Abstract
In pregnancy, vascular nitric oxide (NO) production is increased in the systemic and more so in the uterine vasculature, so supporting maximal perfusion of the uterus. This high level of functionality is matched in the umbilical vein, and in corresponding disease states such as preeclampsia, reduced vascular responses are seen in both uterine artery and umbilical vein. In any endothelial cell, NO actually produced by endothelial nitric oxide synthase (eNOS) is determined by the maximum capacity of the cell (eNOS expression levels), eNOS phosphorylation state, and the intracellular [Ca2+]i concentration in response to circulating hormones or physical forces. Herein we discuss how pregnancy specific reprogramming of NO output is determined as much by pregnancy adaptation of [Ca2+]i signaling responses as it is by eNOS expression and phosphorylation. By examining changes in [Ca2+]i signaling responses from HHVE, UAEC, and HUVEC in (where appropriate) nonpregnant, normal pregnant, and pathological pregnant (preeclamptic) state, it is clear that pregnancy adaptation of NO output occurs at the level of sustained phase ‘capacitative entry’ [Ca2+]i response, and the adapted response is lacking in preeclamptic pregnancies. Further, gap junction function is an essential permissive regulator of the capacitative response and impairment of NO output results from any inhibitor of gap junction function, or capacitative entry using TRPC channels. Identifying these [Ca2+]i signaling mechanisms underlying normal pregnancy adaptation of NO output not only provides novel targets for future treatment of diseases of pregnancy, but may also apply to other common forms of hypertension.
Introduction: Evidence for pregnancy adaptation of cell signaling and associated changes in nitric oxide output
1.1 Pregnancy specific programming of endothelial nitric oxide production
Nitric oxide (NO) is an important vasodilator produced by vascular endothelium as a byproduct of the conversion of L-arginine, NADPH, and oxygen to L-citrulline, NADP+ and H+ by the enzyme endothelial nitric oxide synthase (eNOS). Once formed, NO acutely acts on underlying vascular smooth muscle cells to reduce tension and so relax the vessel. Since NO is both simple to make and a small and highly diffusible molecule, it is ideally suited to the task of quickly adjusting blood pressure in response to changes in local environment. Failure of the vascular endothelium to produce necessary levels of NO is associated with hypertension (eNOS knockout mice: Rees, et al. 1989, Huang, et al. 1995, Shesely, et al. 1996, Van Vliet, et al. 2003; hypertension in humans reviewed in Versari, et al. 2009) suggesting maintenance of chronic vasodilation through NO is a necessary part of chronic regulation of vascular tone and so vascular resistance associated with normal blood pressure and cardiac function. Indeed through long term but otherwise healthy conditions such as pregnancy, there is also evidence that while increased activity of the NO vasodilatory mechanism occurs in the maternal systemic vasculature in general, this is even more pronounced in the uterine vasculature in particular (Reviewed in Sladek, et al. 1997, Bird, et al. 2003). This exceptional upregulation of vasodilation in the uterine vasculature is impressive but also entirely logical; during pregnancy the uterus must adapt from a relatively quiescent state to a highly active state in order to bring about a 30–50 fold increase in blood flow necessary to provide the growing fetus with both the nutrition and oxygen needed for proper development. While this process is achieved through multiple complimentary mechanisms of angiogenesis as well as vasodilation, the increase in vasodilation is profound in itself, and pregnancies associated with failed vasodilatory adaptation due to diseases in humans or artificially created in animal models can also result in intrauterine growth restriction (Sladek, et al. 1997). More than a decade ago it was believed this increase in NO output was simply a result of vessel-specific changes in eNOS expression, and quite simply more enzyme makes more NO. More recent studies in uterine artery endothelial cells and hand vein endothelial cells in particular now suggest the process to be more complex, elegant, and indeed flexible, and that pregnancy associated changes in NO output can also occur though reprogramming at the level of post receptor cell signaling. We use the term programming because such differential responses are retained even with cell passage in vitro under standard culture condition (Mahdy, et al. 1998, Bird, et al. 2000, Di, et al. 2001, and reviewed in Bird, et al. 2003). Since the cells and their descendants literally respond according to which physiologic state they came from, independent of culture conditions, we have coined the phrase pregnancy adaptive programing to describe this phenomenon, and the changes observed at the level of signaling are in turn adaptive signaling mechanisms. An indication this is more than just an academic pursuit is given by the findings of Mahdy et al (Mahdy, et al. 1998) and Steinert et al (Steinert, et al. 2002), who have reported in human hand vein endothelial cells (HHVE) and human umbilical vein endothelial cells (HUVEC) preparations respectively, that cells in culture not only retain appropriate intracellular free calcium (termed [Ca2+]i) signaling function corresponding to nonpregnancy or pregnancy, but also show appropriate dysfunction if their origin is from diseased pregnancy. In this review we will focus on the adaptive signaling mechanisms that underlie normal pregnancy enhancement of eNOS activation in the three endothelial cell types studied in this way so far, namely HHVE, uterine artery endothelial cells (UAEC), and HUVEC, comparing results in the nonpregnant (NP-) uterine artery and hand vein vs late pregnant state (P-) uterine artery, hand vein, and umbilical vein in each case. Our primary goal is to provide insight into how the body is able to program optimal cell signaling for new vessels (umbilical vein) to maximally function, and also reprogram existing vessels (uterine artery and hand vein) to increase their NO output and associated vasodilatory capacity in response to long term changing physiologic needs. Further, we will discuss how these adaptations may fail in diseased pregnancy and exciting new data which shows how certain endocrine factors known to be abnormally high in unhealthy pregnancy may also act to block these same adaptive signaling mechanisms in otherwise healthy cells, compromising the desired NO output and associated vasodilation down to the level of nonpregnancy, and so potentially contributing to the development of associated hypertension.
1.2 Reprogramming of cell signaling underlies pregnancy related changes in NO production
Vascular endothelium has many roles to play, but in terms of vasodilation alone the cell needs to sense the local environment of the blood itself flowing over its surface, the endocrine factors circulating in the blood, the oxygen tension in the blood and tissues, and respond to paracrine signals from the underlying vascular smooth muscle (Esper, et al. 2006). That list alone is impressive and we have ignored for simplicity other interaction with immune cells and platelets. Clearly, to link vasodilation to all these factors requires the cell to integrate many different inputs from multiple receptors through a complex web of signaling pathways. Understanding the signaling events which allow a cell to sense its environment and thus regulate eNOS activity is essential to understanding how much NO a tissue can or will produce, and for how long. This is no small task and if there is any clear outcome to the studies over the past two decades in particular, it is that regulation of eNOS activity is complex. Beyond the initial cloning of its cDNA and deduction of its amino acid primary sequence, secondary and tertiary structure, several studies have suggested regulation through myristoylation, phosphorylation, calmodulin association, and binding of the eNOS dimer to other proteins including HSP90 and AKT (for a recent review see Dudzinski & Michel. 2007 and the companion review in this volume by Black and coworkers). Many studies of eNOS activation in both nonphysiologic (COS cells) models and physiologic (endothelial cells) have suggested that a complex sequence of events liberate eNOS from its binding to the caveolae, potentially aided by an increase in [Ca2+]i and so active calmodulin, and subsequent dimerization and further association with chaperone proteins such as HSP90 and kinases such as AKT, a kinase also associated with phosphorylation of eNOS at position 1177. The initial consensus was that phosphorylation of residues such as 1177 were stimulatory to activity, while phosphorylation of 495 was inhibitory to activity (Dimmeler, et al. 1999, Haynes, et al. 2000, Fleming, et al. 2001), but several recent studies of these and other phosphorylation events on eNOS expressed in Cos-7 cells and also in UAEC in particular have shown that phosphorylation also occurs at multiple other sites, and changes in a single or even multiple phosphorylation sites alone do not always correspond to changes in activity (Cale & Bird. 2006). Indeed phosphorylation can even occur without activation and activation can occur without changes in phosphorylation in intact cells (Cale & Bird. 2006, Sullivan, et al. 2006). Some investigators have further shown eNOS isolated from different subcellular pools show different phosphorylation patterns, and so suggested that subcellular trafficking of eNOS to these subcellular locations may in fact be the purpose of altered phosphorylation of key residues, rather than a means of activation alone (Garcia-Cardena, et al. 1996). Dephosphorylation of eNOS at 495 has also been proposed to promote the association of eNOS with calmodulin, so stabilizing the active state, while 1177 phosphorylation as a result of AKT association may in turn increase electron flux (Reviewed in Dudzinski & Michel. 2007). More recent studies have also shown directly that phosphorylation of residues 1177 and 615 combined shifts the [Ca2+] activation curve for eNOS to the left, i.e. increased [Ca2+]i sensitivity in the physiologic range (Tran, et al. 2009). Such a refinement of the eNOS activation model is certainly more consistent with the findings in Cos-7 and UAEC (Cale & Bird. 2006, Sullivan, et al. 2006) that phosphorylation alone is not sufficient for eNOS activation, and further cautions that reporting of eNOS phosphorylation state alone is not reliable as a surrogate indicator of eNOS activity.
The necessary stimulus alluded to above that is universally accepted as an activator of eNOS, and the focus of this review, is elevated [Ca2+]i. A surprising finding, however, was that while stimulation of a G protein coupled receptor signaling through rapid inositol 1,4,5-trisphosphate (Ins(1,4,5)P3) production may initially promote a rapid Ca2+ release from the ER, it is the subsequent sustained Ca2+ influx across the plasma membrane that is most important in maintaining eNOS activity (Lin, et al. 2000). This observation, however, does make sense when one considers that at rest eNOS is bound quiescent to the caveolae (on CAV-1) in an inactive state and it will take time to translocate in response to an increase in Ca2+-calmodulin complex formation, followed by eNOS dimerization and associated phosphorylation/dephosphorylating steps necessary for full complex activity. An ongoing [Ca2+]i response would then presumably maintain eNOS in the cytosol which remains active, further aided by maintenance of appropriate eNOS phosphorylation and complex assembly. It is thus no coincidence that the most important form of adaptive cell signaling associated with pregnancy enhanced eNOS activation is sustained Ca2+ influx into the cell. We hereafter narrow our focus on this particular adaptation of sustained [Ca2+]i responses in the cell and the molecular events that underlie this adaptive response. A picture is also emerging that certain other hormones may be able to actively oppose these changes at the level of [Ca2+]i signaling, and the MEK/ERK pathway may be a common mediator of this blockade of adaptive [Ca2+]i signaling under the right (or maybe we should say wrong) circumstances.
