Abstract
Objective
To evaluate the validity and reliability of the structured Composite International Diagnostic Interview (CIDI) in diagnosing current major depressive disorder (MDD) among East African adults.
Methods
A sample of 926 patients attending a major referral hospital participated in this diagnostic assessment study. We used a two stage-study design where participants were first interviewed using an Amharic version of the CIDI and a stratified random sample underwent a follow-up semi-structured clinical interview conducted by a psychiatrist, blinded to the screening results, using the Schedules for Clinical Assessment in Neuropsychiatry (SCAN) instrument. We tested construct validity by examining the association of the CIDI and World Health Organization Quality of Life (WHO-QOL) questionnaire. We calculated the psychometric properties of the CIDI using the SCAN diagnostic interview as a gold standard.
Results
We found that the Amharic version of the CIDI diagnostic interview has good internal reliability (Cronbach’s alpha= 0.97) among Ethiopian adults. Compared to the SCAN reference standard, the CIDI had fair specificity (72.2%) but low sensitivity (51.0%). Our study provided evidence for unidimensionality of core depression screening questions on the CIDI interview with good factor loadings on a major core depressive factor.
Conclusion
The Amharic language version of the CIDI had fair specificity and low sensitivity in detecting MDD compared with psychiatrist administered SCAN diagnosis. Our findings are generally consistent with prior studies. Use of fully structured interviews such as the CIDI for MDD diagnosis in clinical settings might lead to under detection of DSM-IV MDD.
Keywords: CIDI, Validation, Africa, Ethiopia, Depression, MDD
INTRODUCTION
Mental health problems in developing countries are largely overlooked despite their high prevalence, their adverse economic impact on families and communities, and their contribution to long-term disability [1–3]. Major depressive disorder (MDD) is a significant contributor to the global burden of disease [4]. However, its recognition and treatment remain low in developing countries due to challenges such as a shortage of skilled mental health workers, stigma associated with mental illness, lack of cross-culturally validated measurement tools, and the prominence of somatic presentations of mental disorders [3, 5, 6].
The Composite International Diagnostic Interview (CIDI) is a fully standardized structured diagnostic interview designed for assessment of mental disorders by trained lay interviewers. The CIDI, developed by the World Health Organization (WHO), is widely used as a research diagnostic interview to obtain information about the prevalence and correlates of mental disorders from large community samples in different countries [7–10]. A number of studies have demonstrated the validity of the CIDI diagnostic assessment against a trained clinical interviewer [9, 11, 12]. Since its development, the instrument has been widely used in community based and health care settings worldwide. The first version of the CIDI did not adequately and consistently measure risk factors, consequences, patterns and correlates of mental health problems [9]. It also had some methodological limitations including complexity of questions and instructions, which hindered its application in cross cultural settings [9]. Cognizant of these limitations the WHO charged a multinational CIDI Editorial Committee to test the instrument in many different countries and established the WHO World Mental Health (WMH) Survey Initiative in 1998. Since then the CIDI has gone through a number of revisions to make the diagnostic sections in accordance with the DSM-IV and International Classification of Diseases 10th edition (ICD-10) systems. The CIDI is currently the most widely used fully structured diagnostic interview in psychiatric epidemiologic research [9]. In 1993 a group of investigators assessed the feasibility and acceptability of an Amharic language translated the CIDI version 1.0 among residents of Addis Ababa, Ethiopia [13]. The primary purpose of their study was to assess feasibility and acceptability of the instrument. However, the diagnostic validity (clinical appraisal) of the instrument against a gold standard has not been established [13]. The new version of the CIDI (version 3.0) has been used in Nigeria and South Africa as part of the WMH survey [14–16]. To date, however, there is no published literature reporting the validity of the CIDI version 3.0 in sub-Saharan Africa. This study aims to address this gap in the literature by evaluating the validity and reliability of the CIDI version 3.0 for detecting depression among adults in Ethiopia, the second most populous African country, using a psychiatrist administered Schedules for Clinical Assessment in Neuropsychiatry (SCAN) reference (or gold) standard.
METHODS AND MATERIALS
Study population
Adults (≥ 18 years of age) attending outpatient departments in St. Paul General Specialized Hospital in Addis Ababa, Ethiopia were invited to participate in the study. The hospital is the second largest public hospital in Ethiopia and serves as a referral and teaching hospital. Patients attending outpatient departments were invited to complete an interview where a trained research nurse interviewer administered the CIDI instrument in a private room. During this interview other general information were collected including socio-demographic characteristics, quality of life, and self-reported health status. Participants were also asked nine depression screening questions from the Patient Health Questionnaire (PHQ-9) [17]. The items were selected correspond to the criteria for the diagnosis of MDD based on DSM-IV [18]. Those who screened positive for depression on initial interview (i.e., positive on PHQ-9), as well as a randomly selected sub-group of participants who screened negative for depression (i.e., screen negative on PHQ-9) were invited for a diagnostic interview with a psychiatrist who was blinded to the CIDI and PHQ-9 screening outcome. This psychiatrist-administered SCAN diagnostic interview was completed after the initial CIDI interview within the same day.
Study Design
The study followed a two-stage design in which study participants first underwent a structured interview using the CIDI. Subsequently, participants’ MDD status was verified by a psychiatrist-administered diagnostic interview using the SCAN instrument.
