SUMMARY
Objective
Knee buckling, in which a knee gives way during weight-bearing, is common in people with knee pain and knee osteoarthritis (OA), but little is known about the prevalence of sensations of knee instability, slipping or shifting in which the knee does not actually buckle, or of the psychosocial and physical consequences of these symptoms.
Design
We asked participants in the Multicenter Osteoarthritis Study (MOST) separately about episodes of knee buckling and sensations of knee instability without buckling in the past 3 months, and assessed fear of falling, poor balance confidence (Activities-specific Balance Confidence (ABC) Scale ≤ 67/100), activity limitation due to concern about buckling, and poor physical function (Western Ontario and McMaster Universities Arthritis Index (WOMAC) physical function ≥ 28/68). We used Poisson regression to estimate prevalence ratios (PRs) for cross-sectional associations of buckling and sensations of instability without buckling with these outcomes, adjusting for confounders.
Results
Of 2120 participants (60% female, 40% ≥ 65 years, mean Body mass index (BMI): 31 kg/m258), 18% reported buckling, 27% had sensations of knee instability without buckling, and 9% reported both symptoms. Buckling and sensations of instability without buckling were each significantly associated with fear of falling, poor balance confidence, activity limitations, and poor WOMAC physical function. Subjects who reported both buckling and instability without buckling and those with at least two buckling episodes (15%) had the strongest association with poor outcomes.
Conclusions
Knee buckling and especially sensations of knee instability without buckling were common and each was significantly associated with fear of falling, poor balance confidence, activity limitations, and poor physical function.
Keywords: Osteoarthritis, Epidemiology, Outcome measures, Falls
Introduction
Knee instability is a common symptom in persons with knee OA and knee pain1,2. Knee instability frequently manifests as buckling, defined as the sudden loss of postural support from ‘giving way’ of the knee due to mechanical failure during weight bearing activities1. While knee buckling is sometimes a complication of injuries to the anterior cruciate ligament or to the menisci, it is also common in people with knee pain who have had no history of such injuries1,2. People with knee buckling and other symptoms of knee instability are also more likely to have radiographic knee osteoarthritis (OA), quadriceps weakness, and limitations in physical function compared with people without knee buckling1,3,4. In a population-based study, 10% of all adults experienced knee buckling and four of five bucklers had knee pain1,3.
Buckling has not been a major focus of OA research, although treatments may be available, including bracing, and risk factors for buckling are remediable, such as quadriceps weakness5–7. While knee buckling has been shown to adversely affect physical function2,4, its impact on psychosocial outcomes such as fear of falling, loss of balance confidence and avoidance of certain activities, has not been examined. It is possible that people whose knees buckle may avoid physical activity because of reduced balance confidence or fear of falling, which may then lead to decreased physical function and deconditioning, resulting in a further increase in the risk of knee buckling.
In addition, while many people with knee OA may not experience mechanical failure of the knee resulting in loss of postural support (knee buckling or giving way), they may experience sensations of knee instability, slipping or shifting without the knee actually giving way. Such sensations of instability without the knee buckling may have a similar association as buckling with adverse health outcomes; however, the frequency of buckling and the instability symptoms that do not involve buckling and their association with health outcomes have not been studied8,9.
The goals of this study were: 1) to examine the prevalence of knee buckling (giving way), and of sensations of knee instability, slipping or shifting without buckling, in a cohort of people with or at high risk of knee OA; 2) to examine the association of a) knee buckling and the frequency of buckling, b) sensations of knee instability, slipping or shifting without buckling, and c) the presence of either or both of these symptoms with functional health outcomes and concern about falls and poor balance.
Methods
Population
The Multicenter Osteoarthritis Study (MOST) is a longitudinal study of people either with or at high risk of knee OA. Details of MOST have been published previously10. In brief, MOST included participants between 50 and 79 years of age at baseline who were community-dwelling in Birmingham, Alabama, or Iowa City, Iowa. Definition of being at high risk for OA included older age, female sex, previous knee injury or surgery, and high body weight11. Baseline exams occurred between April 2003 and April 2005 and participants were followed at the 15, 30 and 60 months visits. We utilized cross-sectional data from the 60-month visit, since that was the examination at which subjects were first asked about knee buckling and instability. The MOST study protocol was approved by the Institutional Review Boards at the University of Alabama at Birmingham, the University of Iowa, the University of California, San Francisco, and Boston University Medical Center.