The mechanistic basis for programmed adaptation of [Ca2+]i signaling
2.1 Hand vein endothelial cell programing
In order to discuss the role of pregnancy adaptive programming and associated adaptive signaling mechanisms, we begin with the earliest hallmark study by Mahdy et al (Mahdy, et al. 1998) using human HHVE maintained in culture under standard conditions for a minimum of 14 days. Despite being removed from the local environment for weeks and undergoing many cell divisions, the HHVE remarkably ‘remembered’ which physiological state they were derived from. Cells removed from healthy nonpregnant women (NP-HHVE) had a predictable [Ca2+]i signaling signature when exposed to a range of agonists, while those harvested from healthy pregnant women (P-HHVE, 35 weeks gestation) behaved in a separate but equally predictable way. This was the first evidence that the fundamental nature of the cell response to its extracellular environment was altered and indeed reprogrammed for pregnancy, such that this behavior could be passed from generation to generation, ensuring long-term maintenance until told otherwise by further factors presumably associated with parturition and/or the post-delivery condition. Of note, while HHVE cells are part of the systemic vasculature and have no direct bearing on uterine and umbilical perfusion, some degree of resistance to pressor effects is indeed seen in the systemic vasculature during pregnancy (Rosenfeld & Gant. 1981). This is of no small consequence, since it suggests that understanding of adaptive signaling mechanisms during pregnancy could also hold the potential to develop new endothelial targeted therapies aimed at systemic disorders such as general hypertension in nonpregnant subjects.
At a more mechanistic level, the principal adaptation described by Mahdy et al is that various agonists (ATP, bradykinin, and histamine) are all able to elicit greater [Ca2+]i and even more sustained responses in P-HHVE than NP-HHVE. In the most convincing case, that of ATP stimulation, upregulation of [Ca2+]i signaling in P-HHVE occurred at two levels. Both the initial peak and the subsequent plateau phases were of greater amplitude compared to NP-HHVE. While 100% of cells from both groups were capable of producing a [Ca2+]i response to ATP, variation was seen with other agonists. Bradykinin was significantly more efficient at stimulating a [Ca2+]i response in pregnant-derived cells than the nonpregnant-derived group, although peak amplitudes in those cells that responded were otherwise relatively unchanged (the nature of the [Ca2+]i response to agonists other than ATP did not allow for peak and plateau comparisons). Histamine, on the other hand, was quite efficient at producing a [Ca2+]i response in cells from both groups, but like ATP, the amplitude was significantly greater in the P-HHVE than NP-HHVE. Furthermore, and as we will discuss in detail in the UAEC model, both peak and sustained (plateau) phase [Ca2+]i responses to ATP were increased in magnitude during pregnancy in endothelial cells. Taken together, these groundbreaking early observations did clearly describe for the first time a programming event, observable at multiple levels of cell [Ca2+]i signaling and maintained in culture independently of tonic pregnancy associated circulating factors. This study did not, however, describe if the changes observed in [Ca2+]i signaling were occurring at the receptor or post receptor level, or indeed how. Nonetheless it was at this point that methods were developed to culture uterine artery endothelial cells (Bird, et al. 2000, Di, et al. 2001), a system derived from the uterine artery endothelium that is known to undergo dramatic increases in blood flow during normal pregnancy, and it was studies of these cells which addressed in more detail these further mechanistic questions.
2.2 Uterine artery endothelial cell programming
2.2.1 The UAEC model
While the systemic circulation undergoes noticeable adaptations with regard to vascular compliance to handle the increased blood volume and cardiac output associated with pregnancy, the uterus undergoes even more extreme adaptive remodeling. Since acquisition of human tissue from pregnant subjects is difficult and in vitro techniques are more closely matched to investigations of cell signaling pathways, an animal cell culture model was used. The ovine model for physiologic pregnancy adaptation has been characterized extensively (Sladek, et al. 1997, Bird, et al. 2003), so creating a cell culture model for this animal was a logical choice. Freshly isolated cells from pregnant sheep do indeed show higher levels of eNOS protein (Bird, et al. 2000) as previously reported in vessels (Magness, et al. 1997) but more recent studies using NO sensitive dyes in freshly isolated cell plaques and more recently in intact vessels (Yi, et al. 2005, Yi, et al. 2010a) have shown that increases in NO output exceed the previously reported change in level of eNOS protein (Magness, et al. 1997, Bird, et al. 2000, Magness, et al. 2001). Furthermore, when freshly isolated uterine artery endothelium (UA Endo – endothelial cells observed either intact on the vessel surface or immediately after isolation in cell sheets) was isolated, placed in culture, and maintained to passage 4 (now termed UAEC), differences in function were still observed, even though eNOS protein levels nearly equilibrated between NP- and P-UAEC preparations by passage 4 (Bird, et al. 2000, Di, et al. 2001, Sullivan, et al. 2006, Grummer, et al. 2009). This ability to activate eNOS and produce NO at a greater level in P-UAEC over NP-UAEC without a corresponding elevation of eNOS protein immediately raised the possibility that while eNOS protein levels may be important in terms of determining the cell capacity for NO output, it may not be the sole determinant of actual NO output. Furthermore, pregnancy enhanced UAEC cell function was apparently programmed, since pregnancy specific adapted function could be maintained through limited cell divisions under standard cell culture conditions even in the absence of elevated eNOS expression. This in turn implied there must be signaling events impacting on eNOS activation that are reprogrammed during pregnancy to increase eNOS activation efficiency and these are retained in UAEC in limited primary culture. Since [Ca2+]i is known to be crucial to eNOS activation, and Mahdy et al demonstrated pregnancy adaptive programming at the level of [Ca2+]i signaling, subsequent work in UAEC has in large part been focused in this area.
2.2.2 Early Studies implicating CCE as the basis for pregnancy adaptation
Early [Ca2+]i studies in UAEC examined low density single cell recordings in a manner closely analogous to that of Mahdy et al (Mahdy, et al. 1998). Recordings for 5 minutes after ATP addition revealed that while a strong initial [Ca2+]i peak was observed in all cases, an enhanced sustained phase of [Ca2+]i response was observed in P-UAEC which did not rapidly return to basal unlike the response seen in NP-UAEC (Di, et al. 2001). Thus the differences between P-UAEC and NP-UAEC were similar to that in HHVE (Mahdy, et al. 1998). Further studies showed that while the immediate [Ca2+]i response was due to release of Ca2+ from an intracellular source, the secondary sustained phase was dependent on extracellular Ca2+. This was consistent with a capacitative calcium entry (CCE) mechanism, and for the 5 minutes duration of these initial recordings in P-UAEC, [Ca2+]i showed no signs of returning to basal levels (Gifford, et al. 2003). In light of these initial findings, subsequent recordings were taken out as far as 1 hour (Gifford, et al. 2006a, Gifford, et al. 2006b), and on average it took roughly 30 minutes for P-UAEC cells grown in patches to return to near basal levels (Fig. 1A). This was 10–15 minutes longer than for NP-UAEC to return to basal after ATP stimulation (Gifford, et al. 2006b). These studies made the point that pregnancy adaptive programming was not simply a short-term phenomenon, but also included changes in sustained phase [Ca2+]i signaling and likely associated NO production. Furthermore, this sustained phase response seemed to be an adaptation of CCE, but precisely what mechanism and specific molecular signaling changes within the cell could account for such a programmed adaptation of cell signaling was unclear.
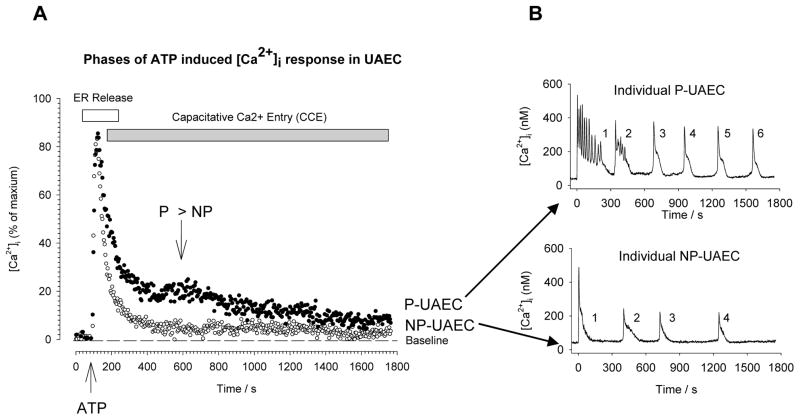
Figure 1. Comparison of grouped average cell response vs individual cell [Ca2+]i response in NP- and P-UAEC.
In all studies cells at high density were loaded with Fura 2 and imaged using the same methodology. In panel A, the results are the combined cell average data from multiple dishes (n=8) with the equipment set to gather data from all cells simultaneously in the entire imaging field (approx. 150 cells). As such this is a reflection of the average combined response and would relate most closely to the overall physiologic activation of NO production experienced by a whole vessel. Note after a broader initial peak in P-UAEC (dark symbols) compared to that in NP-UAEC (open symbols), the sustained CCE phase continues above basal for almost the full remaining 20 minutes, while in NP-UAEC the response falls and remains close to but not quite at baseline. The greatest point of difference in the sustained phase is at approximately 8 minutes after stimulation (agonist added at ~1.5 minutes), as indicated by the arrows. B): An alternative approach is to image individual cells and this reveals clearly that after the initial peak the sustained phase is in fact a series of [Ca2+]i bursts. Since these bursts are both maintained with higher efficiency (more numerous) and occur in more cells in P-UAEC than in NP-UAEC, the average sustained phase CCE response in panel A is greater. The point of greatest differences indicated in panel A occurs simply because the Peak 2 is most likely to occur at that time while the Peaks 3 onward became less and less likely, but still occur more commonly in P-UAEC than in NP-UAEC.
2.2.3 Identifying the adaptive CCE mechanism
Classic G protein coupled receptor (such as P2Y2 for ATP) signaling cascades linked to Ca2+ mobilization commonly function through PLC-beta activation and associated cleavage of PIP2 into Ins(1,4,5)P3 and DAG. The suddenly released Ins(1,4,5)P3 then diffuses through the cytosol and binds Ins(1,4,5)P3 receptors (IP3Rs) in close proximity on the underlying ER membrane, thus opening to release Ca2+ from the ER stores into the cytosol. The subsequent sustained response thereafter shows the properties of CCE, and while it is not sensitive to the L- channel inhibitor nifedipine, it is sensitive to the PLC inhibitor U73122 and the IP3R inhibitor 2-APB (Gifford, et al. 2006a). This infers the involvement of a membrane Ca2+ channel more typical of the TRPC family (Trebak, et al. 2003), and we have recently shown such channels are indeed present and interact with IP3R in NP- and P-UAEC (Gifford, et al. 2006b) (see also Fig 2).
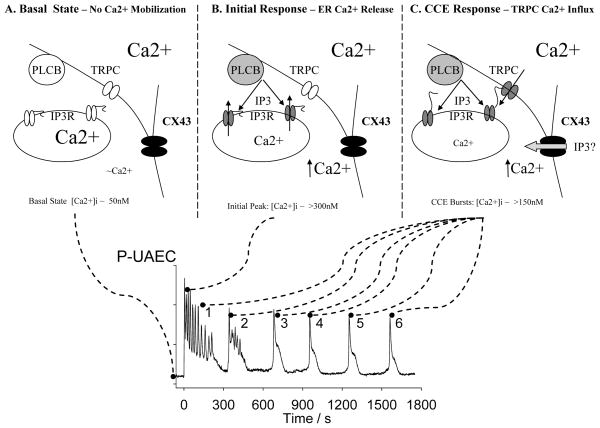
Figure 2. Proposed mechanisms underlying the [Ca2+]i response to ATP over 30 minutes in P-UAEC.