Study Procedures
The data collection was conducted between June and December 2011. Research nurses were recruited and received structured training on administration of the CIDI at Addis Continental Institute of Public Health. The training program was similar to the one that the principal investigator had attended at the Social Survey Institute at the University of Michigan (WHO Training Center). In addition to the structured training course for the interviewers, item-by-item description of questionnaires and role plays were used further by two days of debriefing and review after each interviewer had done at least three practice interviews. Two clinicians (DW and AL) who practiced psychiatry for many years applied the SCAN. Both had formal training on SCAN and were supervised by a senior psychiatrist (TS) who received SCAN training at WHO-designated SCAN training center. To ensure highest quality of data collection, while interviewers were in the field, they were provided strict on-site supervision and support. All paper and pencil recorded questionnaires collected manually were entered using Blaise version 4.6 (Statistics Netherlands), which contained the entire WMH-CIDI algorithm along with an automatic checking mechanism to identify item omissions and unusual responses.
Composite International Diagnostic Interview (CIDI version 3.0)
We used the depression and mania modules of the CIDI 3.0 to diagnose MDD. The CIDI interview, designed for administration by trained lay interviewers, includes three screening (known as STEM) questions about sadness/depressed mood, feelings of discouragement, and loss of interest lasting several days or longer (Appendix Table 1). Participants who endorsed any of the three questions were given the depression module. Those who failed to endorse any of the three STEM questions were skipped out of the depression module. In accordance with DSM-IV criteria, we defined MDD as the presence of five out of nine depressive symptoms that persist for two weeks or longer, are present for most of the day nearly every day, and cause significant distress or impairment. These symptoms include dysphoric mood or anhedonia (cardinal symptoms) that persist most of the day, and clinically significant weight gain/loss or appetite disturbance, insomnia or hypersomnia, psychomotor agitation or retardation, fatigue or loss of energy, feelings of worthlessness or excessive guilt, diminished ability to concentrate or think clearly, and recurrent thoughts of death or suicide. For the purposes of this validation study, we defined current MDD as experiencing MDD in the past 12 months without plausible organic causes and without history of mania or hypomania [7, 9].
Schedules for Clinical Assessment in Neuropsychiatry (SCAN) Diagnosis
The SCAN is a semi structured clinical interview developed by the WHO for use by trained clinicians to assess and diagnose psychiatric disorders among adults [19, 20]. The SCAN was developed within the framework of the WHO and the National Institute of Mental Health (NIMH) Joint Project on Diagnosis and Classification of Mental Disorders, Alcohol and Related Problems [19]. The use of the SCAN gives flexibility in the diagnosis of mental disorders based on ICD-10 and DSM-IV [19]. The depressed mood and ideation module of SCAN has been reported to work well in different languages and cultures including Ethiopia [21]. For the current study, we used SCAN administered in Amharic as a reference (or gold) standard. All SCAN interviews (and diagnoses) were conducted without knowledge of the results of initial CIDI interviews. A total of 384 participants were invited to participate in the SCAN diagnostic interview (178 who screened positive and 276 who screened negative) and 363 of them agreed to do so (94% of selected positive screens and 95% of selected negative screens).
World Health Organization Quality of Life Questionnaire
The WHO Quality of Life questionnaire (WHO-QOL) [22] is a cross-cultural assessment tool that captures an individual’s perception of their position in life in the context of culture and value systems in which they live and in relation to their goals, expectation, standards and concerns [22]. In this study we used the abbreviated version of WHO-QOL (also known as WHOQOL-BREF) which has 26 items. The overall percentile score for each domain ranges from 0% (very poor) to 100% (very good).
Statistical Analysis
Completed data collection instruments were assessed for quality and completeness. Data from CIDI 3.0 paper and pencil interview (PAPI) were entered using direct data entry (DDE) software. After data checking and cleaning, the data were transferred to Stata 11.0 software (Statacorp, College Station, TX) for analyses. Standard descriptive statistics was performed. Participants’ characteristics were summarized using means (± standard deviation) for continuous variables with symmetric distribution and median (interquartile range) for variables with non-normal distribution and counts and percentages for categorical variables. Variables with skewed distributions were transformed into the natural logarithms and summarized using medians (interquartile range).
Diagnostic Validity Measures
We assessed the construct validity, which is defined as how a test measures the underlying construct of depression [23], on the total sample (N=926) using two approaches. First, we used exploratory factor analysis (EFA) to assess the factor structure of the symptoms of depression. Promax oblique rotation was performed because depression symptoms may be inter-correlated with each other. The number of factors to extract was determined by using the criterion of eigenvalue greater than one and the scree plot (shown in Appendix 2). Next, we used the WHO-QOL questionnaire to assess the associations between depression and quality of life. To test this hypothesis, we used a Student’s t-test to compare mean WHO-QOL scores between those classified as depressed (yes/no) according to results from our administration of the CIDI depression screening instrument. The WHOQOL-BREF has been used in diverse cultural settings including sub-Saharan Africa with mean values for healthy subjects ranging from 67% to 89% [24].