Exposures of interest
Knee buckling and sensations of knee instability, slipping or shifting without buckling
To assess episodes of knee buckling or giving way (we use these two terms interchangeably), participants were asked “In the past 3 months, has either of your knees buckled or given way at least once?” We defined knee buckling as those who answered ‘yes’ to this question on knee buckling in the past 3 months. We further classified those who buckled into people who had one buckling episode, and those who had two or more buckling episodes in the previous 3 months. The same question on buckling was also asked in terms of the past 12 months.
In order to assess whether participants experienced a sensation of knee instability, slipping or shifting that did not involve the knee actually buckling, just after the question about knee buckling, we asked all participants “In the past 3 months, has either knee felt like it was shifting, slipping, or going to give way but didn’t actually do so?” We defined sensations of knee instability without buckling as present in those who answered ‘yes’ to this question.
We also classified participants for combinations of knee buckling and sensations of knee instability without buckling in the past 3 months, as follows: Group 1) experienced no episodes of knee buckling and no episodes with sensations of knee instability without buckling; Group 2) experienced sensations of knee instability without buckling but did not experience any separate episodes of knee buckling; Group 3) experienced knee buckling but did not report any separate episodes of sensations of knee instability without buckling; and Group 4) experienced both knee buckling and sensations of knee instability without buckling.
Falls and falling during a buckling episode
We asked all participants “During the past 12 months, have you fallen and landed on the floor, ground, or stairs?” In addition, among people with knee buckling in the past 3 months, we asked “As a result of knee buckling or giving way, did you fall and land on the floor or ground?”
Outcomes of interest
Psychosocial outcomes included fear of falling, balance confidence, and limiting activities out of concerns about knee buckling or giving way. We assessed fear of falling using a single-item question directly asking “Are you ever afraid of falling?” with fear of falling coded as yes; no if otherwise12. Although assessing fear of falling can be done easily in a clinic setting, the prevalence of fear of falling is reported to range as high as 85% in especially high-risk elderly, such that fear of falling can be a non-specific psychosocial outcome measure13. Therefore, we also included a more specific measure of assessing degrees of balance confidence that was ascertained using the validated Activities-specific Balance Confidence (ABC) Scale, which assesses self-reported confidence in performing 16 daily activities without becoming unsteady or falling14–17. The summary ABC score ranges from 0 to 100 (the higher the score, the higher the confidence). Poor balance confidence18 has been defined as having an ABC score of ≤67.
We also asked all participants “Because of concern about buckling or giving way in your knees, have you changed or limited your usual activities in any way?”
We assessed physical function with the WOMAC physical function subscale. The WOMAC physical function subscale consists of a 17-item questionnaire asking participants about difficulty performing specific physical tasks. The range is from 0 to 68 (the higher the score, the worse the function). We defined poor physical functioning as scores of at least 28/68 on the WOMAC physical function scale19, consistent with a previous definition of poor functional outcome for people with knee OA20,21.
Covariates
Knee pain was measured as the mean pain in the past 30 days on a Visual Analogue Scale (VAS) ranging from 0 to 10022. Co-morbidities were assessed using the Charlson co-morbidity index23,24. Body mass index (BMI) was calculated from measures of height and weight as the ratio of measured weight (kg) divided by height (m2). Radiographic knee OA was defined as present when at least one knee showed a Kellgren and Lawrence score of two or greater, as previously described10,25. Quadriceps strength was determined from the maximum of four isokinetic knee extensor torque repetitions at 60 degrees/second, scaled by body weight, and was categorized into sex-specific deciles as previously described26,27. For about 10% of the participants, quadriceps strength data were taken from the baseline visit owing to missing data on this measure. History of any knee injury or surgery was based on self-report of a major knee injury or knee surgery up to the 60-month visit.
Data analysis
For each outcome of interest, we used Poisson regression28 with robust variance29 to estimate the prevalence ratios (PRs) and 95% confidence interval (CI) for the cross-sectional associations of buckling or instability without buckling in the past 3 months with each study outcome of interest. We carried out similar analyses, subdividing those who had a knee buckling in the past 3 months into those who had one buckling episode, and those who had two or more.
