Abstract
Objective: Cognitive models of psychosis suggest that anomalous experiences alone do not always lead to clinical psychosis, with appraisals and responses to experiences being central to understanding the transition to “need for care”. Methods: The appraisals and response styles of Clinical (C; n = 28) and Nonclinical (NC; n = 34) individuals with psychotic experiences were compared following experimental analogues of thought interference (Cards Task) and auditory hallucinations (Virtual Acoustic Space Paradigm). Results: The groups were matched in terms of their psychotic experiences. As predicted, the C group scored higher than the NC group on maladaptive appraisals following both tasks, rated the experience as more personally significant, and was more likely to incorporate the experimental setup into their ongoing experiences. The C group also appraised the Cards Task as more salient, distressing, and threatening; this group scored higher on maladaptive—and lower on adaptive—response styles, than the NC group on both tasks. Conclusions: The findings are consistent with cognitive models of psychosis, with maladaptive appraisals and response styles characterizing the C group only. Clinical applications of both tasks are suggested to facilitate the identification and modification of maladaptive appraisals.
Key words: psychosis continuum, cognitive model of psychosis, appraisals, experimental analogues of psychotic symptoms
Introduction
There is increasing evidence that symptoms associated with psychosis are reported in the general population without an associated “need for care” (ie, leading to a psychotic disorder diagnosis or requiring treatment from mental health services), suggesting that the psychosis phenotype lies on a continuum.1 Recent research has focused on identifying the biological2 and psychological3 processes that distinguish between people who experience psychotic experiences with and without a need for care. Cognitive models of psychosis4–6 propose that beliefs and appraisals play a central role in determining the clinical consequence of psychotic experiences.
Studying non-need for care individuals who report persistent anomalous experiences of a psychotic nature provides a unique opportunity to differentiate those factors that are linked to the clinical disorder from those that are merely associated with benign anomalous experiences. In early studies involving individuals reporting intense spiritual experiences,7,8 it was found that they could not be distinguished from psychotic symptoms phenomenologically. Rather, the differences lay in the interpretation and meaning given to the experiences and in their emotional and behavioral correlates. Similarly, individuals belonging to New Religious Movements scored as highly as inpatients on a delusional ideation questionnaire,9,10 but they were differentiated from their clinical counterparts by lower scores on dimensions of distress and preoccupation.11,12 Using an in-depth interview (AANEX: Appraisals of Anomalous Experiences interview),13 patients with psychosis were more likely to think their experiences were caused by someone else (“personalizing” appraisals) and were less likely to have “normalizing” appraisals (eg, that they are part of the normal range of human experience) than individuals reporting anomalous experiences without a need for care.13,14
Cognitive models of psychosis also propose that maladaptive responses play a key role in maintaining psychotic symptoms and associated distress. Different response styles to psychotic experiences have been variously identified as engagement, resistance, and indifference6 or as active acceptance, passive coping, and resistance coping.15 Symptomatic coping (going along with the content of psychotic symptoms) and active problem solving have been found to be, respectively, more and less common in a group with need for care compared to individuals with psychotic experiences with no need for care and these were associated with, respectively, less and more perceived control over symptoms.16
Previous work on the potential role of appraisals and response style has typically been based on retrospective interviews of participants’ experiences, an approach that makes it difficult to disentangle experiences from appraisals and cannot exclude the possibility that maladaptive appraisals and coping simply reflect intrinsically more distressing experiences within the clinical group. One potential solution is the use of experimental tasks and analogues of psychotic symptoms, allowing all participants to encounter identical anomalous experiences.17
Aims of the Study
The current study compared appraisals and response styles in individuals displaying psychotic experiences with and without need for care. We hypothesized, in line with cognitive models of psychosis, that the Clinical (C) group would be more likely to endorse maladaptive appraisals and response styles and less likely to endorse adaptive appraisals and response styles, on two experimentally induced anomalous experiences, than the Non clinical (NC) group.
Materials and Methods
Design
The independent variable was the grouping variable (2 levels: C and NC), and the dependent variables were scores on visual analogue scales (0–10) for “appraisal” and “response style” ratings following the experimental tasks.
Ethical Approval
Approval for the research project was obtained from the East London and The City Research Ethics Committee (REC Reference number: 09/H0703/83) and the South London & Maudsley/Institute of Psychiatry (SLAM/IOP) Research and Development Office (Reference: R&D2009/064).
Participants
Both groups were recruited on the basis of evidence of at least one positive symptom of psychosis occurring within the previous month. Only individuals who reported at least “occasional” psychotic experiences (the equivalent of 2 or above on at least 1 item of the Scale for the Assessment of Positive Symptoms (SAPS)18 in the absence of drug use and in clear consciousness were invited to participate. Exclusion criteria were non-English speaking, organic or alcohol/drug-induced brain damage, inability to concentrate for short periods, or inability to provide informed consent. Other data from this sample are reported in a separate study.3
C Group.
Inclusion in the C group was deter mined on the basis of current contact with mental health services as a result of their psychotic experiences. The group comprised 28 patients with current (N = 18) or probable (N = 10; these individuals were from Early Intervention services, where it is common practice to refrain from giving a diagnosis at first contact with services) diagnoses F20–39 based on the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10); the patients were recruited through inpatient wards, Community Mental Health Teams, and a psychological therapies service in the South London and Maudsley NHS Foundation (SLAM) Trust. All (except one) of the patients were on antipsychotic medication at the time of testing; 19 were outpatients and 9 were inpatients.
NC Group.
The NC group comprised 34 individuals with enduring psychotic-like experiences who had never been diagnosed with, treated for, or been in contact with mental health services in the context of a psychotic disorder. To determine with confidence that these individuals were not at risk of developing a psychotic disorder in the near future, participants whose anomalous experiences started less than 2 years prior to participation were excluded, based on findings that most of those “at risk” of developing psychosis do so within the first 24 months.19
The NC group was recruited from sources identified by previous studies13,14 as yielding this unique group, such as the College of Psychic Studies and the Society for Psychical Research. A snowballing method was used, encouraging participants to pass on information about the study to contacts whom they considered appropriate.
