PMB, papillomacular bundle; RNFL, retinal nerve fibre layer thickness; RNFL-N, Nsite retinal nerve fibre layer thickness.
Measurements of retinal EDTRS sectors in AD patients were highly reliable using the Cirrus OCT, with a mean COV of 5.33±1.7% (range, 2.50–6.23) and an intraclass correlation coefficient higher than 0.897. There was very high reliability using the Spectralis OCT, with a mean COV of 4.78±1.6% (range, 2.15–5.69) and an intraclass correlation coefficient higher than 0.905. The foveal thickness value had the lowest variability using either OCT device. Figure 2a shows Bland–Altman plots of fovea thickness reliability between different measurements using the Cirrus OCT and the Spectralis OCT.
Figure 2.
Graphs of the concordance in optical coherence tomography (OCT) in 75 eyes of patients with Alzheimer's disease. The difference (mean thickness measurement, 1–2) is represented against the mean of the three measurements of mean thickness. (a) Concordance in fovea thickness measurements using the Cirrus OCT device (top) and the Spectralis OCT device (bottom). (b) Concordance in retinal nerve fibre layer (RNFL) mean thickness measurements using the Cirrus OCT device (top), the glaucoma application of the Spectralis OCT device (middle), and the Nsite Axonal Analytics application of the Spectralis OCT device (bottom).
RNFL measurements performed using the glaucoma application of the Spectralis OCT were the most reliable for all the quadrants and sectors in AD and healthy subjects. The mean COV using this application in AD patients was 2.71±1.5% (range, 2.02–3.23), and the intraclass correlation coefficients were higher than 0.969. The results obtained using the Nsite Axonal Analytics application of the Spectralis OCT and the Cirrus OCT were also highly reliable, but less so than the glaucoma application. The mean COV value in the AD group was 5.96±2.3% (range, 2.21–7.30) with the Nsite Axonal Analytics application of the Spectralis OCT and 4.04±2.1% (range, 2.42–5.21) with the Cirrus OCT. The RNFL parameter with the lowest variability was mean thickness using the three protocols in the study. Figure 2b shows Bland–Altman plots of RNFL mean thickness reliability between different measurements using the Cirrus OCT, the glaucoma application of the Spectralis OCT, and the Nsite Axonal Analytics application of the Spectralis OCT.
Across all parameters, there was less variability in healthy eyes than in AD eyes (Table 3).
Correlation analysis and logistic regression between OCT and neurologic measurements
Retinal measurements obtained with the Cirrus and Spectralis OCT devices were significantly correlated (r=0.800, P=0.005, fovea thickness), but differed significantly (P<0.001, foveal thickness).
RNFL Cirrus OCT measurements significantly correlated with the RNFL measurements provided by the glaucoma application of the Spectralis OCT (r=0.818, P<0.001, RNFL mean thickness) and by the Nsite Axonal Analytics application of the Spectralis OCT(r=0.799; P<0.001, RNFL mean thickness). Correlations between the two Spectralis applications were good (r=0.869; P<0.001, RNFL mean thickness). Mean RNFL thickness values obtained with the three OCT protocols, however, differed significantly (analysis of variance, P=0.027).
Retinal and RNFL mean thickness, provided by the three protocols, did not significantly correlate with MMSE score. RNFL mean thickness correlated with disease duration using the glaucoma application of the Spectralis OCT (r=0.551, P=0.043). RNFL mean and superior thicknesses showed significant reduction in patients with severe cognitive impairment (MMSE≤9) compared with mild severity patients (MMSE between 19 and 24 points).
Logistic regression analysis demonstrated that the only OCT parameter that predicts severity in AD patients (reduction in MMSE) is the RNFL mean thickness provided by the glaucoma application of the Spectralis OCT.
Discussion
The Spectralis OCT is more reliable and more readily detects retinal pathologies than the Cirrus OCT.24, 25 Various reports on Fourier-domain (FD) OCT in healthy and pathologic subjects have been published,11, 23, 25 but no studies have evaluated the reliability of FD-OCT measurements on eyes from AD patients or measurements provided by different FD-OCT devices.
