Abstract
Purpose
The aim of this study was to explore the psychosocial impact of standing devices as experienced by users.
Method
This is the second part of a comprehensive survey in five counties in Sweden where all the subjects with standing devices were invited to participate. The impact of standing devices on functional independence, quality of life and wellbeing was assessed using a questionnaire, Psychosocial Impact of Assistive Devices Scale (PIADS).
Results
The psychosocial impact of the standing devices was perceived as positive. The highest PIADS scores in relation to age were found in the oldest group, aged 65 years and older. The ability to walk and independence in ambulation resulted in higher scores than the use of a wheelchair and/or dependence on others. Those who stood often awarded higher scores in the PIADS questionnaire compared to those who used the device less frequently. When standing was integrated in various activities, its psychosocial impact received high scores.
Conclusion
The psychosocial impact of standing devices was generally experienced positively. The main results indicated that standing in a standing device had a value and we as professionals should ask the users about the intended purpose of their standing in order to prescribe the optimal device.
Implications for Rehabilitation
Standing in standing devices has positive psychosocial impact for the user.
As professionals we should broaden our view of the use of standing devices, i.e. to see the standing device as an aid that not only treats the body’s structures or improves the user’s abilities in activities, but also provides a psychosocial impact on the user’s daily life, and to find meaningful goals for the user from a psychosocial perspective.
Keywords: Assistive devices, disability, prolonged standing, wellbeing
Introduction
The World Health Organization (WHO) published the International Classification of Disability and Health (ICF), which is a system to group and describe how a person is functioning in the environment based on a bio-psycho-social model. According to the ICF an assistive device is described as an environmental factor which can either facilitate or inhibit a person’s participation and activities. Thus assistive devices are aimed at improving the functioning for disabled persons as stated in ICF [1].
The use of an assistive device can promote a person’s quality of life (QoL) by increasing his/her sense of competence, confidence and motivation to exploit the possibilities in their life [2]. The use may provide opportunities by reducing difficulties in activities and decreasing dependence on others, and includes a broader psychosocial impact on a person’s perceived QoL [3–5]. QoL is dynamic and changing over time and over a person’s life and is experienced differently by different individuals, but the components are the same [2]. Renwick [6] defines QOL as “the effect of the device on the degree to which a person enjoys the important possibilities of his/her life” (p. 35). Personal factors such as age, social habits and roles, and past and current experiences can be barriers to or facilitators of the use of assistive devices and personal factors can also influence the user’s QoL [7]. Psychosocial and cultural aspects, including the person’s adaption to the disability in question, influence the meaning which the device holds for the person and whether the device will be used or not [8].
Use of a standing device can develop persons’ everyday activities in particular and according to Nordström et al. [9] the users of standing devices experienced that standing created freedom to perform activities and facilitated participation. The use of a standing device can also be part in treatment of bodily structures and prolonged standing may have beneficial effects on various bodily functions and structures [10,11], which in turn may affect the participation in activities in a positive way. The upright body position also allows communication on equal terms for persons with disabilities [9,12]. Standing devices in the present study follow the international classification and terminology ISO 9999 [13] comprising tilt tables, standing frames, standing frames with rear wheels, standing wheelchairs and standing shells. A previous study (in press 2013) [14] showed that the standing devices were frequently used and the users experienced an increased QoL. However, the non-respond rate of 42% may indicate that the users were dissatisfied with the device or that the device was not used at all. The experiences of increased QoL is consistent with Arva et al. [12] who concluded that standing enables participation in activities of daily living and that the upright position could promote the persons self-esteem and social interaction with other people [12,15]. The usability of an assistive device is characterized by the relationship between the user, the assistive device, the activity and the context [16,17]. Non-use can be related to the feeling of being disabled and in turn affects the person’s identity [18]. People’s reactions to their devices are complex and individual, because different persons have different needs, abilities, preferences and previous experiences [3].
There is a knowledge gap in the significance of standing depending on that assistive devices hold different meanings for different users and there are several possible reasons for using or not using them [8]. The psychosocial impact on the use of a powered wheelchair had a high value on QoL, happiness and independence but also negative impact concerning self-esteem and a feeling of being stigmatized when using the device [19]. The knowledge about the psychosocial impact of the use of standing devices is lacking, therefore it is important to get more knowledge in this area. Based on this, the purpose of the present study was to investigate the psychosocial impact of standing devices as experienced by users.
Methods
This study is the second part of a comprehensive survey conducted in the four northernmost counties and one county in central Sweden and deals with the psychosocial impact of the standing device. The first part concerned the users’ characteristics, their degree of use of the standing device and their experiences of standing [14].
Questionnaire
The questionnaire consisted of background questions concerning the persons responding to the survey to determine whether they responded (1) without assistance, (2) receiving help or (3) through someone else answering on their behalf. The questionnaire had questions about perceived health, to be answered using a thermometer graded from 0 to 100 (the EQ5D thermometer), gender, age, diagnosis, movement skills, the type of standing device used, the time since the prescription and the standing frequency and duration.
