Abstract
Growing evidence shows that early mobilization of patients in the intensive care unit (ICU) is a safe and cost-effective strategy to improve patient outcomes. However, in ICUs where early mobilization has not been practiced, its adoption requires culture change by the multidisciplinary team, including physical therapists, nurses, respiratory therapists, and physicians. We describe a physical therapist–led program to introduce such changes in a medical-surgical and a cardiovascular ICU. Interdisciplinary and multidisciplinary meetings and education sessions informed critical care team members about early mobilization and encouraged knowledge sharing for safety and effectiveness. A lead physical therapist was appointed to advocate for early mobility and developed solutions to overcome the identified barriers. After the initiation of this program, the number of ICU patients receiving physical therapy evaluations increased from 364 in 2011–2012 to 542 in 2012–2013. In this article, we describe our experience from 21 patients who underwent early mobilization. A physical therapist–led initiative can help establish an ICU culture that supports early mobilization, but the change is slow and requires interdisciplinary collaboration to identify and overcome barriers.
Having critically ill patients alert and engaged in progressive rehabilitation (e.g., passive range of motion, active range of motion/bed exercises, sitting at the edge of the bed, transfers) leading to mobilization, even while they require life support therapies, may reduce muscle atrophy and lead to improved strength and physical function (1). Several studies show that providing early physical therapy interventions in the intensive care setting can decrease hospital and/or intensive care unit (ICU) length of stay (LOS) (2–6). In a study by Clark and colleagues, the LOS was 2.4 days shorter (P = 0.02) after the implementation of their early mobility program (2). Titsworth et al's study determined that the monthly average LOS in the neurointensive care unit significantly decreased from 4.0 days prior to the intervention to 3.46 days after the intervention, a 13% difference (P < 0.004) (6). Active mobilization in the ICU has also been shown to increase functional mobility and strength (7–10) and to decrease complications such as venous thromboembolisms, pressure ulcers, and pneumonia (2, 11). In addition, there is some evidence that early mobilization programs can decrease costs of care and risk of readmission or death (4–6). Despite this evidence, early mobility programs in the ICU face significant barriers. Key among these is establishing a culture of open communication and multidisciplinary collaboration that is needed to support the coordination between physical therapists (PTs), physicians, nurses, and respiratory therapists (RTs) to safely and effectively conduct early mobilization. In the studies cited above, the early mobility programs were organized by the hospital administration, nursing staff, physicians, and the rehabilitation department. We describe and provide some data on a PT-led initiative to establish an early mobilization program in one hospital's medical-surgical and cardiovascular ICUs.
METHODS
Baylor All Saints Medical Center at Fort Worth is a 525-bed acute care hospital in Fort Worth, Texas. It is a private, not-for-profit, urban, full-service hospital, providing a broad range of medical services, including cardiology, transplantation, neurosciences, oncology, and women's services. The facilities include a 16-bed medical-surgical ICU and a 15-bed cardiac ICU in which the patient-to–registered nurse (RN) ratios are maintained at 1:1 or 2:1. The ICU has several intensivist groups, most of whom are pulmonologists. The specialties include neurosurgery, cardiovascular surgery, head and neck reconstruction surgery, and liver and kidney transplantation. The patient population in the ICU and cardiac ICU includes those with diagnoses such as pneumonia, sepsis, respiratory failure, diabetic ketoacidosis, myocardial infarction, heart failure exacerbations, and chronic obstructive pulmonary disease. One internal medicine physician rounds on all reconstructive head and neck patients. The PTs and RTs are contractors, and the nurses are staff. There is not a hierarchy among these disciplines.
Prior to implementation of this program, there was no protocol for ordering physical therapy for patients admitted to the ICUs. Rather, physical therapy orders were handled on an ad hoc basis. After receiving the orders, the PT performed chart reviews and contacted the nurses to determine if the patients were stable to participate in physical therapy services, using guidelines taken from a combination of nursing education courses the lead PT attended as well as literature and continuing education courses attended. These guidelines included a heart rate of 40–130 beats per minute; a systolic blood pressure < 180 mm Hg; a mean arterial pressure > 65 mm Hg; mechanical ventilation < 100 mm Hg; pulse oximetry >88%–90%; respiratory rate < 40 breaths per minute; mechanical ventilation settings of fraction of inspired oxygen < 0.60 and positive end-expiratory pressure <10; as well as alertness, ability to follow commands, and lack of agitation.
