Abstract
Diabetes is the sixth leading cause of death in the United States. To date, most research and resulting clinical strategies have focused on the individual with short-term health improvements that have not been maintained over time. Researchers more recently have recognized the need to consider the social determinants of diabetes and health along with individual factors. The purpose of this literature review is to examine current understanding of the social determinants affecting diabetes and health. A search of medical and nursing literature was conducted using PubMed, PsychInfo, CINAHL and MEDLINE databases, selecting articles published between 2000 and 2013. Search terms included: type 2 diabetes, social determinants, and health determinants. Inclusion criteria were: English language, human studies, social determinants of diabetes and health, and research in the United States. Additional search methods included reference chaining of the literature. Twenty research articles met the inclusion criteria for the review and analysis and included quantitative and qualitative methods. All studies selected for this review were descriptive in nature (n = 20). Fifteen studies were quantitative studies and five were qualitative studies. No intervention studies met inclusion criteria. Each study is summarized and critiqued. Study findings indicate that external or upstream factors consistently affect individuals diagnosed with diabetes, influencing self-management. Significant methodological limitations result directly from small sample sizes, convenience or nonprobability sampling, and low statistical power.
Keywords: Type 2 diabetes, Social determinants, Health determinants, Research, United States
Core tip: Social determinants of health and diabetes need to be considered when focusing on improving diabetes outcomes. Future research studies should focus on testing health outcomes of people with diabetes within the social determinants of health framework. Such research is particularly significant due to high rates of diabetes and subsequent disease sequelae.
INTRODUCTION
Diabetes Mellitus affects approximately 25.6 million individuals or 11.3% of those over age 20. It is the sixth leading cause of death in the United States[1]. Diabetes places the individual at risk for serious long term complications including blindness, cardiovascular disease, end stage renal disease, hypertension, stroke, neuropathy, lower limb amputations, and premature death[1]. Estimated annual healthcare cost in 2012 for diabetes and its resulting complications was $245 billion[2]. Given the considerable differences internationally in methods of allocating health care resources, systems of funding and/or paying for care, and cultural attitudes to health and health care, the purpose of this review of the literature is to examine current understanding of the social determinants affecting diabetes and health in the United States, and to make recommendations for future research.
Historically, research and resulting clinical approaches focusing on the individual have led to improvement in self-management outcomes and reduction of cardiovascular risk factors; however, these short-term improvements have not been maintained over time. Researchers more recently have recognized the need to consider factors external to the individual, namely the social determinants of diabetes and health in order to achieve the goal of sustainable improvement in health outcomes[3,4]. For example, the United States government document Healthy People 2020 emphasizes the social and environmental factors that affect the individual and his/her health. A Healthy People 2020 goal for the diabetes health indicator is to “reduce the disease and economic burden of diabetes mellitus, and improve the quality of life for all persons who have, or at risk for diabetes”[5].
Social determinants of health are social-ecological factors affecting health[6]. The person, his/her social network, and cultural and environmental conditions form the overall framework. Constructs include external/environmental socio-ecological influences on the individual (Figure 1); for example, culture, environment, education, working conditions, access to medical care, and community infrastructure[5]. Therefore, external or upstream determinants such as social support and elements of the community affect the health of the individual. Specific socio-ecological factors identified from this literature review are examined below.
Figure 1.
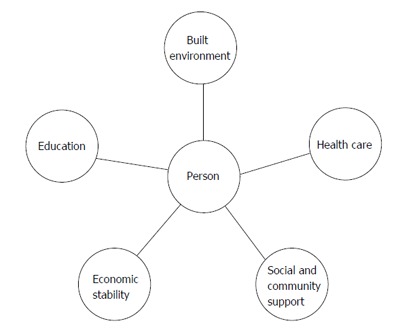
Social determinants influencing the individual’s self-management of type 2 diabetes.
Built environment/community infrastructure
Components of the physical environment include factors such as transportation, neighborhood safety, and healthy food. When barriers to these factors are present to individuals with diabetes, inadequate access to resources among such disadvantaged populations means fewer resources are available to overcome barriers, thus effects are magnified[7-9]. For example, limited transportation in rural areas may require travel outside the local community to gain access to healthcare providers or access to healthy foods[6]. Urban residents may face transportation barriers such as lack of sidewalks[9], discouraging individuals from walking as a form of physical activity. Lack of public transportation in rural or urban areas can hinder travel for access to healthcare. Lack of neighborhood safety contributes to health disparities. An example of compounding factors is as follows: urban centers may have high crime rates with consequently fewer businesses and employment; reduced access to services including food and medical care; and diminished opportunity for outdoor activity including exercise[10]. Research has shown a relationship between improved health outcomes and access to healthy foods[11,12]. Emerging research in the area of nutraceuticals indicates that certain foods may provide health benefits to reduce disease process progression in diabetes and hyperlipidemia[12]. However, this relationship is a complicated one, as demonstrated by Jones-Smith et al[13] who found that, even with access to healthy food, socioeconomic status remains a strong predictor for obesity among African Americans diagnosed with diabetes.