The impact of standing devices on functional independence, QoL and wellbeing was assessed using the Psychosocial Impact of Assistive Devices Scale (PIADS) [20,21]. The PIADS is a self-reported questionnaire with 26 items. The scale of the questionnaire ranges from −3 (the maximum negative impact) to +3 (the maximum positive impact), and the results are presented with a total score and three sub-scores (competence, adaptability and self-esteem) [2,21].
PIADS has proven to be a reliable, valid and responsive measure with good clinical utility [22]. The scale seems to have the power to predict the abandonment and retention of an assistive device [2]. A good example of previous use of the questionnaire is a study on the impact of the use of power wheelchairs on the activities and participation of people with stroke [19].
Procedure
The process was anchored by sending a request and information about the study to the manager for assistive devices in each county and statistics on the prescription of standing devices were obtained. The prescribers and/or the consultants for assistive devices who had knowledge about the potential participants received oral and written information about the study from the first author. Thereafter the recruiting staff made a request about participation to the persons concerned. The persons received information about the study and were informed that the participation was voluntary and that it was free to decline without declaration. Those who accepted received the questionnaire and written information about the study by mail, together with a prepaid self-addressed envelope. The questionnaire was answered by the person himself/herself or a parent/related person. The study was approved by the Regional Ethical Review Board in Umeå (Ref. no.: 09-211Ö).
Participants
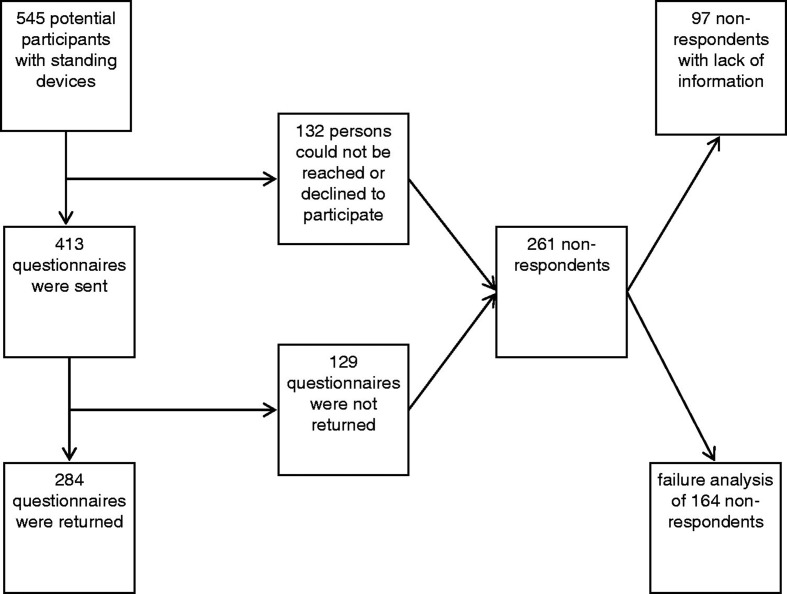
Five hundred and forty-five (545) persons who had received a standing device were identified but 132 of those persons could not be reached or declined to participate. Therefore only 413 questionnaires were sent out and 284 were returned, resulting in a response rate of 52% (Figure 1). The participants were divided as belonging to all age groups, their age ranging from 2 to 86 years. Only 22% of the respondents answered the questionnaire independently, while as many as 44% needed someone else to answer on their behalf. The need for help to respond varied between users with different diagnoses. Persons with acquired disabilities such as amyotrophic lateral sclerosis (ALS) and spinal cord injuries (SCI) were most independent in this respect. Three out of four persons with cerebral palsy (CP) had someone else answering the questionnaire on their behalf. The profiles of the participants are described in Table 1. As can be seen, the most common way to ambulate for the participants was to use a manual wheelchair, and a large proportion of those using a standing device were dependent on others for ambulation.
Figure 1.
The number of questionnaires sent to users of standing devices and the number of eventual participants.
Table 1.
Descriptive data of the participants (n = 284).
| n | % | |
|---|---|---|
| Who answered PIADS | ||
| User | 62 | 22 |
| User with help of someone | 97 | 34 |
| Someone else | 125 | 44 |
| Missing | ||
| Age: 2–86 years median 37 (SD 22.4) | ||
| Age groups | ||
| 0–6 years | 21 | 7 |
| 7–12 years | 37 | 13 |
| 13–19 years | 26 | 9 |
| 20–49 years | 101 | 36 |
| 50–64 years | 54 | 19 |
| 65 years or older | 44 | 16 |
| Missing | 1 | |
| Gender | ||
| Female | 108 | 38 |
| Male | 173 | 61 |
| Missing | 3 | 1 |
| Diagnoses* | ||
| Congenital disease/injury | 129 | 45 |
| Acquired disease/injury | 127 | 45 |
| Undiagn./other diagn. | 18 | 6 |
| Missing | 10 | 4 |
| Walking ability | ||
| Yes | 51 | 18 |
| No | 233 | 82 |
| Most common means of ambulation | ||
| Walking | 16 | 6 |
| Manual wheelchair | 207 | 73 |
| Powered wheelchair | 60 | 21 |
| Missing | 1 | |
| Need for help in ambulation | ||
| Independent | 78 | 28 |
| With some help | 55 | 19 |
| Totally dependent | 151 | 53 |
| Type of standing device | ||
| Standing shell | 66 | 23 |
| Standing frame | 63 | 22 |
| Standing frame with rear wheels | 17 | 6 |
| Tilt table | 66 | 23 |
| Wheelchair with stand-up function | 69 | 25 |
| Other/missing | 3 | 1 |
| Time since prescription | ||
| 0–2 years | 60 | 21 |
| 2–5 years | 78 | 28 |
| 5–10 years | 62 | 22 |
| >10 years | 83 | 29 |
| Missing | 1 |
Congenital disabilities: CP, syndromes, multi-disabilities, spina bifida. Acquired disabilities: MS, ALS, TBI, stroke, virus, tumours. Undiagnosed/other: Persons with no diagnosis or an unusual diagnosis.
