Abstract
Purpose
Less than 24 percent of Veterans received appropriate evaluation and/or treatment for osteoporosis within 6 months of an index fracture. An electronic consult (E-consult) service was implemented at 3 Veterans Affairs Medical Centers to facilitate identification of and to recommend management for patients with recent fracture.
Method
The E-consult service used clinical encounter data based on ICD9 diagnosis codes to prospectively identify patients with potential osteoporotic fractures. Eligible patients' medical records were reviewed by a metabolic bone specialist and an E-consult note was sent to the patient's primary provider with specific recommendations for further management. Recommendations were initiated at the provider's discretion.
Results
Between 2011 and 2013, the E-consult service identified 444 eligible patients with a low-trauma fracture who were not already on treatment. One hundred twenty-nine (29.1%) consults recommended immediate bisphosphonate treatment and 258 (58.1%) recommended bone density assessments. Primary providers responded by prescribing bisphosphonates in 74 patients (57.4%) and by ordering bone density testing in 183 (70.9%) patients. At the facility level, prior to implementation of the E-consult service, the rate of osteoporosis treatment following a fracture was 4.8% for bisphosphonates and 21.3% for calcium/vitamin D. After implementation, the treatment rate increased to 7.3% for bisphosphonates (P = 0.02) and 35.2% for calcium/vitamin D (P < 0.01).
Conclusion
While feasible and relatively low cost, an E-consult service modestly improved the rate of osteoporosis treatment among patients with a recent fracture. These results suggest that a program with direct patient interaction is probably required to substantially improve treatment rates.
Keywords: Osteoporosis, fracture, electronic medical record, bone density, health services research
Introduction
Low trauma fractures at all skeletal sites are associated with increased risk of future fractures.[1,2] Pharmacological interventions in patients with recent osteoporotic fracture have been shown to substantially reduce the risk of subsequent fractures, as well as improve quality of life and reduce mortality.[3,4] Therefore, the occurrence of a low trauma fracture should be considered a sentinel event that prompts providers to assess for and treat osteoporosis for secondary prevention.
Despite effective therapies, studies have demonstrated that osteoporosis management and treatment after a low trauma fracture remains inadequate, especially among men.[5-8] In 2010, the Office of the Inspector General (OIG) reviewed osteoporosis care among Veterans with low trauma fracture, and found that only 24% received appropriate care. System-wide quality improvement interventions were advocated including provider education, patient education, and improved surveillance components.[9]
We previously described the feasibility of the use of a regional clinical data repository to prospectively identify patients with recent fracture for inclusion in a centralized, remote osteoporosis electronic consult (E-consult) service.[10] We report the effects on osteoporosis screening and treatment within 3 Veterans Administration Medical Centers (VAMC) after initiation of the E-consult service among Veterans with recent fracture.
Methods
Patient identification and eligibility
The patient identification process has been described previously.[10] Briefly, potential patients were identified by a report from the central data warehouse based on fracture-related International Classification of Disease (ICD9) codes (733.93 - 733.95; 767.3; 800 - 829; V54.13). Electronic medical record screening was then completed remotely by the consult coordinator. Identified patients were eligible for E-consult if they were over age 50 years, had sustained a low trauma fracture within the last 6 months (fall from standing height or less), and had a primary care provider within the VAMC system. Exclusion criteria included fractures not considered osteoporotic (facial, skull, digital, or pathologic fracture), fractures occurring more than 10 years previously, an active prescription for a bisphosphonate, bone mineral density screening had already been obtained, estimated life expectancy of 1 year or less (e.g. hospice care), the patient had been offered and declined therapy, or interval death of the patient. All remaining patients were referred to a metabolic bone specialist for an osteoporosis E-consult. This study was approved by the Institutional Review Board at the Durham VAMC.