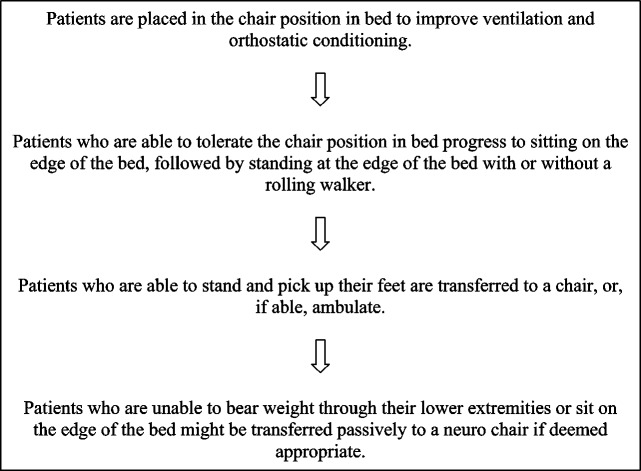
If a patient met these guidelines, he or she was evaluated and received physical therapy 3 to 5 times per week. Patients who were not stable enough to participate were assessed daily to determine their eligibility for participation in physical therapy. Physical therapy sessions were based on both the patients' previous level of function and their ability to participate on the day of the treatment session. Accordingly, exercises could be performed in the supine or chair position in bed, sitting on the edge of the bed, in the chair beside the bed, or standing. Figure 1 outlines the progression.
Figure 1.
Progression of physical therapy exercises for patients in the intensive care unit.
In May 2011, the physical therapy department initiated steps toward introducing early mobilization as standard practice in Baylor All Saints ICUs after a PT began to notice discrepancies in evidence and what was being practiced in the ICU. The PT found that it was acceptable to progressively mobilize patients who had undergone coronary artery bypass graft surgery but not other patients who seemed to meet criteria to participate in PT services. Often these patients were not even receiving orders for PT. Recognizing the importance of interdisciplinary communication and collaboration for early mobilization, the focus was on establishing a culture to support this goal, while simultaneously educating physicians, nurses, RTs, and PTs on both the benefits of early mobilization in the ICU and on factors within each other's domains that needed to be considered in relation to mobilization of critically ill patients.
We began by inviting the ICU nurse manager to our departmental meeting, who then invited us to the critical care quality meetings. We attended one critical care quality meeting and at the next meeting presented early mobility information. While continuing to attend the critical care quality meetings, we invited other team members to our departmental meetings. We held 3 meetings over a 6-month period and included the cardiac ICU nurse manager, who provided education on reading electrocardiography strips and the more common complications seen on the unit and answered questions about the equipment commonly in use in the cardiac ICU, critical lab values that needed to be considered in evaluating patients' readiness for mobilization, and perceived contraindications to activity/mobilization. Also present was an RT, who provided education on the different oxygen delivery devices used in the ICU and the ways they could be adjusted or converted for activity/mobilization. Additionally, there was a critical care nurse, who provided education on continuous dialysis and answered questions about mobilizing patients while they were on these machines.
Two months later, PT team members were invited to attend the monthly hospital critical care quality meetings and to provide education on early mobilization in this forum. As regular attendees of the meeting included an intensivist, nurse managers of both the medical-surgical and the cardiac ICUs, the hospital's critical care director, the respiratory therapy manager, and a nursing representative, PTs took this opportunity to educate the group on the existing evidence of the feasibility of and benefits associated with early mobility in the ICU.