Upper Panels A–C: Note in all upper panels the darker the shading the more active/open the protein. Lower Graph: This represents a typical [Ca2+]i response to 100uM ATP in a single P-UAEC cell over 30 minutes. A) In the basal state the intracellular Ca2+ pool in the Endoplasmic Reticulum (ER) is full and the IP3Rs are at rest. PLC-beta is inactive due to the lack of agonist stimulation. The TRPC3 channels are closed for lack of stimulation. Nonetheless CX43 channels are maintained in a permanently open state. B) On initial agonist stimulation the initial upslope of the first increase in [Ca2+]i is solely due to release of intracellular ER pool of Ca2+. This is in turn due to PLC-beta activation and the resulting rise in Ins(1,4,5,)P3 which then activates IP3R. C) Once the ER is empty of Ca2+ (at the peak) the IP3R detects this change and in turn undergoes a physical change in shape, so allowing physical communication with overlying TRPC channels in the plasma membrane and they are triggered to open. This in turn allows in Ca2+ from the extracellular space. Initially this serves to extend the first major peak. We suspect the rapid superimposed oscillations are the result of rapid [Ca2+]i sensitive changes in the activity of Ins(1,4,5)P3-3 kinase. As in most cells the system operating to produce the first major peak of [Ca2+]i then shuts itself off through as yet unidentified mechanisms. Thereafter, over the remaining 25 minutes, the TRPC activation system again activates periodically, suggesting IP3 production is maintained and the ER remains partially or nearly empty, or other regulatory mechanisms now apply to TRPC activation. While the source of Ca2+ for burst 2 onwards is essentially extracellular through TRPC channels, the process remains entirely dependent on CX43 remaining open to communicate between the cells. In this figure we have shown Ins(1,4,5)P3 moving between the cells (IP3) which is certainly possible but equally CX43 may communicated by passing Ca2+ or providing electrical coupling. Further studies are needed on this specific point.
Given the suggested involvement of TRPC channels in the UAEC CCE response, subsequent studies showed TRPC3 and TRPC6 were readily detectable in whole cell lysates (Gifford, et al. 2006b). Furthermore, IP3R isoforms IP3R1, IP3R2, and IP3R3 were all present (Gifford, et al. 2003 supplemental data, Gifford, et al. 2006a). Of note, while CCE function is clearly different in P-UAEC from that in NP-UAEC in response to the same physiologic and pharmacologic agonists (Gifford, et al. 2006a, Gifford, et al. 2006b), no significant difference in expression could be detected at the level of P2Y2 receptor expression, IP3R isoform expression or TRPC3 or TRPC6 expression (Gifford, et al. 2006b). Nonetheless, co-immunoprecipitation at 8 minutes of treatment with ATP (time of “shoulder” in whole field recordings and coincide with the typical time for peak two in the individual cell recordings, Fig. 1A, B) revealed an agonist and pregnancy sensitive interaction between IP3R2 and TRPC3, such that ATP but not vascular endothelial growth factor (VEGF-165) stimulated significant interaction in P-UAEC but not NP-UAEC. Further, at 19 minutes post-stimulation, a time where the plateau in whole field ‘average’ recordings approaches basal levels in both P- and NP-UAEC (Fig 1A), neither ATP nor VEGF-165 were able to produce a significant co-IP in either cell type. This showed an ATP and pregnancy specific activation of TRPC3 was likely the mediator of pregnancy adapted CCE (Fig 2), but also begs the question of just what might be coordinating the pregnancy-specific increase in the ATP stimulated [Ca2+]i CCE responses, given that protein levels of the key TRPC3 and IP3R2 mediators do not change in UAEC in response to pregnancy?
Some further clues of the difference in P-UAEC vs. NP-UAEC function came from an alternative approach when dissecting CCE mechanisms, namely to use a pharmacologic means to empty the ER directly, independently of a physiologic agonists, using agents such as thapsigargin. Once the initial release of Ca2+ from the ER occurs in response to thapsigargin, and so the ER empties, the subsequent CCE process of TRPC/IP3R coupling is triggered leading to Ca2+ influx across the plasma membrane. Resulting prolonged depletion of the ER Ca2+ stores without refilling can also lead to a hyper-responsive state whereby store operated channels in the plasma membrane can be held in a permanently open state. If the thapsigargin is initially applied without any free Ca2+ in the extracellular buffer, on subsequent re-addition of mM Ca2+ back into the medium the result is a supra physiologic influx of Ca2+ into the cell cytosol which is diagnostic of CCE. Such a response was indeed observed in UAEC (Gifford, et al. 2006a), but most interesting was that two simple experiments illustrated very effectively that this CCE process itself is also greatly enhanced in pregnancy. First, removal of extracellular Ca2+ from the experimental buffer revealed that when cells are then stimulated with ATP, the P-UAEC and NP-UAEC are both depressed to a common level, returning to near basal [Ca2+]i within 5–6 minutes. Thus the initial pool of Ca2+ mobilized by Ins(1,4,5)P3 from the ER is not apparently different (Gifford, et al. 2006b). Nonetheless, when the receptor independent ER store depleting drug thapsigargin was administered to P- and NP-UAEC in Ca2+ free extracellular buffer, and after 15 minutes (a time that allowed nearly complete ER store depletion) Ca2+ was then added back to the buffer to assess CCE, the P-UAEC level of CCE response was greatly enhanced above that in NP-UAEC (Gifford, et al. 2006a). Taken together, the results of these experiments show that while agonists stimulation of early Ins(1,4,5)P3 is apparently similar, and the corresponding pool of Ca2+ available in the ER itself is similar at time zero, the subsequent sustained phase of extracellular Ca2+ influx from extracellular sources through CCE triggered once the ER empties is different in a pregnancy specific manner and this is programmed into the cell rather than to the agonist receptor or G protein/PLC-beta complex. As such this means pregnancy adaptation is a way of increasing [Ca2+]i signaling gain at the level of the CCE mechanism itself, and must lie at the level of function of the IP3R/TRPC coupling unit, rather than at the level of IP3R or TRPC expression. Furthermore it not only follows that all physiologic agonist responses using this same IP3R/TRPC based CCE mechanism will likely be enhanced by pregnancy to the same degree, but also that any manipulation that inhibited these IP3R/TRPC post receptor signaling mechanisms responses would negatively impact on these same agonists responses to the same degree. This is entirely consistent with what had previously been reported in HHVE (Mahdy, et al. 1998).
2.2.4 The role of gap junctions in facilitating adaptive changes in CCE
While much early work was undertaken at low cell density, it was noted NO output was most optimal when UAEC preparations were at 70% confluence or above (Di, et al. 2001). When comparing long term tracings from low density cell recordings with subsequent higher density cells or freshly isolated UA Endo cell patches, an important pattern began to emerge. Those from the high density patches appeared to have a coordinated [Ca2+]i burst pattern that was not apparent in the low density cultures. This prompted studies on individual UAEC cells at varying densities for a 30 minute duration to examine if this was a reflection of synchronized single cell responses. Bursts did occur in UAEC in a periodic and transient manner, and were more abundant in P-UAEC than NP-UAEC (Fig 1B), and also increased in numbers of bursts and duration of time occurring as cell density further increased (Yi, et al. 2010a). Likewise, burst synchronization was also far more apparent in P-UAEC than NP-UAEC (Fig. 1B) and this in turn further increased at cell densities of 70% or above. In those cells which showed synchronous bursts, synchronization was observed in local groups, but not all cell responses between such groups aligned, especially as time increased. This may explain why imaging of the entire field comprising many cells, the average sustained phase CCE response appeared more as a plateau with some smaller bumps superimposed, mostly in the first 10 minutes. In fact, a well-defined shoulder was often observed for average recordings of fields of cells that was very often present between 5–10 minutes after agonist addition. This time point was in fact coincident with when the second [Ca2+]i peak was most commonly observed in individual cell tracings in cells at high density (70% plus). Thus, in high density P-UAEC, the sustained CCE response actually took the form of repeated [Ca2+]i bursts with both the number of bursts and duration of bursting behavior being greater than that observed in NP-UAEC, and that this response was entirely dependent on cell density. These same studies also found the mediator of the cell density dependence of [Ca2+]i bursting and synchronization was cell-cell communication through gap junctions (Yi, et al. 2010a).
Gap junctions play an important role in cell-cell communication in a variety of cell types by creating a pore made of a complex of connexin (CX) molecules, permeable to small molecules and ions (including Ca2+ and Ins(1,4,5)P3) between adjacent cells (Fig 2), as well as possibly altering membrane potential and therefore possibly mediating electrical field effects. Endothelial cells are no exception, and UAEC express CX43 in large quantities, while other connexin proteins commonly seen in endothelial cells (CX37, CX40) are either not present or present below the levels necessary to resolve by western blot. Of note, as for the P2Y2 receptor and other [Ca2+]i signaling molecules in UAEC, CX43 expression levels were again found to be equivalent between P- and NP-UAEC. Nonetheless, basic analysis of connexin permeability with Lucifer yellow dye transfer showed that P-UAEC maintain greater cell-cell communication in the basal state than do NP-UAEC (Yi, et al. 2010a). While no changes in expression of CX43 were observed between P- and NP-UAEC, other considerations beyond cell density include both the placement of CX43 into the plasma membrane itself, and the post-translational modifications (such as phosphorylation at various residues on the C-terminus) it may experience that result in an open or closed functional state. When gap junctions are properly placed in the plasma membrane, organized into local groups, and brought in proximity to those on a neighboring cell, a stable interaction is formed between the extracellular loops of the connexin rafts from each cell (reviewed in Saez, et al. 2003). One way to block this process is to use peptide mimetics of the extracellular loop portions of connexin molecules to competitively and selectively block connexin interactions between cells at high density (Evans & Boitano. 2001, Yi, et al. 2010a). In UAEC the CX43,37 specific mimic, Gap27 is able to completely reverse the pregnancy adaptive programing of P-UAEC CCE [Ca2+]i signaling down to a level common with that of NP-UAEC, while mimetics specific to other connexin isoforms were ineffective, including one specific to CX37 and 40, and a Gap27 scrambled or vehicle control (Yi, et al. 2010a). Thus CX43 is the only connexin functionally responsible for the pregnancy adaptive programming of the UAEC [Ca2+]i response, and blockade of CX43 function reverses pregnancy adaptation of sustained CCE signaling function by TRPC3 and IP3R2 in those same UAEC (Yi, et al. 2010a). Indeed, blockade of CX43 function also removed pregnancy specific differences in eNOS activation in NP- vs. P-UAEC (Yi, et al. 2010a), suggesting CCE bursts to be causally linked to eNOS activation. Beyond this identification of CX43 as the key player in controlling CCE and so pregnancy enhanced eNOS activation in UAEC (Fig 2), the question now arises of the possible physiologic relevance of mechanisms regulating CX43 function through phosphorylation of key residues, so altering overall charge of the open pore, as well as tertiary, and quaternary structures. In many other cells expressing CX43, functionality can be acutely diminished by treatment with the receptor-independent PKC agonist TPA (12-O-tetradecanoylphorbol 13-acetate – also known as PMA), which leads to CX43 phosphorylation at positions 262,368, and the 279/282 combination (reviewed in Solan & Lampe. 2009, Warn-Cramer, et al. 1996, Lampe & Lau. 2000, Lampe & Lau. 2004, Sirnes, et al. 2009). These phosphorylations are commonly mediated through PKC, but also the MEK/ERK signaling pathway. It is therefore of some considerable relevance that P-UAEC which otherwise show enhanced [Ca2+]i bursts can be inhibited in both burst number per cell and in number of cells responding by pre-treatment with 10 nM TPA (Cale & Bird. 2006). Future investigation of changes in phosphorylation state of CX43 at the key residues mentioned above in NP- vs P-UAEC and further identification of physiologic agonists, receptors and kinases that may act on those residues may hold the key to explaining how the observed pregnancy specific changes in function can occur independently of an otherwise common level of CX43 expression in P-UAEC vs NP-UAEC, and possibly how this adaptation may fail.