E-consult process and follow-up
The electronic medical record of each patient was reviewed by a metabolic bone specialist (endocrinologist or geriatrician). Specifically, the physician reviewed pertinent laboratory data (creatinine clearance, serum calcium, and 25-hydroxyvitamin D level), other clinical risk factors for fracture (low BMI, corticosteroid use, medical co-morbidities associated with fractures), and prior osteoporosis treatment if any. The physician then used an E-consult template note to summarize the relevant data and provide recommendations for initiation of osteoporosis treatment and/or further evaluation. Recommendations were based on current clinical practice guidelines from the National Osteoporosis Foundation and the Veterans Administration.[11,9] E-consults were then sent to the patient's primary care provider for review and co-signature. If the note was not co-signed within 1 month, a follow-up email reminder was sent. All E-consults were tracked 3 and 6 months after completion to determine whether recommendations for osteoporosis treatment, bone density testing with DXA scan, referral to Endocrinology and/or Nephrology for further evaluation, and calcium and vitamin D supplements were implemented.
Facility-level comparisons
To determine the impact of the E-consult program on osteoporosis treatment after fracture at a facility level, the proportion of Veterans over age 50 years prescribed a medication for osteoporosis within 3 to 6 months of a fracture was calculated using regional administrative data. For the 3 participating facilities, treatment rates from the 6 months preceding program implementation were compared to a 6-month period 1 year after program implementation. In addition, the changes in treatment rates for the participating facilities were compared to 3 non-participating VAMC facilities in the region. Comparison medical centers were selected on the basis of size, geographic proximity, and academic affiliation status.
For the comparison analysis, all Veterans with a potentially osteoporotic fracture assigned to a VAMC primary care provider were included. Because of the high number of subjects, complete chart abstraction, as was done for E-consults to exclude high trauma or other clinical contraindications to treatment, was not feasible. Therefore, treatment rates are expected to be lower than those reported by the OIG report and not comparable to quality metric thresholds (e.g. HEDIS) because this sample is expected to include patients in whom treatment is not necessary or is contraindicated. However, this convenience sample allows for quick measurement of the E-consult service's impact by comparing the medical centers' treatment rate before and after the implementation of the service, and compared to non-participating facilities.
Statistical Analysis
Baseline characteristics for the patients are described using proportions for categorical variables and means with standard deviations for continuous variables. Comparison of treatment rates prior to and after implementation the E-consult service was performed using Fisher's exact test of proportions. Comparison of the changes in treatment rates between intervention and non-intervention facilities was performed using Breslow-Day test for heterogeneity. Statistical significance was assessed for p < 0.05. Analyses were performed using SAS Version 9.3 (SAS institute, Cary, NC).
Results
Study Population
In the 3 participating VAMC facilities, there were 3840 fractures identified by a fracture-related ICD9 code, during the intervention period (Figure). Of these, 1981 were automatically excluded from E-consult due to ineligibility. The most common reason was because the Veteran was less than age 50 years. An additional 1296 were excluded during the chart extraction phase. The most common reason for exclusion during chart extraction was because the fracture occurred due to high trauma, followed by fracture occurring more than 10 years prior to the index clinic visit or clinical suspicion for a fracture was not confirmed by subsequent radiographic examination. Therefore, of 1859 fractures reviewed during chart extraction, 563 were subsequently reviewed by a metabolic bone specialist.
Figure. Process for identification of Veterans with recent low-trauma fracture, eligible for E-consult.