We also estimated the relative effect on the outcomes of interest of each of the groups in the classification of subjects combining buckling and sensations of instability without buckling, with the referent group consisting of people having neither buckling nor instability without buckling. While episodes of knee buckling and the sensation of knee instability without buckling are both manifestations of knee instability, subjects may not always consistently distinguish between them. Therefore, we also estimated the relative effect of having either knee buckling or sensations of instability without buckling compared with the referent group of people having neither buckling nor sensations of instability without buckling, with each outcome of interest.
For multivariable analyses, we adjusted for sex, age (years), BMI, co-morbidity index, knee pain severity, radiographic OA (ROA), deciles of quadriceps strength, and history of knee injury or surgery. We entered the variable for knee buckling or knee instability without buckling first into the model as the predictor of interest. We then subsequently added covariates into the model. If the covariates change the estimate of effect for knee buckling or knee instability without buckling by more than 10%, that covariate remains in the model. Additionally adjusting for radiographic knee OA, quadriceps strength, and history of knee injury or surgery did not change the estimates of effect. Further sensitivity analyses with and without the imputed quadriceps strength data showed almost identical results. Thus, we present the estimates of effect adjusting for only sex, age, BMI, co-morbidity, and knee pain for all analyses.
To be consistent in our assessment of the same time period for knee buckling and knee instability, we excluded those who reported buckling in the past 12 months but not in the past 3 months. However, we also performed sensitivity analyses by including 173 subjects who buckled in the past 12 but not 3 months as a separate exposure group, or included in the reference (non-exposed) group, in analyses examining buckling in the past 3 months vs non-buckling, and in the combined knee instability and buckling analyses. These analyses did not materially change the results or the inference of the study. All statistical analyses were performed using SAS V9.2 (SAS Institute, Gary, NC).
Results
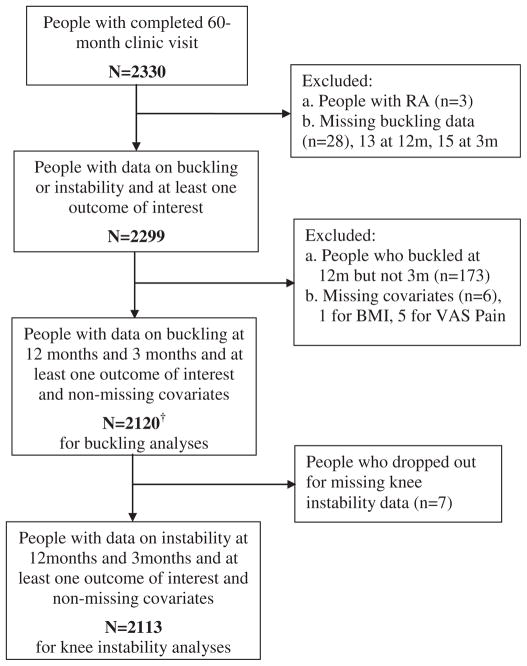
Of 2330 who attended the clinic visit at 60 months, 2299 responded to the questionnaire and had data on buckling or sensations of instability without buckling and at least one of the outcomes of interest. Of those, 173 people were excluded because they had buckling in the past 12 months but not 3 months; this exclusion was done independent of the outcomes of interest. Also, six were missing data on BMI or VAS pain, leaving 2120 and 2113 people, for the analyses of knee buckling and sensations of knee instability without buckling in the past 3 months, respectively [see Fig. 1]. Of the 2120 people, 60% were female, 40% were 65 years or older, and mean BMI was 31 kg/m2.
Fig. 1.
Flow-chart of MOST study population at 60-month in relation to consequences of knee buckling and instability. Please note that for each outcome of interest, a few people further dropped out of the analyses because they were missing that particular outcome. For example, the following people were excluded from the buckling analyses: three for fear of falls, three for balance confidence, 32 for WOMAC physical function score.