Analysis of the non-respondents
The data for 164 of the 261 non-respondents were sufficient for a comparison with the respondents regarding age, sex gender and type of standing device. The mean age (±SD) of the respondents was 37 ± 22.4 years, while that of the non-respondents was 31 ± 20.9 years. The proportion of men who responded to the survey was 61%, while the proportion of men in the group of non-respondents was 46%. The non-participants did not differ from the respondents with respect to the kind of prescribed device, except in the case of the standing wheelchair; there were fewer users of standing wheelchairs amongst the non-respondents. Twenty-five percent of the respondents had standing wheelchairs, while only 12% of those who refrained from responding to the survey had standing wheelchairs. The loss of participants was equally distributed in the northern region and the county in central Sweden.
Analysis of data
The data were analyzed with descriptive statistics including percentages and medians. Since the study was designed to be a survey of a sample population of people who used standing devices in Sweden, no inferential statistics were calculated.
Results
Psychosocial impact of standing devices
The psychosocial impact of the standing devices was perceived by the respondents as positive, deeming from their ratings (Table 2). The medians for the total PIADS score and the PIADS sub-scores turned out to be positive, and even the first quartiles were on the positive side. The competence sub-score showed lower ratings than all the other sub-scores.
Table 2.
PIADS scores.
| Median | Q1 | Q3 | |
|---|---|---|---|
| PIADS total (n = 284) | 0.63 | 0.20 | 1.37 |
| Adaptability (n = 296) | 0.67 | 0.17 | 1.5 |
| Competence (n = 292) | 0.54 | 0.08 | 1.33 |
| Self-esteem (n = 296) | 0.62 | 0.12 | 1.37 |
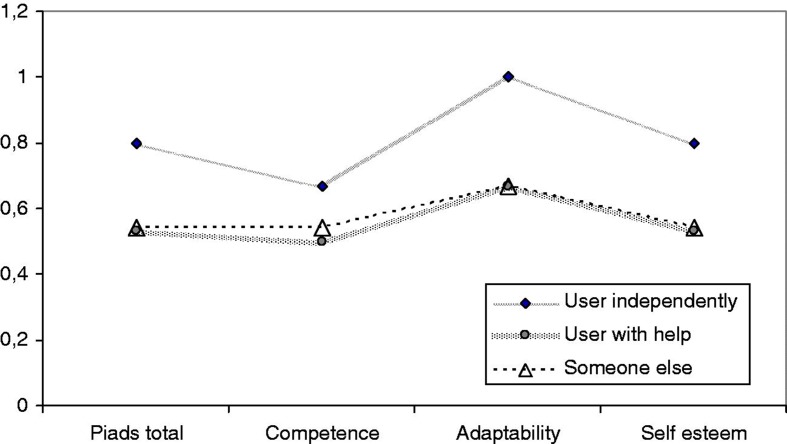
The users answering the questionnaire without assistance awarded higher scores compared to those receiving help or having someone else answering on their behalf. This was the case for the PIADS total score and sub-scores (Figure 2).
Figure 2.
PIADS scores in relation to the level of assistance needed in responding to the questionnaire.
PIADS scores in relation to the participants’ sex, age and diagnosis
The PIADS total scores were equally distributed with regard to gender. The highest value was found in the oldest group, aged 65 years or older (median 0.77), while the lowest value was found in the group aged 13–19 years (median 0.35). Persons with acquired diseases/injuries in general awarded higher PIADS scores compared to those with a congenital disease/injury. Persons between 13 and 19 years of age differed as the group with the lowest PIADS total score and sub-scores, in contrast to children between 7 and 12 years of age, who gave higher scores, particularly concerning the dimension of self-esteem (Table 3).
Table 3.
