Abstract
Objective
To examine professional medical interpreters’ perspectives of in-person and remote interpreting modalities.
Methods
Survey of interpreters at three medical centers assessing satisfaction with aspects of communication using each modality, and adequacy of videoconferencing medical interpretation (VMI) and telephonic interpretation for 21 common clinical scenarios in the hospital and ambulatory care settings.
Results
52 interpreters completed the survey (73% response). All modalities were equally satisfactory for conveying information. Respondents favored in-person to telephonic interpretation for establishing rapport (95% versus 71%, p = .002) and for facilitating clinician understanding of patients’ social and cultural backgrounds (92% versus 69%, p = .002). Scenarios with substantial educational or psychosocial dimensions had no more than 70% of respondents rating telephonic interpretation as adequate (25–70%); for all of these scenarios, VMI represented an improvement (52–87%).
Conclusion
From the interpreter perspective, telephonic interpretation is satisfactory for information exchange, but less so for interpersonal aspects of communication. In scenarios where telephonic interpretation does not suffice, particularly those with substantial educational or psychosocial components, VMI offers improved communication.
Practice implications
Differences in interpreters’ perspectives of modalities based on communication needs and clinical scenario suggest mixed use of multiple modalities may be the best language access strategy.
Keywords: Language access, Medical interpretation, Remote interpretation, Videoconferencing medical interpretation, Interpreter perspective
1. Introduction
The growing number of United States residents with limited English proficiency (LEP) mandates close attention to language issues in health care. About 55 million people living in the U.S. speak a language other than English at home, and about 8.6% speak English less than “very well”; this number has been steadily climbing [1,2]. Patients with LEP have difficulty accessing health care [3,4] and face decreased quality of care in domains including satisfaction, health outcomes, and safety [5–13].
Professional medical interpretation improves access and quality of care for LEP patients [5,14–16]. Despite a national mandate for access to interpreter services in settings receiving federal funds [17], under-use of interpreters persists [18–25]. While in-person medical interpretation by trained interpreters is considered the gold standard when patient–clinician language concordance is not possible, numerous factors limit use in clinical settings including interpreter staffing and schedules, language requirements, and wait times [20,22,23,26]. Remote methods including telephonic interpretation and videoconferencing medical interpretation (VMI), which allows for two-way audio–visual communication using a mobile unit, are increasingly used to increase access where in-person interpretation is unavailable and/ or where demand is high [23,26]. Use of remote modalities leads to increased patient and clinician satisfaction compared to ad hoc or no interpretation [27–29].
Effective communication in clinical encounters depends on exchange of accurate information between clinician and patient and on interpersonal skills that foster understanding of patients’ social or cultural backgrounds and development of patient–clinician rapport. Brennan and Lockridge [37] offer a “grounding framework” in which to discuss the effect of media on communication, emphasizing the process of grounding so that the participants understand one another. In interpreter-mediated clinical encounters, the grounding framework becomes a multilateral process among clinician, patient, and interpreter. All three modalities we examined afford audibility (one participant can hear the other); cotemporality (messages are received without delay); simultaneity (participants can send and receive messages at the same time); and sequentiality (participants take turns in an orderly conversation). A face-to-face encounter affords a physical co-presence, whereas videoconferencing affords visibility, but in a more limited manner.
These factors may be more or less important depending on whether a clinical conversation is more of a simple exchange of information, educational in nature, or emotionally laden due to the content or individual status. Optimal implementation of remote interpretation modalities in resource-constrained health care environments necessitates better understanding of their advantages and limitations for these different aspects of communication in different clinical contexts. Few existing studies compare remote modalities for medical interpretation; those that do focus on outpatient clinical settings [29–32]. Our group investigated clinician perspectives of in-person and VMI interpretation in an ambulatory setting [29], finding similar quality of interpretation for in-person and VMI, although self-assessed cultural competence was greater with in-person interpretation.
In this study we focus on the interpreter perspective. Interpreters are uniquely positioned to address relative merits of in-person and remote modalities over a range of clinical scenarios, given their broad interpreting experience; while one patient or clinician’s experience may be limited to a few specific kinds of clinical interactions, a professional medical interpreter typically has experience in a wide variety of clinical encounters. In their dual roles as participants and observers, medical interpreters have important insights into the quality of clinical interactions. As insiders to the medical system, interpreters may also be more willing than patients to be openly critical of modalities that do not work well.