We evaluated the criterion validity by determining the concordance between the CIDI and SCAN clinical diagnosis. We computed the following parameters: sensitivity, specificity, positive likelihood ratio, negative likelihood ratio, positive predictive values, and negative predictive values for the presence or absence of MDD [25]. Given the likelihood of referral or verification bias, we implemented two analytical strategies to assess and correct for bias introduced as a result of our two-stage study design. First, we evaluated the psychometric properties of the CIDI by excluding all participants with unknown true depression status (i.e., those not selected for a psychiatrist administered diagnostic interview using the SCAN depression module) from analyses. Then, we reported Begg and Greenes adjusted estimates of psychometric properties of the CIDI, where the estimates were corrected for verification bias using inverse probability weighting approach [25–27].
RESULTS
A summary of selected socio-demographic and lifestyle characteristics of study participants is presented in Table 1. A total of 926 participants with an average age of 35 ± 11 years, ranging from 18 to 69 years were included in the study. The majority of participants were women (61%), married (52.3%) and more likely to be Orthodox Christians (74%). Approximately 4% of participants reported that they were current smokers and 9.6% of participants reported drinking at least one alcoholic beverage per week. Khat chewing was reported by 5.3 % of participants. Approximately 44% of participants reported having a fair or poor physical health status, while 33% reported poor mental health status.
Table 1.
Characteristics of the entire study population (N=926)
| Characteristic | N=926 | |
|---|---|---|
| N | % | |
| Mean age (years)* | 35.1±1.7 | |
| Sex | ||
| Women | 568 | 61.3 |
| Men | 358 | 38.7 |
| Marital status | ||
| Married | 486 | 52.5 |
| Never married | 293 | 31.6 |
| Other | 147 | 15.9 |
| Education | ||
| ≤ Primary (1–6) | 400 | 43.2 |
| Secondary (7–12) | 322 | 34.8 |
| College graduate | 204 | 22.0 |
| Smoking status | ||
| Never | 802 | 86.6 |
| Former | 88 | 9.5 |
| Current | 36 | 3.9 |
| Alcohol consumption past year | ||
| Non-drinker | 528 | 57.0 |
| Less than once a month | 309 | 33.4 |
| ≥ 1 day a week | 89 | 9.6 |
| Khat chewing | ||
| None | 679 | 73.7 |
| Former | 198 | 21.4 |
| Current | 49 | 5.3 |
| Self-reported physical health | ||
| Excellent/very good/good | 522 | 56.4 |
| Poor/fair | 404 | 43.6 |
| Self-reported mental health | ||
| Excellent/very good/good | 616 | 66.5 |
| Poor/fair | 310 | 33.5 |
Mean ± standard deviation (SD)
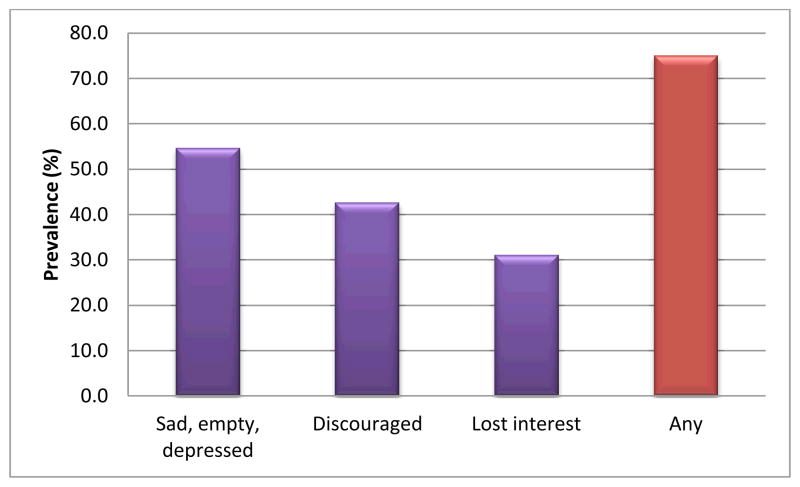
Lifetime prevalence of depressive symptoms derived from response to the initial CIDI STEM questions for depression is presented in Figure 1. The most commonly endorsed depressive symptom was feeling sad, empty or depressed (54.6%) followed by feeling discouraged (42.6%). Distributions of the socio-demographic and lifestyle characteristics according to participants’ current CIDI MDD status are shown in Table 2.
Figure 1.
Depressive symptoms endorsed using CIDI STEM questions for depression
*STEM questions are core questions used at the beginning of CIDI interviews
Table 2.