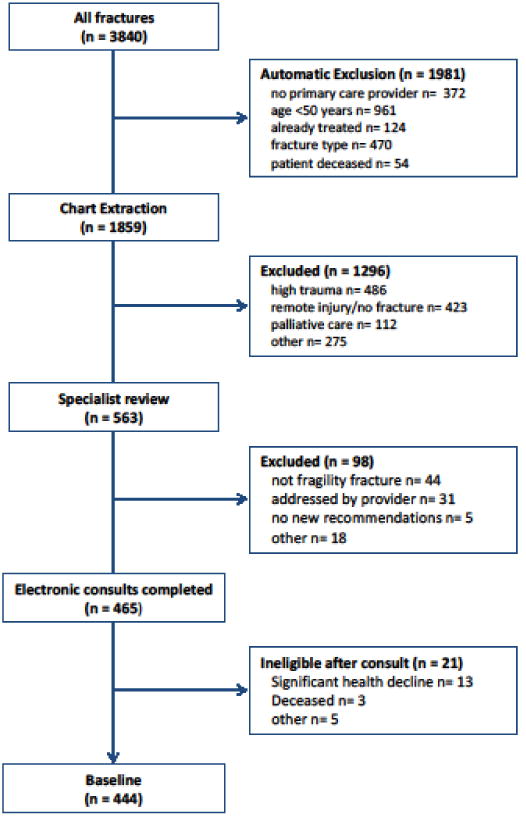
The E-consult service identified 465 eligible individuals with a low-trauma fracture who were not already on treatment between April 2011 and April 2013. However, 21 of these individuals were found to have become ineligible shortly after the specialist's consult, primarily due to a sudden decline in health, leaving 444 eligible individuals. Baseline patient characteristics are presented in Table 1. Veterans were predominantly male (92.8%) with a mean age of 69.1 years. Common medical comorbidities included diabetes mellitus and chronic lung disease. The most common fracture sites were of the lower leg (31.1%) and of the hip or pelvis (16.2%).
Table 1. Baseline Characteristics of Veterans with an E-consult.
| Demographic | Mean ± SD or Percentage | N |
|---|---|---|
| Age | 69.1 ± 11.3 | 444 |
| BMI | 27.9 ± 5.9 | 438 |
| Gender | ||
| Male | 92.8 | 412 |
| Female | 7.2 | 32 |
| Race | ||
| White | 71.2 | 316 |
| Black | 22.3 | 99 |
| Other | 1.6 | 6 |
| Unknown | 5.2 | 23 |
| Comorbidities | Percentage | N |
|---|---|---|
| Diabetes mellitus | 32.4 | 144 |
| Chronic lung disease | 23.2 | 103 |
| Neurologic condition | 22.3 | 99 |
| Alcohol abuse | 20.9 | 93 |
| Prostate Cancer | 9.7 | 43 |
| Rheumatoid arthritis | 1.6 | 7 |
| Corticosteroid use | 1.4 | 6 |
| Fracture site | Percentage | N |
|---|---|---|
| Vertebral | 14.0 | 62 |
| Hip/pelvis | 16.2 | 72 |
| Lower leg | 31.1 | 138 |
| Forearm/wrist | 15.3 | 68 |
| Shoulder | 7.9 | 35 |
| Rib | 15.5 | 69 |
Primary care providers' response
One hundred twenty nine (29.1%) consults recommended immediate bisphosphonate treatment and 258 (58.1%) recommended bone density assessments. The primary providers responded by prescribing bisphosphonates in 74 patients (57.4%). Eight patients refused therapy.
Bone density testing by dual-emission x-ray absorptiometry (DXA) was ordered in 183 (70.9%) patients. Fifty two DXA orders were not completed; the most common reason was that the patient canceled or did not show up for the appointment. Of the DXAs completed, 23% showed osteoporosis and 39% showed osteopenia. Following the DXA, 56% of patients were started on treatment, including calcium/vitamin D and/or anti-osteoporosis medication. Another 21 patients were referred to the Bone clinic for management and follow-up.
Facility-level treatment rates
Prior to implementation of the E-consult service, the rate of osteoporosis treatment between 3 to 6 months following ICD9 code for fracture at the intervention sites, among all patients with recent fractures, was 4.8% for bisphosphonates and 21.3% for calcium/vitamin D. After implementation of the program, the treatment rate increased to 7.3% for bisphosphonates (P = 0.02) and 35.2% for calcium/vitamin D (P < 0.01). Compared to the concurrent change among VAMCs without the E-consult service, the change in treatment rates for bisphosphonates (+2.5% vs. -1.8%, P = 0.02) and calcium/vitamin D (+13.9% vs. -1.2%, P < 0.01) was significantly different (Table 2).