Few studies have examined interpreter perspectives of VMI and other remote modalities of interpretation. A 2003 qualitative study that included 4 interpreters conducted structured interviews with interpreters, clinicians, and patients about their specialty clinic experience with four interpretation modalities (in-person, speakerphone, VMI, and remote simultaneous telephonic interpretation), finding that interpreters preferred VMI to the other remote methods [31]. Another study investigated interpreter, clinician, and patient perspectives of in-person, telephonic, and VMI interpretation in the pediatric and postpartum clinic setting, and included quantitative and time data as well as a larger number of interpreters (7) than the prior study [32]; while clinicians and interpreters rated in-person interpretation more highly, patient ratings showed no difference between the three methods. Clinicians and interpreters demonstrated a preference for VMI over telephonic interpretation.
To our knowledge, no prior studies examine remote modalities of interpretation in multiple clinical scenarios. This study complements existing literature by describing interpreter perspectives on in-person and remote modalities for specific aspects of communication, and in a range of clinical scenarios from three different medical centers. We address the following questions: (1) how satisfied are professional interpreters with specific aspects of communication using in-person interpretation, telephonic interpretation, and VMI; (2) how well do telephonic interpretation and VMI facilitate communication for each of 21 common clinical scenarios; and (3) for scenarios in which telephone interpretation does not adequately facilitate communication, does VMI represent a significant improvement?
2. Methods
2.1. Study design and setting
We conducted a cross-sectional survey of professional medical interpreters at two public hospitals and one university medical center in the San Francisco Bay Area. Overall LEP prevalence at the sites ranges from 15 to 46%. The two most common non-English languages spoken by patients at all three of the hospitals are Chinese and Spanish. The third most common varied between Russian and Vietnamese. Each of the three medical centers has staff interpreter services, and uses the three modalities of in-person, telephonic, and VMI with the clinician and patient physically present in the same room. With in-person professional medical interpretation, a trained interpreter is physically present at the encounter. With telephonic interpretation, the interpreter is available on a dual-headset telephone or a single-headset telephone with a speaker, or passed back and forth between patient and clinician. VMI uses a mobile unit with a camera and a video monitor that can be moved from room to room for patient encounters. The degree of implementation and specific context of utilization of the different modalities of interpretation, and individual interpreters’ experiences with each modality, vary across the sites.
2.2. Participants
All 71 professional interpreters at the three sites were asked to complete the survey. Participants were notified of the electronic version of the survey via e-mail with a secure web link, and paper surveys were distributed to mailboxes of those who did not access the electronic version. Initial non-responders received a second request, and there was a drawing for a gift incentive for all respondents who chose to enter. The Institutional Review Board at the University of California at San Francisco approved recruitment procedures and the survey.
2.3. Survey content
The interpreter survey was developed by study investigators based on prior studies of interpreter use and effectiveness in clinical settings [29,33]. The interpreter services manager at each site provided iterative input regarding content and clarity during survey development, and did not participate in the survey. The survey took 10–20 min to complete, and included interpreters’ age, race, ethnicity, birthplace, languages in which they interpret, education, interpreter training, and level of experience in medical interpreting.
To assess satisfaction with specific aspects of communication for each modality (in-person, telephonic, and VMI), respondents were asked to recall a recent encounter using that modality and to rate, on a 5-point Likert scale, their satisfaction with five specific aspects of patient–clinician communication: “How satisfied were you with your ability to communicate what the patient had to say?/Communicate what the clinician had to say?/Establish rapport between the clinician and the patient?/Facilitate the clinician’s understanding about the patient’s social or cultural background?” and “Overall, how satisfied were you with the quality of the communication during this encounter?” Responses were “extremely satisfied”; “satisfied”; “neither satisfied nor dissatisfied”; “dissatisfied”; and “very dissatisfied”. In analysis, we dichotomized responses as satisfied (extremely satisfied/satisfied) versus less than satisfied.
For each remote interpreting modality participants were asked to rate, on a 5-point Likert scale (“very well”; “well”; “adequate”; “not well”; “poorly”; “don’t know”) the modality’s ability to facilitate communication for each of twenty-one common clinical scenarios. The list of scenarios was developed using author expertise and input from interpreter services managers at each site. Scenarios represented the range of common clinical encounters with respect to location (inpatient versus outpatient), acuity of illness, and information exchanged. They included new evaluations and acute care (nurse triage in the emergency department (ED); ED physician evaluation; new outpatient visit; urgent care visit; inpatient physician history and physical); follow-up/routine care (follow-up outpatient visit, pre-operative exam, routine daily hospital assessment, consent for minor procedure; inpatient nursing assessment, and outpatient nursing assessment); educational or psychosocial encounters (family meeting; consent for a complex procedure; inpatient nursing teaching; hospital discharge instructions; physical or occupational therapy; and case management/social work); and ancillary or administrative scenarios (patient checking in with a clerk; routine blood draw; radiology; financial services interview). In analysis, responses were dichotomized as adequate (very well/well/ adequate) versus inadequate (not well/poorly). “Don’t know” responses were counted as missing.