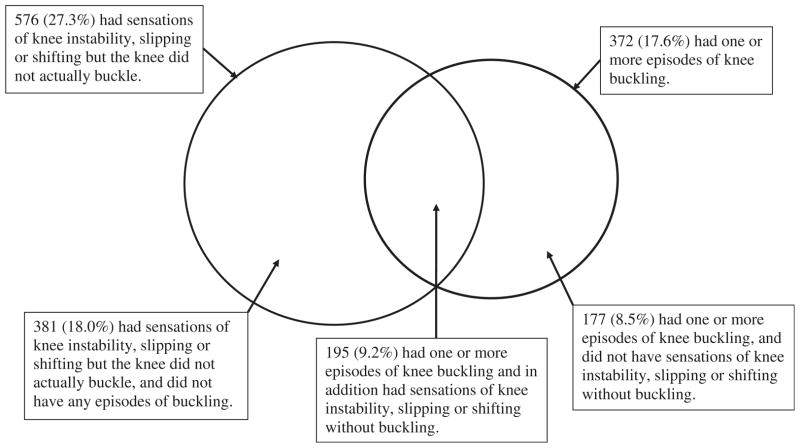
Of these subjects, 27% (576/2113) reported sensations of knee instability without buckling (they may also have had separate episodes of knee buckling), and 18% (377/2120) had knee buckling (they may also have had sensations of instability without buckling) [Fig. 2]. Both the prevalence of instability without buckling and buckling tended to increase with increasing BMI and higher levels of co-morbidity but not necessarily with age, and both were more prevalent in women (see Table I). In addition, among those whose knee buckled, the overwhelming majority (309/377) had two or more episodes of knee buckling during that time. For these people, approximately 74% reported 2–5 buckling episodes, 17% 6–10, and 9% reported 11 or more episodes. Among subjects with buckling in the past 3 months, 18% (69/377) reported that they fell as a result of knee buckling or giving way (data not shown). Among all subjects, 620 people (29%) had at least one fall in the past 12 months.
Fig. 2.
Distribution of symptoms of knee instability in the past 3 months. Among 2113 people with data on both buckling and sensations of instability without buckling, 753 (35.6%) reported either knee buckling or sensations of instability without buckling and 1360 (64.4%) had neither (not included in figure).
Table I.
Characteristics at 60-month visit—MOST study by sensations of knee instability without buckling and buckling status in past 3 months
| Characteristics, n (%) with knee condition, except where specified | Sensations of knee instability without buckling* | Knee buckling | Among people with knee buckling | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| No (n = 1537) | Yes (n = 576) | No (n = 1743) | Yes (n = 377) | 1 episode (n = 68) | 2+ episodes (n = 309) | |
| Sex | ||||||
| Female | 883 (69.9) | 381 (30.1) | 1030 (81.1) | 240 (18.9) | 51 (4.0) | 189 (14.9) |
| Male | 654 (77.0) | 195 (23.0) | 713 (83.9) | 137 (16.1) | 17 (2.0) | 120 (14.1) |
| Age (year) mean ± SD | 62.6 ± 7.9 | 61.2 ± 7.6 | 62.4 ± 7.9 | 61.5 ± 7.7 | 60.8 ± 7.3 | 61.6 ± 7.8 |
| <65 | 899 (70.4) | 377 (29.6) | 1034 (80.9) | 244 (19.1) | 48 (3.8) | 196 (15.3) |
| ≥65 | 638 (76.2) | 199 (23.8) | 709 (84.2) | 133 (15.8) | 20 (2.4) | 113 (13.4) |
| BMI mean ± SD | 30.4 ± 5.8 | 32.1 ± 7.2 | 30.6 ± 6.0 | 32.2 ± 7.1 | 32.0 ± 7.7 | 32.2 ± 6.9 |
| Normal (17.0–24.9) | 235 (74.8) | 79 (25.2) | 269 (84.9) | 48 (15.1) | 10 (3.2) | 38 (12.0) |
| Overweight (25.0–29.9) | 585 (76.5) | 180 (23.5) | 654 (85.3) | 113 (14.7) | 20 (2.6) | 93 (12.1) |
| Obese (30.0–66.0) | 717 (69.3) | 317 (30.7) | 820 (79.2) | 216 (20.8) | 38 (3.7) | 178 (17.2) |
| Charlson co-morbidity index mean ± SD | 0.8 ± 1.2 | 1.0 ± 1.4 | 0.7 ± 1.2 | 1.2 ± 1.6 | 0.9 ± 1.6 | 1.2 ± 1.5 |
| 0 | 933 (75.3) | 306 (24.7) | 1061 (85.4) | 182 (14.6) | 40 (3.2) | 142 (11.4) |
| 1 | 297 (71.7) | 117 (28.3) | 344 (82.9) | 71 (17.1) | 11 (2.6) | 60 (14.5) |
| 2–10 | 307 (66.7) | 153 (33.3) | 338 (73.2) | 124 (26.8) | 17 (3.7) | 107 (23.1) |