Economic stability
Research has demonstrated a direct relationship between socio-economic status and health outcomes; however, other factors may explain a degree of variance in this relationship[14]. Zheng et al[14] found that education level, employment, and family income affect socioeconomic status and therefore health.
Education
Greater educational attainment has been linked with improved health outcomes[15] possibly because of a greater likelihood of socio-economic stability compared to those with lower levels of education. Other related factors may be the stability derived from marriage and/or a wider range of opportunities for better employment[15]. Moreover, research has shown that individuals with higher levels of education are more likely to participate in preventive healthcare including eating healthier (foods), being more physically active, and avoiding obesity[16].
Health care/access to medical care
Individuals may be subject to disparity in the availability of healthcare resources, including access to medical care, based on factors such as socioeconomic status, place of residence, race/ethnicity, and culture. Socioeconomic factors include educational level which in turn influences health insurance status[16]. Low income inner cities and remote rural regions often lack both primary and specialty healthcare providers, decreasing access to healthcare for inhabitants with chronic illnesses such as diabetes, hypertension, and cardiovascular disease. Absent or inadequate care may result in worsening or compounding of long-term effects of chronic diseases[17,18]. For example, recent research focusing on infants born preterm or with low birth weight demonstrates an increase in the development of insulin resistance and impaired glucose tolerance as adults[19,20]. Lower socioeconomic status may be associated with an individual’s perception that lack of a collaborative patient-provider relationship is associated with improved diabetes outcomes[21].
Culture/social and community support
Social support includes individuals’ “formal and informal relationships that give rise to a belief that one is cared for or supported emotionally in a defined situation such as working toward improving health outcomes”[22]. Degree of social support may vary between individuals and among ethnic groups; for example, research revealed that Hispanic individuals diagnosed with diabetes prefer group medical visits for self-management support whereas individuals from other ethnic groups have no preference[23]. Just as greater social support correlates with improved self-management outcomes, the perception of negative or low levels of social support has been shown to increase the risk of fewer self-management behaviors[24].
RESEARCH
A search of medical and nursing literature was conducted using PubMed, PsychInfo, CINAHL and MEDLINE databases. Additional search methods included reference chaining of the literature. Search terms included type 2 diabetes, social determinants and health determinants. Inclusion criteria were English language, human studies, social determinants of diabetes and health, and research in the United States. Exclusion criteria were type 1 diabetes, reviews, and studies not focusing primarily on social determinants of diabetes and health; for example, biomarkers. The initial search of the literature retrieved 59036 articles on type 2 diabetes; 12871 articles on social determinants; 14866 articles on health determinants. Sixty one duplicate articles, one book review brief, one editorial commentary, and two conference proceeding abstracts were also excluded (Figure 2). Twenty articles met criteria for the review (Table 1).
Figure 2.
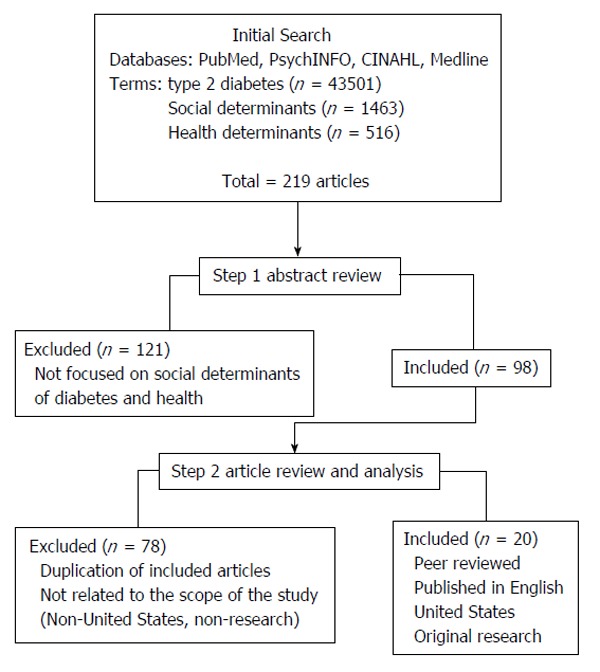
Manuscript selection for systematic review of the social determinants of diabetes and health.
Table 1.