Additionally, we organized phone conferences with other physical therapy departments within the hospital system to determine what the other facilities, namely Baylor University Medical Center at Dallas, Baylor Regional Medical Center at Grapevine, and Baylor Medical Center at Garland, were doing in their ICUs regarding mobility. Based on the information gathered, we made two important changes to our own department's functioning to better facilitate our aim of promoting early mobilization in the ICU. First, we stopped automatically placing patients transferred to one of the ICUs from the step-down units on a physical therapy “hold,” which meant we would wait for new orders from the physician. This was done after discussions with the PTs, nurses, and physicians revealed that some of the physicians were not aware that was the practice. One of the primary intensivists stated that he expected the therapists and nurses to discuss the case and make a clinical judgment about whether the patient could continue to participate. Second, we designated a lead PT for critical care. Third, the lead PT instituted ad hoc meetings with the ICU nurse managers in addition to the respiratory therapy manager, both together and separately, to provide further education on the importance of early mobility and gain their support. It was communicated to the managers that PTs often met resistance from nursing to provide interventions. The need to have PTs, RNs, and RTs work as a team to determine appropriateness for mobility and any needed oxygen or medication changes, i.e., decreasing sedation, changing the timing of pain medication, and increasing oxygenation support, was discussed in these meetings.
The meetings with the RTs and nurse managers focused on advocating early mobilization and the importance of collaboration across the entire critical care team in this process. We also discussed the changes made within the physical therapy department related to facilitating early mobilization and discussed the perceived barriers that were encountered.
Additionally, the lead PT was tasked with attending the multidisciplinary ICU rounds thrice weekly to advocate for early mobilization, request physical therapy orders for patients, and answer any questions the critical care team had about early mobilization. The lead PT also sought out and attended continuing education courses provided through various PT continuing education providers and taught by published, experienced critical care PTs. The courses provided information that was relevant to safely mobilizing ICU patients attached to multiple lines such as the ventilator, continuous dialysis, femoral lines, and arterial lines, as well properly monitoring their vital sign response to the dosage of activity. This material was passed on to the other PTs during the monthly critical care meeting we instituted in our department to review updates from the critical care quality meetings. The lead PT also provided education at critical care nursing staff meetings and nursing internship courses. The information addressed both the evidence supporting early mobilization in the ICU and the practical matters of when physical therapy orders should be requested, as well as what the PT was assessing/targeting when evaluating and treating a patient. Participation in all education sessions was voluntary.
During the middle of this process, the lead PT conducted an anonymous e-mail survey of the critical care nursing and respiratory therapy staff to identify their concerns regarding any perceived barriers to early mobility in the ICU, as well as opportunities to improve the quality of care the physical therapy department could address. The 9-question survey, which included yes/no questions and open-ended questions (Table 1), was administered to build an open culture of communication and collaboration. It enabled the PT to demonstrate to the ICU managers and RT managers that there were still issues that needed to be addressed to accomplish early mobility in the ICUs.
Table 1.
Survey questions
| 1. Do you think physical therapy should evaluate/screen all intensive care unit/cardiovascular intensive care unit patients? |
| 2. Do you feel comfortable getting patients into neuro chairs without physical therapy? |
| 3. Do you feel comfortable using the mechanical lifts without physical therapy? |
| 4. Do you get patients out of bed/ambulate without physical therapy if they are able? |
| 5. Do you think patients should be getting up on ventilators? |
| 6. What are the barriers to mobilizing patients on ventilators? |
| 7. What are the harmful effects of physical therapy working with patients in the intensive care unit? |
| 8. What can physical therapy do to improve communication with the RNs, MDs, respiratory therapists, patients, families, etc.? Please be specific. |
| 9. What can physical therapy do to improve patient care? Please be specific. |
Finally, in conjunction with our efforts to promote early mobility in the ICU, we reviewed a convenience sample of 21 charts for patients who had an ICU stay of 3 days or longer between May 2012 and May 2013 and who participated in physical therapy sessions in the ICU. The purpose of this review was to gain a sense of the characteristics of the patients receiving physical therapy interventions in the wake of our efforts to promote early mobilization in the ICU, as well as of the type of physical therapy intervention appropriate for these patients. We excluded patients who had head or neck reconstructive surgery as well as those who were discharged to hospice or died during their hospitalization. All data—including the number and type of physical therapy sessions, patient demographics, diagnoses, and clinical characteristics—were extracted from the electronic medical record and entered manually into a database created for this purpose. We also examined the total number of physical therapy evaluations performed on ICU patients during the first (April 2011–April 2012) versus the second (May 2012–May 2013) years of our intervention to determine if the number of PT orders had increased after some of the initiatives were implemented.
