Abstract
A 61-year-old man with no significant medical history presented with fever, muscle pain, and weakness. He was found to be in multiorgan failure due to leptospirosis, a condition known as Weil's disease. A timely workup, combined with early initiation of antibiotics, led to effective treatment for this patient.
Leptospirosis is a worldwide zoonotic infection often resulting from environmental factors such as hurricanes and floods, which are prevalent in the southern USA. The diagnosis is challenging, as the incidence is relatively low in the USA and can often present with highly variable clinical symptoms. The purpose of this report is to remind practitioners of the signs and symptoms of leptospirosis infection so that prompt supportive care and treatment can be started. Mortality from Weil's disease ranges from 5% to 15%.
CASE REPORT
A 61-year-old man presented with 5 days of fever, pain, and weakness in lower extremities. His vital signs and physical exam were unremarkable. He chronically ingested dietary supplements and Chinese herbal medications. Additionally, he was restoring a house built in southern Louisiana in the late 1800s. His blood work and imaging results from day 1 and day 5 are listed in the Table.
Table 1.
Laboratory and imaging results
| Test | Day 1 | Day 5 |
|---|---|---|
| White blood cell count × 103/μL | 5.7 | 9.3 |
| Hemoglobin (g/dL) | 14.4 | 11.1 |
| Platelets (cells/mm3) | 33,000 | 31,000 |
| Blood urea nitrogen (mg/dL) | 54 | 41* |
| Creatinine (mg/dL) | 4.9 | 3.2* |
| Creatine kinase (U/L) | 8000 | 4500 |
| Total bilirubin (mg/dL) | 1.1 | 29 |
| Alkaline phosphatase (U/L) | 77 | 245 |
| Aspartate aminotransferase (U/L) | 403 | 453 |
| Alanine aminotransferase (U/L) | 216 | 355 |
| International normalized ratio | 1.2 | 1.6 |
| Abdominal ultrasound with Doppler | Gallbladder sludge. No gallstones. Normal biliary ducts. Patent vessels. Splenomegaly. |
Required temporary dialysis.
Several infectious diagnoses (bacterial, viral, parasitic) were considered, including leptospirosis. Given the environmental exposures of restoring an old home in the humid climate of New Orleans—which is prone to flooding and infestation with rodents and rodent urine—the patient was at increased risk of transmission. He was started on N-acetylcysteine for his acute liver injury and ceftriaxone for possible zoonotic infections such as leptospirosis. Transjugular liver biopsy revealed increased mitosis and regeneration (Figure 1). Initial results were also suggestive of leptospirosis and were later confirmed by the Centers for Disease Control and Prevention to be Leptospira based upon Warthin-Starry and immunohistochemistry stains (Figure 2). Ten days later, his serum was positive for leptospira antibodies, which normalized with the antibiotics. He recovered fully.
Figure 1.
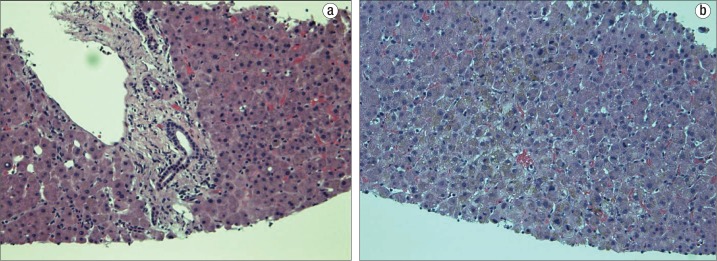
Liver biopsy results showing (a) mild periportal hepatitis with hepatocanalicular cholestasis and (b) an increase in mitotic activity, which suggests regenerative changes from an injury.
Figure 2.
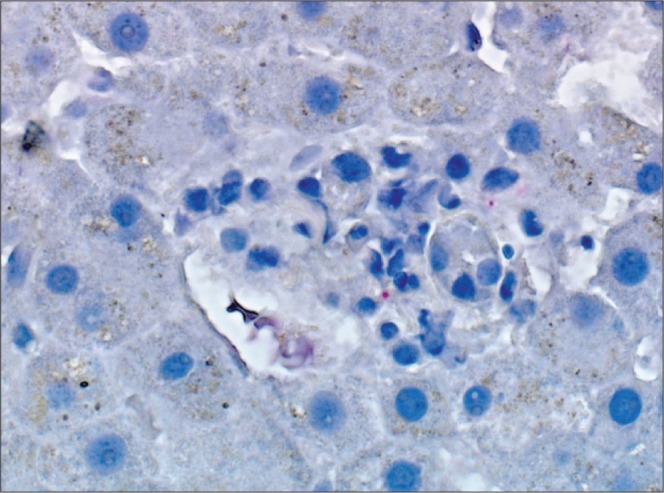
Immunohistochemical stain showing leptospirosis antigen, as demonstrated by the punctate red granules. Magnification at 400×.