Demographic information on the groups is presented in table 1. There were no significant differences between the groups in terms of age, gender distribution, religious affiliation, or having children. The mean intelligence quotient (IQ) in the NC group was significantly higher than that in the C group, they were more likely to be married/cohabiting, to be in employment/training, and to describe their ethnicity as white. Their mean age at onset was significantly lower than that of the C group, whereas their mean “years since onset of experiences” was significantly higher. Depression and anxiety scores were significantly higher in the C group than in the NC group.
Table 1.
Demographic Characteristics of the 2 Groups
| Variable | Clinical (C) (N = 28) | Nonclinical (NC) (N = 34) | Group Differences |
|---|---|---|---|
| Mean age in years (SD) | 34.6 (12.4) | 40.3 (11.7) | t(60) = 1.9, P =.07 |
| Mean age at onset (SD)a | 22.3 (13.8) | 11.0 (9.4) | U = 153, P =.001 |
| Mean years since onset (SD)a | 10.7 (11.1) | 29.0 (11.3) | U = 88, P < .001 |
| Mean estimated IQ (SD)b | 90.8 (16.0) | 103.9 (11.9) | t (27) = −2.5, P = .02 |
| Number of male participants (%) | 50 | 35 | χ2 (1) = 1.4, P = .2 |
| Number from BME background | 50.0 | 14.7 | χ 2 (1) = 9.0, P < .01 |
| Number of participants employed/in training (%)c | 17.9 | 69.7 | χ 2 (1) = 16.4, P < .001 |
| Number of single participants (%)c | 85.7 | 42.4 | χ 2 (1) = 12.1, P = .001 |
| Number of participants with children (%)d | 28.0 | 31.0 | χ2 (1) = 0.06, P = .8 |
| Religious affiliation? (%)c | |||
| “Traditional” | 53.6 | 27.3 | χ2 (2) = 4.4, P = .1 |
| “Nontraditional” | 21.4 | 36.4 | |
| None | 25.0 | 36.4 | |
| Anxiety (BAI)e | 18.1 (13.2) | 4.2 (6.5) | U = 132.5, P < .001 |
| Depression (BDI)f | 23 (17.8) | 5.2 (6.4) | U = 110, P < .001 |
Note: Nonparametric tests were conducted on all nonnormally distributed variables. Bold face denotes significant differences between the groups. It was not possible to collect complete data on each individual (aC = 23; NC = 30; bC = 11; NC = 18; cNC = 33; dC = 25; NC = 29; eC= 24; NC = 31; fC = 25; NC = 33). BME, Black and Minority Ethnic groups; BDI, Beck Depression Inventory; BAI, Beck Anxiety Inventory; IQ, intelligence quotient.
Measures
“Unusual Experiences Questionnaire”–Screening Tool.
This was used to screen participants in the NC group and consisted of questions assessing 9 out of the 17 items used in the AANEX inventory.13 It assesses the presence within the past month of a range of positive symptoms of psychosis, including First-Rank symptoms (eg, voices, thought transmission and insertion, “made” emotions), in the absence of drug use and in clear consciousness.
AANEX Inventory—17 Item Version.14
The AANEX13 is a semistructured interview developed to assess phenomenological, psychological, and contextual factors surrounding the experience of psychotic-like experiences. The first part of the interview (AANEX Inventory, short version) consists of 17 anomalies, rated for the presence of each experience, both in the past and currently. Each experience was rated as either “not present,” “unclear,” or “present,” giving a score of 1–3, respectively. The inventory yields 5 factors of experiences: “Meaning–Reference” (ideas of reference, sense of having insights, elation), “Paranormal–Hallucinatory” (visual or somatic hallucinations, passivity, magical and precognitive experiences), “Cognitive–Attention” (thought blockages, distractibility, loss of automatic skills), “Dissociative–Perceptual” (depersonalization, derealization, Out-of-Body Experi ences, oversensitivity to stimuli), and “First-Rank Symptoms” (voices, thought transmission and insertion, “made” emotions). Factor scores were obtained by summing individual item scores for each factor (range of scores for each factor: 3–9, except “Meaning–Reference” and “First-Rank Symptoms,” where the range was 4–12). Total potential range of scores on the AANEX Inventory is 17–51. The AANEX has demonstrated good reliability and construct validity.13
Beck Depression and Anxiety Inventories.
The Beck Depression Inventory (BDI)-II20 and the Beck Anxiety Inventory (BAI)21 are widely used 21-item self-report questionnaires assessing the severity of depression and anxiety, respectively. The participant chooses 1 of 4 statements (0–3), which best describes their experience with respect to each item during the previous 2 weeks. Higher total scores indicate more severe pathology (potential range of scores: 0–63). The BDI-II has been shown to have high internal consistency (α = .92) and test–retest reliability (r = .93).20 Similarly, the BAI has high internal consistency (α = .92–.94) and test–retest reliability (r = .75) and has also been found to be significantly correlated with accepted measures of anxiety.22,23
Quick Test of Intelligence.
The Quick Test of Intelligence (QT)24 was devised as a measure of verbal intelligence and has been found to be highly correlated with IQ scores obtained on more standard tests in participants with schizophrenia.25 Participants are shown 4 pictures, and a list of 50 words is read aloud. Participants are asked to point to the picture that matches the word. The number of correct responses is used to derive an estimated IQ.
Experimental Tasks
Cards Task17 (http://sprott.physics.wisc.edu/pickover/esp2.html; last accessed July 1, 2013).