PIADS scores in relation to different variables.
| PIADS total | Adaptability | Competence | Self-esteem | |
|---|---|---|---|---|
| Sex | ||||
| Female (n = 108) | 0.63 | 0.67 | 0.50 | 0.62 |
| Male (n = 173) | 0.65 | 0.83 | 0.58 | 0.62 |
| Missing (n = 3) | ||||
| Age groups | ||||
| 0–6 years (n = 21) | 0.50 | 0.58 | 0.50 | 0.25 |
| 7–12 years (n = 37) | 0.69 | 0.67 | 0.67 | 0.87 |
| 13–19 years (n = 26) | 0.35 | 0.33 | 0.25 | 0.37 |
| 20–49 years (n = 101) | 0.65 | 0.67 | 0.58 | 0.62 |
| 50–64 years (n = 54) | 0.65 | 0.83 | 0.50 | 0.75 |
| 65 years or older (n = 44) | 0.77 | 1.00 | 0.58 | 0.62 |
| Missing (n = 1) | ||||
| Diagnoses* | ||||
| Congenital disease/injury (n = 129) | 0.54 | 0.67 | 0.50 | 0.56 |
| Acquired disease/injury (n = 127) | 0.69 | 0.83 | 0.58 | 0.75 |
| Undiagn./other diagn. (n = 28) | 0.56 | 0.67 | 0.58 | 0.62 |
| Type of standing device | ||||
| Standing shell (n = 66) | 0.52 | 0.50 | 0.51 | 0.62 |
| Standing frame (n = 63) | 0.69 | 0.75 | 0.50 | 0.62 |
| Standing frame with rear wheels (n = 17) | 0.46 | 0.42 | 0.37 | 0.5 |
| Tilt table (n = 66) | 0.63 | 0.83 | 0.58 | 0.75 |
| Wheelchair with stand-up function (n = 69) | 0.65 | 0.67 | 0.62 | 0.62 |
| Other type/missing (n = 3) | ||||
| Time since prescription | ||||
| 0–2 years (n = 60) | 0.71 | 1.00 | 0.58 | 0.69 |
| 2–5 years (n = 78) | 0.42 | 0.67 | 0.42 | 0.37 |
| 5–10 years(n = 62) | 0.58 | 0.58 | 0.42 | 0.62 |
| >10 years (n = 83) | 0.77 | 0.83 | 0.58 | 0.77 |
| Missing (n = 1) | ||||
| Walking ability with or without help | ||||
| Yes (n = 51) | 0.88 | 0.92 | 0.83 | 0.75 |
| No (n = 233) | 0.58 | 0.67 | 0.50 | 0.62 |
| Most common means of ambulation | ||||
| Walking (n = 16) | 1.48 | 1.17 | 1.12 | 1.50 |
| Manual wheelchair (n = 207) | 0.65 | 0.67 | 0.58 | 0.62 |
| Powered wheelchair (n = 60) | 0.46 | 0.67 | 0.42 | 0.37 |
| Missing (n = 1) | ||||
| Need for help in ambulation | ||||
| Independent (n = 78) | 0.77 | 1.00 | 0.67 | 0.62 |
| With some help (n = 55) | 0.50 | 0.50 | 0.42 | 0.62 |
| Totally dependent (n = 151) | 0.61 | 0.67 | 0.50 | 0.62 |
| Frequency of standing** | ||||
| Often (n = 167) | 0.69 | 0.67 | 0.58 | 0.75 |
| Quite often (n = 86) | 0.54 | 0.92 | 0.50 | 0.50 |
| Rarely (n = 31) | 0.31 | 0.33 | 0.21 | 0.37 |
| Standing time | ||||
| <15 min (n = 20) | 0.42 | 0.33 | 0.50 | 0.37 |
| 15–30 min (n = 126) | 0.54 | 0.67 | 0.50 | 0.62 |
| 30–60 min (n = 111) | 0.69 | 0.83 | 0.58 | 0.75 |
| >60 min (n = 14) | 0.38 | 0.42 | 0.33 | 0.31 |
| Short periods in different activities (n = 13) | 1.07 | 1.5 | 0.92 | 0.87 |
Congenital disease/injury: CP, syndromes, multi-disabled, spina bifida. Acquired disease/injury: MS, ALS, SCI, TBI, stroke, virus, tumours. Undiagnosed/other diagnoses: Persons with no diagnosis and unusual diagnoses.
Often: Several times a day, daily, almost daily. Quite often: Several times a week. Rarely: Once a week, almost never, never.
PIADS scores in relation to the type of standing device used and the time since the device was prescribed
The PIADS total scores were quite similar for all the types of standing devices, except for standing shells and standing frames with rear wheels, which showed lower scores. When examining the PIADS scores in relation to the length of time the respondents had had their standing device, it was found that persons who had been using a standing device for 10 years or longer awarded the highest scores, while those who had received their device 2–5 years previously gave the lowest scores (Table 3).
PIADS scores in relation to ambulation and the need for help
Respondents who possessed the ability to walk with or without help awarded higher PIADS scores compared to those who did not walk. It appeared that those who used walking as their most common means of ambulation assessed that standing had a greater psychosocial impact than was assessed by persons who had manual or powered wheelchairs as their most common means of ambulation. Persons who were independent in ambulation awarded higher scores than persons who were totally dependent on help for ambulation, and also gave higher scores than those who needed some help for ambulation (Table 3). An analysis of the persons who could walk showed that the majority of the 51 persons who had the ability to walk had congenital disabilities. Nine persons with a congenital disability could walk independently, with or without a device, while no one with an acquired disability had an independent walking ability. Forty-two persons could walk with help from someone and nine of them had an acquired disability. Persons who had walking as the most common means of ambulation awarded a PIADS total score of 1.48 and persons who had the ability to walk with or without help scored higher than those who did not have the ability to walk.