We evaluated the ability of the new Nsite Axonal Analytics application of the Spectralis OCT to detect RNFL changes in healthy and AD eyes. We also compared measurements from the Nsite Axonal Analytics application of the Spectralis OCT with those from the glaucoma application of the Spectralis OCT, and with the Cirrus OCT. Our findings indicate that the new FD-OCT technology, which includes the Cirrus and Spectralis OCT devices, can detect axonal defects in AD patients, and the Nsite Axonal application of the Spectralis OCT provides the most sensitive measure for detecting subclinical RNFL atrophy in AD.26
RNFL thickness in patients with AD compared with healthy subjects using time domain OCT reveals significant thinning in the superior and inferior RNFL quadrants in AD patients,6, 8 similar to our results. These findings demonstrated that AD progression is associated with optic nerve degeneration, but we also demonstrated retinal thinning in AD patients. Although Iseri et al7 reported a reduction in macular volume in AD patients that correlated with the severity of the disease, no previous studies have evaluated all ETDRS sectors using FD-OCT devices.
Because of the distribution of ganglionic cell fibres in the optic nerve head, the inferior RNFL quadrant undergoes a slight physiologic alteration with age; hence, thinning suggests an underlying pathology such as chronic glaucoma27 or a neurodegenerative disease such as AD. The superior RNFL quadrant alteration is consistent with a greater density of senile plaques and neurofibrillary tangles found by Armstrong et al28 in the cuneus gyrus compared with the lingual gyrus (two specific regions of the visual cortex). The temporal quadrant is the sector most affected in early neurodegenerative diseases,27 as the fibres of the temporal quadrant follow the PMB. Our results agree with these findings: RNFL-N parameters showed that PMB thickness decreased in patients with AD and the temporal sector was most susceptible (the N/T index was higher in the AD group because the RNFL thinning affected the temporal quadrant more than the other quadrants). We found that mean and superior RNFL thickness presented higher affectation in patients with severe cognitive impairment.
There is histopathologic evidence of retinal ganglion cell loss and optic nerve degeneration in patients with AD.29, 30 Neuroimaging reveals alterations in AD patients, even in early stages of the disease.31 Thus, we postulate that axonal loss secondary to other pathologic changes that occur in the brain can be detected by scanning the RNFL and the optic nerve, as these non-myelinated axons form the optic path that culminates in the occipital cortex. In recent years, many new instruments have been introduced to quantify retinal ganglion cells. Changes in the RNFL may reflect similar pathologic changes occurring elsewhere in the brain.32, 33 Ocular imaging technologies, such as OCT, scanning laser polarimetry, or confocal scanning laser ophthalmoscopy, allow the axonal constituents of the anterior visual pathway to be observed, thereby allowing direct visualization of part of the central nervous system. As the RNFL comprises only unmyelinated axons, measuring RNFL thickness may be a method for monitoring axonal loss in AD patients.34 A good correlation between RNFL thickness and magnetic resonance imaging measurements of the brain, such as the parenchymal fraction and brain volumes, has been described in multiple sclerosis patients, and mean RNFL thickness is strongly associated with normalized brain volume.33, 35
We also analysed the differences between OCT applications and devices, and the reliability of all retinal and RNFL measurements. These data should be considered when following up the changes in a patient, because an increase or reduction in retinal or RNFL thicknesses may be due to the instrument used rather than actual pathologic changes. The Cirrus OCT uses the internal limiting membrane as the anterior limit of the RNFL and the posterior border as the posterior RNFL limit. In contrast, thickness measurements using the Spectralis OCT are derived from delineation of the anterior (internal limiting membrane) and posterior borders along a single a-scan at the appropriate eccentricity within each radial b-scan. This eccentricity was determined to be equivalent to 1400 μm from the centre of the optic nerve head, measured using a ruler within the OCT visualization software. In converting angular span to linear distance, the Spectralis instrument assumes an emmetropic human eye with an average axial length.36 Ophthalmologists are incorporating the new Nsite Axonal Analytics application in their clinical practice, especially for evaluating neuro-ophthalmic patients, so the findings of the present study may help in the interpretation of the results and changes. We found significant differences between the standard Spectralis glaucoma application measurements and the Axonal NSite application measurements, although both applications measure the same peripapillary area. Differences in acquisition techniques may be the cause for this disparity, although more studies comparing populations with other pathologies should be performed to analyse and interpret these differences. Nevertheless, the same tomography device should be used to evaluate the RNFL of patients to detect progression or changes in disease, as has been suggested for other tomography devices.37, 38
Our reliability study demonstrates that the high precision of FD-OCT devices can be used to evaluate AD patients. The most reliable retinal parameter was foveal thickness, but this was the only parameter that did not reveal differences between AD and healthy subjects. These findings should be considered by ophthalmologists when evaluating changes in prospective OCT exams because OCT variability may demonstrate apparent RNFL thinning rather than actual thinning due to disease progression. This limitation may be reduced using the follow-up functions of FD-OCT.