Participants were asked to silently choose and memorize 1 of 6 playing cards (face cards only) presented on a computer. They were informed that the card they had chosen would be selected by the computer and removed from the pile. They were then shown 5 different cards for 3 s. This trick relies on the fact that people only scan for the card they have chosen and do not notice that all the cards are different. This task was used as an experimental analogue of thought interference symptoms, ie, first-rank type symptoms primarily involving believing that one’s thoughts are not fully under one’s own control and/or are not private (eg, thought insertion, thought withdrawal, thought broadcasting, thought control, and mind reading).
Virtual Acoustic Space Paradigm.
The Virtual Acoustic Space Paradigm (VASP)26 permits sounds to be perceived as externally spatially located, despite presentation via headphones (normally perceived as spatially located “inside the head”). This task represented an analogue of auditory hallucinations or “loud thoughts.” Previous use of this paradigm has demonstrated 100% accuracy in identifying “outside the head” stimuli.27 Achieving the virtual acoustic effect depends on convolution of the acoustic stimulus with the spatially variable transfer function of the pinnae, the head-related transfer function (HRTF).26 Full details of the HRTF technique are provided elsewhere.27 The VASP was used in conjunction with a distractor task (a visual “Jumping to Perceptions” [JTP] task).28 In Part A, they completed the distractor task while listening to auditory white noise (perceived “inside the head”) on headphones. Participants were instructed to speak out loud any thoughts relating to the task that went through their mind while they were completing it (eg, “this task is dull”), which, unbeknown to them, were recorded by the laptop sound card. Three segments of speech for each participant (1–3 s in duration) were then manipulated using Adobe Soundbooth software (including lowering of the pitch by 2 semitones). The convolution, achieved using MATLAB (R2009a) software, involved presentation of the speech to the right ear (azimuth −90) and at an elevation of (+)45°. The 3 convoluted output files (now located “outside the head”) were then pasted into a 3-min segment of auditory white noise (perceived “inside the head”), providing the auditory stimuli for Part B of the distractor task.
Apparatus
The Cards Task and VASP were presented on a laptop. Auditory feedback was passed through an Edirol-UA-4FX audio capture sound card to control the level of auditory presentation (the output level was set at 3/10 of the dial). The auditory stimuli were presented to the participants using Sennheiser Headphones.
Procedures
The ordering of the experimental tasks was counterbalanced across participants.
Appraisals.
At the end of both the Cards Task and the VASP, participants rated, using visual analogue scales (VAS; 0–10), (a) how unusual, (b) how distressing, and (c) how threatening they had found the experiences, and their conviction in 7 appraisal items (see Appendix), ranging from 0 (do not agree at all) to 10 (totally agree). There were 5 “maladaptive” and 2 “adaptive” appraisal items. In the event that an appraisal item was endorsed (ie, any conviction rating greater than 0), the personal significance of each appraisal was assessed by a further probe asking whether the task “works the same for everybody” or “is specific to them” (Yes/No answer). Finally, participants were asked whether the experience was related to their own experiences (assessing “incorporation”).
Response Styles.
Following the appraisal ratings, participants were asked to rate the likelihood that they would endorse each of 8 response styles (see Appendix) in the event that the experience began to occur regularly (VAS ranging from 0–10; “not at all likely” to “extremely likely”). There were 6 maladaptive and 2 adaptive response style items.
At the end of the study, individuals were debriefed and provided with an honorarium. Completion time for the study varied between 75 and 120 min. No participant reported any adverse effects following participation in the study either at the time or at a 1-week follow-up.
Statistical Analysis
Data analysis was carried out using SPSS for Windows (version 15.0, 2006). Independent t tests or Mann-Whitney tests were used for group comparisons depending on whether assumptions for the use of parametric tests were met. Mean ratings for adaptive and maladaptive appraisals—and for ratings of “striking/threatening/distressing” and “specific to self” items—on both tasks were positively skewed and the variances differed considerably between groups. No transformations succeeded in making the variables normally distributed. The mean ratings for adaptive and maladaptive response styles on both tasks did not violate the assumptions of parametric statistics. Post hoc analyses were conducted to explore individual appraisal items and response styles using Mann-Whitney and independent t tests, respectively.
Results
Group Differences on AANEX Inventory
As shown in table 2, there were no differences between the groups on AANEX Inventory (Past or Current) overall score, indicating that both groups were equivalent in terms of psychotic-like experiences. On the individual factors, there were no differences on “First-Rank symptoms,” “Meaning–Reference,” or “Dissociative–Perceptual” scores. Replicating previous findings,13,14 the C group scored higher on the “Cognitive–Attention” factor and lower on the “Paranormal–Hallucinatory” factor than the NC group.
Table 2.
The AANEX Inventory13 Scores by Group
| Scores | Clinical (C) (N = 28) | Nonclinical (NC) (N = 34) |
|---|---|---|
| Mean (SD) | Mean (SD) | |
| Meaning/reference (Total) | 15.0 (5.0) | 17.2 (5.1) |
| “Paranormal–hallucinatory” (Total) | 10.2 (3.4) | 13.4 (2.9)** |
| “Cognitive–attention” (Total) | 9.1 (3.6)* | 6.9 (2.6) |
| “Dissociative–perceptual” (Total) | 8.7 (3.0) | 8.8 (2.6) |
| First-rank symptoms (Total) | 16.6 (4.5) | 15.4 (4.0) |
| AANEX total of past experiences | 32.0 (6.4) | 33.2 (6.3) |
| AANEX current experiences | 27.5 (6.6) | 28.5 (5.9) |
| Total AANEX score | 59.4 (11.9) | 61.7 (11.8) |
Note: *P < .01, t(60) = 2.91; **P < .001, t(60) = −3.95. AANEX, Appraisals of Anomalous Experiences interview.
Appraisals and Ratings of Experience
Cards Task.
Six NC (17.7%) and no C participants correctly identified the nature of the card trick (ie, the replacement of the entire first set of cards), and their data were excluded. One C participant had seen the Cards Task before and did not complete the task, leaving 27 C and 28 NC participants.