| VAS pain score† | ||||||
| Mean ± SD | 15.2 ± 19.4 | 32.6 ± 24.7 | 16.4 ± 19.8 | 36.7 ± 25.7 | 31.5 ± 24.5 | 37.9 ± 25.9 |
| 0–9 | 771 (88.9) | 96 (11.1) | 822 (94.7) | 46 (5.3) | 10 (1.2) | 36 (4.2) |
| 10–39 | 559 (67.3) | 272 (32.7) | 668 (80.0) | 167 (20.0) | 35 (4.2) | 132 (15.8) |
| 40+ | 207 (49.9) | 208 (50.1) | 253 (60.7) | 164 (39.3) | 23 (5.5) | 141 (33.8) |
| ROA (KL ≥ 2)‡ | ||||||
| Yes | 630 (65.5) | 332 (34.5) | 750 (77.7) | 215 (22.3) | 42 (4.4) | 173 (17.9) |
| No | 708 (80.6) | 170 (19.4) | 769 (87.3) | 112 (12.7) | 21 (2.4) | 91 (10.3) |
| History of injury/surgery | ||||||
| Yes | 859 (70.6) | 358 (29.4) | 976 (79.9) | 246 (20.1) | 40 (3.3) | 206 (16.9) |
| No | 673 (75.5) | 218 (24.5) | 762 (85.3) | 131 (14.7) | 28 (3.1) | 103 (11.5) |
| Falls past 12 months | ||||||
| Yes | 400 (65.0) | 215 (35.0) | 459 (74.0) | 161 (26.0) | 30 (4.8) | 131 (21.1) |
| No | 1136 (76.0) | 359 (24.0) | 1281 (85.6) | 216 (14.4) | 38 (2.5) | 178 (11.9) |
Missing knee instability data seven people.
Maximum VAS for pain severity.
Missing ROA data for 274 people.
Table II shows the prevalence and PR for each study outcome of interest by report of knee instability without buckling and report of buckling. Of participants with data on buckling, covariates, and outcomes, 33% ((507 + 199)/2117) reported a fear of falling, 13% (276/2117) had low confidence in their balance, 17% (357/2120) limited their usual activity owing to concerns about knee buckling or giving way, and 13% (273/2088) had poor WOMAC physical function.
Table II.
Association of sensations of knee instability without buckling, knee buckling, and frequency of buckling with outcomes of interest
| Outcome of interest | Sensations of knee instability without buckling* | Knee buckling | Among people with knee buckling† | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| No (n = 1537) | Yes (n = 576) | No (n = 1743) | Yes (n = 377) | 1 episode (n = 68) | 2+ episodes (n = 309) | |
| Fear of falling‡, n (%) | 425/1536 (27.7) | 276/574 (48.1) | 507/1740 (29.1) | 199/377 (52.8) | 27/68 (39.7) | 172/309 (55.7) |
| Adjusted PR (95% CI)|| | REF | 1.4 (1.3, 1.6) | REF | 1.4 (1.3, 1.6) | 1.1 (0.8, 1.5) | 1.5 (1.3, 1.7) |
| Poor balance confidence‡ (ABC score ≤ 67) n (%) | 138/1536 (9.0) | 135/574 (23.5) | 153/1740 (8.8) | 123/377 (32.6) | 14/68 (20.6) | 109/309 (35.3) |
| Adjusted PR (95% CI)|| | REF | 1.6 (1.3, 2.0) | REF | 2.2 (1.8, 2.8) | 1.5 (0.9, 2.4) | 2.4 (1.9, 3.0) |
| Limit activity due to concern about knee buckling, n (%) | 94/1537 (6.1) | 260/576 (45.1) | 191/1743 (11.0) | 166/377 (44.0) | 20/68 (29.4) | 146/309 (47.3) |
| Adjusted PR (95% CI)|| | REF | 5.3 (4.2, 6.8) | REF | 2.5 (2.0, 3.0) | 1.8 (1.3, 2.6) | 2.6 (2.1, 3.2) |
| WOMAC physical function score§ ≥ 28.0, n (%) | 115/1521 (7.6) | 157/561 (28.0) | 149/1726 (8.6) | 124/362 (34.3) | 14/67 (20.9) | 110/295 (37.3) |
| Adjusted PR (95% CI)|| | REF | 1.6 (1.3, 2.0) | REF | 1.5 (1.2, 1.9) | 1.1 (0.7, 1.7) | 1.6 (1.3, 2.0) |
Missing knee instability data seven people.