Table 2.
Comparison of treatment rates for bisphosphonate and calcium/vitamin D between intervention and control facilities.
| Intervention Facilities | Control Facilities | ||||||
|---|---|---|---|---|---|---|---|
| All clinical fractures | |||||||
| Baseline | Follow-up | P | Baseline | Follow-up | P | P* | |
| N=900 | N=1062 | N=599 | N=520 | ||||
| Bisphosphonate | 43 (4.8%) | 78 (7.3%) | 0.02 | 37 (6.2%) | 23 (4.4%) | 0.23 | 0.02 |
| CA and/or Vit. D | 192 (21.3%) | 374 (35.2%) | <0.01 | 213 (35.6%) | 179 (34.4%) | 0.71 | <0.01 |
| Major osteoporotic fractures | |||||||
| Baseline | Follow-up | Baseline | Follow-up | ||||
| N=249 | N=309 | N=163 | N=162 | ||||
| Bisphosphonate | 19 (7.6%) | 35 (11.3%) | 0.15 | 14 (8.6%) | 11 (6.8%) | 0.68 | 0.18 |
| CA and/or Vit. D | 69 (27.7%) | 132 (42.7%) | <0.01 | 64 (39.3%) | 64 (39.5%) | 1.00 | 0.02 |
P compares treatment rates before and after implementation of the E-consult service within facilities group
P compares treatment rates between intervention and control facilities
Among patients who sustained a major osteoporotic fracture, defined as low-trauma fracture of the shoulder, wrist, hip, or spine, there was an increase in the treatment rate for bisphosphonates from 7.6% to 11.3% that was not statistically significant (P = 0.15). The treatment rate among Veterans age 50 to 69 years increased 2.7% and that among those over age 70 years increased 6.2%, though neither result reached statistical significance. However, there was a significant increase in calcium/vitamin D treatment. In comparison to facilities without the E-consult service, the change in treatment rates for bisphosphonates (+1.6 vs. - 2.3%) and calcium/vitamin D (+14.4 vs. +0.2%) among Veterans age 50 to 69 years was significantly improved in the intervention facilities (P = 0.03 and P < 0.01, respectively).
Discussion
In the current study, we have demonstrated that a centralized, regional E-consult service for patients with a recent low-trauma fracture who were not already treated for osteoporosis is feasible. The service is relatively low cost, employing a half-time program coordinator and a quarter-time metabolic bone physician to perform the screening, medical chart review, and osteoporosis E-consult note for 3 Medical Centers. In contrast to other secondary prevention programs, the current E-consult program serves predominantly male patients. More than half of the E-consult recommendations were acted on by primary care physicians and the service significantly improved osteoporosis management and treatment rates among patients with recent fracture at a facility level, both when evaluated before and after the service's implementation within participating facilities, and when compared to non-participating centers. Overall post-fracture treatment rates within the facilities with the E-consult service had a significant 2.5% increase in bisphosphonate prescription and 11.6% increase in vitamin D supplementation, while declines or no improvement were observed in control facilities. However, the magnitude of this figure is difficult to interpret because the sample likely includes a substantial number of Veterans for whom treatment is not needed or contraindicated. During the E-consult service period, over two-thirds of identified fractures were excluded by chart abstraction, most commonly because the fractures occurred during high trauma. Assuming a comparable proportion of Veterans at the facility level sample were also ineligible for treatment, the observed change in bisphosphonate treatment among eligible patients in the intervention facilities would be an increase from 14% to nearly 22%.