Summary of reviewed studies
| Ref. | Purpose | Design/method | Sample | Findings | Strengths/limitations/implications |
| Chaufan et al[25] (2011) | To examine “upstream” social determinants of health in a Latino immigrant population focusing on T2DM risk and food environment | Mixed methods focus groups, Food store survey instrument California | Staff members (n = 6); clients (n = 15) | Poverty prevented Latino immigrants from access to adequate housing, high quality education, and culturally appropriate food choices | Community-based interviews elicited lived experience of Latino immigrant population Limitations: small sample size, nonrandomized, descriptive study Implications: Policy change to enable access to affordable culturally acceptable healthy foods |
| Carbone et al[26] (2007) | To describe factors influencing Latino (Puerto Rican) diabetes self-management | Qualitative-focus groups Health center in Massachusetts, United States | Healthcare providers (n = 15) Patients (n = 37) | Cultural influence of family through traditional gender roles; financial restraints Social network (family and friends) source of strength; spirituality and faith important; discrepancy between healthcare provider and patient focus in self-management | Community-based limitations: Small sample size, qualitative study, not generalizable to all Latino populations Implications: account for inclusion of family and social networks in diabetes self-management education, need for increased cultural awareness by Healthcare provider of influencing factors on patient self-management |
| Chaufan et al[27] (2011) | To gain understanding how food environments influence a low income immigrant population | Qualitative-focus groups | Staff (n = 6) Clients (n = 15) | Barriers to food access: transportation, language barriers, poverty, employment | Strengths: community based Limitations: small sample size, not generalizable Implications: Need for policy to increase food access for immigrant populations in lower socio-economic levels |
| Tjia et al[28] (2008) | To gain understanding of barriers to medication adherence among older adults with T2DM | Qualitative-semi structured interviews | Adults over age 65 (n = 22) Female n = 16 | Older adults with T2DM had concerns about medication cost or medication burden but did not discuss with physician | Strengths: perspective of older adults Limitations: small sample size, not generalizable Implications: need for increased patient-physician communication; policy level for messages to encourage open patient-physician dialogue for medical treatment |
| Denham et al[29] (2010) | To explore perceived patient barriers to diabetes education among healthcare providers | Cross-sectional survey | Healthcare providers from three practice settings: federally qualified healthcare centers; health departments; clinics (n = 182) | Perceived barriers: transportation; fewer diabetes educators and physicians; lack of insurance; education materials not screened for literacy levels nor cultural appropriateness | Strengths: look at perceived barriers to diabetes education among healthcare providers Limitations: small sample size, multiple sites, sample bias Implications: policy need to increase diabetes education reimbursement to providers for all individuals nationally; need to screen materials for literacy levels |
| Heuer et al[30] (2006) | To describe Hispanic migrant farmworkers perceptions of diabetes | Qualitative phenomenological study | Migrant farmworkers (n = 12) Female n = 6 | Cultural/folk beliefs that diabetes was caused by stress or emotions | Strengths: focused on hispanic explanatory model of diabetes Limitations: small sample size, not generalizable Implications: need to tailor diabetes education to address culture and health beliefs |
| Shigaki et al[31] (2010) | To examine how patients diagnosed with type 2 diabetes view role of nurses in disease management | Qualitative Semi-structured individual interviews | n = 13 Female n = 7 White n = 9 African American n = 3 Other n = 1 | Nurse viewed as a positive partner in disease management, patients prefer team-based medical care, open communication between healthcare providers and patient | Strengths: Patient perspective on nurse as partner in healthcare Limitation: small sample size; sample bias Implications: Nurse partner may provide link between patient and improving health outcomes in individuals with multiple co-morbidities including diabetes |
| Fitzgerald et al[32] (2008) | To determine diabetes care perceptions in patient and provider | Quantitative cross sectional survey | Providers n = 71 Patients: n = 273 female 61% White 63% African American 33% | Patient and provider differences included patients with more positive attitudes family support, paying for diabetes care | Strengths: quantitative study using reliable and valid instrument Limitations: may not be representative for patients with no co-morbidities Implications: Importance of communication between patient and provider and not making assumptions about patients |
| Zulkowski et al[33] (2005) | To examine differences between patient self-report and provider documentation in rural health center | Quantitative cross sectional survey; medical record review | n = 149 Female n = 86 | Statistical difference between patient and provider on medical management or diabetes knowledge; most patients had not been seen by diabetes educator or dietician | Strengths: good response rate (61%); limitations: race not documented Implications: Need for increased access to diabetes education in rural areas; need for open communication between patient and provider |
| Ford et al[34] (2002) | To determine relationship between socio-economic status and race on diabetes management | Quantitative-random sampling by socio-economic status and race | n = 50 African American n = 21 Caucasian n = 29 Female n = 22 | Differences in perception of sense of loss by race but not socio-economic status | Strengths: Limitations: small sample size: not generalizable; underpowered (α = 0.34) Implications: Need for education to stress management to prevent disease related complications |
| Mani et al[35] (2011) | To determine the influence of social networks on diabetes self-management | Cross-sectional survey | n = 154 Female n = 88 White n = 78 African American n = 61 | Diabetes concern increased when larger social network diagnosed with diabetes | Strengths: patient perspective of importance of social networks Limitations: not generalizable-sample from two inner city clinics, only English speaking, data skewed Implications: Important to consider the influence of social networks on diabetes self-management |