The C group scored significantly higher than the NC group on how striking (C: mean = 5.6 (SD = 3.7); NC: mean = 3.1 (SD = 3.2); U = 228, P =.01), distressing (C: mean = 1.3 (SD = 2.1); NC: mean = 0.0 (SD = 0.0); U = 224, P < .001), and threatening (C: mean = 1.2 (SD = 2.6); NC: mean = 0.1 (SD = 0.4); U = 302, P < .05) they found the experience.
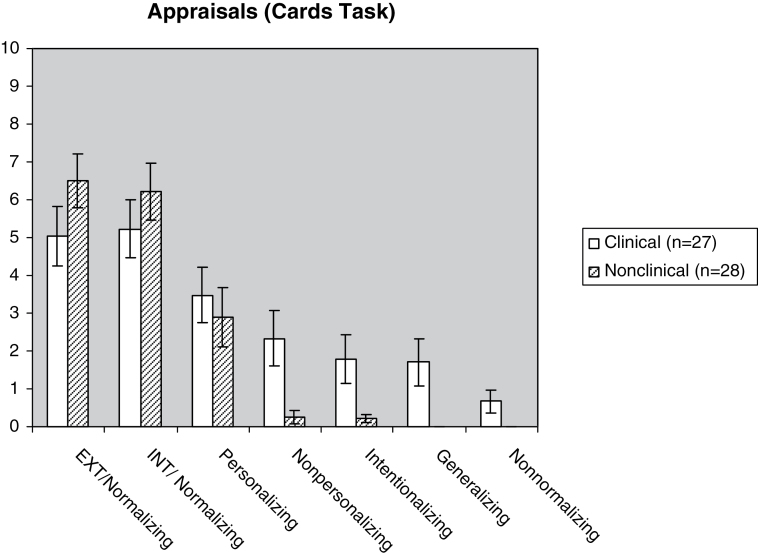
There were no differences between the C group (mean = 5.2, SD = 3.4) and the NC group (mean = 6.4, SD = 3.0) in adaptive appraisals (U = 302.5, P = .2). In contrast, the C group (mean = 2.0, SD = 2.3) scored significantly higher than the NC group (mean = 0.7, SD = 0.8) on maladaptive appraisals (U = 245, P = .02). Conviction ratings of individual appraisals in the 2 groups are presented in figure 1. Post hoc analyses showed that 3 of the 5 maladaptive appraisals (“Internal/Non normalizing”: P = .02; “External/Non personalizing”: P = .01; “External/ Generalizing”:P = <.01) were significant, in the predicted direction, but neither adaptive appraisal was significant.
Fig. 1.
Group differences in appraisals on the Cards Task (error bars represent SE).
VASP task.
Eleven C (39%) and 11 NC (32%) participants gave spontaneous appraisals that correctly identified the experimental setup. Their data were excluded, leaving 17 C and 23 NC participants.
There were no differences between the 2 groups on how striking (C: mean = 3.2 (SD = 3.2); NC: mean = 3.3 (SD = 2.8); U = 183.5, P = .7), distressing (C: mean = 1.5 (SD = 2.0); NC: mean = 1.2 (SD = 2.2); U = 175, P = .5), and threatening (C: mean = 1.7 (SD = 3.3); NC: mean = 0.5 (SD = 1.2); U = 182.5, P = .6) they found the experience.
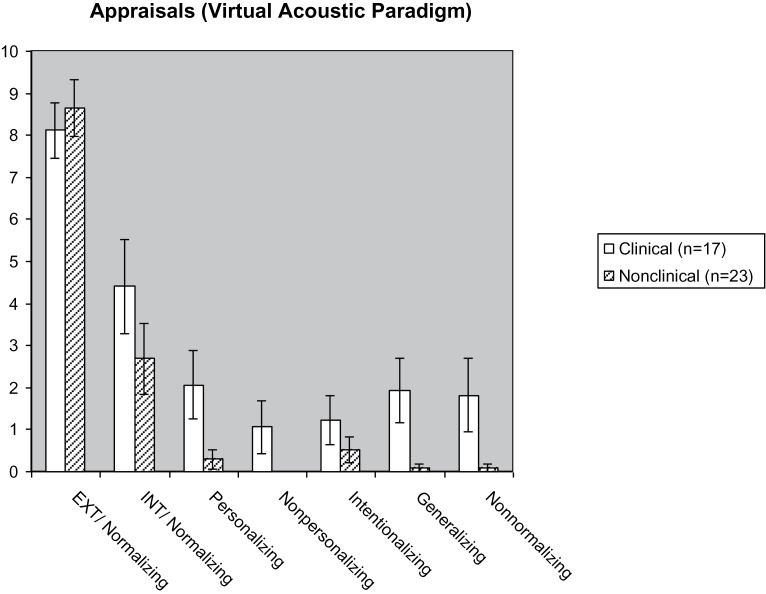
There were no differences between the C group (mean = 6.3, SD = 2.9) and the NC group (mean =5.7, SD = 2.9) in adaptive appraisals (U =181, P = .68). In contrast, the C group (mean = 1.6, SD = 1.9) scored significantly higher than the NC group (mean = 0.2, SD = 0.5) on maladaptive appraisals (U = 96.5, P = .002). Conviction ratings in individual appraisals in the 2 groups are presented in figure 2. Post hoc analyses showed that 4 out of the 5 maladaptive appraisals were significant in the predicted direction (“ External/ Personalizing”: P = .03; “ Internal/Non normalizing”: P = .03; “External/Non personalizing”: P = .04; “External/ Generalizing”: P = <.01), but neither adaptive appraisal was significant.
Fig. 2.
Group differences in appraisals on the Virtual Acoustic Space Paradigm (error bars represent SE).
Personally Significant Appraisals.