These treatment rates and subsequent improvement appear modest, and not improved over the prior OIG report. There are several reasons why the impact of the E-consult service may be limited. First, consults were initiated by the coding of a fracture-related diagnosis during a clinical encounter and not by the patient's primary care provider. However, the service relied on primary care providers to implement evaluation and treatment recommendations. Treatment recommendations were based on clear, guideline-driven indications, noted in the patient's medical record. However, among the E-consults that recommended initiation of bisphosphonates, less than 60% of providers subsequently ordered a prescription. While most providers expressed familiarity and satisfaction of the program, in a post-implementation survey, providers cited time constraints and following up on test results as barriers to implementing recommendations. There were no differences in implementation of recommendations based on fracture site. Second, there was no direct patient contact or education from the E-consult service, which may have further limited adherence to recommendations. Among those with recommended DXA, for example, approximately two-thirds were ordered, but many patients cancelled the appointment. Programs which do not rely on primary care providers for all ordering, or which include patient education, may address these issues. Also, as this program served predominantly male patients, educational components regarding male osteoporosis evaluation and treatment, directed at both patients and primary care providers, may improve acceptance and adherence to recommendations.
Several quality improvement interventions and care delivery models have been reported to improve osteoporosis treatment after a fracture. These interventions have varied widely from education initiatives for providers to coordinator-based, facilitated care of fracture patients. Overall, educational programs alone have had limited to no impact on testing and treatment rates.[12-15] Programs utilizing a care coordinator who is responsible for identifying and facilitating evaluation and treatment of all fracture patients within a hospital system appear to substantially improve osteoporosis care at modest cost.[16-18] Prior studies of the osteoporosis care-coordinator models have demonstrated that these interventions significantly improve osteoporosis screening and treatment rates and are also cost-effective, sometimes cost-saving, programs.[17,19,20]
However, these programs including a “Fracture Liaison Services” may be inefficient for small medical centers with lower fracture volume to provide. Moreover, osteoporosis testing and treatment decisions may be more complex in men or patients with multiple co-morbidities, requiring physician input. The Veterans Health Administration provides a unique opportunity to test improvements to the current management and treatment paradigm of osteoporosis. The current E-consult service, in response to the OIG report, was initiated as a proof-of-concept that the centralization of fracture coordinator services, with an opportunity for physician review when needed, is an effective strategy for healthcare systems where there are multiple centers with variable fracture volumes and complex patient characteristics.
The limitations of the E-consult service should be considered. The patient identification process depends on accurate and consistent coding by clinicians. Although fracture coding has been documented to be more than 90% accurate in a Medicare population,[21,22] it may be less so in the VA setting where fracture care may be obtained from non-VA providers, or for other chronic conditions important in managing osteoporosis. However, other clinical data that inform evaluation and treatment recommendations for osteoporosis are readily available from the VA electronic medical record, including laboratory results and medication prescriptions. In the current service, implementation of E-consult recommendations was deferred to the primary care provider's discretion. Although all patients were identified as a consequence of a low trauma fracture, because of the remote consultation without direct interactions with the patient, recommendations for treatment were made conservatively and based on well-documented indications within the patient's medical record. Thus, the number of treatment recommendations likely reflects a lower rate than would be clinically indicated if the patient was evaluated in person. Nevertheless, we were able to demonstrate a significant, though modest, increase in the treatment rate. Further improvement in the treatment rate would likely require a program similar to the current E-consult service to identify and evaluate patients, coordinated with services to engage both primary care providers and patients.
Acknowledgments
This project was funded by the VISN 6 Specialty Care Office. We are grateful for the assistance of Dr. Kim Voss, Dr. Parag Dalsania, Dr. Peter Chung, and Ms. Katherine McMullin.
Drs. Lee, Lyles, and Colon-Emeric acknowledge support from the Duke Claude A. Pepper Center (NIA 2P30AG028716-08).