Characteristics of subjects according to CIDI and SCAN major depressive disorder status
| Characteristic | CIDI | SCAN | ||
|---|---|---|---|---|
|
| ||||
| Depressed N=60 | Non-depressed N=866 | Depressed N= 46 | Non-depressed N=317 | |
|
| ||||
| % | % | % | % | |
| Mean age (years) | 35.1 ± 11.5 | 35.6 ± 12.9 | 33.7 ± 9.6 | 35.1 ± 11.9 |
| Gender | ||||
| Women | 60.0 | 61.4 | 80.4 | 60.6 |
| Men | 40.0 | 38.6 | 19.6 | 39.4 |
| Marital status | ||||
| Married | 40.0 | 53.1 | 36.9 | 53.3 |
| Never married | 36.7 | 31.4 | 28.3 | 30.3 |
| Other | 23.3 | 15.5 | 34.8 | 16.4 |
| Education | ||||
| ≤ Primary (1–6) | 33.3 | 43.9 | 52.2 | 45.7 |
| Secondary (7–12) | 46.7 | 33.9 | 30.4 | 34.7 |
| College graduate | 20.0 | 22.2 | 17.4 | 19.6 |
| Smoking status | ||||
| Never | 81.7 | 86.9 | 78.3 | 86.4 |
| Former | 5.0 | 3.8 | 17.4 | 10.4 |
| Current | 13.3 | 9.2 | 4.3 | 3.2 |
| Alcohol consumption past year | ||||
| Never | 58.3 | 56.9 | 73.9 | 55.2 |
| Former | 31.7 | 33.5 | 21.7 | 34.4 |
| Current | 10.0 | 9.6 | 4.4 | 10.4 |
| Khat consumption | ||||
| None | 76.7 | 73.1 | 69.6 | 72.3 |
| Former | 1.7 | 5.5 | 2.2 | 3.8 |
| Current | 21.6 | 21.4 | 28.2 | 23.9 |
| Self-reported physical health | ||||
| Excellent/very good/good | 33.0 | 58.0 | 36.9 | 47.9 |
| Poor/fair | 66.0 | 42.0 | 63.1 | 52.1 |
| Self-reported mental health | ||||
| Excellent/very good/good | 45.0 | 68.0 | 34.8 | 56.2 |
| Poor/fair | 55.0 | 32.0 | 65.2 | 43.8 |
Mean ± standard deviation (SD)
Overall, the 12 month prevalence estimate of the CIDI MDD in the total 926 sample was 6.5% (95% CI, 4.9–8.1) (Table 2). Distributions of the socio-demographic and lifestyle characteristics according to participants’ CIDI MDD status are also presented in Table 2. Those who were classified as depressed were less likely to be married, more likely to be smokers, and more likely to report poor physical and mental health. A total of 46 patients fulfilled the DSM-IV criteria for MDD using the SCAN depression module. Women were more likely to be diagnosed with MDD (14.4%; 95%CI 11.5–17.4%) than men (6.0%; 95%CI 5.4–6.5%). Overall, participants diagnosed with MDD, as compared with those not diagnosed, were more likely to have lower educational attainment, to be divorced or widowed, and to report poor physical and mental health status
The exploratory factor analysis of the CIDI depressive symptoms questions showed that a rotated factor solution contained one factor with eigenvalues greater than 1.0, which accounted for 84.3% of the variance (Table 3). Item loadings ranged from 0.54 to 0.95. Depressed mood, diminished ability to concentrate or think, and change in appetite were most strongly related to the underlying construct (loading values over 0.90). Anhedonia and suicidal thoughts were the next items strongly related to the underlying construct. For these two variables the correlation between the item and the construct was over 0.85. The items that loaded least strongly included psychomotor agitation or retardation (0.54) worthlessness or excessive or inappropriate guilt (0.75).
Table 3.
Exploratory factor analysis of depressive symptoms using CIDI
| Depressive symptoms | Factor Loadings Factor 1 |
|---|---|
| Anhedonia | 0.894 |
| Depressed mood | 0.950 |
| Insomnia or hypersomnia | 0.838 |
| Fatigue or loss of energy | 0.878 |
| Significant weight loss when not dieting or weight gain | 0.908 |
| Worthlessness or excessive or inappropriate guilt | 0.750 |
| Diminished ability to think or concentrate | 0.951 |
| Psychomotor agitation or retardation | 0.544 |
| Recurrent suicidal thoughts | 0.880 |
| Eigenvalue | 7.95 |
| % Variance | 84.3 |
The WHO-QOL scores for physical, psychological, social relationship and environmental domains are summarized in Tables 4. Since the scores have fairly symmetrical distributions, we provide mean (SD) summaries. The mean WHO-QOL scores for depressed women were significantly lower in each domain as compared to men. Across all domains for both men and women, the mean scores for those classified as depressed were significantly lower than those not depressed. For instance, for psychological domain participants with MDD, compared to non-depressed, were more likely to have lower mean WHO-QOL scores (46.9 (SD=18.8) versus 57.6 (SD=17.5), p<0.001). Similar significantly lower mean WHO-QOL scores were noted for social relationship, physical and environmental domains.
Table 4.
Mean WHH-QOL scores according to CIDI determined major depressive disorder status by domain
| Quality of life assessed by Domain | Depressed | Not Depressed | P-value | ||
|---|---|---|---|---|---|
|
| |||||
| Mean score | SD | Mean score | SD | ||
| Physical | 46.1 | 13.0 | 52.4 | 13.4 | <0.001 |
| Psychological | 46.9 | 18.8 | 57.6 | 17.5 | <0.001 |
| Social relationships | 54.4 | 24.9 | 65.2 | 22.1 | <0.001 |
| Environmental | 35.7 | 15.0 | 43.6 | 15.6 | <0.001 |
Table 5 shows the psychometric characteristics of CIDI using SCAN as a gold standard. First, we evaluated the psychometric properties of CIDI using MCAR assumptions where all patients with unknown true MDD status were discarded. For instance, the sensitivity and specificity of the CIDI under naïve estimators for all participants were 43.5% (95%CI: 28.9–58.9%) and 77.9% (95%CI: 72.9–82.4%), respectively. The positive predictive value for detecting MDD with the CIDI was 22.4%, and the negative predictive value was 90.5%. After adjusting for verification bias, the sensitivity was 51% (95%CI: 41.3–60.6%) and specificity was 72.2% (95%CI: 68.7–75.6%). The positive predictive value for detecting MDD with the CIDI assessment was 22.4%, and the negative predictive value was 90.5%. The sex stratified analysis showed that sensitivity was higher in women (sensitivity= 56.1% and specificity =69.3%) compared with men (sensitivity=45.0% and specificity= 69.6%).