The correlation between RNFL mean thickness (provided by the glaucoma application of Spectralis OCT) and disease duration indicates that progression of AD is associated with a progressive loss of ganglion cells.
There is RNFL thinning in AD patients, and the Nsite Axonal Analytics application of Spectralis OCT is the most sensitive protocol for detecting this subclinical atrophy. Prospective studies are needed, however, to analyse whether RNFL measurements can function as a biomarker of disease progression in AD patients.
Acknowledgments
This work was supported in part by the Fundación Mutua Madrileña grant FMMA 02/12. We thank the Federación Aragonesa de Asociaciones de Familiares de Alzheimer y otras demencias (FARAL) for helping with the patient inclusion.
The authors declare no conflict of interest.
References
- Georges J. Giving a voice to people with dementia. Dementia in Europe: The Alzheimer Europe Magazine. 2012;4:1. [Google Scholar]
- Wimo A, Winblad B, Jonsson L. The worldwide societal costs of dementia: estimates for 2009. Alzheimers Dement. 2010;6 (2:98–103. doi: 10.1016/j.jalz.2010.01.010. [DOI] [PubMed] [Google Scholar]
- Sadun AA, Borchert M, De Vita E, Hinton DR, Bassi CJ. Assessment of visual impairment in patients with Alzheimer's disease. Am J Ophthalmol. 1987;104:113–120. doi: 10.1016/0002-9394(87)90001-8. [DOI] [PubMed] [Google Scholar]
- Lewis DA, Campbell MJ, Terry RD, Morrison JH. Laminar and regional distributions of neurofibrillary tangles and neuritic plaques in Alzheimer's disease: a quantitative study of visual and auditory cortices. J Neurosc. 1987;7:1799–1808. doi: 10.1523/JNEUROSCI.07-06-01799.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hof PR, Morrison JH. Quantitative analysis of a vulnerable subset of pyramidal neurons in Alzheimer's disease: II. Primary and secondary visual cortex. J Comp Neurol. 1990;301:55–64. doi: 10.1002/cne.903010106. [DOI] [PubMed] [Google Scholar]
- Berisha F, Feke GT, Trempe CL, McMeel JW, Schepens CL. Retinal abnormalities in early Alzheimer's disease. Invest Ophthalmol Vis Sci. 2007;48 (5:2285–2289. doi: 10.1167/iovs.06-1029. [DOI] [PubMed] [Google Scholar]
- Iseri PK, Altinaş O, Tokay T, Yüksel N. Relationship between cognitive impairment and retinal morphological and visual functional abnormalities in Alzheimer disease. J Neuro-Ophthalmol. 2006;26 (1:18–24. doi: 10.1097/01.wno.0000204645.56873.26. [DOI] [PubMed] [Google Scholar]
- Kesler A, Vakhapova V, Korczyn AD, Naftaliev E, Neudorfer M. Retinal thickness in patients with mild cognitive impairment and Alzheimer's disease. Clin Neurol Neurosurg. 2011;113 (7:523–526. doi: 10.1016/j.clineuro.2011.02.014. [DOI] [PubMed] [Google Scholar]
- Schuman JS, Pedut-Kloizman T, Hertzmark E, Hee MR, Wilkins JR, Coker JG, et al. Reproducibility of nerve fibre layer thickness measurements using optical coherence tomography. Ophthalmology. 1996;103 (11:1889–1898. doi: 10.1016/s0161-6420(96)30410-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Martin E, Rodriguez-Mena D, Herrero R, Almarcegui C, Dolz I, Martin J, et al. Neuro-ophthalmologic evaluation, quality of life, and functional disability in patients with MS. Neurology. 2013;81 (1:76–83. doi: 10.1212/WNL.0b013e318299ccd9. [DOI] [PubMed] [Google Scholar]