There were strong trends for the C group (Cards Task: mean = 20.5, SD = 38.1; VASP: mean = 32.5, SD = 42.5) to score higher on appraisals regarding personal significance than the NC group (Cards Task: mean = 4.8, SD = 19.70; VASP: mean = 10.9, SD = 30.0) on both the Cards Task (U = 305.5, P = .058) and the VASP (U = 142, P = .054).
“Incorporation.”
Fisher’s exact tests showed that the members of the C group were significantly more likely to incorporate the experience of both tasks with their own anomalous experiences (Cards Task: χ 2 (1) = 12.1, P < .001; VASP: χ 2 (1) = 8.3, P < .01). On the Cards Task, no individuals in the NC group incorporated this experience, compared to 9 (36.0%) in the C group, and on the VASP, 1 (4.3%) NC—compared to 7 (41.2%) C participants—incorporated the experience.
Response Styles
No participant was excluded for the response style analyses (apart from the C participant who did not complete the Cards Task) because those who had guessed the experimental procedures could still make a judgment on how they would respond should such an experience start to occur on a frequent basis.
As shown in table 3, there were significant differences between the groups on both adaptive and maladaptive response styles for both tasks in the predicted directions.
Table 3.
Group Differences for Response Styles on Each of the 2 Experimental Tasks
| VASP | Cards Task | |||||
|---|---|---|---|---|---|---|
| Clinical (C) (N = 28) | Nonclinical (NC) (N = 34) | t (P value) | Clinical (C)(N = 27) | Nonclinical (NC) (N = 34) | t (P value) | |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||
| Response styles | ||||||
| Adaptive response styles | 5.2 (2.3) | 6.7 (2.4) | −2.6 (.01) | 5.1 (2.4) | 6.7 (2.2) | −2.7 (<.01) |
| Decentering (reappraisal) | 5.5 (3.6) | 8.3 (2.9) | −3.3 (<.01) | 6.6 (3.3) | 7.8 (3.7) | −1.4 (.2) |
| Decentering (mindfulness) | 4.9 (3.7) | 5.2 (3.9) | −0.4 (.7) | 3.6 (3.13) | 5.6 (3.6) | −2.2 (.03) |
| Maladaptive response styles | 4.9 (1.8) | 3.9 (1.6) | −2.4 (.02) | 4.6 (2.0) | 2.8 (2.0) | 3.5 (.001) |
| Active resistance (distraction) | 5.8 (3.7) | 3.8 (3.7) | 2.1 (.04) | 5.0 (3.5) | 1.7 (3.0) | 4.0 (<.001) |
| Active resistance (control) | 5.3 (3.5) | 6.2 (3.8) | −1.0 (.3) | 4.8 (3.7) | 3.4 (4.0) | 1.4 (.2) |
| Active engagement (immersion) | 6.2 (3.8) | 5.9 (3.7) | 0.3 (.7) | 4.9 (3.8) | 5.2 (4.1) | −0.3 (.8) |
| Active engagement (rumination) | 4.9 (3.7) | 3.2 (3.4) | 1.9 (.07) | 5.9 (3.7) | 1.8 (2.9) | 5.0 (<.001) |
| Passive (trusting) | 4.4 (4.1) | 3.1 (3.5) | 1.4 (.2) | 3.7 (3.6) | 2.4 (3.2) | 1.6 (.1) |
| Passive (giving up) | 3.00 (3.2) | 1.3 (2.7) | 2.3 (.03) | 3.0 (3.5) | 2.1 (3.4) | 1.0 (.3) |
Note: Bold face denotes significant findings. VASP, Virtual Acoustic Space Paradigm.
Post hoc tests on individual response styles in the Cards Task showed that the C group had significantly higher ratings on “Active engagement/rumination” and “Active resistance/ distraction ” and lower ratings on “Decentering/ mindfulness ” than the NC group. On the VASP, the C group scored higher on “Passive/ giving up” style and “Active resistance/distraction ” and lower on “Decentering/ reappraisal ” than the NC group.
Discussion
Summary of Main Findings
The 2 groups were comparable in terms of the presence of overall anomalous experiences, as measured by the AANEX Inventory.13 As predicted, they differed on their appraisals of experimentally induced experiences, with the C group being more likely than the NC group to endorse maladaptive appraisals on both tasks. The former were more likely to incorporate the experimental setup into their ongoing experiences and showed strong trends in rating the experience as more personally significant. They also appraised the Cards Task as more salient, distressing, and threatening. The 2 groups were also found to differ on response styles on both tasks, with the C group more likely to endorse maladaptive response styles, whereas the NC group was more likely to endorse adaptive response styles. These findings provide support for cognitive models of psychosis,4–6 which argue that appraisals and response styles play a key role in the transition to need for care.
Individual Appraisal and Response Style Items
The C group was more likely than the NC group to endorse the following maladaptive appraisals: External/ generalizing (both tasks), Internal/ non normali zing (both tasks), External/ non personali zing (both tasks), and External/ personali zing (VASP only). In light of the putative role of negative schematic models of the self and the world in cognitive models of psychosis,4,29 it was of interest that unusual experiences with even relatively neutral content can cue in self-denigrating (ie, “something wrong with me”) appraisals in the C group, in addition to being related to wider conspiracies. Therefore, although the results from the current study provide support for the proposition that the C group is more likely to have externalizing and personalizing appraisals (as postulated by one influential cognitive model),4 they also point to a potential role for a wider range of maladaptive appraisals when faced with anomalous experiences.