| Song et al[36] (2012) | To examine social networks among Korean Americans diagnosed with type 2 diabetes | Cross-sectional survey from a larger study | n = 83 Female n = 35 Married n = 73 | Gender differences in source of support, men sought spouse, women had higher unmet needs for social support than men, self-efficacy negatively associated with unmet social support, education level strong predictor of self-care activities, unmet needs for social support negatively associated with diabetes self-care | Strengths: patient perception of social support Limitations: small homogenous sample; not generalizable Implications: need to recognize the role of gender in determining social support among Korean Americans |
| Kollannoor-Samuel et al[37] (2011) | To identify influence of social determinants of health on FPG and HbA1c among low income Latinos | Cross-sectional | n = 211 Female n = 155 Puerto Rican n = 171 Unemployed n = 178 Spanish speaking only n = 138 | Lower socio-economic status had higher FPG and HbA1c levels; better long term glycemic control when insured; increased physical activity associated with lower FPG and HbA1c levels | Strengths: sample size; part of larger RCT Limitations: large number of female participants-not generalizable or transferable to other Latino populations; unknown length of time since diagnosis Implications: Importance of physical activity for improved glycemic control; need for health insurance, increase in education to improve glycemic outcomes over the long term |
| Chiu et al[38] (2011) | To determine how gender influences functional limitations with type 2 diabetes | Secondary data analysis | n = 1619 Female n = 861 | Psychosocial factors mediator between biological and exercise factors | Strengths: consistent with previous research Limitations: participant self report; no causal pathway Implications: Need to incorporate gender and psychosocial factors in diabetes treatment plan |
| Iida et al[39] (2010) | Examine role of spousal support for individual diagnosed with type 2 diabetes | Mixed methods-longitudinal Computer diary survey; individual interviews | n = 129 married couples Caucasian 75%; African American 23.6% | Physical symptoms increased spousal support; women gave higher level of support when spouse worried about diabetes; less spousal support when negative emotional effect from previous day | Strengths: sample size Longitudinal study, diary Limitations: unable to determine causal effect Implications: Need to measure and include spousal support in diabetes self-management plan |
| Mayberry et al[40] (2005) | To assess determinants of glycemic monitoring by primary care provider among medicaid beneficiaries | Retrospective cohort study | n = 3321 African American (2025) 61%; White (1296) 39%; Female 74.6%; Urban 49.6%; rural 50.4% | African Americans diagnosed at younger age; frequency of physician visits and medication prescription strong predictor of meeting ADA recommendation guideline for HbA1c monitoring; low monitoring of HbA1c and FPG among medicaid beneficiaries with type 2 diabetes, no significance between Black and White Medicaid beneficiaries for diabetes monitoring | Strengths: provides insight into determinants of glucose monitoring in Medicaid beneficiaries Limitations: Secondary data analysis; inability to determine patient-physician relationship Implications: Need to establish ADA evidence guidance protocol in office practice settings |
| Ford et al[41] (2005) | To determine estimates of obesity and diabetes weight information from healthcare providers in 100 United States metropolitan service areas | Cross sectional survey: 2000 Behavioral Risk Factor Surveillance System | n =81917 individuals with BMI data Sample size varied due to missing data | Highest prevalence of obesity Appalachian region; OR of being diagnosed with diabetes 3.5 higher in Charleston WV than Santa Fe NM; weight loss or maintenance discussed with physician 11.7%-34.6% | Strength: study at community level Limitation: secondary data analysis, missing data; self report Implications: Policy level- need to examine determinants of obesity and diabetes at local metropolitan service areas. Healthcare providers need to include discussion of weight management for individuals diagnosed with obesity or diabetes |
| Adams et al[42] (2008) | To examine medication adherence as a factor of glycemic control based on race | Secondary data analysis newly diagnosed patients prescribed oral medications | n = 1806 Black n = 467 White n = 1339 | Black patients higher A1c at diagnosis; insufficient evidence to determine medication adherence by race | Strengths: limitations: unable to determine causal effect; potential overestimation of medication adherence based on data; implications: Need at policy level to provide screening for earlier diagnosis of Black and female patients |
| Aikens et al[43] (2005) | To examine the relationship of patient-provider communication on diabetes self-management and outcomes | Cross-sectional Telephone survey | n = 736 White 51% Black 20% Hispanic 11.9% Female 31.6% | Primary care provider main manager of diabetes (70.9%) General patient-provider communication related to improved quality of life; diabetes specific patient-provider communication related to glycemic control | Strengths: sample across three health systems; limitations: cross-sectional study; self-report; implications: need for open patient-provider communication to enhance problem solving, need to tailor management plan to individual patient |
| Paris et al[44] (2001) | To determine if determinants of type 2 diabetes were present in personnel entering the military | Cross-sectional secondary data analysis | Diagnosed with diabetes n = 419 Not diagnosed with diabetes n = 627 | Enlisted military rank as socioeconomic measure for diabetes diagnosis higher in lower rank, minorities higher level of diabetes; educational not significant variable | Strengths: adequate power Limitations: no causal effect; potential for misclassification of diabetes diagnosis in database; implications: need for focus on policy level for increased physical activity and body mass index monitoring |
FPG: Fasting plasma glucose; HbA1c: Glycosylated hemoglobin A1c; BMI: Body mass index; T2DM: Type 2 diabetes mellitus; RCT: Randomized control trial; ADA: American diabetes Association.