- Garcia-Martin E, Satue M, Fuertes I, Otin S, Alarcia R, Herrero R, et al. Ability and reproducibility of Fourier-domain optical coherence tomography to detect retinal nerve fiber layer atrophy in Parkinson's disease. Ophthalmology. 2012;119 (10:2161–2167. doi: 10.1016/j.ophtha.2012.05.003. [DOI] [PubMed] [Google Scholar]
- Valenti DA. Alzheimer's disease and glaucoma: imaging the biomarkers of neurodegenerative disease. Int J Alzheimers. 2011;2010:793931. doi: 10.4061/2010/793931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Martin E, Pablo LE, Herrero R, Satue M, Polo V, Larrosa JM, et al. Diagnostic ability of a linear discriminant function for Spectral domain optical coherence tomography in multiple sclerosis patients. Ophthalmology. 2012;119 (8:1705–1711. doi: 10.1016/j.ophtha.2012.01.046. [DOI] [PubMed] [Google Scholar]
- Ratchford JN, Quigg ME, Conger A, Frohman T, Frohman E, Balcer LJ, et al. Optical coherence tomography helps differentiate neuromyelitis optica and MS optic neuropathies. Neurology. 2009;73:302–308. doi: 10.1212/WNL.0b013e3181af78b8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aaker GD, Myung JS, Ehrlich JR, Mohammed M, Henchcliffe C, Kiss S. Detection of retinal changes in Parkinson's disease with spectral-domain optical coherence tomography. Clin Ophthalmol. 2010;4:1427–1432. doi: 10.2147/OPTH.S15136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satue M, Garcia-Martin E, Fuertes I, Otin S, Alarcia R, Herrero R, et al. Use of Fourier-domain OCT to detect retinal nerve fiber layer degeneration in Parkinson's disease patients. Eye. 2013;27 (4:507–514. doi: 10.1038/eye.2013.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984;34:939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders (DSM-IV)4th ed.American Psychiatric Association: Washington, DC, USA; 1994 [Google Scholar]
- Gupta PK, Asrani S, Freedman SF, El-Dairi M, Bhatti MT. Differentiating glaucomatous from non-glaucomatous optic nerve cupping by optical coherence tomography. Open Neurol J. 2011;5:1–7. doi: 10.2174/1874205X01105010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Z, Huang J, Dustin L, Sadda SR. Signal strength is an important determinant of accuracy of nerve fiber layer thickness measurement by optical coherence tomography. J Glaucoma. 2009;18:213–216. doi: 10.1097/IJG.0b013e31817eee20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Early Treatment Diabetic Retinopathy Study Research Group Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study Report No. 1. 1985;103:1796–1806. [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. ‘Mini-Mental State Examination: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Rebok G, Brandt J, Folstein M. Longitudinal cognitive decline in patients with Alzheimer's disease. J Geriat Psychiat Neurol. 1990;3:91–97. doi: 10.1177/089198879000300207. [DOI] [PubMed] [Google Scholar]
- Garcia-Martin E, Pueyo V, Pinilla I, Ara JR, Martin J, Fernandez J. Fourier-domain OCT in multiple sclerosis patients: reproducibility and ability to detect retinal nerve fiber layer atrophy. Invest Ophthalmol Vis Sci. 2011;52:4124–4131. doi: 10.1167/iovs.10-6643. [DOI] [PubMed] [Google Scholar]
- Parikh RS, Parikh SR, Sekhar GC, Prabakaran S, Babu JG, Thomas R. Normal age-related decay of retinal nerve fiber layer thickness. Ophthalmology. 2007;114:921–926. doi: 10.1016/j.ophtha.2007.01.023. [DOI] [PubMed] [Google Scholar]