2.3 Human umbilical vein endothelial cell adaptive programming
While of considerable value in defining what normal pregnancy adaptation relative to nonpregnancy may be, the inherent drawback in the UAEC model is that there is no corresponding condition in sheep whereby it is clear this adaptation has actually failed. Nonetheless, there is one easily acquired set of vessels from the maternal-fetal unit that can be used to study maladaptation, rather than a lack of adaptation. This tissue is the umbilical cord, most notably the umbilical vein and the endothelial cells derived from it, the HUVEC. Of course, there is no umbilical cord without pregnancy, so there clearly cannot be a nonpregnant ‘control’ for HUVEC studies. Given that the umbilical vein may be functionally similar to uterine arteries in normal pregnancy in terms of [Ca2+]i signaling and NO production, and knowing the uterine vascular adaptation is lacking in preeclamptic humans (Sladek, et al. 1997, Bird, et al. 2003, Roberts & Hubel. 2010), one might predict umbilical vein dysfunction may look like uterine artery in the nonpregnant state. In a study by Steinert et al (Steinert, et al. 2002), histamine treated HUVEC from normal pregnancies did indeed show some of the same phenomenology of pregnancy adaptive programming otherwise reported in ATP treated HHVE and UAECs. These studies by Steinert et al also addressed functional signaling differences between cells cultured from dysfunctional (preeclamptic) and healthy pregnancies and indeed those from preeclamptic subjects did show reduced CCE response comparable to responses of UAEC or indeed HHVE from nonpregnant subjects.
On a mechanistic basis, the findings pertaining to the [Ca2+]i signaling in normal HUVECs when treated with histamine can be summarized in two key observations: The response was biphasic, with an initial peak and an extended plateau phase, and further, the plateau was dependent on influx of extracellular calcium, presumably through CCE (Steinert, et al. 2002). The recordings were short (less than 5 minutes), but a clear peak and plateau were visible. When Ca2+ was removed from the experimental media, histamine treatment was still able to produce an initial [Ca2+]i peak of comparable magnitude to that observed with Ca2+ present in the media. The initial peak quickly came back to basal levels, without any sustained CCE phase in the Ca2+ free media, which was very similar to that observed in UAEC in similar conditions after ATP treatment (Steinert, et al. 2002, Gifford, et al. 2006b). When Ca2+ was then added back to the media, [Ca2+]i again rose in HUVEC taking the form of a small peak which very quickly plateaued into a sustained phase (Steinert, et al. 2002). This again is consistent with what would be expected of a cell that undergoes efficient (pregnancy adapted?) CCE after agonist stimulated store depletion. Unfortunately, the short duration of these experiments did not allow for the detection or quantification of long-term transient burst patterns, which histamine has otherwise been shown to induce in HUVEC and other endothelial cell types (Morgan & Jacob. 1998, Hu, et al. 2002). Similar studies were also undertaken in a spontaneously transformed HUVEC cell line (HUVEC-CS, Gifford, et al. 2004) showing that the cells would also respond to 10 minute treatment with ATP with an initial peak and subsequent sustained response. Of note, the initial peak was not reproduced if cells were pretreated with thapsigargin, suggesting the initial [Ca2+]i response to ATP to be of intracellular origin. Also the sustained phase was not inhibited by L-channel antagonists suggesting while CCE may occur, L-channels at least were not responsible. So is it possible the HUVEC from normal cords and possibly HUVEC-CS cells also use TRPC channels for adapted CCE function, and that this is enhanced by CX43 with increasing cell density, as reported in UAEC (Yi, et al. 2010a)? While that question cannot yet be definitively answered, a number of indirect observations suggest it is likely. In these same HUVEC-CS, P2Y2 receptor protein was shown to be abundantly expressed (Gifford, et al. 2004) and functionally coupled to [Ca2+]i signaling, probably via Gq (Gifford, et al. 2004, Tanaka, et al. 2004). PLC-beta 3 is also known to be present in HUVEC (Bhattacharya, et al. 2009), and both TRPC3 (Groschner, et al. 1998) and CX43 (Van Rijen, et al. 1997) protein expression have been reported, just as we have described in UAEC preparations (Yi, et al. 2010b). In HUVEC-CS cells the CX43 associated protein ZO-1 is also abundantly detected (Gifford, et al. 2004). To be clear, CX43 is not the only connexin isoform in HUVEC, indeed three types of connexin protein are reportedly expressed, namely CX37, CX40 and CX43, but studies of paired patch clamped cells have also shown that cell-cell electrical communication is only mediated by CX43 (Van Rijen, et al. 1997), the same isoform that is responsible for cell-cell coupling of [Ca2+]i responses in UAEC. Indeed Yi et al have also suggested this coupling of P-UAEC to be electrical given the tight burst synchronization observed between cells (Yi, et al. 2010a).
Evidence that changes in adaptive CCE signaling during pregnancy directly underlies changes in NO output by endothelial cells beyond changes in eNOS expression
3.1 Establishing cause and effect between the pregnancy adapted CCE [Ca2+]i response and increased NO output
Discussions of agonist stimulated [Ca2+]i responses and mechanisms are important in and of themselves, but ultimately pregnancy adaptation of the CCE response is most important in the context of eNOS activation. Simply put, eNOS cannot be maximally activated without increased [Ca2+]i and particularly it seems sustained [Ca2+]i elevation through CCE (Yi, et al. 2005, Sullivan, et al. 2006, Yi, et al. 2010a). Studying direct effects of [Ca2+]i on NO production to firmly establish cause and effect is no small task given the difficulty of detecting NO directly, so much of what is known to date is mostly from indirect measures of NO or NO action.
3.1.1 Considerations in measuring ‘NO output’
Techniques such as vessel myography, nitrate/nitrite detection assays, and arginine-citrulline conversion assays allow us to monitor vessel relaxation and infer eNOS activity but the involvement of eNOS under these experimental conditions is most often implicated through L-NAME blockade of the observed changes and comparison to the removal of the endothelium (i.e. a ‘proof by deduction’ approach) (Sladek, et al. 1997). It also follows that if the assay for NO production is relaxation of preconstricted vessels, and given that [Ca2+]i elevation also mediates at least in part the contraction of vascular smooth muscle cells to obtain that preconstriction, then simple application of Ca2+ antagonists in such assay systems always raises the question of the absolute specificity of which cells were impacted by the drug. It follows, therefore, that while any such study may indeed show that NO mediated relaxation has occurred, these limitations mean that direct demonstration of the cause and effect relationship between [Ca2+]i elevation in endothelium and NO production in endothelium is rarely achieved and at best data is correlative. Fortunately there are two ways around this. The first is to separate the cells. Such experiments in isolated endothelial cell systems in the past have typically required that eNOS activity is measured through assays such as nitrate/nitrite detection or Arginine->Citrulline conversion but given such methods are successful (i.e. sufficiently sensitive), then parallel measures of [Ca2+]i and ‘NO’ (or eNOS activity) combined with use of additional ‘Ca2+ antagonists’ can demonstrate the cause and effect relationship between [Ca2+]i and NO. Alternatively, it is now possible to use NO sensing dyes inside cells alongside the use of [Ca2+]i sensitive Fura 2, so parallel measures can not only be made, but can even be made in individual cells in real time. Simply by virtue of optical focal plane considerations, endothelium on the intact vessels ex vivo can also be investigated in their native vascular architecture, without interference of optical signals from underlying smooth muscle. Given such measures of endothelium function are now direct, then [Ca2+]i signaling antagonists can be used to show cause and effect relationships with NO production on a per cell as well as per vessel basis.
3.1.2 Studies based on measures of eNOS activity in UAEC
Of the three vessels discussed above, there is no apparent data relating programming of cell signaling to eNOS activity in HHVE or HUVEC, but a number of studies have been undertaken in UAEC using Arg->Citr conversion and/or detection of nitrate/nitrite (Di, et al. 2001, Sullivan, et al. 2006, Grummer, et al. 2009, Yi, et al. 2010a). Initial studies in UAEC (Sullivan, et al. 2006) have shown that the ATP stimulation of both initial peak and sustained phase [Ca2+]i responses in both NP- and P-UAEC are blocked by 2-APB (a blocker of IP3R activation) and U37122 (a blocker of PLC-beta). With the complete blockade of [Ca2+]i elevation a 40–60% reduction in eNOS activity is also observed from that of ATP alone (Sullivan, et al. 2006). Of greater significance is the finding that when the ATP stimulated [Ca2+]i response is blocked by 2-APB or U73122, the pregnancy-specific increase in eNOS activity is also lost, and P-UAEC and NP-UAEC equilibrate to equivalent levels of reduced eNOS activation, as measured by Arg->Citr conversion. These data suggest that if the [Ca2+]i response is completely blocked, ATP stimulated eNOS activity can, at best, reach 40% of maximal activation and further, the increase in P-UAEC over that in NP-UAEC which is so critical for enhanced vasodilation is completely lost. It should again be noted that in passage 4 UAEC, the pregnancy-specific increase in eNOS expression of freshly isolated P-UAEC has fallen to that maintained in NP-UAEC, so nearly identical amounts of eNOS protein are available in each case (Bird, et al. 2000, Grummer, et al. 2009).
While the 2-APB/U73122 experiments elegantly display the importance of [Ca2+]i in eNOS activation and infer the pregnancy adapted increases in eNOS activity is also regulated by pregnancy adaptation of [Ca2+]i signaling, they tell us very little about the relative importance of the initial vs sustained phases of the [Ca2+]i response. Nonetheless, the CX43 gap junction inhibitor Gap27 specifically inhibits only the sustained phase burst pattern during long-term ATP stimulation in P-UAEC to NP-UAEC levels, and so the initial peak remains intact and is identical between ATP treatments alone and after incubation in the presence of Gap27, while the subsequent bursts are blocked to a common low level without the need to remove Ca2+ from the medium. When UAEC are incubated with Gap27, and the [Ca2+]i bursts are lost (Yi, et al. 2010a) eNOS activity in P-UAEC is also reduced to a similar extent to the effect of 2-APB or U73122, i.e. by 60% to a level indistinguishable from NP-UAEC (Yi, et al. 2010a). Therefore, we can conclude that not only is [Ca2+]i an important regulator of eNOS activation, and accounts for the pregnancy specific difference in activations, it is indeed the sustained phase CCE [Ca2+]i response alone that is responsible for pregnancy adaptive programming of eNOS activation. While in all of these treatments blocking CCE, 40% of eNOS activity remains, presumably through other mechanisms such as phosphorylation, this ‘partition’ of some degree of eNOS activation by kinases is not primarily responsible for the divergence in eNOS activation efficiency between P-UAEC and NP-UAEC, while changes in the CCE response clearly is.