Table 5.
Sensitivity and Specificity for the detection of major depressive disorder of CIDI by sex
| Sensitivity | Specificity | LR+ | LR− | PPV+ | PPV− | |
|---|---|---|---|---|---|---|
| All subjects | ||||||
| Naïve | 43.5 (28.9–58.9) | 77.9 (72.9–82.4) | 2.0 (1.3–2.9) | 0.7 (0.6–0.9) | 22.2 (14.1–32.2) | 90.5 (86.4–93.7) |
| Adjusted | 51.0 (41.3–60.6) | 72.2 (68.7–75.6) | 1.8 (1.4–2.3) | 0.7 (0.5–0.8) | 22.4 (17.3–28.0) | 90.5 (88.3–92.4) |
| Women | ||||||
| Naïve | 45.9 (31.9–56.0) | 77.1 (70.5–82.8) | 2.0 (1.3–3.1) | 0.7 (0.5–0.9) | 27.9 (17.1–40.8) | 88.1 (82.2–92.6) |
| Adjusted | 56.1 (45.3–66.3) | 69.3 (64.6–73.3) | 1.8 (1.4–2.3) | 0.6 (0.5–0.8) | 27.9 (21.6–35.2) | 88.2 (84.1–91.4) |
| Men | ||||||
| Naïve | 33.1 (7.5–70.1) | 79.2 (71.0–85.9) | 1.6 (0.6–4.3) | 0.8 (0.5–1.3) | 10.3 (2.2–27.4) | 94.3 (88.0–97.9) |
| Adjusted | 45.0 (26.0–65.8) | 73.3 (63.6–76.8) | 1.5 (0.9–2.5) | 0.8 (0.5–1.2) | 10.6 (5.7–18.9) | 94.1 (89.7–96.6) |
Naive estimates are using missing completely random assumption and adjusted estimates are Begg and Greenes estimates;
LR+: positive likelihood ratio, LR−: negative likelihood ratio, PPV+:positive predictive value, PPV−:negative predictive value
DISCUSSION
Our results provided evidence that the Amharic version of the CIDI is a tool with high internal reliability (Cronbach’s alpha =0.97) among Ethiopian adults. Our study also provided strong evidence for the construct validity of the Amharic version of the CIDI in diagnosing MDD. The factor analysis revealed unidimensionality of core depression screening questions with good factor loadings on a major core depressive factor. Adults classified with MDD by the CIDI had lower quality of life scores across physical, psychological, social relationship and environmental domains. Compared to SCAN reference standard, the CIDI is modestly effective in MDD diagnosis with a moderate specificity (72.2%) but low sensitivity (51.0%). Finally, the CIDI was most successful at identifying a person without MDD (with a good negative predictive value of 90.5%). In other words, a person who was identified as non-depressed using CIDI had more than 90% probability of not having MDD diagnosis using SCAN. However, a person who identified as depressed using CIDI had 22% (PPV) chance of having MDD diagnosis using SCAN. The low PPV could be due to the low prevalence of MDD in our study. The positive LR commonly considered to “rule in disease” of the CIDI was 1.8. The negative LR commonly considered to “rule out of disease” was 0.7. This means that clinically in a similar outpatient settings, patients with MDD are 1.8-times more likely to have an MDD diagnosis using CIDI compared to patients without MDD. Similarly patients without MDD are 1.4 (1/0.7) times more likely to have negative test results using CIDI compared to those with MDD.
Findings from our study are generally consistent with prior validation studies conducted in other countries. In their study among UK residents, Brugha et al [28] compared the performance of the CIDI in diagnosing depression using SCAN diagnostic interview as a reference standard [28]. The authors employed a two phased study design where participants were initially screened using the CIDI instrument and then evaluated using the SCAN clinical interview. They reported a sensitivity of 50% (95%CI: 12–88%) and a specificity of 87% (95%CI: 81–91%). Similarly, a recent reappraisal study conducted by Haro et al compared the current version of CIDI (CIDI 3.0) with a clinician-administered Structured Clinical Interview for DSM-IV (SCID) in a probability subsamples of the WHO World Mental Health (WMH) surveys in France, Italy, Spain, and the US [12]. The investigators noted a sensitivity of 55.3 % and specificity of 93.7% for MDD. In contrast, Jordanova and colleagues [29] in their study among 105 primary care attendees in UK evaluated the diagnostic properties of CIDI with reference to a clinician administered SCAN. The authors used ICD-10 diagnostic categories to compare the two instruments. Although the concordance for depressive disorders was fair (kappa=54%), the sensitivity was 100% and specificity of 88%. CIDI prevalence estimates of depression (18.1%) were more than two-fold higher compared with SCAN prevalence estimates (7.6%) [29] although the CIDI estimates are generally conservative compared with semi-structured interviews [30]. Reasons for the differences in test characteristics across studies are unclear. We speculate that the lower sensitivity of the CIDI noted in our study and those of others [12, 28] may stem from the fact that the CIDI is a fully structured interview that employs precisely worded questions that cannot be rephrased or reworded [9, 28, 30]. In addition, the CIDI is designed to be used by lay interviewers, thus does not allow use of clinical judgment. Whereas the gold standard for our comparison was the semi-structured psychiatrist administered SCAN interview with freedom for probing and rephrasing questions [20]. Moreover, given that a large proportion of patients endorsed the STEM questions of depression (75%), it is possible that the strict skip structure of CIDI led to poor sensitivity. The diagnostic STEM (core) questions used at the beginning of the CIDI and SCAN interviews are similar. However, SCAN allows clinicians to elicit more information based upon open ended probing whereas CIDI follows a strict Yes/No structure [28]. It is important to recognize that relaxing the threshold of the symptoms might be something that merits consideration in future studies.