Footnotes
Conflict of Interest Disclosures: Richard H. Lee: No disclosures or conflicts
- Research Support: Novartis, Amgen, Kirin Pharmaceuticals
- Consultant: Novartis, Amgen, UCB
- Cofounder and Equity Owner: BisCardia, Inc; Faculty Connection, LLC
- Co-Inventor of US Patent Application: “Methods for preventing or reducing secondary fractures after hip fracture” Number 20050272707
- Inventor of US Patent Application: “Medication Kits and Formulations for Preventing, Treating or Reducing Secondary Fractures After Previous Fracture” Number 12532285
- Co-Inventor of US Patent Application: “Bisphosphonate Compositions and Methods for Treating Heart Failure” Number 20104717
- Co-Inventor of US Patent Application: “Bisphophonate Compositions and Methods for Treating and/or Reducing Cardiac Dysfunction” Number 61/560,328
Megan Pearson: No disclosures or conflicts
Karen Barnard: No disclosures or conflicts
- consultant to Novartis and Amgen
- Equity owner Biscardia Inc
- Inventor of 2 use patents related to bisphosphonates and cardiovascular disease
Some results from this study were presented at the American Society of Bone and Mineral Research 2013 annual meeting in Baltimore, MD.
References
- 1.Colon-Emeric C, Kuchibhatla M, Pieper C, Hawkes W, Fredman L, Magaziner J, Zimmerman S, Lyles KW. The contribution of hip fracture to risk of subsequent fractures: data from two longitudinal studies. Osteoporos Int. 2003;14:879–883. doi: 10.1007/s00198-003-1460-x. [DOI] [PubMed] [Google Scholar]
- 2.Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA, 3rd, Berger M. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. 2000;15:721–739. doi: 10.1359/jbmr.2000.15.4.721. [DOI] [PubMed] [Google Scholar]
- 3.Beaupre LA, Morrish DW, Hanley DA, Maksymowych WP, Bell NR, Juby AG, Majumdar SR. Oral bisphosphonates are associated with reduced mortality after hip fracture. Osteoporos Int. 2011;22:983–991. doi: 10.1007/s00198-010-1411-2. [DOI] [PubMed] [Google Scholar]
- 4.Lyles KW, Colon-Emeric CS, Magaziner JS, Adachi JD, Pieper CF, Mautalen C, Hyldstrup L, Recknor C, Nordsletten L, Moore KA, Lavecchia C, Zhang J, Mesenbrink P, Hodgson PK, Abrams K, Orloff JJ, Horowitz Z, Eriksen EF, Boonen S. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 2007;357:1799–1809. doi: 10.1056/NEJMoa074941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Feldstein AC, Nichols G, Orwoll E, Elmer PJ, Smith DH, Herson M, Aickin M. The near absence of osteoporosis treatment in older men with fractures. Osteoporos Int. 2005;16:953–962. doi: 10.1007/s00198-005-1950-0. [DOI] [PubMed] [Google Scholar]
- 6.Fraser LA, Ioannidis G, Adachi JD, Pickard L, Kaiser SM, Prior J, Brown JP, Hanley DA, Olszynski WP, Anastassiades T, Jamal S, Josse R, Goltzman D, Papaioannou A. Fragility fractures and the osteoporosis care gap in women: the Canadian Multicentre Osteoporosis Study. Osteoporos Int. 2011;22:789–796. doi: 10.1007/s00198-010-1359-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ganda K, Puech M, Chen JS, Speerin R, Bleasel J, Center JR, Eisman JA, March L, Seibel MJ. Models of care for the secondary prevention of osteoporotic fractures: a systematic review and meta-analysis. Osteoporos Int. 2013;24:393–406. doi: 10.1007/s00198-012-2090-y. [DOI] [PubMed] [Google Scholar]
- 8.Giangregorio L, Papaioannou A, Cranney A, Zytaruk N, Adachi JD. Fragility fractures and the osteoporosis care gap: an international phenomenon. Semin Arthritis Rheum. 2006;35:293–305. doi: 10.1016/j.semarthrit.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 9.Report of the Office of the Inspector General. Washington, DC: 2010. Management of Osteoporosis in Veterans with Fractures. [Google Scholar]