With reference to individual response styles, the C group was more likely than the NC group to endorse the “Active engagement/rumination” (Cards Task), “Passive/ giving up” style (VASP), and “ Active resistance/ distraction” (both tasks). The findings with reference to rumination are consistent with a growing acknowledgment of the relevance of anxiety and worry processes in clinical psychosis.30 The fact that the C group was more likely to endorse both the “Active resistance/ distraction” style and the “Passive/ giving up” style, following the VASP, is consistent with the finding that voices perceived as powerful and malevolent are at first resisted but ultimately submitted to or appeased.31 In contrast, the NC group was more likely to endorse a “Decentering ” response style characterized by either mindfulness or reappraisal, thus supporting the normalizing and decentering rationale of Cognitive Behavioral Therapy32 and third-wave therapies for psychosis.33
Limitations and Future Research
The findings reported in this study need to be viewed in the context of a number of limitations. Given the cross-sectional nature of the study, it is not possible to determine whether any group differences in appraisal or response style has a causal influence with respect to the transition to the need for care stage. The rating scales for appraisals and responses to the tasks had strong face validity, but their reliability and validity when used by participants as single-item assessments of complex constructs were unknown. Hence, although the hypothesis that appraisals and responses do meaningfully differ was supported, it is harder to interpret the magnitudes of group differences for specific appraisals/responses, which may reflect scale performance as much as true differences.
The results suggest that the Cards Task may have had more ecological validity than the VASP as a symptom analogue; indeed, the fact that a number of individuals guessed the experimental setup resulted in a lower-than-optimal sample size. Future use of the VASP should focus on increasing the emotional salience of the task in line with the proposition that external misattribution bias on both immediate and real-time tasks appears most evident for items of emotional content.34 In addition, the relationship between “on-line” appraisals of unusual experiences and broader aspects of social cognition is an important area for future research in light of reported deficits in contextual processing and social inference within clinical samples.35
The NC group had higher IQ than the C group, intimating that IQ may be a significant factor in how individuals appraise their experiences. More research investigating the role of cognitive resources in equipping individuals with the ability to respond adaptively to persistent anomalous experiences is indicated. Similarly, the relationship between aversive life experiences and maladaptive appraisals warrants further research because there is preliminary evidence of a cognitive route between victimization and psychosis.14,36
Finally, there were significant differences between the 2 groups on a number of further demographic and clinical variables (age at onset of experiences, marital status, employment, ethnicity, current anxiety, and depression). The possibility that these may have played a role in the reported differences on appraisals and response styles cannot be excluded. However, the demographic and clinical differences that were found are likely to be either intrinsic to group status (such as impaired functioning and distress) and/or reflecting the risk factors inherent in the development of need for care (such as low IQ or social isolation). The view that ANCOVA (analysis of covariance, commonly employed in psychological research) can be used to achieve the goal of “controlling for” real group differences on a covariate has been condemned, and it has been argued that no analytic method can achieve this goal.37 This caveat extends to any variable that is related to group status. Future research could employ an additional C group (with high anxiety and depression but without anomalous experiences) to exclude the possibility that the observed differences simply reflect increased anxiety and depression in the C group. Use of a healthy control group would also be helpful to determine standard reactions to the experimental tasks.
Clinical Implications
The current study has provided some support for psychological interventions that target maladaptive appraisals (eg, self-denigrating and conspiratorial appraisals) and unhelpful modes of responding (such as rumination). A framework for response styles grounded in previous research that achieved face validity for clinicians and appeared meaningful to C and NC participants (see Appendix for further details) has been presented. It has been suggested that the adoption of a more explicit model of coping may be useful with respect to integrating research findings and clarifying clinical implications.38
In addition to the Cards Task, which already forms part of a Metacognitive Training package,39 the VASP may also have a range of potential clinical applications. First, following assessment of the content and topography of their voices, the client could be supported to develop an analogue of his/her own voice activity. In addition to the possibility of habituation to voice content, this active process may also be relevant to the individual’s sense of power and control in the context of the voice content. Use of the VASP in this manner would be consistent with treatments of voices that emphasize acceptance of the voice (rather than avoidance), followed by disengagement (such as Acceptance and Commitment Therapy for voices).40 Finally, given inconsistent research findings regarding the benefits of distraction, the VASP could be used to examine the relative efficacy of acceptance- vs distraction-based response styles.
Conclusions
This study has shown differences in appraisals and response styles in individuals experiencing psychotic experiences with and without need for care, on experimental tasks inducing anomalous experiences. The findings are consistent with cognitive models of psychosis. They further suggest that a range of maladaptive appraisals, rather than simply external appraisals, may be relevant and that benign outcomes may be associated with decentering response styles, whereas need for care status may be associated with rumination and distraction.
Funding
National Institute of Mental Health (NIHR) Biomedical Research Centre for Mental Health, King’s Health Partners (E.P. and P.G.).
Acknowledgments
The authors have declared that there are no conflicts of interest in relation to the subject of this study.
Appendix
Assessment of Appraisals
Statements representing 7 different appraisals for the tasks were created, based on the categories employed in earlier studies.13,17 Items were rated on a scale of 0 (“not at all”) to 10 (“totally”) in terms of how much the participant believed the statements to be a true explanation of the anomalous experience. The 7 types were grouped into adaptive and maladaptive appraisals by calculating a mean score for each:
Adaptive Appraisals
1. External– Normalizing: an externalizing appraisal that the explanation for the experience lies in some benign feature of the experimental setup.
“It is just a simple card puzzle” (Card task);
“It is part of the study and involves a prerecorded voice” (VASP).
2. Internal– Normalizing: appraisals in terms of the normal, natural range of human capacities, experiences, or processes.
“It is because of the way my mind works, just part of normal human experience” (both tasks).
Maladaptive Appraisals
1. External– Personalizing: appraising that the anomalous experiences are caused by another person/group of people.
“It is not the computer which guessed; there is someone involved in this” (Card Task).
“Someone was speaking my thoughts out loud” (VASP).
2. External–Non personalizing: appraised as being externally caused but not attributed to another person; included in this category are non normalizing appraisals featuring some aspect of the machine/equipment, paranormal, and spiritual appraisals.
“It works because the system is able to read people’s minds.” (Card Task);
“There was a spirit or some kind of entity in the room” (VASP).
3. External– Intentionalizing: appraising that the anomalous experiences are caused by another person with reference to a specific intention on the part of the other person.