Twenty articles met the inclusion criteria for the review and analysis. All studies selected for this review were descriptive in nature (n = 20). Fifteen studies were quantitative studies and five were qualitative studies[25-29,32-44]. Although sample size ranged from 15 to 81917 participants, many samples were fewer than one hundred subjects. All studies focused on individuals diagnosed with diabetes. There were no interventional or randomized control trial studies. The majority were cross-sectional, collecting data only once. For quantitative studies, two were mixed methods, including a survey and interview; five were secondary data analysis, and eight were surveys. Qualitative studies used either focus groups or individual semi-structured interviews (n = 5). Fourteen studies focused on social determinants from the patient or client perspective; three studies focused both on staff/healthcare provider and patient/client, while three studies viewed social determinants of health from the perspective of the healthcare provider alone. All studies focused on one or more of the constructs of social determinants of health: built environment, economic stability, health care, or culture/social support.
Built environment/community infrastructure
Authors of four articles discussed the built environment and community infrastructure. Research studies used purposive sampling, limiting the generalizability of findings to other populations. Three studies focused on populations known to have a disproportionate burden of type 2 diabetes, including African Americans and Hispanic/Latino. The built environment was a stronger predictor of health outcomes than race. Three studies[25-27] reported on upstream social determinants and the influence on food environments for at risk immigrant Hispanic population. Findings included high rates of poverty with 60% of living below United States definition of poverty and 40% living at 170% below federal poverty level. Educational attainment was less than the United States average with 80% of individuals not entering college. Thirty-three percent had not completed elementary school. In comparison the national United States rate of high school completion is 89.9% in 2010[25]. One study focused on Asian Americans. No studies included American Indians or Pacific Islanders. Two studies were community-based, focusing on food environment and access to healthy food. Transportation was discussed in three articles as a barrier to access both healthcare and healthy food. Research participants reported lack of access to quality, quantity, and culturally-acceptable food choices[25-27]. Study limitations include small sample size and descriptive statistics.
Economic stability
Five articles focused on economic stability. Three studies were cross-sectional survey, one involved focus group interviews, and one was a secondary analysis. Sample size in these studies ranged from 50 to 419. Discussion focused on health insurance, financial barriers, poverty, and affordability of medication from the patient or client perspective. One study focused on indirect economic factors, such as military rank, as a predictor of diabetes diagnosis[44]. Two studies compared patient/client perspectives to healthcare provider perceptions of economic barriers to diabetes self-management[25,32]. Three of the five studies compared race as a factor in economic stability within Latino and African American populations[26,34,37]. Findings included individual acknowledgement that economic distress in diabetes self-management was important however, factors were also identified as sources of additional strength for individuals diagnosed with diabetes. Sources of support included culture and/or social support[26,34]. The influences of economic factors by race/ethnicity on diabetes outcomes were non-conclusive. Therefore, economic stability may be a strong determinant of diabetes and health regardless of race/ethnicity. Studies focused on target populations, limiting to selected urban regions for study.
Health care/access to medical care
There were nine studies found in which researchers examined the role of health care and/or access to medical care within the social determinants of diabetes and health framework. One study compared patients’ and healthcare providers’ perspectives on diabetes management[32]. Another research report examined healthcare providers’ perception of patient barriers to diabetes management[29]. The remaining seven articles focused on the patient’s perceptions of healthcare related to diabetes management and barriers to care. Sample size for the patient-only studies ranged from 13 to 81917. Eight studies were cross-sectional descriptive in design, and one was a secondary data analysis from the Behavioral Risk Factor Surveillance System. Most researchers reported that patients viewed their health in a more positive light than did providers based on medical record reviews. The concerns of healthcare provider included the costs associated with diabetes management[29,32]. Patient-provider communication varied among patients. Three articles focused on positive health outcomes with open patient-provider communication[31,40,43]. One article described physicians as often initiating communication about medication adherence, whereas patients were hesitant to initiate communication with physicians relating to medication burden and costs[28]. This may, in part, explain perceived lack of patient medication adherence which increases the potential for poorer health outcomes. One qualitative study described patients’ preference for diabetes care teams in which the team’s link between patient and physician was a nurse[31]. Two studies demonstrated increased quality of life and better glycemic control with positive patient-provider communication[40,43]. However, when looking at diabetes prevention and knowledge, two studies reported the need for provision of diabetes education focusing on basic management and the need for discussion of weight management or weight loss for diabetes prevention[33,41].