2.4. Statistical analysis
Data analysis was performed using SAS software, version 9.2. Descriptive statistics were used to illustrate demographics, training, and experience. Logistic regression models were used to examine interpreters’ satisfaction with each modality of interpretation for each of the five aspects of communication. Since individual respondents were asked the same questions for all three modalities, generalized estimating equations clustered on respondent were used to account for correlation within interpreters. We also adjusted for clinical site. Unadjusted percentages of satisfaction with each modality were reported, with tests for significance based on adjusted models. For aspects of communication where overall significant differences were found between modalities, we performed pair-wise comparisons between the modalities with in-person interpretation as the referent.
To determine adequacy of telephonic interpretation and VMI for facilitating communication in specific clinical scenarios, we calculated the proportion of respondents answering that each modality was at least adequate (“adequate”, “well”, or “very well”) for each scenario. We divided the 21 scenarios into tertiles based on these proportions. To focus on the scenarios most problematic for telephonic interpretation and determine whether VMI represents a way to improve communication during these scenarios, we used logistic regression to model the odds of reporting VMI as at least adequate compared to telephonic interpretation, for each scenario in the lowest tertile. Generalized estimating equations were used to cluster responses within interpreters. Our models also controlled for clinical site and number of years of interpreting experience. Because three scenarios at the upper bound of this tertile had equal proportions of interpreters rating telephonic interpretation as at least adequate, we included all of them in this analysis (8 scenarios total).
3. Results
3.1. Participant characteristics
Of the 71 professional medical interpreters at the three participating hospitals, 52 (73%) completed the survey (Table 1). Their average age was 50 years (SD = 9), and most (86%) were born outside the U.S. A majority were college graduates (65%), almost all (90%) had received formal training in medical interpretation, and 72% of those had been through a certification program. Twenty-two languages were represented, with the most common being Spanish and Chinese. All interpreters had experience with telephonic interpretation; most had experience with VMI.
Table 1.
Demographic profile of 52 interpreters responding to the survey at three San Francisco Bay Area Hospitals, 2008.
| N = 52 (%) | |
|---|---|
| Demographics | |
| Age (mean, median) | 50, 50 |
| Women | 34 (65) |
| Born outside the U.S. | 44 (86) |
| Training and experience | |
| Interpreting as primary job | 49 (94) |
| Years of interpreting experience (mean, SD) | 10 (8) |
| Education | |
| Some high school | 1 (2) |
| High school diploma | 2 (4) |
| Some college | 12 (23) |
| College graduate | 22 (42) |
| Some postgraduate training | 12 (23) |
| Vocational/technical school | 3 (6) |
| Formal training in interpretation | 47 (90) |
| Formal classroom training | 27 (57) |
| Certificate program | 34 (72) |
| Language used for interpreting (most common)a | |
| Spanish | 22 (42) |
| Cantonese | 21 (40) |
| Mandarin | 19 (36) |
| Vietnamese | 10 (19) |
| Russian | 6 (12) |
| Number of encounters per week (N = 48) | |
| Fewer than 10 | 2 (4) |
| 10–49 | 18 (38) |
| 50–99 | 19 (40) |
| 100 or over | 9 (19) |
| Experience with remote modalities | |
| Telephonic interpretation | |
| Ever used | 52 (100) |
| At least half of the time | 27 (52) |
| Some of the time or rarely | 25 (48) |
| VMI | |
| Ever used | 45 (87) |
| At least half of the time | 30 (67) |
| Some of the time or rarely | 15 (33) |
Not mutually exclusive.
3.2. Interpreter satisfaction in facilitating specific aspects of communication
A large majority of interpreters reported satisfaction with each modality for communicating what the patient said and what the clinician said (Fig. 1). However, significantly fewer were satisfied with their ability to establish rapport or facilitate clinician understanding about the patient’s cultural or social background via telephonic interpretation compared to in-person. Likewise, significantly fewer respondents reported satisfaction with the overall quality of telephonic compared to in-person interpretation. Fewer respondents reported satisfaction with VMI compared to in-person interpretation for each of these three aspects of communication, though this difference reached statistical significance only for establishing rapport between patient and clinician.
Fig. 1.