Reference group in analytic models is participants with no buckling in the past 3 months.
Missing data on three people for this outcome of interest.
Missing WOMAC physical function score for 32 people.
Adjusted for sex, age, BMI, co-morbidity, knee pain severity. Further adjusting for ROA, quadriceps strength, and history of knee injury or surgery materially did not change the estimates.
Participants who reported having sensations of instability without buckling, as well as those with buckling, were more likely to report fear of falling, low balance confidence, limit their usual activity due to concerns about buckling, and have poor physical function compared with their respective comparison groups. For example, 45% of those with sensations of instability without buckling reported limiting their activity because of concerns about knee buckling compared with 6% in those with no instability; 44% of persons with buckling reported limiting their activity compared with 11% of those without buckling.
Once we controlled for age, sex, BMI, co-morbidity, and knee pain severity, people reporting sensations of instability without buckling, as well as those with buckling, had a significantly increased risk of all four adverse outcomes. The association between knee buckling and each of the outcomes was generally higher for those with two or more episodes of knee buckling than those who had one buckling episode in the previous 3 months, relative to the people who did not have any knee buckling. Additional breakdown of the number of buckling episodes did not suggest a further increase in risk of adverse outcomes with more frequent buckling (data not shown).
Results of the combined instability-buckling groups compared with the referent group of people having neither buckling nor sensations of knee instability without buckling are shown in Table III. Of 2113 people, 64% (1360/2113) did not report either symptom in the past 3 months, 18% reported only sensations of knee instability without buckling (381/2113), 8% reported only buckling but no episodes of knee instability without buckling (177/2113), and 9% (195/2113) reported both symptoms [Fig. 2]. Relative to people in the reference group with neither symptom (Group 1), the group with buckling only (Group 3), and those reporting only sensations of instability without buckling and no separate episodes of buckling (Group 2) had increased risks of all adverse outcomes. People who reported both buckling and instability without buckling (Group 4) had greatest increased risk of all adverse outcomes.
Table III.
Association of symptoms of knee instability with outcomes of interest, by occurrence of buckling in past 3 months
| Outcome of interest, n (%) | No buckling episodes in past 3 months
|
One or more buckling episodes in past 3 months
|
||
|---|---|---|---|---|
| Group 1. No symptoms of knee instability (n = 1360) | Group 2. Sensations of knee instability without bucking (n = 381) | Group 3. No sensations of knee instability without buckling (n = 177) | Group 4. Sensations of knee instability without buckling (n = 195) | |
| Fear of falling*,n (%) | 349/1359 (25.7) | 157/379 (41.4) | 76/177 (42.9) | 119/195 (61.0) |
| Adjusted PR (95% CI)‡ | REF | 1.4 (1.2, 1.6) | 1.4 (1.2, 1.7) | 1.8 (1.5, 2.1) |
| Poor balance confidence (ABC score* ≤ 67), n (%) | 103/1359 (7.6) | 50/379 (13.2) | 35/177 (19.8) | 85/195 (43.6) |
| Adjusted PR (95% CI)‡ | REF | 1.3 (1.0, 1.8) | 1.8 (1.3, 2.5) | 3.0 (2.2, 4.0) |
| Limit activity due to concern about knee buckling, n (%) | 42/1360 (3.1) | 148/381 (38.9) | 52/177 (29.4) | 112/195 (57.4) |
| Adjusted PR (95% CI)‡ | REF | 10.5 (7.5, 14.7) | 7.7 (5.2, 11.3) | 12.2 (8.6, 17.5) |
| WOMAC physical score† ≥ 28.0, n (%) | 75/1348 (5.6) | 74/376 (19.7) | 40/173 (23.1) | 83/185 (44.9) |
| Adjusted PR (95% CI)‡ | REF | 1.8 (1.3, 2.4) | 1.8 (1.3, 2.4) | 2.2 (1.6, 3.0) |
Missing data on three people for this outcome of interest.