Investigators have discussed the importance of using factor structure when an instrument is applied in a new context or cultural group[31]. However, to date, we are not aware of previous studies that examined the factor structure of CIDI depression screening instrument. Our study provided the first evidence of the unidimensional nature of the depression symptom questions included in CIDI. As shown in our factor analysis, the correlations between the item and the construct for depressed mood, diminished ability to concentrate or think and change in appetite were over 0.90 showing strong correlation to the construct underlying these items. This is important in that depressed mood is one of the cardinal symptoms of depression, diminished ability to concentrate or think and changes in appetite are secondary diagnostic symptoms. Anhedonia and suicidal thoughts were the next set of items strongly related to the underlying construct. This finding is consistent with what is reported with other depression screening instruments such as the PHQ-9 [32].
Several potential limitations must be considered when interpreting results from our study. First, our study was conducted in a clinical setting. Some investigators have noted that in community based studies of CIDI, respondents were more comfortable admitting personal or socially unacceptable feelings and behaviors to lay interviewers than to clinical interviewers [7, 33]. The concordance of our results with those from other studies that have included community based samples, however, serve to attenuate some of these concerns. It will be important for future studies to evaluate the diagnostic validity of the Amharic version of the CIDI within the general population. Second, to ensure proper expression and conceptualization of terminologies in local contexts, we used a standard approach of iterative back translation by panels of bilingual experts. Some investigators have noted that that standard translation and back-translation procedures might be inadequate to produce a culturally valid version of these instruments in non-Western countries [34]. Future studies in our setting need to evaluate how harmonization and adaption might increase the accuracy of fully-structured diagnostic interviews in assessing mental disorders. Third, some investigators have argued that semi-structured diagnostic interviews such as SCAN or SCID do not represent a valid gold standard, as neither perfectly reflects the DSM diagnosis [30]. Hence, they suggest evaluating the standard psychometric properties with performance measures such as sensitivity or specificity may not be appropriate. Furthermore, it is important to recognize that the self-report of subjective symptoms is an inherent problem in measurement of mental disorders in clinical and research settings that cannot be solved by use of any standardized instruments such as SCAN or SCID [35]. Notwithstanding the noted limitations, our study has several strengths. First, we used strict protocols of a two-stage study design and appropriate statistical analysis ensuring there is no verification bias. Second, psychiatrists who administered the criterion reference standard SCAN were blinded to the results of the CIDI interviews.
In conclusion, this study provided fundamental information concerning the reliability and validity of an Amharic language translated the CIDI for depression diagnosis among Ethiopian adults. Knowledge gained from this study will facilitate efforts in identifying unmet mental health needs and improving mental health services. There is epidemiologic evidence suggesting that locally validated screening instruments can be used by non-physicians and community health workers [36]. The benefits of having well characterized instruments like the CIDI in low income and resource limited clinical and research settings are far reaching [37, 38]. First, they have the ability to provide reliable local data on specific disorders. Having local data compels health personnel and policy makers in specific countries or regions and to evaluate unmet needs and to evaluate implementation of health programs and policies. Second, they can be used to evaluate modifiable risk factors associated with depression in the local context. Lastly, they provide a basis for designing and evaluating the impact of intervention programs [39–41]. Given that semi-structured interviews such as SCAN are time-demanding, expensive and require a trained clinician, the use of fully structured interviews like CIDI is critical. However, in light of our findings and those of others, researchers should interpret the findings of these surveys in the general population cautiously.
Supplementary Material
Acknowledgments
This research was supported, in part, by an award from the National Institutes of Health, National Institute of Minority Health and Health Disparities (T37-MD001449). The authors wish to thank the staff of Addis Continental Institute of Public Health for their expert technical assistance. The authors would also like to thank Saint Paul Hospital for granting access to conduct the study.