PIADS scores in relation to the standing frequency and duration
Those who stood often (several times/day, daily, almost daily) awarded higher scores in the PIADS questionnaire compared to those who used their device less frequently. When standing was integrated in various activities, high scores were awarded. Standing several times in different activities resulted in the highest scores, followed by standing for 30–60 min each time.
Perceived health according to the EQ5D thermometer
The ratings made according to the EQ5D thermometer were spread across the whole range of the scale. There were some differences depending on who answered the questionnaire. The value was the same when the user rated without help and when someone else rated on behalf of the user (70), but when the user rated with the help of someone else, the score was lower (61). There was a trend towards a small positive correlation between the scoring according to the EQ5D thermometer and the PIADS total score and the three sub-scores. Age had an impact on the rating in that the values declined with age, from 73 on the scale for the youngest (1–6 years of age) to 56 for the oldest (65 years of age or older).
Discussion
Based on our knowledge, this is one of the first studies that emphasize the meaning of using a standing device. The use of standing devices had a positive impact on psychosocial factors, which implies that the standing position holds a meaning for the users. Independence in communication and ambulation affected the scores positively. The individually highest scores in the PIADS questionnaire were awarded by persons who had the ability to walk. The teenagers gave the lowest scores, which applied to both the total score and all the sub-scores, and persons with acquired disabilities gave higher scores compared to persons with congenital disabilities. The scores increased with a higher frequency of use and the persons who had had their device for 10 years or longer awarded higher scores than the persons who had had their device for a shorter time. Analyzing the psychosocial impact in relation to the standing duration showed that standing for several short periods integrated in activities in daily life revealed higher scores compared to other selectable options. That finding coincides well with the ICF’s definition of assistive devices, which implies that an assistive device has the potential to facilitate activities [1]. Despite the fact that the physical effects of prolonged standing have been reported to be limited and inconclusive [11], this study provides a generally positive image of standing which reinforces the importance of standing from a psychosocial aspect.
The teenagers (13–19 years of age) gave the lowest values for the PIADS total score and the three sub-scores (concerning adaptability, competence and self-esteem), and the youngest group (0–6 years of age) also awarded low scores concerning self-esteem. The low rating concerning self-esteem can be explained by the fact that it was parents/related persons who responded to the questionnaire on the children’s behalf. This is in line with the findings of Upton et al. [23] who showed that the parents of children with health conditions tend to underestimate the child health-related QoL. Furthermore, the scores concerning self-esteem could be influenced by parent–child connectedness. A previous study has shown that the parents’ psychological state should also be measured with respect to their physical and mental health, because the parents’ self-esteem is one factor that may affect proxy reports of QOL [24].
A previous study by Nordström et al. [14] showed that teenagers stood less frequently compared to the younger users and that the standing time decreased with increasing age. In the present study, frequent standing was shown to result in higher PIADS total scores and sub-scores. Huang et al. [25] showed that children with CP between 8 and 15 years of age had a negative impression of standing devices and experienced them as uncomfortable and limiting. Muscle shortening in children with CP is common [26] and that can contribute to the deterioration of standing skills [27]. The shortening of muscles and chronic pain are common problems for youths with neuromuscular diseases. This in turn can contribute to making the standing position painful [28]. Studies examining the period of “transition” from childhood to adult life have reported a decline in both health and functional ability [29,30]. The low values for PIADS scores for teenagers could be a possible sign that they demonstrate a heightened level of self-consciousness and want to be like others [31]. Possibly, the standing device makes them feel different from other teenagers. According to Larsson-Lund and Nygård [32], an assistive device can not only facilitate an activity, but also be stigmatizing for the user. Hemmingsson et al. [33] showed that psychosocial aspects such as how the device influenced one’s self-image and one’s peers’ reactions to the assistive device were important from the teenager’s perspective.
Persons with acquired disabilities awarded slightly higher PIADS scores than persons with congenital disabilities. People with acquired disabilities may value the psychosocial impact of their standing device higher because the standing position can contribute to the feeling of being like others, a sense of normality, being like before [9]. Louise-Bender Pape, Kim and Weiner [8] concluded that the meaning of a device differs depending on whether the person using it has a congenital or an acquired disability. In contrast to the above-mentioned positive effect, a device can also clarify the consequences of a disability by highlighting the body’s limitations for persons with progressive disabilities [8,9]. Use of the device can be seen as the beginning of the end [8]. Persons with congenital disabilities do not have the time before and the time after the disease/injury to consider, and for them the use of standing devices may therefore have a natural meaning. However, deterioration in function is common for persons with congenital disabilities, e.g. persons with CP, for whom normal ageing may emerge earlier in life [34,35]. This may contribute to the meaning of an assistive device being altered during a person’s lifetime [8].