- 10.Colon-Emeric C, Lee R, Barnard K, Pearson M, Lyles KW. Use of regional clinical data to identify veterans for a multi-center osteoporosis electronic consult quality improvement intervention. J Hosp Adm. 2013;2:8–14. [Google Scholar]
- 11.Clinician's Guide to Prevention and Treatment of Osteoporosis. National Osteoporosis Foundation; Washington DC: 2010. [Google Scholar]
- 12.Bliuc D, Eisman JA, Center JR. A randomized study of two different information-based interventions on the management of osteoporosis in minimal and moderate trauma fractures. Osteoporos Int. 2006;17:1309–1317. doi: 10.1007/s00198-006-0078-1. [DOI] [PubMed] [Google Scholar]
- 13.Cranney A, Lam M, Ruhland L, Brison R, Godwin M, Harrison MM, Harrison MB, Anastassiades T, Grimshaw JM, Graham ID. A multifaceted intervention to improve treatment of osteoporosis in postmenopausal women with wrist fractures: a cluster randomized trial. Osteoporos Int. 2008;19:1733–1740. doi: 10.1007/s00198-008-0669-0. [DOI] [PubMed] [Google Scholar]
- 14.Cuddihy MT, Amadio PC, Gabriel SE, Pankratz VS, Kurland RL, Melton LJ., 3rd A prospective clinical practice intervention to improve osteoporosis management following distal forearm fracture. Osteoporos Int. 2004;15:695–700. doi: 10.1007/s00198-004-1597-2. [DOI] [PubMed] [Google Scholar]
- 15.Hawker G, Ridout R, Ricupero M, Jaglal S, Bogoch E. The impact of a simple fracture clinic intervention in improving the diagnosis and treatment of osteoporosis in fragility fracture patients. Osteoporos Int. 2003;14:171–178. doi: 10.1007/s00198-003-1377-4. [DOI] [PubMed] [Google Scholar]
- 16.Che M, Ettinger B, Liang J, Pressman AR, Johnston J. Outcomes of a disease-management program for patients with recent osteoporotic fracture. Osteoporos Int. 2006;17:847–854. doi: 10.1007/s00198-005-0057-y. [DOI] [PubMed] [Google Scholar]
- 17.Dell RM, Greene D, Anderson D, Williams K. Osteoporosis disease management: What every orthopaedic surgeon should know. J Bone Joint Surg Am. 2009;91(S6):79–86. doi: 10.2106/jbjs.i.00521. [DOI] [PubMed] [Google Scholar]
- 18.Majumdar SR, Beaupre LA, Harley CH, Hanley DA, Lier DA, Juby AG, Maksymowych WP, Cinats JG, Bell NR, Morrish DW. Use of a case manager to improve osteoporosis treatment after hip fracture: results of a randomized controlled trial. Arch Intern Med. 2007;167:2110–2115. doi: 10.1001/archinte.167.19.2110. [DOI] [PubMed] [Google Scholar]
- 19.Sander B, Elliot-Gibson V, Beaton DE, Bogoch ER, Maetzel A. A coordinator program in post-fracture osteoporosis management improves outcomes and saves costs. J Bone Joint Surg Am. 2008;90:1197–1205. doi: 10.2106/jbjs.g.00980. [DOI] [PubMed] [Google Scholar]
- 20.Cooper MS, Palmer AJ, Seibel MJ. Cost-effectiveness of the Concord Minimal Trauma Fracture Liaison service, a prospective, controlled fracture prevention study. Osteoporos Int. 2012;23:97–107. doi: 10.1007/s00198-011-1802-z. [DOI] [PubMed] [Google Scholar]
- 21.Ray WA, Griffin MR, Fought RL, Adams ML. Identification of fractures from computerized Medicare files. J Clin Epidemiol. 1992;45:703–714. doi: 10.1016/0895-4356(92)90047-q. [DOI] [PubMed] [Google Scholar]
- 22.Rigler SK, Ellerbeck E, Whittle J, Mahnken J, Cook-Wiens G, Shireman TI. Comparing methods to identify hip fracture in a nursing home population using Medicare claims. Osteoporos Int. 2011;22:57–61. doi: 10.1007/s00198-010-1264-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