RESULTS
Findings from the shared meetings showed that inviting members of the critical care team to share their knowledge with the physical therapy department opened the door to the interdisciplinary communication and collaboration needed to support early mobilization in the ICU. The meetings also provided an important opportunity for members of the physical therapy department to raise any questions or concerns they had related to early mobilization in the ICU with the experts best able to address them. For example, we discussed whether there were policies against mobilizing patients with certain lines such as femoral or Quinton catheters as well as critical lab values that may affect PT interventions. In addition, we learned that often we were limiting our patients' mobility based upon outdated notions rather than current evidence. For example, in one instance, a PT did not see a patient because his potassium was critically low. Subsequently, the nurse manager educated the team that we should ask the nurses if the patient is receiving a K+ rider because, in most instances, the potassium had been replaced since that lab value was drawn. From findings from the phone conferences with the other physical therapy departments in the Baylor system, it was determined that there was a benefit in having a dedicated ICU therapist because this helped to build trust and confidence with the nursing and RT staff. It was also found that the other facilities utilized a tech more frequently to assist with treatments. Specifically, this led us to designate a critical care lead PT who was able to devote time to learning more about safely providing physical therapy in this context and to representing the physical therapy department and advocating for early mobilization at the critical care quality meetings and interdisciplinary rounds. We also changed department policy to stop placing patients participating in physical therapy on automatic hold if they were transferred to one of the ICUs.
Furthermore, in other findings, the results of instituting meetings with the respiratory therapy and critical care nurse managers led to the identification of important perceived barriers. During these meetings, the PT discussed with the managers the barriers to early mobilization, which included the nursing staff being resistant to PTs getting patients out of bed, working with patients who had multiple lines, and scheduling mobility with RTs and RNs when the patient was on a ventilator. The meetings were beneficial because the managers felt early mobility was important and were able to relay this message to the nursing and RT staff, resulting in a collaborative effort.
Survey results from 32 RTs and nurses uncovered some additional perceived barriers as well as some opportunities for improvement. Barriers that individuals indicated on the survey included the severity of patients' illness, safety concerns, time constraints, staff shortages, fear of pulling out lines and tubes, and the need for culture change. All respondents agreed that all ICU patients should be evaluated by PT. Twenty-eight percent of the respondents indicated that patients should mobilize on ventilators but cited the barriers mentioned above. It was determined after reading some of the responses to the survey that ongoing education needed to be provided, not only to address the barriers but also to inform the nursing staff of the role of physical therapy and the type of education we have. An interesting finding was that often the nurses felt as though PT was not progressing the patients adequately.
Results from our review of the 21 charts of patients who participated in physical therapy in the ICU are shown in Tables 2 and 3. From April 2011 to April 2012, 364 physical therapy evaluations were performed on patients admitted to the ICU. From May 2012 to May 2013, this number increased to 542.
Table 2.
Characteristics of 21 randomly selected patients who participated in physical therapy sessions in the medical-surgical or cardiac intensive care unit between May 2012 and May 2013
| Characteristic | Value |
|---|---|
| Age, mean ± SD | 60.4 ± 15.4 |
| Male | 10 (48%) |
| Ventilator | 12 (57%) |
| Non-Hispanic Caucasian | 12 (63%) |
| Body mass index, mean ± SD (kg/m2) | 30.0 ± 12.7 |
| Insurance | |
| Medicare | 12 (57%) |
| Private | 9 (43%) |
| Admitting unit | |
| Intensive care unit | 9 (43%) |
| Cardiovascular intensive care unit | 12 (57%) |
| Days in hospital, median (IR) | 10 (6, 18) |
| Days in ICU, median (IR) | 9 (5, 18) |
| Able to ambulate prior to ICU admission | 17 (81%) |
| Severity criteria as of day 3 of ICU stay | |
| On a ventilator | 7 (33%) |
| Postoperative | 7 (33%) |
| Received continuous renal replacement therapy | 2 (10%) |
| On a vasopressor | 9 (43%) |
| Unable to follow commands | 5 (26%) |
ICU indicates intensive care unit; IR, interquartile range; SD, standard deviation.