“It was done on purpose to trick me, or make me look stupid” (both tasks).
4. External– Generalizing: interpretations based on the relationship between the experiences and a wider conspiracy.
“It is a trick that is part of a bigger conspiracy” (both tasks).
5. Internal–Non normalizing: interpretations in terms of illness, disorder, or any (nonnormalizing) material, internal attribution of cause.
“This means that something is wrong with me” (both tasks).
Assessment of Response Styles
A system of categorizing response styles was devised, building on the categories used in earlier work13 while integrating dimensions of responding noted elsewhere in the literature (eg, “active/passive” and “acceptance/rejection” dimensions).41 Once again, the items were rated on a scale of 0 (“not at all”) to 10 (“totally”), representing endorsement of the individual response style. Items were then divided into response styles viewed as adaptive vs maladaptive, and mean scores were calculated for each.
Adaptive
1. “Decentering style”
a. Active acceptance and disengaging (Mindful response style)—overlapping with “Neutral response.”13
“I would let the experiences come and go without getting involved with them” (both tasks).
b. Active cognitive reappraisal of experiences (“Appraisal–Decentering”13;
“I would try to think of a sensible explanation of the experiences/find different way of thinking about them” (both tasks).
Maladaptive
2. “ Active resistance”—analogous to “resistance”6 and mirroring “resistance coping.”15 Includes the following:
a. Avoidance/distraction;
“I would find ways to escape these experiences or take my mind off them” (both tasks).
b. Attempts to control the experience.
“I would find ways to control these things or stop them from happening” (both tasks).
3. “ Active engagement”–including the following:
a. Immersion in experience (including active listening and compliance)—seen as analogous to “engagement,”6 overlapping with “immersion” style,13 and “symptomatic coping.”16
“I would listen closely to these voices” (VASP).
“I would try to get into these experiences as much as possible” (Cards Task).
b. Rumination (nondecentering).13
“I would worry about the experiences, running them over and over in my mind, trying to get to the bottom of what they mean” (both tasks).
4. “ Passive style”–including the following:
a. Trusting in external sources (eg, trusting in God)—this mirrors “passive coping”15 and “passive, hopeful, acceptance.”41
“I would trust that someone/something would sort this out for me” (both tasks).
b. “Giving up”—(corresponding to “passive, despairing acceptance.”41
“I would give up—there is nothing I can do about it” (both tasks).
Assessing Face Validity of Individual Items
Individual items were devised to serve as exemplars for each category, for both the appraisals and the response styles. All items were submitted for inspection to a panel of 5 experts in the field. The experts were asked to (a) match the items with the category of appraisal/response styles and (b) rate the goodness of fit for each item to the category of appraisal/response style (maximum score = 10). Each of the 5 experts coded 100% of the items into the correct category for appraisals. The range of “Average goodness of fit” scores across the 5 experts was 5.8 (External/Intentionalizing) to 10 (Internal/nonnormalizing), with an average score of 8.5. Goodness of fit was considered adequate for each item with minor changes made, as recommended by the panel, to 2 items (External– Intentionalizing and the External–Normalizing item on the VASP). With reference to response styles, each of the 5 experts again coded 100% of the items into the correct category. The average goodness of fit ranged from 8.5 to 9.9, with an overall average of 9.1 per item. Goodness of fit was considered adequate for each item with no changes deemed to be necessary.
References
- 1. van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. 2009;39:179–195 [DOI] [PubMed] [Google Scholar]
- 2. Diederen KM, Daalman K, de Weijer AD, et al. Auditory hallucinations elicit similar brain activation in psychotic and nonpsychotic individuals. Schizophr Bull. 2012;38:1074–1082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gaynor K, Ward T, Garety P, Peters E. The role of safety-seeking behaviours in maintaining threat appraisals in psychosis. Behav Res Ther. 2013;51:75–81 [DOI] [PubMed] [Google Scholar]
- 4. Garety PA, Kuipers E, Fowler D, Freeman D, Bebbington PE. A cognitive model of the positive symptoms of psychosis. Psychol Med. 2001;31:189–195 [DOI] [PubMed] [Google Scholar]
- 5. Morrison AP. The interpretation of intrusions in psychosis: an integrative cognitive approach to hallucinations and delusions. Behav Cogn Psychoth. 2001;29:257–276 [Google Scholar]
- 6. Chadwick P, Birchwood M. The omnipotence of voices. A cognitive approach to auditory hallucinations. Br J Psychiatry. 1994;164:190–201 [DOI] [PubMed] [Google Scholar]
- 7. Jackson MC. Benign schizotypy? The case of spiritual experience. In: Claridge GS, ed. Schizotypy: Relations to Illness and Health. Oxford, UK: Oxford University Press; 1997. [Google Scholar]
- 8. Jackson MC, Fulford KWM. Spiritual experience and psychopathology. Phil Psych Psychol. 1997;1:41–65 [Google Scholar]
- 9. Peters E, Day S, McKenna J, Orbach G. Delusional ideation in religious and psychotic populations. Br J Clin Psychol. 1999;38:83–96 [DOI] [PubMed] [Google Scholar]
- 10. Peters ER, Joseph SA, Garety PA. Measurement of delusional ideation in the normal population: introducing the PDI (Peters et al. Delusions Inventory). Schizophr Bull. 1999;25:553–576 [DOI] [PubMed] [Google Scholar]