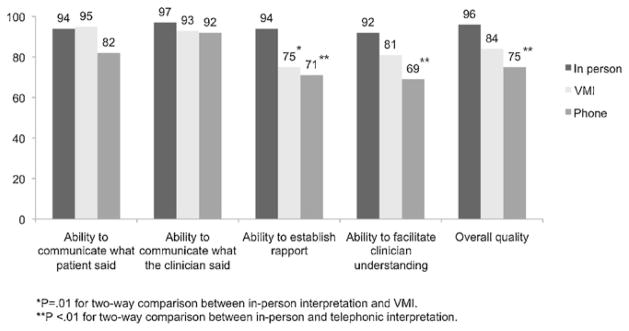
Percent of 52 interpreters “satisfied” or “extremely satisfied” with each modality for five aspects of patient–clinician communication, San Francisco Bay Area, 2008.
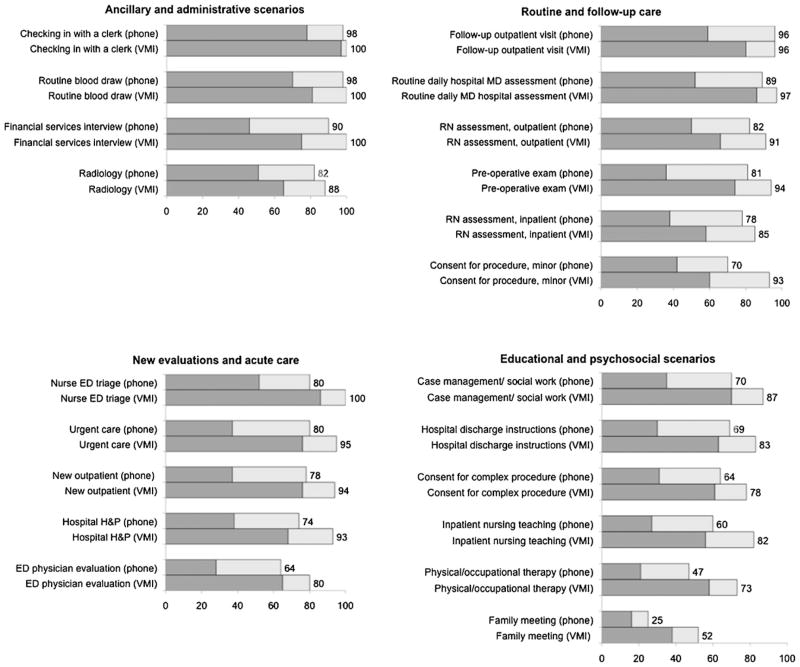
3.3. Adequacy of telephonic and VMI interpretation for clinical scenarios
The number of respondents for telephonic interpretation for each scenario ranged from 39 to 51, and the proportion rating telephonic interpretation as adequate or better ranged from 26% for family meetings to 98% for routine blood draw or checking in with a clerk (Fig. 2). The upper tertile of clinical scenarios for telephonic interpretation (those for which the most respondents felt telephonic interpretation facilitated communication adequately) included all ancillary and administrative scenarios (checking in with a clerk 98%; routine blood draw 98%; financial services interview 90%; radiology 82%) and three follow-up/routine care scenarios (follow up outpatient visit 96%; routine daily hospital physician evaluation 89%; outpatient nursing assessment 82%).
Fig. 2.
Percent of 52 interpreters stating that telephonic interpretation and VMI work “well/very well” (dark gray bar) or “adequately” (light gray bar) for each clinical scenario, San Francisco Bay Area, 2008.
The middle tertile included four new/acute care scenarios (urgent care visit 80%; nurse triage in the ED 80%; new outpatient visit 78%; hospital history and physical 74%) and two follow-up/ routine scenarios (pre-operative exam 81%; RN inpatient assessment 77%).
The lowest tertile of scenarios for telephonic interpretation included all six educational/psychosocial scenarios (hospital discharge instructions 70%; case management/social work 70%; consent for complex procedure 65%; inpatient nursing teaching 60%; physical/occupational therapy 47%; family meeting 26%), one follow-up/routine care scenario of consent for minor procedure (70%), and one new evaluation/acute care scenario of ED physician evaluation (64%).
For VMI, the number of respondents for each scenario ranged from 20 to 44, and the proportion of interpreters rating VMI as facilitating communication adequately or better ranged from 52% (family meeting) to 100% (patient checking in, ED nurse triage, routine blood draw, and financial services interview). The scenarios for which the most interpreters did not feel VMI adequately facilitated communication were family meeting (48%) and physical therapy/occupational therapy (27%).