Table 3.
Characteristics of physical therapy sessions conducted with the 21 randomly selected patients who participated in physical therapy sessions in the medical-surgical or cardiac intensive care unit between May 2012 and May 2013
| Description | Any episode | Median (IR), if any |
|---|---|---|
| Duration in minutes, median (IR) | – | 49 (35, 80) |
| Median total number of physical therapy sessions (IR) | – | 2 (1, 3) |
| Day of first exercise session after critical care admission | – | 3 (2, 6) |
| Episodes of passive range of motion (patient did not participate) | 3 (14%) | 1 (1, 6) |
| Episodes of active exercise sessions with lower extremities | 9 (43%) | 2 (1, 3) |
| Episodes of sitting on edge of bed | 16 (76%) | 1 (1, 2) |
| Episodes of standing | 15 (71%) | 1 (1, 2) |
| Episodes of transferring to chair by weight bearing through lower extremities | 8 (38%) | 1 (1, 1.5) |
| Episodes of ambulating | 6 (29%) | 1.5 (1, 3) |
| Episodes of neuro chair transfer (passive) | 0 | – |
IR indicates interquartile range.
DISCUSSION
The physical therapy department at Baylor All Saints Medical Center at Fort Worth initiated and led a series of education sessions and discussions intended to establish a culture of interdisciplinary communication and collaboration to support the use of early mobilization in its medical-surgical and cardiac ICUs. Through these efforts, we identified important perceived barriers and concerns about early mobilization (e.g., concerns for safety with critically ill patients who have multiple lines, having enough staffing, needing multidisciplinary collaboration, and accounting for educational needs and the time required) across multiple disciplines, which we were able to start addressing through education and training involving nurses, RTs, PTs, and intensivists.
Previous studies have shown early mobility protocols to improve ICU patients' outcomes and decrease the costs associated with their care (4–6, 12). They have also identified barriers at the organizational level to implementing early mobility protocols, including a need for both institutional and project leadership; additional staffing and equipment; increased physician referrals for physical therapy closer to patient ICU admission; and management of patients' pain, delirium, and tolerance for activity and safety (13, 14). We examined the perceived barriers and concerns from the perspective of the frontline critical care staff—nurses, RTs, and PTs. The barriers found here were similar to those described in other research, including staffing needs and multidisciplinary collaboration, but also included safety concerns, educational needs, and the amount of time it takes to mobilize patients on multiple lines (12, 15, 16).
Our review of the 21 patients who participated in physical therapy sessions in the ICU provides other physical therapy departments that want to implement an early mobility program some idea of the kinds of patients and the type of session they can expect. Significant proportions of the participating patients were on ventilators or continuous dialysis, meaning that PTs need to plan for sessions that accommodate the restrictions these pieces of equipment impose. We also found that most patients were able to participate in at least some sessions sitting on the edge of the bed or standing next to the bed; a surprising proportion were also able to transfer to a chair or ambulate during some sessions. Through this process, it was found that if given the time for the patient to adjust to positional changes such as supine to sit, sit to stand, and so forth, these patients could progress further and tolerate more activity. This is important information, as PTs unfamiliar with the critical care setting might be hesitant to conduct such sessions, and while caution is obviously the watchword in this context, in achieving the full benefits of early mobility, avoiding “underchallenging” patients might be almost as important as avoiding “overchallenging” them.