3.1.3 Studies based on the direct measure of NO production in UA Endo
While the studies in UAEC have yielded much valuable information, the use of Arg->Citr conversion does not allow real time temporal monitoring of NO output as can otherwise be achieved in monitoring of [Ca2+]i with Fura 2. Nonetheless, freshly isolated endothelium has sufficient eNOS expression to allow real time monitoring using DAF-FM or DAF-2 dye. Intact vessels and freshly isolated sheets of UA Endo present a unique opportunity to study the ability of individual cells to produce NO as part of an intact sheet of endothelium ex vivo. Indeed the spectral properties of Fura2 and DAF based dyes are complimentary, so simultaneous [Ca2+]i and NO imaging can also be achieved, allowing us to observe direct [Ca2+]i and NO correlations within each cell. Not surprisingly, such studies have been most revealing. In initial studies wherein isolated UA Endo sheets were treated with ATP and monitored for [Ca2+]i and NO (Yi, et al. 2005), several important observations were made. While the [Ca2+]i data for cell sheets en mass agreed with that previously, i.e. that while pregnancy does have some effect to increase the size of the initial peak in freshly isolated cells, its main action is to enhance the sustained CCE phase of [Ca2+]i response and maintain it for at least twice the duration of that seen in NP – UA Endo. The more striking result was that by using DAF-FM it was clear that the NO output was a strong initial burst of greater magnitude in P-UA Endo than in NP-UA Endo but also that NO production was more sustained in P-UA Endo than in NP-UA Endo, and further that the duration of NO output was most closely related to the magnitude and duration of the sustained CCE phase [Ca2+]i response. Cause and effect was also established as once again the application of 2-APB showed that the loss of [Ca2+]i response was paralleled by a loss of NO output to a common low level, and again this was similar to the 60% inhibition observed in P-UAEC. More recently, in light of the recent observations of pregnancy adaptation of [Ca2+]i bursts at an individual cell level in P-UAEC and NP-UAEC these studies have been examined more closely on a cell by cell basis in ‘intact’ vessels, i.e. on endothelium still attached to the vessel lumen (Yi, et al. 2011). As anticipated, [Ca2+]i burst patterns were indeed detected in individual endothelial cells of the intact vessel, and while the bursts per 30 minute period were slightly less numerous in intact vessels than in UAEC at passage 4, they were also broader, and still clearly enhanced in both occurrence and duration by pregnancy. Again the P-UA Endo output of NO was both larger and more sustained than in NP-UA Endo, and again as long as this burst pattern continued, NO production followed. Furthermore, the beginning of NO production coincided with the beginning of the plateau of the initial peak (beginning of the sustained phase) rather than with the earliest onset of the initial peak. This is indeed consistent with the notion that the initial [Ca2+]i peak translocates eNOS from the caveolae, so liberating it to form dimeric complexes, while sustained [Ca2+]i actually maintains the free active eNOS complexes away from the caveolae. This point is however still speculation and would require further testing. Finally, the sustained phase burst response in the P-UA Endo is not only more sustained but more synchronous than that of the NP-UA Endo and the response is sustained in a greater number of cells in P-UA Endo cells than in NP-UA Endo cells (Yi, et al. 2011). Thus while Gap27 based experiments have yet to be performed in intact vessels ex vivo, there is growing evidence to support the case for increased endothelial gap junction function in the pregnant state in vivo.
3.1.4 Relative roles of eNOS expression vs. extent and duration of CCE dependent eNOS activation as determinants of pregnancy induced changes in NO output
It is of course important to recognize that while in studies of NP- and P-UAEC in culture the level of eNOS are similar, in intact vessel endothelium they are not. It is therefore relevant that in both the Yi et al 2005 and 2011 studies, ionomycin treatment was also used as a functional assay for eNOS expression (maximally elevating [Ca2+]i and therefore maximally activating eNOS as an indirect measure of total expression). Such ionomycin treatment was able to elicit a greater NO response in P-UA Endo than NP-UA Endo (Yi, et al. 2005, Yi, et al. 2011), but only to an extent consistent with the previously reported increased eNOS protein expression during pregnancy (Magness, et al. 1997, Bird, et al. 2000). In contrast, ATP stimulated a disproportionately higher level of NO production in P-UA Endo over that observed in NP-UA Endo. This demonstrates that the ability of physiologic agonists to sustain a longer [Ca2+]i response in P-UA Endo is indeed physiologically relevant in turn to achieving the pregnancy adapted increase in NO output, and applies over and above that due to increased eNOS expression alone. Indeed the authors concluded that while the actual NO output of a single cell may be very much influenced by the amount of eNOS expressed, it is the compounding impact of increased duration of [Ca2+]i bursts, the increased number of cells responding, and the increase in eNOS expression per cell that synergize together to bring about the dramatic overall increase and duration of increase in NO output in pregnancy. Furthermore, while the evidence suggests that in vivo this form of [Ca2+]i signaling adaptation during pregnancy is mediated at the level of increased cell-cell communication by CX43, data from UA Endo of luteal phase vs. follicular phase nonpregnant sheep in the same study revealed no changes in [Ca2+]i signaling or cell synchronization was observed, and the modest but significant improvement in NO output seen in the follicular phase was solely due to the slight increase in expression of eNOS that occurs in the follicular phase (Magness, et al. 2001, Yi, et al. 2011). Thus adaptation of the [Ca2+]i signaling response is indeed unique to the physiology of pregnancy rather than the ovarian cycle, and this in turn suggests if control of adaptation has an as yet unidentified endocrine origin, then perhaps factors of placental rather than ovarian origin are responsible. While the studies of uterine vasculature are the most definitive, these observations match those of Mahdy et al who proposed both greater cell recruitment and increased response amplitude in P-HHVE, and so it is clear that while this adaptation is most profound in the uterine vasculature, it may also apply systemically.
Studies of pregnancy adaptive CCE dysfunction and corresponding changes in NO response in experimental models and human disease
4.1 Preeclampsia is associated with altered cell signaling adaptation
Up to this point we have focused mainly on the adaptive response to a healthy pregnancy but further insights are possible when we also consider diseases whereby this adaptive response is apparently lacking. Up to now we have only made passing mention of disorders associated with impaired or failed pregnancy adaptation, most specific of which is preeclampsia. Preeclampsia is a disorder characterized in part by maternal hypertension due to expansion of blood volume but without sufficient increase in blood perfusion through the uteroplacental unit (Sheppard & Khalil. 2010). This failure to divert blood to the uterus is symptomatic of a failure to otherwise lower uterine vascular resistance and is also in part characterized by a failure of an otherwise profound enhancement of uterine artery endothelial vasodilatory function. Preeclampsia is not only of danger to the mother, but is also of danger to the fetus and is common associated with intrauterine growth restriction. An inability of uterine artery endothelial cells to produce enhanced quantities of NO is clearly a hallmark of the insufficient vasodilation characteristic of preeclamptic pregnancies (Sladek, et al. 1997, Roberts & Hubel. 2010), but the more important question, both clinically and mechanistically, is why? Given the evidence that normal pregnancy adapted NO production is mediated by a correspondingly increased sustained phase [Ca2+]i responses in maternal uterine vasculature that is matched in healthy fetal (umbilical) vasculature, then examining exactly if and why this is lacking in dysfunctional pregnancies may be the next step in both understanding pregnancy adaptive CCE mechanisms, and perhaps give us clues as to how to treat such conditions. Comparing the actual function of cells isolated from normal and preeclamptic umbilical cords in otherwise normal culture conditions ex vivo has certainly shown that programmed differences exist in HUVEC cells, just as are observed in HHVE from normal vs preeclamptic pregnancy, and that in preeclamptic subjects the otherwise expected adaptive signaling at the level of sustained CCE is missing in each case (Mahdy, et al. 1998, Steinert, et al. 2002). More recently studies in uterine artery have shown this preeclampsia-like dysfunction can also be reproduced in pregnancy adapted UA Endo by acute treatment using agents known to block CX43 function (Yi, et al. 2011). If we accept the evidence that pregnancy adapted changes in CCE [Ca2+]i signaling are due to changes in CX43 function, and apply it to the lack of ‘adapted’ CCE-like responses in HHVE or HUVEC from preeclamptic subjects, then is it true that Cx43 function fails in preeclampsia, and if so, then how? Is it also the case that adaptation of CX43 function never developed or was it actively suppressed? In the remaining sections we review these questions in more detail.
4.2 Known consequences of preeclampsia on HHVE and HUVEC function
The Mahdy et al study on HHVE elegantly described [Ca2+]i signaling changes between the pregnant and nonpregnant states, but also investigated the nature of the [Ca2+]i response to various agonists in cells from preeclamptic mothers (PE-HHVE, 36 weeks gestation) (Mahdy, et al. 1998). In response to ATP and histamine, both peak and plateau response amplitudes in PE-HHVE were significantly lower than in P-HHVE and indistinguishable from NP-HHVE. There was also no longer any difference in percentage of cells responding between these groups. Bradykinin induced a significantly lower percentage of PE-HHVE cells to respond when compared to P-HHVE, and was now equivalent to that of NP-HHVE. These studies show clearly that even in the systemic circulation, where pregnancy mediated vasodilation is comparatively modest, preeclamptic endothelial cells respond to [Ca2+]i mobilizing agonists more like NP-HHVE than P-HHVE (Mahdy, et al. 1998). Again, these agonist stimulations were less than 5 minutes in duration, thus only taking into account the onset of the sustained CCE [Ca2+]i response. Nonetheless, dysfunction is clearly occurring during the CCE phase of the [Ca2+]i response, is maintained in otherwise normal culture, and occurs at the level of adaptive cell signaling, either as a failure of or self-imposed suppression of programmed adaptive function.
While the literature on HHVE is limited, it is of particular value in setting reference points for comparison of observations in HUVEC of normal vs preeclamptic subjects (PE-HUVEC). In addition to the findings in healthy pregnancy derived HUVEC above, Steinert et al (Steinert, et al. 2002) also showed that while the initial peak amplitude of the histamine stimulated [Ca2+]i response is identical in cells derived from normal and preeclamptic cords, the plateau CCE phase is significantly depressed in PE-HUVEC when compared to normal. This was confirmed to be the result of altered CCE Ca2+ influx from extracellular sources, since histamine treatment in the presence of a Ca2+-free buffer produces a reduced sustained phase initial peak which quickly returns to basal levels in both normal and PE-HUVEC, but when Ca2+ is returned to the media the resultant CCE [Ca2+]i overshoot response is less robust in the PE-HUVEC. The rate of Ca2+ influx, the peak amplitude after Ca2+ addition, and plateau amplitude after Ca2+ addition are all reduced in PE-HUVEC when compared to those derived from normal pregnancies. Although specific initial peak amplitude analysis in HHVE was only undertaken for ATP as an agonist, the histamine response amplitude in normal vs preeclamptic derived cells is consistent between HHVE and HUVEC (Mahdy, et al. 1998, Steinert, et al. 2002). The HUVEC data also clearly points to dysfunction in preeclamptic [Ca2+]i signaling being a matter of reduced sustained phase [Ca2+]i responsiveness through reduced CCE response (Steinert, et al. 2002).