Although most respondents found both telephonic and VMI interpretation to be adequate or better for many clinical scenarios, the distribution of those responding that the modality worked well/very well as compared to those responding that it adequately facilitated communication differed between modalities. Across all clinical scenarios, the proportion of “well/very well” versus “adequate” responses was higher for VMI than for telephonic interpretation.
3.4. VMI in scenarios where telephonic interpretation was inadequate
For each of the eight scenarios in the lowest tertile for adequacy of telephonic interpretation, we explored whether VMI was an improvement by modeling odds of reporting VMI to be adequate or better (Table 2). Respondents had significantly higher odds of reporting VMI as facilitating communication adequately for all of these scenarios except for two – complex consent for procedure and physician evaluation in the ED – which did not reach statistical significance.
Table 2.
Odds ratios for interpreters’ reporting VMI to be adequate or better for facilitating communication in scenarios compared to telephonic interpretation, San Francisco Bay Area, 2008.
| Scenario | Respondents reporting telephonic interpretation adequate or better (%)a | Respondents reporting VMI adequate or better (%)b | Odds ratio (95% CI) for reporting VMI adequate or better (referent telephonic)c |
|---|---|---|---|
| Family meeting | 26 | 52 | 3.4 (1.5–7.7) |
| Physical/occupational therapy | 47 | 73 | 4.4 (1.6–12.1) |
| Inpatient nursing teaching | 60 | 82 | 3.0 (1.2–7.9) |
| Physician evaluation in ED | 64 | 80 | 1.4 (0.8–2.5) |
| Consent for procedure (complex) | 65 | 78 | 1.7 (0.9–3.3) |
| Consent for procedure (minor) | 70 | 93 | 5.0 (1.6–15.8) |
| Hospital discharge instructions | 70 | 83 | 3.2 (1.1–9.2) |
| Case management/social work | 70 | 87 | 2.5 (1.2–5.4) |
N = 39–51 respondents for adequacy of telephonic interpretation.
N = 20–44 respondents for adequacy of VMI.
Models clustered on interpreter; adjusted for site and years of interpreting experience.
4. Discussion and conclusion
4.1. Discussion
In this study we report on a survey of professional interpreter perspectives on in-person and remote interpretation for different types of communication and in different clinical contexts. Our results suggest that from the interpreter perspective, remote modalities function as well as in-person interpreting for straightforward information exchange. For more nuanced aspects of communication such as establishing rapport between patient and clinician and understanding of patients’ socio-cultural backgrounds, in-person interpretation may be more effective. Our group’s study of physicians’ perspective on interpreter-mediated encounters in an ambulatory care setting has similarly found that in-person interpretation more effectively facilitates cultural and social dimensions of communication compared to VMI [29].
Most interpreters find telephonic interpretation adequate for administrative, ancillary, and follow-up care clinical scenarios. For other scenarios with substantial educational or psychosocial components, telephonic interpretation may not suffice, and video-conferencing offers improved communication. These scenarios include physical/occupational therapy and family meetings, which were rated least adequate for telephonic interpretation and have high emotional or educational content. However, even VMI was considered inadequate by 48% of interpreters for family meeting and by 27% for physical/occupational therapy, suggesting that, from the interpreter perspective, efforts should still be made to use in-person professional interpreters for these situations when possible.
The similarities in communication tools outlined by Brennan and Lockridge [37] among the modalities may explain why interpreters view telephonic interpretation as working well for many clinical scenarios, and in particular for those requiring only exchange of information. In these scenarios, audibility, cotemporality, simultaneity and sequentiality are all in play. However, the key differences among the modalities may explain our findings that interpreters view telephonic interpretation as inadequate for clinical scenarios requiring extensive education or an interaction involving significant emotional content. For example, in scenarios with substantial educational components such as working with a physical or occupational therapist, or a nurse teaching about glucometer use, grounding or multilateral understanding may depend on use of gestures or physical movement. In these situations, an interpreter’s effectiveness may be decreased if she/he is unable to visually interact with the clinician and patient. Similarly, scenarios with substantial emotional components such as prognosis or end-of-life discussions may include more non-verbal communication (e.g. facial expressions and gestures), increasing the value of visibility for these interactions.