References
- 1.Patel V, Garrison P, de Jesus Mari J, Minas H, Prince M, Saxena S. The Lancet’s series on global mental health: 1 year on. Lancet. 2008;372(9646):1354–1357. doi: 10.1016/S0140-6736(08)61556-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patel V, Prince M. Global mental health: a new global health field comes of age. JAMA. 2010;303(19):1976–1977. doi: 10.1001/jama.2010.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wig NN. WHO and mental health--a view from developing countries. Bull World Health Organ. 2000;78(4):502–503. [PMC free article] [PubMed] [Google Scholar]
- 4.Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 5.Patel V, Araya R, Chowdhary N, King M, Kirkwood B, Nayak S, Simon G, Weiss HA. Detecting common mental disorders in primary care in India: a comparison of five screening questionnaires. Psychol Med. 2008;38(2):221–228. doi: 10.1017/S0033291707002334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patel V, Sartorius N. From science to action: the Lancet Series on Global Mental Health. Curr Opin Psychiatry. 2008;21(2):109–113. doi: 10.1097/YCO.0b013e3282f43c7f. [DOI] [PubMed] [Google Scholar]
- 7.Kessler RC, Abelson J, Demler O, Escobar JI, Gibbon M, Guyer ME, Howes MJ, Jin R, Vega WA, Walters EE, et al. Clinical calibration of DSM-IV diagnoses in the World Mental Health (WMH) version of the World Health Organization (WHO) Composite International Diagnostic Interview (WMHCIDI) Int J Methods Psychiatr Res. 2004;13(2):122–139. doi: 10.1002/mpr.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kessler RC, Angermeyer M, Anthony JC, RDEG, Demyttenaere K, Gasquet I, GDEG, Gluzman S, Gureje O, Haro JM, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry. 2007;6(3):168–176. [PMC free article] [PubMed] [Google Scholar]
- 9.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) International Journal of Methods in Psychiatric Research. 2004;13(2):93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Robins LN, Wing J, Wittchen HU, Helzer JE, Babor TF, Burke J, Farmer A, Jablenski A, Pickens R, Regier DA, et al. The Composite International Diagnostic Interview. An epidemiologic Instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Archives of general psychiatry. 1988;45(12):1069–1077. doi: 10.1001/archpsyc.1988.01800360017003. [DOI] [PubMed] [Google Scholar]
- 11.Kessler RC, Abelson J, Demler O, Escobar JI, Gibbon M, Guyer ME, Howes MJ, Jin R, Vega WA, Walters EE, et al. Clinical calibration of DSM-IV diagnoses in the World Mental Health (WMH) version of the World Health Organization (WHO) Composite International Diagnostic Interview (WMHCIDI) International Journal of Methods in Psychiatric Research. 2004;13(2):122–139. doi: 10.1002/mpr.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haro JM, Arbabzadeh-Bouchez S, Brugha TS, de Girolamo G, Guyer ME, Jin R, Lepine JP, Mazzi F, Reneses B, Vilagut G, et al. Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3. 0) with standardized clinical assessments in the WHO World Mental Health surveys. International Journal of Methods in Psychiatric Research. 2006;15(4):167–180. doi: 10.1002/mpr.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rashid E, Kebede D, Alem A. Evaluation of an Amharic version of the Composite International Diagnostic Interview (CIDI) in Ethiopia. Ethiop J Health Dev. 1996;10:69–77. [Google Scholar]
- 14.Bass JK, Bolton PA, Murray LK. Do not forget culture when studying mental health. Lancet. 2007;370(9591):918–919. doi: 10.1016/S0140-6736(07)61426-3. [DOI] [PubMed] [Google Scholar]
- 15.Johnson LR, Mayanja MK, Bangirana P, Kizito S. Contrasting concepts of depression in Uganda: implications for service delivery in a multicultural context. Am J Orthopsychiatry. 2009;79(2):275–289. doi: 10.1037/a0015818. [DOI] [PubMed] [Google Scholar]
- 16.Lloyd CE, Dyer PH, Barnett AH. Prevalence of symptoms of depression and anxiety in a diabetes clinic population. Diabetic medicine. 2000;17(3):198–202. doi: 10.1046/j.1464-5491.2000.00260.x. [DOI] [PubMed] [Google Scholar]
- 17.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American Psychiatric A, American Psychiatric Association. Task Force on D-I. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 19.Aboraya A, Tien A, Stevenson J, Crosby K. Schedules for Clinical Assessment in Neuropsychiatry (SCAN): introduction to WV’s mental health community. W V Med J. 1998;94(6):326–328. [PubMed] [Google Scholar]
- 20.Wing JK, Babor T, Brugha T, Burke J, Cooper JE, Giel R, Jablenski A, Regier D, Sartorius N. SCAN Schedules for Clinical Assessment in Neuropsychiatry. Arch Gen Psychiatry. 1990;47(6):589–593. doi: 10.1001/archpsyc.1990.01810180089012. [DOI] [PubMed] [Google Scholar]
- 21.Alem A, Kebede D, Shibre T, Negash A, Deyassa N. Comparison of computer assisted scan diagnoses and clinical diagnoses of major mental disorders in Butajira, rural Ethiopia. Ethiop Med J. 2004;42(2):137–143. [PubMed] [Google Scholar]