4.3 Artificial induction of preeclampsia like dysfunction in ovine UA endothelium by suppression of CX43 function
While studies in sheep allow parallel comparison of the nonpregnant and pregnant state, one issue is that there is no natural condition or single model which actually replicates all the symptoms of preeclampsia. It is perhaps not surprising that a natural condition has not been reported since sheep that are inefficient breeders are simply not maintained by herd owners, so there are negative selection pressures constantly imposed to eliminate preeclampsia-like conditions. Nonetheless this is the model in which the strongest mechanistic understanding for normal pregnancy adaptation has been derived and it centers on the proposal that pregnancy adaptation occurs through an increase in CX43 gap junction function to thereby facilitate the CCE response. One would expect in turn that inhibitors of CX43 function, either by closing the channel through inhibitory phosphorylation, or removing it from the plasma membrane to prevent function, would be expected to invoke failed adaptation through active suppression.
4.3.1 Cellular mechanisms through which CX43 function may be dysregulated
The two physiologic factors that are most clearly associated with preeclampsia and could act to inhibit CX43 function are VEGF-165 and TNF-alpha. Treatment of endothelial cells with VEGF-165 is thought to phosphorylate CX43 through the activation of PKC and/or ERK, which would correspond to positions 262, 368, and 279/282 (reviewed in Suarez & Ballmer-Hofer. 2001, Solan & Lampe. 2009) and so functionally close the gap junctions. Conversely TNF-alpha is known to act through different signaling pathways to promote CX43 closure and even internalization of CX43, so removing CX43 from its functional plasma membrane location and even reducing its expression (Van Rijen, et al. 1998, Vandamme, et al. 2004). Either way, CX43 function is impaired and one would predict treatment of P-UA Endo or P-UAEC to promote such inhibition of CX43 function would in turn induce a nonpregnant like CCE response. While studies of the actions of such agents are incomplete, there is compelling evidence that both VEGF-165 and TNF-alpha may indeed both negatively regulate otherwise normal pregnancy adapted signaling function.
4.3.2 VEGF-165 as a potential negative regulator of CCE
When intact uterine arteries are pretreated ex vivo with VEGF-165 before subsequent ATP addition, the resultant [Ca2+]i bursts in P-UA Endo are indeed reduced to levels equivalent to those of NP-UA Endo (Yi, et al. 2011). Like the histamine treated HUVEC from normal and preeclamptic pregnancies, VEGF-165 pretreatment selectively inhibits the sustained phase [Ca2+]i response, without producing as significant a change in initial peak amplitude. This selective inhibition of sustained CCE phase [Ca2+]i response by VEGF-165 is exactly what would be predicted for a blockage of CX43 gap junction function, as shown by the Gap27 studies in UAEC (Yi, et al. 2010a). Once again, cause and effect is also established given that treatment of pregnancy adapted intact UA vessels ex vivo with VEGF-165 for just 30 minutes also results in UA Endo NO response (detected by change in DAF fluorescence) being reduced down to the levels of vessels from unadapted nonpregnant ewes (Yi, et al. 2011). Thus, a physiologic agonist known to be elevated locally and thought by some to be elevated systemically in conditions such as preeclampsia (Hayman, et al. 1999, Soleymanlou, et al. 2005, Bosco, et al. 2010, Hertig & Liere. 2010), can also bring about a preeclamptic-like suppression in sustained phase [Ca2+]i CCE response and so severely inhibit pregnancy adapted NO production in intact uterine artery endothelial tissue. It should be noted that VEGF-165 is capable of promoting its own [Ca2+]i response and therefore is also capable of inducing NO production (Yi, et al. 2011). However, as Yi et al show, this response is small in terms of immediate [Ca2+]i and NO responses, and is far from being able to offset the inhibition of any subsequent ATP induced [Ca2+]i or NO response (Yi, et al. 2011). Essentially, VEGF-165 has shut down the sustained response to G protein coupled receptors such as P2Y2 that activate PLC-beta and the associated TRPC/IP3R mediated CCE response, and while VEGF has otherwise taken control, it is a poor substitute. The question now is how this occurs. Given the literature on the role of PKC and ERK as negative regulators of CX43 function, if VEGF-165 is acting through these pathways then pharmacologic agents activating PKC and/or ERK would be predicted to also replicate the acute inhibitory effect of VEGF-165. Treatment with TPA certainly produces similar inhibitory results on CCE responses in P-UAEC (Cale & Bird. 2006) consistent with its known inhibition of CX43 gap junction function by way of phosphorylation through PKC and/or ERK pathways in other cells (above). It remains to be seen if the inhibitory action of VEGF-165 does indeed result in CX43 phosphorylation at positions that are clearly associated with inhibition of function, and further if this action of VEGF-165 can be reversed by blockers of the PKC and/or ERK pathways.
4.3.3 TNF-alpha as a potential negative regulator of CCE
While TNF-alpha is known to promote internalization of connexin proteins in other cell models (above), the direct study of this in pregnancy adapted tissues has not yet been undertaken. Elevated TNF-alpha levels are clearly associated with preeclamptic pregnancies (Anim-Nyame, et al. 2003) and studies in blood-brain barrier endothelial cells at least have shown TNF-alpha can block sustained [Ca2+]i responses by blocking gap junction function (Vandamme, et al. 2004). Like VEGF-165, this is thought in part to be mediated by connexin phosphorylation through PKC and ERK signaling pathways, but further studies in HUVEC also implicate TNF-alpha in altering connexin expression and even relocalization into the perinuclear region (van Rijen, et al. 1998). These areas are clearly understudied in HHVE, UAEC and HUVEC with respect to pregnancy adaptation and dysfunctional (preeclamptic) pregnancies, and future studies are clearly justified to assess the impacts of this inflammatory cytokine on the pregnancy adapted sustained phase [Ca2+]i response both alone and in combination with agents such as VEGF-165. Such studies in particular may be of considerable value, not only in identifying additional key regulatory pathways that may destabilize the otherwise upregulated state of CX43 function that underlies normal pregnancy adapted endothelial CCE function, but may also lay a foundation for new strategies for treatment of failed adaptation as is seen in inflammatory conditions including preeclampsia.
Conclusions
5.1 Summary
Numerous studies in HHVE, UAEC and HUVEC have clearly established that pregnancy adaptation of endothelial NO production is in large part an adaptive signaling phenomenon that is programmed at the functional level of CCE [Ca2+]i signaling, most likely mediated by an IP3R/TRPC interaction at the plasma membrane and is under the control of increased gap junction communication. Given that this adaptation of CCE is a rewiring of the cell itself at the level of the plasma membrane CCE signaling equipment at a post receptor level rather than a change in the individual hormone receptors themselves, its impact is to globally alter the response to all agonists that can evoke this form of TRPC/IP3R associated CCE response. For the cell to fully demonstrate enhanced CCE it is necessary for cells to be coupled through gap junctions, particularly of type CX43. While the exact coupling mechanism of CX43 function to increased IP3R2/TRPC3 association that mediates CCE is unknown, dramatic increases in CCE occur both in the form of more sustained CCE bursts per cell, and through recruitment of more cells to the response. The overwhelming evidence is the change in CCE and increase in NO is casually linked. While increases in eNOS expression during pregnancy may contribute in part to the overall increase in NO response, the dramatic increases in NO output both in magnitude and duration observed in intact vessels is at least as much again due to pregnancy adaptation of CCE signaling per cell and the number of cells responding, if not more so. Just as such adaptation at the level of cell signaling is a normal part of pregnancy, so its failure is associated with diseased pregnancy. At least two known factors associated with diseased pregnancy and known to inhibit CX43 mediated cell-cell communication through the PKC and/or ERK pathway are also capable of closing down pregnancy adapted signaling and blunting eNOS activation to nonpregnant levels in uterine vasculature.
5.2 Future questions
While many advances have been made, there are still many questions left to answer. Whether endothelial dysfunction associated with preeclampsia in particular results from a lack of adaptation, or is caused by a suppression of an adapted response by presumed local or circulating factor(s) is not clear for a number of reasons related to the nature of the vascular and endothelial cell models studied to date. Although of less relevance above, in vitro treatment of endothelial cells from otherwise healthy animal or human subjects with serum or serum components from preeclamptic subjects has been undertaken and been shown to induce dysfunction in otherwise healthy cells of isolated vessels (see for instance Hayman, et al. 2000, Wang, et al. 2002a, Zhang, et al. 2003). Such studies starting with normal pregnancy adapted cells do indeed indicate circulating factors are capable of tonically suppressing the effect on pregnancy adapted cell function and indeed it is highly likely among these factors are hormones that are or act like VEGF-165 on intact P-UA vessels or possibly TNF-alpha on blood brain barrier endothelial cells. Nonetheless the findings are also limited when one also recognizes that results vary according to the actual cells used for functional assays (Wellings, et al. 1998). Perhaps more relevant is the finding that even in cells maintained in normal serum conditions, cells from preeclamptic subjects still show dysfunction which is programmed to be ongoing, i.e. is maintained in a manner more dependent on the cells origin, than serum or acute treatment conditions used in culture (in addition to those cited above see for example (Wang, et al. 2002b) regarding changes in endothelial permeability). Thus while some degree of suppression of pregnancy adapted vascular endothelial function may indeed be induced by blood borne factors elevated in preeclamptic subjects in late pregnancy, and this may well contribute to the severity of late stage disease, an underlying lack of adaptive programing has also likely occurred long before that time, and is of equal if not greater relevance. Clearly further studies are needed and while no one approach (study of normal pregnancy adaptation, study of factors that interfere with normal pregnancy adaptation, or study of disease related dysfunction) is sufficient in itself, a combination of such approaches will allow us to appreciate more fully the underlying mechanism of pregnancy adaptation of CCE [Ca2+]i signaling due to changes in CX43 function, and how it is achieved, as well as how it may fail.
Further questions for immediate study include how changes in CX43 function are communicated to TRPC3 opening. Is it simply a factor transported by CX43 such as Ins(1,4,5)P3 or indeed Ca2+ itself, or is it an electric field effect resulting from coupling cells into an electric ‘array’? Is there in fact another mediator such as a signaling protein between them or are we instead seeing the result of a subtle change in ion channel activity in response to CX43 coupling of groups of cells that thereby alters opening probability of TRPC3? Is TRPC3 the only channel allowing Ca2+ entry and if not, does the isoform involved change with time? While not definitively conclusive, studies of differences of Gd3+ transport into HUVEC of normal vs. preeclamptic subjects suggest perhaps TRPC3 is not always the only channel involved (Steinert, et al. 2002). Are the spatial distributions of these interacting proteins in the cell plasma membrane altered both in absolute and relative terms by pregnancy? How do these proteins change with regard to expression and/or relative proximity when adaptation is functionally lacking such in preeclampsia? Additional approaches utilizing shear stress application to the cell models discussed herein could also be of further physiological relevance. Shear stress is known to stimulate [Ca2+]i and NO responses in endothelial cells, although the exact role shear-induced [Ca2+]i plays in eNOS activation remains controversial (Ayajiki, et al. 1996). Nonetheless, shear stress has the added ability to alter cell morphology through cytoskeletal arrangement, resulting in cells aligned in the direction of flow (Wechezak, et al. 1985). Does such alignment also have effects on cell function and coordination through gap junctions?