- Garcia-Martin E, Pueyo V, Almarcegui C, Martin J, Ara JR, Sancho E. Risk factors for progressive axonal degeneration of the retinal nerve fibre layer in multiple sclerosis patients. Br J Ophthalmol. 2011;95:1577–1582. doi: 10.1136/bjo.2010.199232. [DOI] [PubMed] [Google Scholar]
- Vizzeri G, Balasubramanian M, Bowd C, Weinreb RN, Medeiros FA, Zangwill LM. Spectral domain-optical coherence tomography to detect localized retinal nerve fiber layer defects in glaucomatous eyes. Opt Express. 2009;17:4004–4018. doi: 10.1364/oe.17.004004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong RA. Visual field defects in Alzheimeŕs disease patients may reflect differential pathology in the primary visual cortex. Optom Vis Sci. 1996;73:677–682. doi: 10.1097/00006324-199611000-00001. [DOI] [PubMed] [Google Scholar]
- Blanks JC, Torigoe Y, Hinton DR, Blanks RH. Retinal pathology in Alzheimer disease. I. Ganglion cell loss in foveal/parafoveal retina. Neurobiol Aging. 1996;17:377–384. doi: 10.1016/0197-4580(96)00010-3. [DOI] [PubMed] [Google Scholar]
- Blanks JC, Schmidt SY, Torigoe Y, Porrello KV, Hinton DR, Blanks RH. Retinal pathology in Alzheimeŕs disease. II. Regional neuron loss and glial changes in GCL. Neurobiol Aging. 1996;17:385–395. doi: 10.1016/0197-4580(96)00009-7. [DOI] [PubMed] [Google Scholar]
- Ewers M, Sperling RA, Klunk WE, Weiner MW, Hampel H. Neuroimaging markers for the prediction and early diagnosis of Alzheimeŕs disease dementia. Trends Neurosci. 2011;34 (8:430–442. doi: 10.1016/j.tins.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon-Lipkin E, Chodkowski B, Reich DS, Smith SA, Pulicken M, Balcer LJ, et al. Retinal nerve fiber layer is associated with brain atrophy in multiple sclerosis. Neurology. 2007;69:1603–1609. doi: 10.1212/01.wnl.0000295995.46586.ae. [DOI] [PubMed] [Google Scholar]
- Pulicken M, Gordon-Lipkin E, Balcer LJ, Frohman E, Cutter G, Calabresi PA. Optical coherence tomography and disease subtype in multiple sclerosis. Neurology. 2007;69:2085–2092. doi: 10.1212/01.wnl.0000294876.49861.dc. [DOI] [PubMed] [Google Scholar]
- Inzelberg R, Ramirez JA, Nisipeanu P, Ophir A. Retinal nerve fiber layer thinning in Parkinson disease. Vision Res. 2004;44:2793–2797. doi: 10.1016/j.visres.2004.06.009. [DOI] [PubMed] [Google Scholar]
- Grazioli E, Zivadinov R, Weinstock-Guttman B, Lincoff N, Baier M, Wong JR, et al. Retinal nerve fiber layer thickness is associated with brain MRI outcomes in multiple sclerosis. J Neurol Sci. 2008;268:12–17. doi: 10.1016/j.jns.2007.10.020. [DOI] [PubMed] [Google Scholar]
- Fortune B, Cull GA, Burgoyne CF. Relative course of retinal nerve fiber layer birefringence and thickness and retinal function changes after optic nerve transection. Invest Ophthalmol Vis Sci. 2008;49:4444–4452. doi: 10.1167/iovs.08-2255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight OJ, Chang RT, Feuer WJ, Budenz DL. Comparison of retinal nerve fiber layer measurements using time domain and spectral domain optical coherent tomography. Ophthalmology. 2009;116:1271–1277. doi: 10.1016/j.ophtha.2008.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung CK, Cheung CY, Weinreb RN, Qiu Q, Liu S, Li H, et al. Retinal nerve fiber layer imaging with spectral-domain optical coherence tomography: a variability and diagnostic performance study. Ophthalmology. 2009;116:1257–1263. doi: 10.1016/j.ophtha.2009.04.013. [DOI] [PubMed] [Google Scholar]