- 11. Lincoln TM. Relevant dimensions of delusions: continuing the continuum versus category debate. Schizophr Res. 2007;93:211–220 [DOI] [PubMed] [Google Scholar]
- 12. Sisti D, Rocchi MB, Siddi S, et al. Preoccupation and distress are relevant dimensions in delusional beliefs. Compr Psychiatry. 2012;53:1039–1043 [DOI] [PubMed] [Google Scholar]
- 13. Brett CM, Peters EP, Johns LC, Tabraham P, Valmaggia LR, McGuire P. Appraisals of Anomalous Experiences Interview (AANEX): a multidimensional measure of psychological responses to anomalies associated with psychosis. Br J Psychiatry. 2007;51(suppl):s23–s30 [DOI] [PubMed] [Google Scholar]
- 14. Lovatt A, Mason O, Brett C, Peters E. Psychotic-like experiences, appraisals, and trauma. J Nerv Ment Dis. 2010;198:813–819 [DOI] [PubMed] [Google Scholar]
- 15. Farhall J, Gehrke M. Coping with hallucinations: exploring stress and coping framework. Br J Clin Psychol. 1997;36 (Pt 2):259–261 [DOI] [PubMed] [Google Scholar]
- 16. Bak M, Myin-Germeys I, Hanssen M, et al. When does experience of psychosis result in a need for care? A prospective general population study. Schizophr Bull. 2003;29:349–358 [DOI] [PubMed] [Google Scholar]
- 17. Linney YM, Peters ER. The psychological processes underlying symptoms of thought interference in psychosis. Behav Res Ther. 2007;45:2726–2741 [DOI] [PubMed] [Google Scholar]
- 18. Andreasen NC. The Scale of the Assessment of Positive Symptoms (SAPS). Iowa City, IA: University of Iowa; 1984. [Google Scholar]
- 19. Yung AR, McGorry PD. The prodromal phase of first-episode psychosis: past and current conceptualizations. Schizophr Bull. 1996;22:353–370 [DOI] [PubMed] [Google Scholar]
- 20. Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 21. Beck AT, Steer RA. Manual for the Beck Anxiety Inventory. San Antonio, TX: Psychological Corporation; 1990. [Google Scholar]
- 22. Fydrich T, Dowdall D, Chambless DL. Reliability and. validity of the Beck Anxiety Inventory. J Anxiety Disord. 1992;6:55–61 [Google Scholar]
- 23. Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56:893–897 [DOI] [PubMed] [Google Scholar]
- 24. Ammons R, Ammons C. Quick Test. Missoula, MT: Psycholo gical Test Specialists; 1962. [Google Scholar]
- 25. Frith CD, Leary J, Cahill C, Johnstone EC. Performance on psychological tests. Demographic and clinical correlates of the results of these tests. Br J Psych. 1991; (suppl):26–29 [PubMed] [Google Scholar]
- 26. Wightman FL, Kistler DJ. Headphone simulation of free-field listening. I: Stimulus synthesis. J Acoust Soc Am. 1989; 85:858–867 [DOI] [PubMed] [Google Scholar]
- 27. Hunter MD, Griffiths TD, Farrow TF, et al. A neural basis for the perception of voices in external auditory space. Brain. 2003;126:161–169 [DOI] [PubMed] [Google Scholar]
- 28. Peters E, Smedley N, Tabraham P. Do deluded individuals jump to perceptions, as well as to conclusions? Schizophr Bull. 2005;31:371 [Google Scholar]
- 29. Fowler D, Hodgekins J, Garety P, et al. Negative cognition, depressed mood, and paranoia: a longitudinal pathway analysis using structural equation modeling. Schizophr Bull. 2012;38:1063–1073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Startup H, Freeman D, Garety PA. Persecutory delusions and catastrophic worry in psychosis: developing the understanding of delusion distress and persistence. Behav Res Ther. 2007;45:523–537 [DOI] [PubMed] [Google Scholar]
- 31. Birchwood M, Chadwick P. The omnipotence of voices: testing the validity of a cognitive model. Psychol Med. 1997;27:1345–1353 [DOI] [PubMed] [Google Scholar]
- 32. Peters E, Landau S, McCrone P, et al. A randomised controlled trial of cognitive behaviour therapy for psychosis in a routine clinical service. Acta Psychiatr Scand. 2010;122:302–318 [DOI] [PubMed] [Google Scholar]
- 33. Chadwick P, Hughes S, Russell D, Russell I, Dagnan D. Mindfulness groups for distressing voices and paranoia: a replication and randomized feasibility trial. Behav Cogn Psychother. 2009;37:403–412 [DOI] [PubMed] [Google Scholar]
- 34. Ditman T, Kuperberg GR. A source-monitoring account of auditory verbal hallucinations in patients with schizophrenia. Harv Rev Psychiatry. 2005;13:280–299 [DOI] [PubMed] [Google Scholar]
- 35. Chung YS, Mathews JR, Barch DM. The effect of context processing on different aspects of social cognition in schizophrenia. Schizophr Bull. 2011;37:1048–1056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Gracie A, Freeman D, Green S, et al. The association between traumatic experience, paranoia and hallucinations: a test of the predictions of psychological models. Acta Psychiatr Scand. 2007;116:280–289 [DOI] [PubMed] [Google Scholar]
- 37. Miller GA, Chapman JP. Misunderstanding analysis of covariance. J Abnorm Psychol. 2001;110:40–48 [DOI] [PubMed] [Google Scholar]
- 38. Farhall J, Greenwood KM, Jackson HJ. Coping with hallucinated voices in schizophrenia: a review of self-initiated strategies and therapeutic interventions. Clin Psychol Rev. 2007;27:476–493 [DOI] [PubMed] [Google Scholar]
- 39. Moritz S, Woodward TS. Metacognitive training in schizophrenia: from basic research to knowledge translation and intervention. Curr Opin Psychiatry. 2007;20:619–625 [DOI] [PubMed] [Google Scholar]
- 40. Bach P, Hayes SC. The use of acceptance and commitment therapy to prevent the rehospitalization of psychotic patients: a randomized controlled trial. J Consult Clin Psychol. 2002;70:1129–1139 [DOI] [PubMed] [Google Scholar]
- 41. O’Sullivan K. Dimensions of coping with auditory hallucinations. J Mental Health. 1994;3:351–361 [Google Scholar]