Interpreters’ perspectives on the effectiveness of modalities may not always align with those of patients and clinicians, and interpreters may be more critical of remote modalities than other stakeholders. A study in the postpartum and pediatric clinic setting examined patient, clinician, and interpreter assessments of clinical encounters using in-person, telephonic, and video-conferencing interpretation. While patients rated all modalities highly, interpreters and clinicians gave higher ratings to in-person than to remote modalities, with a trend favoring video over telephonic interpretation [32]. Another recent study in the pediatric emergency department assessed patient satisfaction after an ED visit using telephonic interpretation, in-person interpretation, or a bilingual clinician [34]. Patient satisfaction with language services was high for all groups and did not differ significantly for those who received telephonic versus in-person professional interpretation. This differs from our finding that in the setting of a visit with an ED physician, 36% of interpreters felt that telephonic interpretation was inadequate. The differences between interpreters’ and other stakeholders’ assessments may reflect interpreter insights into the clinical encounters as well as interpreter preferences in terms of ease of use and other workday considerations. As interpreter assessments of modalities vary substantially depending on the clinical encounter, the degree of concordance between interpreter, patient, and clinician assessments of interpreting modalities may vary across clinical scenarios as well.
This study had several limitations. Our survey addressed perspectives of interpreters only. However, this is the first study addressing modalities of medical interpretation in a range of clinical scenarios. What we lose in richness of detail from obtaining multiple perspectives we gain in breadth of clinical experience that would not be feasible to address from all perspectives in one study. We focused on three medical centers in a limited geographic region, although these three sites represent institutions with considerable diversity of patients. Interpreters at these medical centers had a range of experience with each modality and their individual responses may reflect that experience. However, at all three of the medical centers, the staff interpreters included in our study use all three modalities on a daily basis and thus their responses likely reflect real-world clinical experience. Our study does not encompass the full range of potential of interpretation utilization, including use of third-party vendors for telephonic interpretation and remote simultaneous medical interpreting (“United Nations-style” interpretation via headset or telephone with near-simultaneous voice-over). While patients and clinicians may prefer certain aspects of remote simultaneous interpreting to consecutive telephonic and even in-person interpretation [35,36], remote simultaneous interpreting requires additional expertise on the part of the interpreter and thus is not as widely available. Although this survey addresses a large number of common clinical scenarios, there may be differences even within these scenarios that can affect the success of a given interpretation modality. A “routine outpatient visit” for a young and relatively healthy person differs substantially from a visit for a patient with multiple chronic active medical problems, social challenges, mental illness, or any combination of the above.
4.2. Conclusion
This is the first study evaluating modalities of interpretation in different clinical scenarios. Our study adds depth to the existing literature by highlighting interpreters’ evaluation of in-person, telephonic, and VMI interpretation to facilitate patient–clinician communication, with regard to specific communication needs and in different types of clinical encounters. Interpreters view telephonic interpretation as satisfactory for information exchange, but less satisfactory for interpersonal aspects of communication. VMI represents an improvement for communication taking place in clinical scenarios with substantial educational/psychosocial components, where telephonic interpretation is often inadequate.
4.3. Practice implications
This survey has implications for implementation of language access measures. Our results suggest that, from the medical interpreter perspective, mixed use of multiple modalities is the most effective language access strategy. Resources should be directed towards implementation of telephonic interpretation where it works well, particularly in administrative, ancillary, and non-complex follow-up clinical scenarios. For scenarios where in-person interpretation is unavailable and telephonic interpretation may be inadequate, VMI represents an improvement from the interpreter perspective. However, it may still have limitations; thus, wherever feasible, in-person professional interpreters should be directed toward those clinical encounters with substantial educational or psychosocial components.
Acknowledgments
This study was supported by grant no. 20061003 from The California Endowment and by grant no. P30-AG15272 of the Resource Centers for Minority Aging Research program funded by the National Institute on Aging, National Institutes of Health, and the National Research Service Award grant no. T32HP19025. We would like to thank Gloria Garcia-Orme and Tatyana Latushkin for their input on the survey design as well as all of the professional interpreters who participated.
Footnotes
Conflict of interest
None.
These data have been presented as oral presentations at the 2010 Annual Meeting of the Society of General Internal Medicine and at the annual Health Disparities Research Symposium at the University of California, San Francisco.
Contributor Information
Erika Leemann Price, Email: erika.price@ucsf.edu.
Eliseo J. Pérez-Stable, Email: eliseops@medicine.ucsf.edu.
Dana Nickleach, Email: dana.nickleach@ucsf.edu.
Monica López, Email: mlopez@medicine.ucsf.edu.
Leah S. Karliner, Email: leah.karliner@ucsf.edu.