DISCUSSION
Leptospirosis is a worldwide zoonotic infection due to Leptospira spp. Animals, specifically rodents, are the primary vectors of disease. Human infection results from exposure to the urine of infected animals or through contact with contaminated soil or water. Regions prone to hurricanes and floods are at higher risk of exposure (1–3). The diagnosis is challenging for several reasons: 1) its low incidence in the United States, 2) its highly variable clinical symptoms, and 3) its mimicry of common diseases such as viral hepatitis.
Typically, leptospirosis has a biphasic disease course. The first phase lasts up to 7 days and presents with unspecific symptoms such as fever, headache, and myalgia. The second phase can be categorized into anicteric and icteric forms. Most patients undergo the milder anicteric form. Rarely, leptospirosis presents with a severe icteric form with multiple organ involvement called Weil's disease. Weil's disease can lead to acute kidney failure, acute liver failure, rhabdomyolysis, and thrombocytopenia with possible hemorrhagic diathesis. Its mortality rate ranges from 5% to 15% without treatment. Transaminase levels are moderately elevated in the 100s IU/L, with a mild increase of alkaline phosphatase (1). An aspartate aminotransferase–alanine aminotransferase ratio of >3 may indicate a poorer prognosis (4). Serum bilirubin may rise as high as 30 to 40 mg/dL (1). Jaundice as a result of septic cholestasis typically appears during day 5 to 9 of the disease course. Liver function usually returns to normal without complications, as observed in this patient.
The diagnosis can be confirmed by serological tests detecting leptospiral antibodies or through polymerase chain reaction assay (1). Pathologists may also perform leptospiral immunohistochemistry staining on liver biopsies for diagnosis, but this must be specifically requested (5).
Treatment of leptospirosis with antibiotics remains controversial (6). A Cochrane review of 7 randomized clinical trials was inconclusive on the role of antibiotics (penicillin) in leptospirosis, regardless of severity (7). Nearly 90% of cases are considered mild, and oral doxycycline or amoxicillin may be used. For severe cases, parenteral high-dose penicillin G or ceftriaxone is recommended (8).
References
- 1.Bharti AR, Nally JE, Ricaldi JN, Matthias MA, Diaz MM, Lovett MA, Levett PN, Gilman RH, Willig MR, Gotuzzo E, Vinetz JM. Peru-United States Leptospirosis Consortium. Leptospirosis: a zoonotic disease of global importance. Lancet Infect Dis. 2003;3(12):757–771. doi: 10.1016/s1473-3099(03)00830-2. [DOI] [PubMed] [Google Scholar]
- 2.Vinetz JM, Glass GE, Flexner CE, Mueller P, Kaslow DC. Sporadic urban leptospirosis. Ann Intern Med. 1996;125(10):794–798. doi: 10.7326/0003-4819-125-10-199611150-00002. [DOI] [PubMed] [Google Scholar]
- 3.Wasiński B, Dutkiewicz J. Leptospirosis—current risk factors connected with human activity and the environment. Ann Agric Environ Med. 2013;20(2):239–244. [PubMed] [Google Scholar]
- 4.Chang ML, Yang CW, Chen JC, Ho YP, Pan MJ, Lin CH, Lin DY. Disproportional exaggerated aspartate transaminase is a useful prognostic parameter in late leptospirosis. World J Gastroenterol. 2005;11(35):5553–5556. doi: 10.3748/wjg.v11.i35.5553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rockey DC, Caldwell SH, Goodman ZD, Nelson RC, Smith AD. American Association for the Study of Liver Diseases. Liver biopsy. Hepatology. 2009;49(3):1017–1044. doi: 10.1002/hep.22742. [DOI] [PubMed] [Google Scholar]
- 6.Wang LS, Wang CC, Huang SH, Chao H, Lin SH, Chang JH, Ho YH. Leptospirosis with transient paraparesis and thrombocytopenia: a case report. J Microbiol Immunol Infect. 2012;45(1):75–78. doi: 10.1016/j.jmii.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 7.Brett-Major DM, Coldren R. Antibiotics for leptospirosis. Cochrane Database Syst Rev. 2012;2:CD008264. doi: 10.1002/14651858.CD008264.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maroun E, Kushawaha A, El-Charabaty E, Mobarakai N, El-Sayegh S. Fulminant leptospirosis (Weil's disease) in an urban setting as an overlooked cause of multiorgan failure: a case report. J Med Case Rep. 2011;5:7. doi: 10.1186/1752-1947-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]