In terms of future therapy, screening of substances that either induce pregnancy like functional adaptation in nonpregnant subjects or conversely impair pregnancy adapted function down to nonpregnant/dysfunctional preeclamptic levels would be of value. Once we have a more complete understanding from all combined approaches we will we be able to answer the question of what exactly pregnancy adaptation of CCE [Ca2+]i signaling is, and if its absence in cells from preeclamptic subjects is due to failed adaptation or suppressed adaptation. We may also along the way identify unique and novel strategies that could not only assist treatment of preeclampsia by restoring normal endothelial function, but perhaps also improve vascular function in nonpregnant women and indeed men who are otherwise moving towards hypertension. Given our increasingly aging population this may be the most valuable outcome of future work in this field.
Acknowledgments
This work was funded in part by grants NIH HL079020, and HD38843. This work was also undertaken in partial fulfillment of the PhD in Endocrinology and Reproductive Physiology of DSB who was also funded by T32HD41921, and is currently supported by a Shapiro Predoctoral Award from UW Madison School Medicine and Public Health.
References
- Anim-Nyame N, Gamble J, Sooranna SR, Johnson MR, Steer PJ. Microvascular permeability is related to circulating levels of tumour necrosis factor-alpha in pre-eclampsia. Cardiovascular research. 2003;58:162–169. doi: 10.1016/s0008-6363(02)00844-1. [DOI] [PubMed] [Google Scholar]
- Ayajiki K, Kindermann M, Hecker M, Fleming I, Busse R. Intracellular pH and tyrosine phosphorylation but not calcium determine shear stress-induced nitric oxide production in native endothelial cells. Circulation research. 1996;78:750–758. doi: 10.1161/01.res.78.5.750. [DOI] [PubMed] [Google Scholar]
- Bhattacharya R, Kwon J, Li X, Wang E, Patra S, Bida JP, Bajzer Z, Claesson-Welsh L, Mukhopadhyay D. Distinct role of PLCbeta3 in VEGF-mediated directional migration and vascular sprouting. Journal of cell science. 2009;122:1025–1034. doi: 10.1242/jcs.041913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird IM, Zhang L, Magness RR. Possible mechanisms underlying pregnancy-induced changes in uterine artery endothelial function. American journal of physiology. Regulatory, integrative and comparative physiology. 2003;284:R245–58. doi: 10.1152/ajpregu.00108.2002. [DOI] [PubMed] [Google Scholar]
- Bird IM, Sullivan JA, Di T, Cale JM, Zhang L, Zheng J, Magness RR. Pregnancy-dependent changes in cell signaling underlie changes in differential control of vasodilator production in uterine artery endothelial cells. Endocrinology. 2000;141:1107–1117. doi: 10.1210/endo.141.3.7367. [DOI] [PubMed] [Google Scholar]
- Bosco C, Buffet C, Diaz E, Rodrigo R, Morales P, Barja P, Terra R, Parra-Cordero M. VEGF in the muscular layer of placental blood vessels: Immuno-expression in preeclampsia and intrauterine growth restriction and its association with the antioxidant status. Cardiovascular & hematological agents in medicinal chemistry. 2010;8:87–95. doi: 10.2174/187152510791170951. [DOI] [PubMed] [Google Scholar]
- Cale JM, Bird IM. Dissociation of endothelial nitric oxide synthase phosphorylation and activity in uterine artery endothelial cells. 2006;290:H1433–H1445. doi: 10.1152/ajpheart.00942.2005. [DOI] [PubMed] [Google Scholar]
- Di T, Sullivan JA, Magness RR, Zhang L, Bird IM. Pregnancy-specific enhancement of agonist-stimulated ERK-1/2 signaling in uterine artery endothelial cells increases ca(2+) sensitivity of endothelial nitric oxide synthase as well as cytosolic phospholipase A(2) Endocrinology. 2001;142:3014–3026. doi: 10.1210/endo.142.7.8278. [DOI] [PubMed] [Google Scholar]
- Dimmeler S, Fleming I, Fisslthaler B, Hermann C, Busse R, Zeiher AM. Activation of nitric oxide synthase in endothelial cells by akt-dependent phosphorylation. Nature. 1999;399:601–605. doi: 10.1038/21224. [DOI] [PubMed] [Google Scholar]
- Dudzinski DM, Michel T. Life history of eNOS: Partners and pathways. Cardiovascular research. 2007;75:247–260. doi: 10.1016/j.cardiores.2007.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esper RJ, Nordaby RA, Vilarino JO, Paragano A, Cacharron JL, Machado RA. Endothelial dysfunction: A comprehensive appraisal. Cardiovascular diabetology. 2006;5:4. doi: 10.1186/1475-2840-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans WH, Boitano S. Connexin mimetic peptides: Specific inhibitors of gap-junctional intercellular communication. Biochemical Society transactions. 2001;29:606–612. doi: 10.1042/bst0290606. [DOI] [PubMed] [Google Scholar]
- Fleming I, Fisslthaler B, Dimmeler S, Kemp BE, Busse R. Phosphorylation of thr(495) regulates ca(2+)/calmodulin-dependent endothelial nitric oxide synthase activity. Circulation research. 2001;88:E68–75. doi: 10.1161/hh1101.092677. [DOI] [PubMed] [Google Scholar]
- Garcia-Cardena G, Fan R, Stern DF, Liu J, Sessa WC. Endothelial nitric oxide synthase is regulated by tyrosine phosphorylation and interacts with caveolin-1. The Journal of biological chemistry. 1996;271:27237–27240. doi: 10.1074/jbc.271.44.27237. [DOI] [PubMed] [Google Scholar]
- Gifford SM, Yi FX, Bird IM. Pregnancy-enhanced Ca2+ responses to ATP in uterine artery endothelial cells is due to greater capacitative Ca2+ entry rather than altered receptor coupling. The Journal of endocrinology. 2006a;190:373–384. doi: 10.1677/joe.1.06635. [DOI] [PubMed] [Google Scholar]
- Gifford SM, Yi FX, Bird IM. Pregnancy-enhanced store-operated Ca2+ channel function in uterine artery endothelial cells is associated with enhanced agonist-specific transient receptor potential channel 3-inositol 1,4,5-trisphosphate receptor 2 interaction. The Journal of endocrinology. 2006b;190:385–395. doi: 10.1677/joe.1.06773. [DOI] [PubMed] [Google Scholar]
- Gifford SM, Cale JM, Tsoi S, Magness RR, Bird IM. Pregnancy-specific changes in uterine artery endothelial cell signaling in vivo are both programmed and retained in primary culture. Endocrinology. 2003;144:3639–3650. doi: 10.1210/en.2002-0006. [DOI] [PubMed] [Google Scholar]
- Gifford SM, Grummer MA, Pierre SA, Austin JL, Zheng J, Bird IM. Functional characterization of HUVEC-CS: Ca2+ signaling, ERK 1/2 activation, mitogenesis and vasodilator production. The Journal of endocrinology. 2004;182:485–499. doi: 10.1677/joe.0.1820485. [DOI] [PubMed] [Google Scholar]
- Groschner K, Hingel S, Lintschinger B, Balzer M, Romanin C, Zhu X, Schreibmayer W. Trp proteins form store-operated cation channels in human vascular endothelial cells. FEBS letters. 1998;437:101–106. doi: 10.1016/s0014-5793(98)01212-5. [DOI] [PubMed] [Google Scholar]
- Grummer MA, Sullivan JA, Magness RR, Bird IM. Vascular endothelial growth factor acts through novel, pregnancy-enhanced receptor signalling pathways to stimulate endothelial nitric oxide synthase activity in uterine artery endothelial cells. The Biochemical journal. 2009;417:501–511. doi: 10.1042/BJ20081013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayman R, Warren A, Brockelsby J, Johnson I, Baker P. Plasma from women with pre-eclampsia induces an in vitro alteration in the endothelium-dependent behaviour of myometrial resistance arteries. BJOG: an international journal of obstetrics and gynaecology. 2000;107:108–115. doi: 10.1111/j.1471-0528.2000.tb11586.x. [DOI] [PubMed] [Google Scholar]
- Hayman R, Brockelsby J, Kenny L, Baker P. Preeclampsia: The endothelium, circulating factor(s) and vascular endothelial growth factor. Journal of the Society for Gynecologic Investigation. 1999;6:3–10. [PubMed] [Google Scholar]
- Haynes MP, Sinha D, Russell KS, Collinge M, Fulton D, Morales-Ruiz M, Sessa WC, Bender JR. Membrane estrogen receptor engagement activates endothelial nitric oxide synthase via the PI3-kinase-akt pathway in human endothelial cells. Circulation research. 2000;87:677–682. doi: 10.1161/01.res.87.8.677. [DOI] [PubMed] [Google Scholar]
- Hertig A, Liere P. New markers in preeclampsia. Clinica chimica acta; international journal of clinical chemistry. 2010;411:1591–1595. doi: 10.1016/j.cca.2010.07.020. [DOI] [PubMed] [Google Scholar]
- Hu Q, Yu ZX, Ferrans VJ, Takeda K, Irani K, Ziegelstein RC. Critical role of NADPH oxidase-derived reactive oxygen species in generating Ca2+ oscillations in human aortic endothelial cells stimulated by histamine. The Journal of biological chemistry. 2002;277:32546–32551. doi: 10.1074/jbc.M201550200. [DOI] [PubMed] [Google Scholar]
- Huang PL, Huang Z, Mashimo H, Bloch KD, Moskowitz MA, Bevan JA, Fishman MC. Hypertension in mice lacking the gene for endothelial nitric oxide synthase. Nature. 1995;377:239–242. doi: 10.1038/377239a0. [DOI] [PubMed] [Google Scholar]
- Lampe PD, Lau AF. The effects of connexin phosphorylation on gap junctional communication. The international journal of biochemistry & cell biology. 2004;36:1171–1186. doi: 10.1016/S1357-2725(03)00264-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lampe PD, Lau AF. Regulation of gap junctions by phosphorylation of connexins. Archives of Biochemistry and Biophysics. 2000;384:205–215. doi: 10.1006/abbi.2000.2131. [DOI] [PubMed] [Google Scholar]
- Lin S, Fagan KA, Li KX, Shaul PW, Cooper DM, Rodman DM. Sustained endothelial nitric-oxide synthase activation requires capacitative Ca2+ entry. The Journal of biological chemistry. 2000;275:17979–17985. doi: 10.1074/jbc.275.24.17979. [DOI] [PubMed] [Google Scholar]
- Magness RR, Sullivan JA, Li Y, Phernetton TM, Bird IM. Endothelial vasodilator production by uterine and systemic arteries. VI. ovarian and pregnancy effects on eNOS and NO(x) American journal of physiology. Heart and circulatory physiology. 2001;280:H1692–8. doi: 10.1152/ajpheart.2001.280.4.H1692. [DOI] [PubMed] [Google Scholar]
- Magness RR, Shaw CE, Phernetton TM, Zheng J, Bird IM. Endothelial vasodilator production by uterine and systemic arteries. II. pregnancy effects on NO synthase expression. The American Journal of Physiology. 1997;272:H1730–40. doi: 10.1152/ajpheart.1997.272.4.H1730. [DOI] [PubMed] [Google Scholar]