Missing WOMAC physical ability score for 31 people.
Adjusted for sex, age, BMI, co-morbidity, knee pain severity. Further adjusting for ROA, quadriceps strength, and history of knee injury or surgery materially did not change the estimates.
Over one third (36%; 758/2118) reported some symptoms of knee instability, either buckling or sensations of instability without buckling or both (Table IV). Associations between having any symptom of knee instability with adverse outcomes are shown in Table IV. For example, people reporting either type of knee instability had about a 2-fold greater risk of poor balance confidence, as well as poor physical function, compared to those who did not report any symptoms of knee instability in the past 3 months.
Table IV.
Association of any symptoms of knee instability in the past 3 months with outcomes of interest
| Outcome of interest, n (%) | No buckling and no sensations of instability without buckling (n = 1360) | Buckling or sensations of instability without buckling (n = 758) |
|---|---|---|
| Fear of falling*, n (%) | 349/1359 (25.7) | 356/756 (47.1) |
| Adjusted PR (95% CI)‡ | REF | 1.5 (1.3, 1.7) |
| Poor balance confidence (ABC score* ≤ 67), n (%) | 103/1359 (7.6) | 173/756 (22.9) |
| Adjusted PR (95% CI)‡ | REF | 1.9 (1.5, 2.4) |
| Limit activity due to concern about knee buckling, n (%) | 42/1360 (3.1) | 314/758 (41.4) |
| Adjusted PR (95% CI)‡ | REF | 10.2 (7.3, 14.1) |
| WOMAC physical score† ≥ 28.0, n (%) | 75/1348 (5.6) | 198/738 (26.8) |
| Adjusted PR (95% CI)‡ | REF | 1.9 (1.5, 2.5) |
Missing data on three people for this outcome of interest.
Missing WOMAC physical ability score for 31 people.
Adjusted for sex, age, BMI, co-morbidity, knee pain severity. Further adjusting for ROA, quadriceps strength, and history of knee injury or surgery materially did not change the estimates.
Discussion
In a population with knee OA or at risk of knee OA, we found that 27% of participants reported having sensations of knee instability, slipping or shifting that did not result in buckling, 18% reported having knee buckling, and 36% reported one or both of these symptoms in the previous 3 months. Both knee instability without buckling and buckling, especially having two or more buckling episodes, were associated with adverse psychosocial (e.g., fear of falling and poor balance confidence) and physical function (e.g., poor WOMAC function scores) outcomes. Having sensations of knee instability even in people who had no episodes of knee buckling in the past 3 months was associated with an increased risk of fear of falling, activity limitation out of concern about a knee buckling or giving way, and poor WOMAC physical function. It is noteworthy that nearly one-half of people who reported buckling also limited their activities due to concern about buckling, as did a similar proportion of those who had episodes of instability without buckling. People who reported knee buckling and who also reported having sensations of instability without buckling had the greatest risk of all adverse outcomes.
Ours is the first study to link knee buckling and sensations of instability, slipping or shifting without buckling with fear of falling, poor balance confidence and limitations of activity due to concern about knee buckling in an older population. Our results suggest that fear of falling in people with knee instability is a common consequence of knee OA and may contribute to poor functional outcomes of the disease. Poor balance and increased fear of falling is associated with decreased physical function even in people who have not had a fall30,31. Fear of falling is likely a reason that such a high proportion of those with knee instability limit their activities out of concern about buckling. Surprisingly, even among those who reported having episodes of sensations of knee instability without buckling and had no separate episodes of buckling, 40% limited their activities due to concern about buckling, perhaps in some instances resulting from buckling in years past. Whether such self-imposed limitations in activity reduce the risk of buckling and falls, or contribute to deconditioning and loss of physical function and possibly even a further increase in instability deserves further investigation.