The scores awarded were rather equal regardless of the type of standing device used. Persons with standing shells and standing frames with rear wheels gave slightly lower values. This can be explained by the fact that the users of these devices were younger and had a congenital disability and that other persons awarded scores for them. All these factors affected the scores negatively. According to the process of prescribing assistive devices [36] and to Scherer and Craddock [37], individual needs and goals should guide and govern the choice of device so that individual needs can be fulfilled. Persons using their device for >10 years awarded the highest scores and this could be an indication that the individual needs of this group have been fulfilled, in contrast to the lowest scoring group, who had had their device for 2–5 years. This may imply, in the latter case, that the assessment prior to the prescription of the device and the follow-ups had failed and that the psychosocial aspects of the device had not been taken into account. Clinical experiences indicate that sometimes an adjustment or a replacement of the device has positive effects on the users’ experience in terms of the psychosocial impact of the device. As professionals we need to ensure that the person with a disability has been provided with the optimal standing device.
Surprisingly, persons who had the ability to walk awarded higher PIADS scores compared to those who did not. There can be many different reasons for this. The majority of the persons who could walk had a congenital disability and it may be the case that standing was seen as a treatment which could improve their potential to walk. This is in line with a study by Salem et al. [38], who showed that prolonged standing for children with CP improved their walking ability. Furthermore, standing itself could also be the starting-point for independence [39] and/or, according to McKeever et al. [40], for the provision of a symbolic value. One can also speculate whether a user’s ability to walk and to be independent in ambulation can mean that he/she has the ability to get in and out of the device independently, which in turn means that the device is used more and is perceived to have a greater psychosocial impact for the user.
It is satisfying to note that those who stood most frequently rated the psychosocial impact of the standing device highest. Being able to stand for several short periods in activities was highly valued. Since the physical effects of standing are contradictory, we as professionals should focus on the user’s perceived meaning of standing. If a standing device is used frequently and is perceived to have a positive psychosocial impact, this could mean that the person using it has the optimal standing device for their needs [36]. According to Alerby [41], a pen should be regarded as an integrated part of the body and not just an object that makes writing become a habit, and the assistive device should be considered in a similar way. The optimal standing device should therefore, adopting this view, be perceived as an extension of the body [42] and not only an object whose purpose is to exercise the physical body. The highest PIADS scores in relation to the standing frequency and duration were found when standing was performed for several short periods in different activities. One explanation for this could be that, when the device is used in an activity, the standing position holds a meaning for the person using it. Our mission as professionals is to broaden our view of the use of standing devices, i.e. to see the standing device as an aid that not only treats the body’s structures or improves the user’s abilities in activities, but also provides a psychosocial impact on the user’s daily life, and to find meaningful goals for the user from a psychosocial aspect.
We chose to use PIADS as an instrument for our purpose because it is an instrument that is especially designed to evaluate the psychosocial impact of the device. Further, PIADS was developed with users involved and it also tested to be reliable in cases where someone else is answering the questionnaire on behalf of the user which is a common case among people who use standing devices [2].
There are several limitations to take into account which affect the generalisation of this comprehensive survey. Firstly, 48% of the potential participants did not respond to the survey. This fact raises the question of whether or not these non-respondents were users of standing devices with which they were dissatisfied. Secondly, all the respondents were not autonomous and other persons were involved in answering the questionnaires. PIADS is supposed to work even if the survey is completed by another person, but that fact may have contributed to the high failure rate. Many users of standing devices are not autonomous and it is important to obtain their knowledge with the help of those who know them best. However, we have to be aware that the outcome could have been different if all the users had been able to speak for themselves. It is known that the parents of children with health conditions tend to underestimate their children’s health-related QoL [25], and this kind of underestimation may have had an impact in this study. Or could it be the case that those users who did not respond independently had a lower health status and consistently experienced a lower psychosocial impact from the device? The fact that the requesting staff knew the participants could be a limitation from a confidentially perspective, therefore the participants were assured that their data would be presented in such a way that no single participant could be recognizable.
Conclusions
The objective of this research study has been to measure the experience of standing of users of standing devices. For this purpose PIADS appears to serve a useful purpose. The main results of the study was that the psychosocial impact of standing devices was generally experienced positively, but there were some differences among the participants of the survey. It was shown that those respondents who possessed a higher physical capacity and an ability to respond independently considered it even more important to stand. Being able to stand in activities and having the ability to walk seemed to be important. Being a teenager was associated with lower scores, as was a standing time of >60 min each time.
The main results indicated that standing in a standing device had a value and we as professionals should ask the users about the intended purpose of their standing in order to prescribe the optimal device. The prescribers ought to try to influence the suppliers of standing devices to design a device that the users are asking for. Future research should investigate the meaning which standing in the device holds for the person using it, and should focus on the psychosocial impact of using a standing device which the results of this study have confirmed. Furthermore studies should focus on a detailed analysis of psychosocial aspects.