Culture/social and community support
Seven articles met the inclusion criteria focusing on the constructs of culture and community support. Four of the seven researchers reported on cross-sectional surveys, one study involved focus groups in a community setting, one study used a phenomenological method of analysis, and one used mixed methods incorporating a computer diary and individual interviews. Two of the seven articles included healthcare provider perceptions. Of these two articles, one had a sample of both patient and healthcare provider. Sample size for the seven articles ranged from 12 to 273. Two articles focused on cultural determinants of diabetes and health in Latino/Hispanic populations. Cultural beliefs in Hispanic populations included the belief that diabetes was caused by increased stress[30]. The authors noted that the discovery of this belief provides an opportunity for healthcare providers or trusted community sources to provide education to increase diabetes knowledge. Three articles focused on the traditional roles of gender and culture, whereby married women provided increased support to their spouse when he voiced concerns about diabetes and health[26,36,39]. One article focusing on Korean Americans found that women had an increase in unmet needs when providing support for their spouses, which negatively affected their diabetes self-care[36]. Two articles discussed social support or social networks as positive influences for diabetes self-management and health[26,32]. However, one article described African American patients’ concern about their diabetes management and health when multiple members of their social network were diagnosed with diabetes or experienced complications of diabetes[35]. One article discussed healthcare providers’ perceived barriers in rural healthcare settings[29], pointing out an apparent lack of culturally appropriate educational materials within healthcare clinic settings.
CONCLUSION
This critique of the literature about social determinants of diabetes and health focused on research of United States populations published between 2000 and 2013. A total of 20 research studies met established criteria. All 20 studies identified for this review were descriptive. The majority of studies were published in journals with a focus on public health or nursing. Results of this review are useful for health professionals who develop programs and/or interventions for people diagnosed with diabetes because evidence indicates that social determinants affect patient adherence, effectiveness of treatments, and overall health outcomes.
Study findings indicate that external or upstream factors prominently affect individuals diagnosed with diabetes, in part by influencing self-management and in turn exerting lasting effects on long-term diabetes and health outcomes. The most significant methodological limitations of the studies examined result directly from small sample size, convenience or nonprobability sampling, and low statistical power. Methodological limitations of studies included in this review also include a lack of intervention studies. Future research needs to include community-based intervention studies focusing on the reduction of diabetes disparities and improvement of health outcomes within the social determinants of health framework. Such research is particularly needed given the high rates of diabetes and subsequent disease sequelae. Cultural tailoring of diabetes prevention educational materials and cultural tailoring of education in group settings may afford the means to increase patients’ knowledge of the disease for earlier diagnosis and earlier intervention to prevent diabetes complications. Encouragement of spousal support within the construct of acknowledging cultural norms may provide a means for improving diabetes outcomes and health. The influence of social determinants of health on diabetes outcomes needs to be tested in intervention studies to provide a foundation for effective interventions to impact the current epidemic of diabetes in the United States and around the globe. Prospective interventional studies evaluating the influence of social determinants will be key to lay a foundation for effective interventions and improvement of diabetes and health outcomes.
Footnotes
P- Reviewers: Ciccone MM, Cui WP S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
References
- 1.Centers for Disease Control and Prevention. Diabetes Report Card 2012. Atlanta, GA: US Department of Health and Human Services; 2012. [Google Scholar]
- 2.Dall TM, Zhang Y, Chen YJ, Quick WW, Yang WG, Fogli J. The economic burden of diabetes. Health Aff (Millwood) 2010;29:297–303. doi: 10.1377/hlthaff.2009.0155. [DOI] [PubMed] [Google Scholar]
- 3.Hill J, Nielsen M, Fox MH. Understanding the social factors that contribute to diabetes: a means to informing health care and social policies for the chronically ill. Perm J. 2013;17:67–72. doi: 10.7812/TPP/12-099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liburd LC, Jack L, Williams S, Tucker P. Intervening on the social determinants of cardiovascular disease and diabetes. Am J Prev Med. 2005;29:18–24. doi: 10.1016/j.amepre.2005.07.013. [DOI] [PubMed] [Google Scholar]
- 5.Healthy People 2020. US Department of Health and Human Services. Available from: http: //www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=8.