- 22.Saxena S, Carlson D, Billington R, Life WGWHOQO. The WHO quality of life assessment instrument (WHOQOL-Bref): the importance of its items for cross-cultural research. Quality of life research: an international journal of quality of life aspects of treatment, care and rehabilitation. 2001;10(8):711–721. doi: 10.1023/a:1013867826835. [DOI] [PubMed] [Google Scholar]
- 23.Moller-Leimkuhler AM. Higher comorbidity of depression and cardiovascular disease in women: a biopsychosocial perspective. The world journal of biological psychiatry. 11(8):922–933. doi: 10.3109/15622975.2010.523481. [DOI] [PubMed] [Google Scholar]
- 24.Akinyemi OO, Owoaje ET, Ige OK, Popoola OA. Comparative study of mental health and quality of life in long-term refugees and host populations in Oru-Ijebu, Southwest Nigeria. BMC research notes. 2012;5:394. doi: 10.1186/1756-0500-5-394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhou X-h, McClish DK, Obuchowski NA. Statistical methods in diagnostic medicine. 2. Oxford: Wiley-Blackwell; 2011. [Google Scholar]
- 26.Begg CB, Greenes RA. Assessment of diagnostic tests when disease verification is subject to selection bias. Biometrics. 1983;39(1):207–215. [PubMed] [Google Scholar]
- 27.Pepe M. The statistical evaluation of medical tests for classification and prediction. Oxford: Oxford University Press; 2003. [Google Scholar]
- 28.Brugha TS, Jenkins R, Taub N, Meltzer H, Bebbington PE. A general population comparison of the Composite International Diagnostic Interview (CIDI) and the Schedules for Clinical Assessment in Neuropsychiatry (SCAN) Psychol Med. 2001;31(6):1001–1013. doi: 10.1017/s0033291701004184. [DOI] [PubMed] [Google Scholar]
- 29.Jordanova V, Wickramesinghe C, Gerada C, Prince M. Validation of two survey diagnostic interviews among primary care attendees: a comparison of CIS-R and CIDI with SCAN ICD-10 diagnostic categories. Psychol Med. 2004;34(6):1013–1024. doi: 10.1017/s0033291703001727. [DOI] [PubMed] [Google Scholar]
- 30.Kessler RC, Ustün TB World Health O. The WHO World Mental Health Surveys: global perspectives on the epidemiology of mental disorders. Cambridge; New York; Geneva: Cambridge University Press; 2008. Published in collaboration with the World Health Organization. [Google Scholar]
- 31.Reise SP, Widaman KF, Pugh RH. Confirmatory factor analysis and item response theory: two approaches for exploring measurement invariance. Psychological bulletin. 1993;114(3):552–566. doi: 10.1037/0033-2909.114.3.552. [DOI] [PubMed] [Google Scholar]
- 32.Yu X, Tam WW, Wong PT, Lam TH, Stewart SM. The Patient Health Questionnaire-9 for measuring depressive symptoms among the general population in Hong Kong. Comprehensive psychiatry. 2012 doi: 10.1016/j.comppsych.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 33.Kessler RC, Andrews G, Mroczek D, Ustun B, Wittchen H-U. The World Health Organization Composite International Diagnostic Interview short-form (CIDI-SF) International Journal of Methods in Psychiatric Research. 1998;7(4):171–185. [Google Scholar]
- 34.Ghimire DJ, Chardoul S, Kessler RC, Axinn WG, Adhikari BP. Modifying and validating the Composite International Diagnostic Interview (CIDI) for use in Nepal. Int J Methods Psychiatr Res. 2013;22(1):71–81. doi: 10.1002/mpr.1375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tsuang MT, Tohen M, Jones PB. Textbook of psychiatric epidemiology. Chichester, West Sussex; Hoboken, NJ: Wiley-Blackwell; 2011. [Google Scholar]
- 36.Patel V, Simon G, Chowdhary N, Kaaya S, Araya R. Packages of care for depression in low- and middle-income countries. PLoS medicine. 2009;6(10):e1000159. doi: 10.1371/journal.pmed.1000159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alem A. Mental health services and epidemiology of mental health problems in Ethiopia. Ethiopian medical journal. 2001;39(2):153–165. [PubMed] [Google Scholar]
- 38.Giel R. The prehistory of psychiatry in Ethiopia. Acta psychiatrica Scandinavica supplementum. 1999;397:2–4. doi: 10.1111/j.1600-0447.1999.tb10686.x. [DOI] [PubMed] [Google Scholar]
- 39.Araya R, Rojas G, Fritsch R, Gaete J, Rojas M, Simon G, Peters TJ. Treating depression in primary care in low-income women in Santiago, Chile: a randomised controlled trial. Lancet. 2003;361(9362):995–1000. doi: 10.1016/S0140-6736(03)12825-5. [DOI] [PubMed] [Google Scholar]
- 40.Bolton P, Bass J, Neugebauer R, Verdeli H, Clougherty KF, Wickramaratne P, Speelman L, Ndogoni L, Weissman M. Group interpersonal psychotherapy for depression in rural Uganda: a randomized controlled trial. JAMA. 2003;289(23):3117–3124. doi: 10.1001/jama.289.23.3117. [DOI] [PubMed] [Google Scholar]
- 41.Patel V, Chisholm D, Rabe-Hesketh S, Dias-Saxena F, Andrew G, Mann A. Efficacy and cost-effectiveness of drug and psychological treatments for common mental disorders in general health care in Goa, India: a randomised, controlled trial. Lancet. 2003;361(9351):33–39. doi: 10.1016/S0140-6736(03)12119-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.