Acknowledgements
The authors would like to thank the participants in this study.
Footnotes
Declaration of interest: Financial support was kindly provided by the Norrbacka Eugenia Foundation, Stockholm, Sweden.
References
- 1. ICF W. International classification of functioning, disability and health. Geneva: World Health Organization 2001:3–25.
- 2.Day H, Jutai J, Campbell KA. Development of a scale to measure the psychosocial impact of assistive devices: lessons learned and the road ahead. Disabil Rehabil. 2002;24:31–7. doi: 10.1080/09638280110066343. [DOI] [PubMed] [Google Scholar]
- 3.Scherer MJ. Outcomes of assistive technology use on quality of life. Disabil Rehabil. 1996;18:439–48. doi: 10.3109/09638289609165907. [DOI] [PubMed] [Google Scholar]
- 4.Day HY, Jutai J, Woolrich W, Strong G. The stability of impact of assistive devices. Disabil Rehabil. 2001;23:400–4. doi: 10.1080/09638280010008906. [DOI] [PubMed] [Google Scholar]
- 5.Agree E. A quality-of-life scale for assistive technology: results of a pilot study of aging and technology. Phys Ther. 2011;91:1780–8. doi: 10.2522/ptj.20100375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Renwick R, Nourhaghighi N, Manns PJ, Rudman DL. Quality of life for people with physical disabilities: a new instrument. Int J Rehabil Res. 2003;26:279–87. doi: 10.1097/00004356-200312000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Scherer M. The relationship of personal factors and subjective well-being to the use of assistive technology devices. Disabil Rehabil. 2011;33:811–17. doi: 10.3109/09638288.2010.511418. [DOI] [PubMed] [Google Scholar]
- 8.Louise-Bender P. The shaping of individual meanings assigned to assistive technology: a review of personal factors. Disabil Rehabil. 2002;24:5–20. doi: 10.1080/09638280110066235. [DOI] [PubMed] [Google Scholar]
- 9.Nordström B, Näslund A, Ekenberg L. On an equal footing: adults’ accounts of the experience of using assistive devices for standing. Disabil Rehabil Assist Technol. 2013;8:49–57. doi: 10.3109/17483107.2012.678031. [DOI] [PubMed] [Google Scholar]
- 10.Newman M. The effect of supported standing in adults with upper motor neurone disorders: a systematic review. Clin Rehabil. 2012;26:1059–77. doi: 10.1177/0269215512443373. [DOI] [PubMed] [Google Scholar]
- 11.Glickman LB, Geigle PR, Paleg GS. A systematic review of supported standing programs. J Pediatr Rehabil Med. 2010;3:197–213. doi: 10.3233/PRM-2010-0129. [DOI] [PubMed] [Google Scholar]
- 12.Arva J, Paleg G, Lange M, et al. RESNA position on the application of wheelchair standing devices. Assist Technol. 2009;21:161. doi: 10.1080/10400430903175622. 168; quiz 169–171. [DOI] [PubMed] [Google Scholar]
- 13. International Organization for Standardization. International Standard ISO 9999; 2007 (e) Assistive products for persons with disability. Classification and terminology, 4th ed.
- 14. Nordström B, Näslund A, Nyberg L, et al. The impact of supported standing on wellbeing and quality of life. 2013. [DOI] [PMC free article] [PubMed]
- 15.Taylor K. Factors affecting prescription and implementation of standing-frame programs by school-based physical therapists for children with impaired mobility. Pediatr Phys Ther. 2009;21:282–8. doi: 10.1097/PEP.0b013e3181b175cd. [DOI] [PubMed] [Google Scholar]
- 16.Lenker J. A new conceptual model for assistive technology outcomes research and practice. Assist Technol. 2004;16:1–10. doi: 10.1080/10400435.2004.10132069. [DOI] [PubMed] [Google Scholar]
- 17.Arthanat S, Bauer SM, Lenker JA, et al. Conceptualization and measurement of assistive technology usability. Disability and Rehabilitation: assist Technol. 2007;2:235–48. doi: 10.1080/17483100701343665. [DOI] [PubMed] [Google Scholar]
- 18.Hocking C. Function or feelings: factors in abandonment of assistive devices. Technol Disabil. 1999;11:3–11. [Google Scholar]
- 19.Pettersson I, Ahlström G, Törnquist K. The value of an outdoor powered wheelchair with regard to the quality of life of persons with stroke: a follow-up study. Assist Technol. 2007;19:143–53. doi: 10.1080/10400435.2007.10131871. [DOI] [PubMed] [Google Scholar]
- 20.Demers L, Monette M, Descent M, et al. The psychosocial impact of assistive devices scale (PIADS): translation and preliminary psychometric evaluation of a canadian-french version. Qual Life Res. 2002;11:583–92. doi: 10.1023/a:1016397412708. [DOI] [PubMed] [Google Scholar]
- 21.Day H, Jutai J. PIADS: the psychosocial impact of assistive devices scale. Toronto: Authors; 1996. [Google Scholar]