References
- 1.Fan E, Zanni JM, Dennison CR, Lepre SJ, Needham DM. Critical illness neuromyopathy and muscle weakness in patients in the intensive care unit. AACN Adv Crit Care. 2009;20(3):243–253. doi: 10.1097/NCI.0b013e3181ac2551. [DOI] [PubMed] [Google Scholar]
- 2.Clark DE, Lowman JD, Griffin RL, Matthews HM, Reiff DA. Effectiveness of an early mobilization protocol in a trauma and burns intensive care unit: a retrospective cohort study. Phys Ther. 2013;93(2):186–196. doi: 10.2522/ptj.20110417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Malkoc M, Karadibak D, Yildirim Y. The effect of physiotherapy on ventilatory dependency and the length of stay in an intensive care unit. Int J Rehabil Res. 2009;32(1):85–88. doi: 10.1097/MRR.0b013e3282fc0fce. [DOI] [PubMed] [Google Scholar]
- 4.Morris PE, Goad A, Thompson C, Taylor K, Harry B, Passmore L, Ross A, Anderson L, Baker S, Sanchez M, Penley L, Howard A, Dixon L, Leach S, Small R, Hite RD, Haponik E. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med. 2008;36(8):2238–2243. doi: 10.1097/CCM.0b013e318180b90e. [DOI] [PubMed] [Google Scholar]
- 5.Ronnebaum JA, Weir JP, Hilsabeck TA. Earlier mobilization decreases the length of stay in the intensive care unit. J Acute Care Phys Ther. 2012;3(2):204–210. [Google Scholar]
- 6.Titsworth WL, Hester J, Correia T, Hester J, Correia T, Reed R, Guin P, Archibald L, Layon AJ, Mocco J. The effect of increased mobility on morbidity in the neurointensive care unit. J Neurosurg. 2012;116(6):1379–1388. doi: 10.3171/2012.2.JNS111881. [DOI] [PubMed] [Google Scholar]
- 7.Chen YH, Lin HL, Hsiao HF, Chou LT, Kao KC, Huang CC, Tsai YH. Effects of exercise training on pulmonary mechanics and functional status in patients with prolonged mechanical ventilation. Respir Care. 2012;57(5):727–734. doi: 10.4187/respcare.01341. [DOI] [PubMed] [Google Scholar]
- 8.Chiang LL, Wang LY, Wu CP, Wu HD, Wu YT. Effects of physical training on functional status in patients with prolonged mechanical ventilation. Phys Ther. 2006;86(9):1271–1281. doi: 10.2522/ptj.20050036. [DOI] [PubMed] [Google Scholar]
- 9.Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, Spears L, Miller M, Franczyk M, Deprizio D, Schmidt GA, Bowman A, Barr R, McCallister KE, Hall JB, Kress JP. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009;373(9678):1874–1882. doi: 10.1016/S0140-6736(09)60658-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Talley CL, Wonnacott RO, Schuette JK, Jamieson J, Heung M. Extending the benefits of early mobility to critically ill patients undergoing continuous renal replacement therapy: the Michigan experience. Crit Care Nurs Q. 2013;36(1):89–100. doi: 10.1097/CNQ.0b013e3182753387. [DOI] [PubMed] [Google Scholar]
- 11.Winkelman C, Higgins PA, Chen YJ. Activity in the chronically critically ill. Dimens Crit Care Nurs. 2005;24(6):281–290. doi: 10.1097/00003465-200511000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Engel HJ, Needham DM, Morris PE, Gropper MA. ICU early mobilization: from recommendation to implementation at three medical centers. Crit Care Med. 2013;41(9 Suppl 1):S69–S80. doi: 10.1097/CCM.0b013e3182a240d5. [DOI] [PubMed] [Google Scholar]
- 13.Needham DM, Korupolu R. Rehabilitation quality improvement in an intensive care unit setting: implementation of a quality improvement model. Top Stroke Rehabil. 2010;17(4):271–281. doi: 10.1310/tsr1704-271. [DOI] [PubMed] [Google Scholar]
- 14.Zanni JM, Korupolu R, Fan E, et al. Rehabilitation therapy and outcomes in acute respiratory failure: an observational pilot project. J Crit Care. 2010;25(2):254–262. doi: 10.1016/j.jcrc.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 15.Dang SL. ABDCEs of ICU. Early mobility. Crit Car Nurs. 2013;36(2):163–168. doi: 10.1097/CNQ.0b013e318283cf45. [DOI] [PubMed] [Google Scholar]
- 16.Hopkins RO, Spuhler VJ. Strategies for promoting early activity in critically ill mechanically ventilated patients. AACN Adv Crit Care. 2009;20(3):277–289. doi: 10.1097/NCI.0b013e3181acaef0. [DOI] [PubMed] [Google Scholar]