- 6.Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health. 2011;32:381–398. doi: 10.1146/annurev-publhealth-031210-101218. [DOI] [PubMed] [Google Scholar]
- 7.Hutch DJ, Bouye KE, Skillen E, Lee C, Whitehead L, Rashid JR. Potential strategies to eliminate built environment disparities for disadvantaged and vulnerable communities. Am J Public Health. 2011;101:587–595. doi: 10.2105/AJPH.2009.173872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DeGuzman PB, Kulbok PA. Changing health outcomes of vulnerable populations through nursing’s influence on neighborhood built environment: a framework for nursing research. J Nurs Scholarsh. 2012;44:341–348. doi: 10.1111/j.1547-5069.2012.01470.x. [DOI] [PubMed] [Google Scholar]
- 9.Hood E. Dwelling disparities: how poor housing leads to poor health. Environ Health Perspect. 2005;113:A310–A317. doi: 10.1289/ehp.113-a310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rashid JR, Spengler RF, Wagner RM, Melanson C, Skillen EL, Mays RA, Heurtin-Roberts S, Long JA. Eliminating health disparities through transdisciplinary research, cross-agency collaboration, and public participation. Am J Public Health. 2009;99:1955–1961. doi: 10.2105/AJPH.2009.167932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matson-Koffman DM, Brownstein JN, Greany ML. A site-specific literature review of policy and environmental interventions that promote physical activity and nutrition for cardiovascular health: what works? Am J Health Promot. 2005;19:167–193. doi: 10.4278/0890-1171-19.3.167. [DOI] [PubMed] [Google Scholar]
- 12.Scicchitano P, Cameli M, Maiello M, Modesti PA, Muiesan NL, Novo S. Nutraceuticals and dyslipidaemia: Beyond the common therapeutics. J Funct Foods. 2014;6:11–32. [Google Scholar]
- 13.Jones-Smith JC, Karter AJ, Warton EM, Kelly M, Kersten E, Moffet HH, Adler N, Schillinger D, Laraia BA. Obesity and the food environment: income and ethnicity differences among people with diabetes: the Diabetes Study of Northern California (DISTANCE) Diabetes Care. 2013;36:2697–2705. doi: 10.2337/dc12-2190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zheng H, George LK. Rising U.S. income inequality and the changing gradient of socioeconomic status on physical functioning and activity limitations, 1984-2007. Soc Sci Med. 2012;75:2170–2182. doi: 10.1016/j.socscimed.2012.08.014. [DOI] [PubMed] [Google Scholar]
- 15.Montez JK, Zajacova A. Explaining the widening education gap in mortality among U.S. white women. J Health Soc Behav. 2013;54:166–182. doi: 10.1177/0022146513481230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pampel FC, Krueger PM, Denney JT. Socioeconomic Disparities in Health Behaviors. Annu Rev Sociol. 2010;36:349–370. doi: 10.1146/annurev.soc.012809.102529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Behringer B, Friedell GH. Appalachia: where place matters in health. Prev Chronic Dis. 2006;3:A113. [PMC free article] [PubMed] [Google Scholar]
- 18.Murray CJ, Kulkarni S, Ezzati M. Eight Americas: new perspectives on U.S. health disparities. Am J Prev Med. 2005;29:4–10. doi: 10.1016/j.amepre.2005.07.031. [DOI] [PubMed] [Google Scholar]
- 19.Ciccone MM, Scicchitano P, Salerno C, Gesualdo M, Fornarelli F, Zito A, Filippucci L, Riccardi R, Cortese F, Pini F, et al. Aorta structural alterations in term neonates: the role of birth and maternal characteristics. Biomed Res Int. 2013;2013:459168. doi: 10.1155/2013/459168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ingelfinger JR, Nuyt AM. Impact of fetal programming, birth weight, and infant feeding on later hypertension. J Clin Hypertens (Greenwich) 2012;14:365–371. doi: 10.1111/j.1751-7176.2012.00660.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nam S, Chesla C, Stotts NA, Kroon L, Janson SL. Barriers to diabetes management: patient and provider factors. Diabetes Res Clin Pract. 2011;93:1–9. doi: 10.1016/j.diabres.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 22.Strom JL, Egede LE. The impact of social support on outcomes in adult patients with type 2 diabetes: a systematic review. Curr Diab Rep. 2012;12:769–781. doi: 10.1007/s11892-012-0317-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sarkar U, Piette JD, Gonzales R, Lessler D, Chew LD, Reilly B, Johnson J. Preferences for self-management support: findings froma survey of diabetes patients in safety-net health systems. Patient Educ Couns. 2008;34:1037–1044. doi: 10.1016/j.pec.2007.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tang TS, Brown MB, Funnell MM, Anderson RM. Social support, quality of life, and self-care behaviors amongAfrican Americans with type 2 diabetes. Diabetes Educ. 2008;34:266–276. doi: 10.1177/0145721708315680. [DOI] [PubMed] [Google Scholar]