- 22.Jutai J, Day H. Psychosocial impact of assistive devices scale (PIADS) Technol Disabil. 2002;14:107–11. [Google Scholar]
- 23.Upton P, Lawford J, Eiser C. Parent–child agreement across child health-related quality of life instruments: a review of the literature. Qual Life Res. 2008;17:895–913. doi: 10.1007/s11136-008-9350-5. [DOI] [PubMed] [Google Scholar]
- 24.Davis E, Mackinnon A, Waters E. Parent proxy-reported quality of life for children with cerebral palsy: is it related to parental psychosocial distress? Child Care Health Dev. 2011;38:553–60. doi: 10.1111/j.1365-2214.2011.01267.x. [DOI] [PubMed] [Google Scholar]
- 25.Huang I-, Sugden D, Beveridge S. Children’s perceptions of their use of assistive devices in home and school settings. Assist Technol. 2009;4:95–105. doi: 10.1080/17483100802613701. [DOI] [PubMed] [Google Scholar]
- 26.Boyd RN, Graham HK. Objective measurement of clinical findings in the use of botulinum toxin type A for the management of children with cerebral palsy. Eur J Neurol. 2007;6:s23–35. [Google Scholar]
- 27.Hägglund G, Wagner P. Development of spasticity with age in a total population of children with cerebral palsy. BMC Musculoskel Disord. 2008;9:150. doi: 10.1186/1471-2474-9-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Engel JM, Kartin D, Carter GT, et al. Pain in youths with neuromuscular disease. Am J Hosp Palliat Med. 2009;26:405–12. doi: 10.1177/1049909109346165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hagberg B, Hagberg G, Olow I, Wendt L. The changing panorama of cerebral palsy in sweden. VII. prevalence and origin in the birth year period 1987–90. Acta Paediatr. 1996;85:954–60. doi: 10.1111/j.1651-2227.1996.tb14193.x. [DOI] [PubMed] [Google Scholar]
- 30.Stevenson CJ, Pharoah POD, Stevenson R. Cerebral palsy-the transition from youth to adulthood. Dev Med Child Neurol. 2008;39:336–42. doi: 10.1111/j.1469-8749.1997.tb07441.x. [DOI] [PubMed] [Google Scholar]
- 31.Ruffin N. Adolescent growth and development. Retrieved. 2009;7:2010. [Google Scholar]
- 32.Larsson-Lund M, Nygård L. Incorporating or resisting assistive devices: different approaches to achieving a desired occupational self-image. Occup Part Health. 2003;23:67–75. [Google Scholar]
- 33.Hemmingsson H, Lidström H, Nygård L. Use of assistive technology devices in mainstream schools: students’ perspective. Am J Occup Ther. 2009;63:463–72. [PubMed] [Google Scholar]
- 34.Bottos M, Feliciangeli A, Sciuto L, et al. Functional status of adults with cerebral palsy and implications for treatment of children. Dev Med Child Neurol. 2001;43:516–28. doi: 10.1017/s0012162201000950. [DOI] [PubMed] [Google Scholar]
- 35.Sandström K, Alinder J, Öberg B. Descriptions of functioning and health and relations to a gross motor classification in adults with cerebral palsy. Disabil Rehabil. 2004;26:1023–31. doi: 10.1080/09638280410001703503. [DOI] [PubMed] [Google Scholar]
- 36. Förskrivningsprocessen för hjälpmedel till personer med funktionshinder (prescribing assistive devices for for people with disabilities) [Internet] Stockholm: Hjälpmedelsinstitutet; c2011. Available from: http://www.hi.se/Global/pdf/2011/11357-forskrivningsprocessen.pdf [last accessed 15 Mar 2013]
- 37.Scherer MJ, Craddock G. Matching person & technology (MPT) assessment process. Technol Disabil. 2002;14:125–31. [Google Scholar]
- 38. Salem Y, Lovelace-Chandler V, Zabel RJ, McMillan AG. Effects of prolonged standing on gait in children with spastic cerebral palsy. Phys Occup Ther Pediatr 2010, 2012/12;30:54–65. [DOI] [PubMed]
- 39. Straus EW. Phenomenological psychology: the selected papers of erwin W.strauss. Tavistock Publications; 1966. translated in part from the German by Erling Eng; This selection originally published, Basic Books; 1966.
- 40.McKeever P, Rośsen BE, Robinson-Vincent K, Wright V. The significance of uprightness: parents’ reflections on children’s responses to a hands-free walker for children. Disabil Soc. 2012;28:1–13. [Google Scholar]
- 41.Alerby E. Knowledge as a ‘body run’: learning of writing as embodied experience in accordance with Merleau-Ponty’s theory of the lived body. Indo Pac J Phenomenol. 2009;9:Edition 1. [Google Scholar]
- 42.Berndtsson I. Tekniska hjälpmedel, synskadade och samhället. In: Bengtsson J, editor. Med livsvärlden som grund: Bidrag till utvecklandet av en livsvärldsfenomenologisk ansats i pedagogisk forskning. Lund: Studentlitteratur; 1999. [Google Scholar]