References
- 1.2006–008 American Community Survey 3-Year Estimates. U.S. Census Bureau; 2008. [Accessed September 3, 2010]. 2010, at http://factfinder.census.gov/servlet/STTable?_bm=y&-geo_id=01000US&-qr_name=ACS_2008_3YR_G00_S1603&-ds_name=ACS_2008_3YR_G00_. [Google Scholar]
- 2.Shin H, Bruno R. Language Use and English-Speaking Ability: 2000. U.S. Census Bureau; 2003. Oct, [Google Scholar]
- 3.Fiscella K, Shin P. The inverse care law: implications for healthcare of vulnerable populations. J Ambul Care Manage. 2005;28:304–12. doi: 10.1097/00004479-200510000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Cheng EM, Chen A, Cunningham W. Primary language and receipt of recommended health care among Hispanics in the United States. J Gen Intern Med. 2007;22:283–8. doi: 10.1007/s11606-007-0346-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moreno G, Morales LS. Hablamos juntos (together we speak): interpreters, provider communication, and satisfaction with care. J Gen Intern Med. 2010 doi: 10.1007/s11606-010-1467-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gany F, Kapelusznik L, Prakash K, Gonzalez J, Orta LY, Tseng CH, et al. The impact of medical interpretation method on time and errors. J Gen Intern Med. 2007;22:319–23. doi: 10.1007/s11606-007-0361-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gandhi TK, Weingart SN, Borus J, Seger AC, Peterson J, Burdick E, et al. Adverse drug events in ambulatory care. N Engl J Med. 2003;348:1556–64. doi: 10.1056/NEJMsa020703. [DOI] [PubMed] [Google Scholar]
- 8.Cohen AL, Rivara F, Marcuse EK, McPhillips H, Davis R. Are language barriers associated with serious medical events in hospitalized pediatric patients? Pediatrics. 2005;116:575–9. doi: 10.1542/peds.2005-0521. [DOI] [PubMed] [Google Scholar]
- 9.Divi C, Koss RG, Schmaltz SP, Loeb JM. Language proficiency and adverse events in US hospitals: a pilot study. Int J Qual Health Care. 2007;19:60–7. doi: 10.1093/intqhc/mzl069. [DOI] [PubMed] [Google Scholar]
- 10.Flores G, Laws MB, Mayo SJ, Zuckerman B, Abreu M, Medina L, et al. Errors in medical interpretation and their potential clinical consequences in pediatric encounters. Pediatrics. 2003;111:6–14. doi: 10.1542/peds.111.1.6. [DOI] [PubMed] [Google Scholar]
- 11.Todd KH, Samaroo N, Hoffman JR. Ethnicity as a risk factor for inadequate emergency department analgesia. J Am Med Assoc. 1993;269:1537–9. [PubMed] [Google Scholar]
- 12.Pérez-Stable EJ, Napoles-Springer A, Miramontes JM. The effects of ethnicity and language on medical outcomes of patients with hypertension or diabetes. Med Care. 1997;35:1212–9. doi: 10.1097/00005650-199712000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Wilson E, Chen AH, Grumbach K, Wang F, Fernández A. Effects of limited English proficiency and physician language on health care comprehension. J Gen Intern Med. 2005;20:800–6. doi: 10.1111/j.1525-1497.2005.0174.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jacobs EA, Lauderdale DS, Meltzer D, Shorey JM, Levinson W, Thisted RA. Impact of interpreter services on delivery of health care to limited-English-proficient patients. J Gen Intern Med. 2001;16:468–74. doi: 10.1046/j.1525-1497.2001.016007468.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev. 2005;62:255–99. doi: 10.1177/1077558705275416. [DOI] [PubMed] [Google Scholar]
- 16.Karliner LS, Jacobs EA, Chen AH, Mutha S. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42:727–54. doi: 10.1111/j.1475-6773.2006.00629.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen AH, Youdelman MK, Brooks J. The legal framework for language access in healthcare settings: title VI and beyond. J Gen Intern Med. 2007;22:362–7. doi: 10.1007/s11606-007-0366-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baker DW, Parker RM, Williams MV, Coates WC, Pitkin K. Use and effectiveness of interpreters in an emergency department. J Am Med Assoc. 1996;275:783–8. [PubMed] [Google Scholar]
- 19.Yawman D, McIntosh S, Fernández D, Auinger P, Allan M, Weitzman M. The use of Spanish by medical students and residents at one university hospital. Acad Med. 2006;81:468–73. doi: 10.1097/01.ACM.0000222280.05953.19. [DOI] [PubMed] [Google Scholar]