- 25.Chaufan C, Davis M, Constantino S. The twin epidemics of poverty and diabetes: understanding diabetes disparities in a low-income Latino and immigrant neighborhood. J Community Health. 2011;36:1032–1043. doi: 10.1007/s10900-011-9406-2. [DOI] [PubMed] [Google Scholar]
- 26.Carbone ET, Rosal MC, Torres MI, Goins KV, Bermudez OI. Diabetes self-management: perspectives of Latino patients and their health care providers. Patient Educ Couns. 2007;66:202–210. doi: 10.1016/j.pec.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 27.Chaufan C, Constantino S, Davis M. ‘It’s a full time job being poor’: understanding barriers to diabetes prevention in immigrant communities in the USA. Pub Health. 2012;22:147–158. [Google Scholar]
- 28.Tjia J, Givens JL, Karlawish JH, Okoli-Umeweni A, Barg FK. Beneath the surface: discovering the unvoiced concerns of older adults with type 2 diabetes mellitus. Health Educ Res. 2008;23:40–52. doi: 10.1093/her/cyl161. [DOI] [PubMed] [Google Scholar]
- 29.Denham SA, Remsburg K, Wood L. Diabetes education in the Appalachian region: providers’ views. Rural Remote Health. 2010;10:1321. [PubMed] [Google Scholar]
- 30.Heuer L, Lausch C. Living with diabetes: perceptions of Hispanic migrant farmworkers. J Community Health Nurs. 2006;23:49–64. doi: 10.1207/s15327655jchn2301_5. [DOI] [PubMed] [Google Scholar]
- 31.Shigaki CL, Moore C, Wakefield B, Campbell J, LeMaster J. Nurse partners in chronic illness care: patients’ perceptions and their implications for nursing leadership. Nurs Adm Q. 2010;34:130–140. doi: 10.1097/NAQ.0b013e3181d917bd. [DOI] [PubMed] [Google Scholar]
- 32.Fitzgerald JT, Stansfield RB, Tang T, Oh M, Frohna A, Armbruster B, Gruppen L, Anderson R. Patient and provider perceptions of diabetes: measuring and evaluating differences. Patient Educ Couns. 2008;70:118–125. doi: 10.1016/j.pec.2007.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zulkowski K, Coon P. Patient perceptions and provider documentation of diabetes care in rural areas. Ostomy Wound Manage. 2005;51:50–58. [PubMed] [Google Scholar]
- 34.Ford ME, Havstad SL, Brooks BL, Tilley BC. Perceptions of diabetes among patients in an urban health care system. Ethn Health. 2002;7:243–254. doi: 10.1080/1355785022000060709. [DOI] [PubMed] [Google Scholar]
- 35.Mani N, Caiola E, Fortuna RJ. The influence of social networks on patients’ attitudes toward type II diabetes. J Community Health. 2011;36:728–732. doi: 10.1007/s10900-011-9366-6. [DOI] [PubMed] [Google Scholar]
- 36.Song Y, Song HJ, Han HR, Park SY, Nam S, Kim MT. Unmet needs for social support and effects on diabetes self-care activities in Korean Americans with type 2 diabetes. Diabetes Educ. 2016;38:77–85. doi: 10.1177/0145721711432456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kollannoor-Samuel G, Chhabra J, Fernandez ML, Vega-López S, Pérez SS, Damio G, Calle MC, D’Agostino D, Pérez-Escamilla R. Determinants of fasting plasma glucose and glycosylated hemoglobin among low income Latinos with poorly controlled type 2 diabetes. J Immigr Minor Health. 2011;13:809–817. doi: 10.1007/s10903-010-9428-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chiu CJ, Wray LA. Gender differences in functional limitations in adults living with type 2 diabetes: biobehavioral and psychosocial mediators. Ann Behav Med. 2011;41:71–82. doi: 10.1007/s12160-010-9226-0. [DOI] [PubMed] [Google Scholar]
- 39.Iida M, Parris Stephens MA, Rook KS, Franks MM, Salem JK. When the going gets tough, does support get going? Determinants of spousal support provision to type 2 diabetic patients. Pers Soc Psychol Bull. 2010;36:780–791. doi: 10.1177/0146167210369897. [DOI] [PubMed] [Google Scholar]
- 40.Mayberry RM, Davis T, Alema-Mensah E, Samadi AR, Finley R, Jones A. Determinants of glycemic status monitoring in Black and White Medicaid beneficiaries with diabetes mellitus. J Health Care Poor Underserved. 2005;16:31–49. doi: 10.1353/hpu.2005.0128. [DOI] [PubMed] [Google Scholar]
- 41.Ford ES, Mokdad AH, Giles WH, Galuska DA, Serdula MK. Geographic variation in the prevalence of obesity, diabetes, and obesity-related behaviors. Obes Res. 2005;13:118–122. doi: 10.1038/oby.2005.15. [DOI] [PubMed] [Google Scholar]
- 42.Adams AS, Trinacty CM, Zhang F, Kleinman K, Grant RW, Meigs JB, Soumerai SB, Ross-Degnan D. Medication adherence and racial differences in A1C control. Diabetes Care. 2008;31:916–921. doi: 10.2337/dc07-1924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Aikens JE, Bingham R, Piette JD. Patient-provider communication and self-care behavior among type 2 diabetes patients. Diabetes Educ. 2005;31:681–690. doi: 10.1177/0145721705280829. [DOI] [PubMed] [Google Scholar]
- 44.Paris RM, Bedno SA, Krauss MR, Keep LW, Rubertone MV. Weighing in on type 2 diabetes in the military: characteristics of U.S. military personnel at entry who develop type 2 diabetes. Diabetes Care. 2001;24:1894–1898. doi: 10.2337/diacare.24.11.1894. [DOI] [PubMed] [Google Scholar]