- Mahdy Z, Otun HA, Dunlop W, Gillespie JI. The responsiveness of isolated human hand vein endothelial cells in normal pregnancy and in pre-eclampsia. The Journal of physiology. 1998;508(Pt 2):609–617. doi: 10.1111/j.1469-7793.1998.00609.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan AJ, Jacob R. Differential modulation of the phases of a Ca2+ spike by the store Ca2+-ATPase in human umbilical vein endothelial cells. The Journal of physiology. 1998;513(Pt 1):83–101. doi: 10.1111/j.1469-7793.1998.083by.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rees DD, Palmer RM, Moncada S. Role of endothelium-derived nitric oxide in the regulation of blood pressure. Proceedings of the National Academy of Sciences of the United States of America. 1989;86:3375–3378. doi: 10.1073/pnas.86.9.3375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts JM, Hubel CA. Pregnancy: A screening test for later life cardiovascular disease. Women’s health issues: official publication of the Jacobs Institute of Women’s Health. 2010;20:304–307. doi: 10.1016/j.whi.2010.05.004. [DOI] [PubMed] [Google Scholar]
- Rosenfeld CR, Gant NF., Jr The chronically instrumental ewe: A model for studying vascular reactivity to angiotensin II in pregnancy. The Journal of clinical investigation. 1981;67:486–492. doi: 10.1172/JCI110057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saez JC, Berthoud VM, Branes MC, Martinez AD, Beyer EC. Plasma membrane channels formed by connexins: Their regulation and functions. Physiological Reviews. 2003;83:1359–1400. doi: 10.1152/physrev.00007.2003. [DOI] [PubMed] [Google Scholar]
- Sheppard SJ, Khalil RA. Risk factors and mediators of the vascular dysfunction associated with hypertension in pregnancy. Cardiovascular & hematological disorders drug targets. 2010;10:33–52. doi: 10.2174/187152910790780096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shesely EG, Maeda N, Kim HS, Desai KM, Krege JH, Laubach VE, Sherman PA, Sessa WC, Smithies O. Elevated blood pressures in mice lacking endothelial nitric oxide synthase. Proceedings of the National Academy of Sciences of the United States of America. 1996;93:13176–13181. doi: 10.1073/pnas.93.23.13176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirnes S, Kjenseth A, Leithe E, Rivedal E. Interplay between PKC and the MAP kinase pathway in Connexin43 phosphorylation and inhibition of gap junction intercellular communication. Biochemical and biophysical research communications. 2009;382:41–45. doi: 10.1016/j.bbrc.2009.02.141. [DOI] [PubMed] [Google Scholar]
- Sladek SM, Magness RR, Conrad KP. Nitric oxide and pregnancy. The American Journal of Physiology. 1997;272:R441–63. doi: 10.1152/ajpregu.1997.272.2.R441. [DOI] [PubMed] [Google Scholar]
- Solan JL, Lampe PD. Connexin43 phosphorylation: Structural changes and biological effects. The Biochemical journal. 2009;419:261–272. doi: 10.1042/BJ20082319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soleymanlou N, Jurisica I, Nevo O, Ietta F, Zhang X, Zamudio S, Post M, Caniggia I. Molecular evidence of placental hypoxia in preeclampsia. The Journal of clinical endocrinology and metabolism. 2005;90:4299–4308. doi: 10.1210/jc.2005-0078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinert JR, Wyatt AW, Poston L, Jacob R, Mann GE. Preeclampsia is associated with altered Ca2+ regulation and NO production in human fetal venous endothelial cells. The FASEB journal: official publication of the Federation of American Societies for Experimental Biology. 2002;16:721–723. doi: 10.1096/fj.01-0916fje. [DOI] [PubMed] [Google Scholar]
- Suarez S, Ballmer-Hofer K. VEGF transiently disrupts gap junctional communication in endothelial cells. Journal of cell science. 2001;114:1229–1235. doi: 10.1242/jcs.114.6.1229. [DOI] [PubMed] [Google Scholar]
- Sullivan JA, Grummer MA, Yi FX, Bird IM. Pregnancy-enhanced endothelial nitric oxide synthase (eNOS) activation in uterine artery endothelial cells shows altered sensitivity to Ca2+, U0126, and wortmannin but not LY294002--evidence that pregnancy adaptation of eNOS activation occurs at multiple levels of cell signaling. Endocrinology. 2006;147:2442–2457. doi: 10.1210/en.2005-0399. [DOI] [PubMed] [Google Scholar]
- Tanaka N, Kawasaki K, Nejime N, Kubota Y, Nakamura K, Kunitomo M, Takahashi K, Hashimoto M, Shinozuka K. P2Y receptor-mediated ca(2+) signaling increases human vascular endothelial cell permeability. Journal of pharmacological sciences. 2004;95:174–180. doi: 10.1254/jphs.fpj03036x. [DOI] [PubMed] [Google Scholar]
- Tran QK, Leonard J, Black DJ, Nadeau OW, Boulatnikov IG, Persechini A. Effects of combined phosphorylation at ser-617 and ser-1179 in endothelial nitric-oxide synthase on EC50(Ca2+) values for calmodulin binding and enzyme activation. The Journal of biological chemistry. 2009;284:11892–11899. doi: 10.1074/jbc.M806205200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trebak M, Vazquez G, Bird GS, Putney JW., Jr The TRPC3/6/7 subfamily of cation channels. Cell calcium. 2003;33:451–461. doi: 10.1016/s0143-4160(03)00056-3. [DOI] [PubMed] [Google Scholar]
- Van Rijen H, van Kempen MJ, Analbers LJ, Rook MB, van Ginneken AC, Gros D, Jongsma HJ. Gap junctions in human umbilical cord endothelial cells contain multiple connexins. The American Journal of Physiology. 1997;272:C117–30. doi: 10.1152/ajpcell.1997.272.1.C117. [DOI] [PubMed] [Google Scholar]
- Van Rijen HV, van Kempen MJ, Postma S, Jongsma HJ. Tumour necrosis factor alpha alters the expression of connexin43, connexin40, and connexin37 in human umbilical vein endothelial cells. Cytokine. 1998;10:258–264. doi: 10.1006/cyto.1997.0287. [DOI] [PubMed] [Google Scholar]
- Van Vliet BN, Chafe LL, Montani JP. Characteristics of 24 h telemetered blood pressure in eNOS-knockout and C57Bl/6J control mice. The Journal of physiology. 2003;549:313–325. doi: 10.1113/jphysiol.2003.041897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandamme W, Braet K, Cabooter L, Leybaert L. Tumour necrosis factor alpha inhibits purinergic calcium signalling in blood-brain barrier endothelial cells. Journal of neurochemistry. 2004;88:411–421. doi: 10.1046/j.1471-4159.2003.02163.x. [DOI] [PubMed] [Google Scholar]
- Versari D, Daghini E, Virdis A, Ghiadoni L, Taddei S. Endothelium-dependent contractions and endothelial dysfunction in human hypertension. British journal of pharmacology. 2009;157:527–536. doi: 10.1111/j.1476-5381.2009.00240.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X, Athayde N, Trudinger B. Endothelial cell expression of adhesion molecules is induced by fetal plasma from pregnancies with umbilical placental vascular disease. BJOG: an international journal of obstetrics and gynaecology. 2002a;109:770–777. doi: 10.1111/j.1471-0528.2002.01240.x. [DOI] [PubMed] [Google Scholar]
- Wang Y, Gu Y, Granger DN, Roberts JM, Alexander JS. Endothelial junctional protein redistribution and increased monolayer permeability in human umbilical vein endothelial cells isolated during preeclampsia. American Journal of Obstetrics and Gynecology. 2002b;186:214–220. doi: 10.1067/mob.2002.119638. [DOI] [PubMed] [Google Scholar]
- Warn-Cramer BJ, Lampe PD, Kurata WE, Kanemitsu MY, Loo LW, Eckhart W, Lau AF. Characterization of the mitogen-activated protein kinase phosphorylation sites on the connexin-43 gap junction protein. The Journal of biological chemistry. 1996;271:3779–3786. doi: 10.1074/jbc.271.7.3779. [DOI] [PubMed] [Google Scholar]
- Wechezak AR, Viggers RF, Sauvage LR. Fibronectin and F-actin redistribution in cultured endothelial cells exposed to shear stress. Laboratory investigation; a journal of technical methods and pathology. 1985;53:639–647. [PubMed] [Google Scholar]
- Wellings RP, Brockelsby JC, Baker PN. Activation of endothelial cells by plasma from women with preeclampsia: Differential effects on four endothelial cell types. Journal of the Society for Gynecologic Investigation. 1998;5:31–37. doi: 10.1016/s1071-5576(97)00100-7. [DOI] [PubMed] [Google Scholar]
- Yi FX, Boeldt DS, Bird IM. Pregnancy induced reprogramming of endothelial function in response to ATP: Evidence for post receptor Ca2+ signaling plasticity. In: Gerasimovskaya, Kaczmarek E, editors. Extracellular ATP and Adensosine as the Regulators of Endothelial Cell Function. Springer Publications; 2010b. pp. 197–213E. [Google Scholar]
- Yi F, Boeldt DS, Magness RR, Bird IM. Ca2+]i signaling vs eNOS expression as determinants of NO output in uterine artery endothelium: Relative roles in pregnancy adaptation and reversal by VEGF165. American journal of physiology. Heart and circulatory physiology. 2011 doi: 10.1152/ajpheart.01108.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi FX, Magness RR, Bird IM. Simultaneous imaging of [Ca2+]i and intracellular NO production in freshly isolated uterine artery endothelial cells: Effects of ovarian cycle and pregnancy. American journal of physiology. Regulatory, integrative and comparative physiology. 2005;288:R140–8. doi: 10.1152/ajpregu.00302.2004. [DOI] [PubMed] [Google Scholar]
- Yi FX, Boeldt DS, Gifford SM, Sullivan JA, Grummer MA, Magness RR, Bird IM. Pregnancy enhances sustained Ca2+ bursts and endothelial nitric oxide synthase activation in ovine uterine artery endothelial cells through increased connexin 43 function. Biology of reproduction. 2010a;82:66–75. doi: 10.1095/biolreprod.109.078253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Gu Y, Li H, Lucas MJ, Wang Y. Increased endothelial monolayer permeability is induced by serum from women with preeclampsia but not by serum from women with normal pregnancy or that are not pregnant. Hypertension in pregnancy: official journal of the International Society for the Study of Hypertension in Pregnancy. 2003;22:99–108. doi: 10.1081/PRG-120017008. [DOI] [PubMed] [Google Scholar]