- 20.Diamond LC, Schenker Y, Curry L, Bradley EH, Fernández A. Getting by: underuse of interpreters by resident physicians. J Gen Intern Med. 2009;24:256–62. doi: 10.1007/s11606-008-0875-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schenker Y, Wang F, Selig SJ, Ng R, Fernández A. The impact of language barriers on documentation of informed consent at a hospital with on-site interpreter services. J Gen Intern Med. 2007;22:294–9. doi: 10.1007/s11606-007-0359-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilson-Stronks A, Galvez E. Hospitals, language, and culture: a snapshot of the Nation. The Joint Commission and The California Endowment; 2007. [Google Scholar]
- 23.Regenstein M, Trott J, West C, Huang J. In any language: improving the quality and availability of language services in hospitals. Robert Wood Johnson Foundation; 2008. [Google Scholar]
- 24.Grubbs V, Chen AH, Bindman AB, Vittinghoff E, Fernández A. Effect of awareness of language law on language access in the health care setting. J Gen Intern Med. 2006;21:683–8. doi: 10.1111/j.1525-1497.2006.00492.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Burbano O’Leary SC, Federico S, Hampers LC. The truth about language barriers: one residency program’s experience. Pediatrics. 2003;111:e569–73. doi: 10.1542/peds.111.5.e569. [DOI] [PubMed] [Google Scholar]
- 26.Karliner LS, Mutha S. Achieving quality in health care through language access services: lessons from a California public hospital. Am J Med Qual. 2010;25:51–9. doi: 10.1177/1062860609351237. [DOI] [PubMed] [Google Scholar]
- 27.Cunningham H, Cushman LF, Akuete-Penn C, Meyer DD. Satisfaction with telephonic interpreters in pediatric care. J Natl Med Assoc. 2008;100:429–34. doi: 10.1016/s0027-9684(15)31277-3. [DOI] [PubMed] [Google Scholar]
- 28.Lee LJ, Batal HA, Maselli JH, Kutner JS. Effect of Spanish interpretation method on patient satisfaction in an urban walk-in clinic. J Gen Intern Med. 2002;17:641–5. doi: 10.1046/j.1525-1497.2002.10742.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Napoles AM, Santoyo-Olsson J, Karliner LS, O’Brien H, Gregorich SE, Pérez-Stable EJ. Clinician ratings of interpreter mediated visits in underserved primary care settings with ad hoc, in-person professional, and video conferencing modes. J Health Care Poor Underserved. 2010;21:301–17. doi: 10.1353/hpu.0.0269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jones D, Gill P, Harrison R, Meakin R, Wallace P. An exploratory study of language interpretation services provided by videoconferencing. J Telemed Telecare. 2003;9:51–6. doi: 10.1258/135763303321159701. [DOI] [PubMed] [Google Scholar]
- 31.Saint-Louis L, Friedman E, Chiasson E, Quessa A, Novaes F. Testing new technologies in medical interpreting. Cambridge (MA): Cambridge Health Alliance; 2003. [Google Scholar]
- 32.Locatis C, Williamson D, Gould-Kabler C, Zone-Smith L, Detzler I, Roberson J, et al. Comparing in-person, video, and telephonic medical interpretation. J Gen Intern Med. 2010;25:345–50. doi: 10.1007/s11606-009-1236-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Karliner LS, Pérez-Stable EJ, Gildengorin G. The language divide. The importance of training in the use of interpreters for outpatient practice. J Gen Intern Med. 2004;19:175–83. doi: 10.1111/j.1525-1497.2004.30268.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Crossman KL, Wiener E, Roosevelt G, Bajaj L, Hampers LC. Interpreters: telephonic, in-person interpretation and bilingual providers. Pediatrics. 2010;125:e631–8. doi: 10.1542/peds.2009-0769. [DOI] [PubMed] [Google Scholar]
- 35.Hornberger JC, Gibson CD, Jr, Wood W, Dequeldre C, Corso I, Palla B, et al. Eliminating language barriers for non-English-speaking patients. Med Care. 1996;34:845–56. doi: 10.1097/00005650-199608000-00011. [DOI] [PubMed] [Google Scholar]
- 36.Gany F, Leng J, Shapiro E, Abramson D, Motola I, Shield DC, et al. Patient satisfaction with different interpreting methods: a randomized controlled trial. J Gen Intern Med. 2007;22:312–8. doi: 10.1007/s11606-007-0360-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brennan SE, Lockridge CB. Computer-mediated communication: a cognitive science approach. In: Brown K, editor. Encyclopedia of language and linguistics. 2. Oxford, UK: Elsevier; 2006. pp. 775–80. [Google Scholar]