It is possible that the sensation of knee instability, slipping or shifting without buckling and actual knee buckling are part of a continuum, with the latter representing a more severe form of instability. Hence, while instability without buckling alone is associated with adverse outcomes, experiencing both buckling and sensations of instability without buckling was associated with even greater impacts. These findings warrant better assessment in clinical settings not only of knee buckling, but also of less severe sensations of knee instability. Asking patients specifically about sensations of knee instability without buckling could identify people at risk and may help them receive interventions to prevent knee buckling and its consequences. However, self-report of these conditions asks subjects to make subtle distinctions (“buckling or giving way” vs “going to give way but didn’t”) that may not be reliable. Further investigation into methods for assessing knee instability is needed, including further research into the potential for objective measures32–34.
Ours is also the first study to analyze whether the number of buckling episodes reported is associated with the risk of adverse outcomes, and suggests that those who buckle multiple times have worse outcomes than those who buckle less frequently. While the association of buckling just once in 3 months with fear of falling and WOMAC function were close to null, a single episode of buckling was associated with a significantly increased risk of limiting activity due to concern about buckling and with a trend for reduced balance confidence (the wide CIs for the latter may reflect the small sample size in this stratum). Thus, even isolated episodes of buckling may be associated with some adverse outcomes.
Knee pain is likely to be an important factor in determining the risk of knee instability and buckling and is also known to affect knee OA outcomes like physical function. Even after adjusting for knee pain, the associations of all outcomes of interest with knee buckling and knee instability without buckling were statistically significant and clinically meaningful. Other confounders such as ROA, quadriceps strength, and history of knee injury or surgery did not materially influence the association between buckling or instability without buckling and the outcomes we studied after adjustment for knee pain and other covariates. These factors may increase the likelihood of buckling or instability by increasing knee pain. Thus, by adjusting for knee pain, we have also adjusted for the precursors of knee pain.
Our results confirm those of previous studies in persons with knee OA that have found an association between having knee instability (defined as buckling, shifting or giving way) and poor physical function outcomes2,4,35. van der Esch et al.4 analyzed WOMAC physical function on a continuous scale and found that once adjusting for knee pain and muscle strength, only unilateral knee instability was significantly associated with function but not bilateral knee instability. Small numbers in the latter group could explain the lack of statistically significant results. Fitzgerald et al.2 also found an association between knee instability and physical function after adjusting for knee pain, quadriceps strength, and other covariates. However, their outcome was a principal component score combining WOMAC pain, stiffness and function sub-scales and a physical performance measure, and the instability measure incorporated the degree of its effect on activities, making it difficult to compare their results directly with ours. Schmitt et al.35 used this same measure of knee instability and found it was associated with worse function as assessed on the WOMAC physical function scale, adjusting for quadriceps strength but not for knee pain.
Based on our findings for a broader spectrum of adverse outcomes, we speculate that the consistently strong independent association between knee instability and poor functional outcomes observed in multiple studies may be due, at least in part, to the impact of knee instability on fear of falling, poor balance confidence and restriction in activity due to concern about buckling. This hypothesis warrants further investigation.
Of note, our data are cross sectional, although instability and buckling would likely have immediate impacts on fear of falling and the functional outcomes we studied. It is possible that current fear of falling or activity limitation originated when the subject buckled or buckled and fell in the past, and this could help explain the finding that individuals who did not buckle and had only sensations of instability in the past 3 months had an increased risk of fear of falling and limiting their activity due to concern about buckling. However, only about one in five people who had knee buckling in the previous 3 months in our study said they had a fall as a result of the knee buckling. It is also possible that limiting activity due to concern about falls or buckling causes deconditioning that contributes to knee instability and buckling.
Our study has several limitations. We did not study the association of buckling and falls. This will be addressed in future analyses. Further, the prevalence of self-reported knee instability in our study was about half that in previous studies of instability and functional outcome2,4,35. However, subjects in these studies all had knee OA while those in our study was a mixture of persons with knee OA and those without knee OA but with an increased risk by virtue of having risk factors for knee OA. We defined knee buckling and the sensation of knee instability without buckling based on self-report, and buckling and instability may be poorly recalled. Given the cross-sectional nature of the study design, it is possible that there may be some recall bias with regard to buckling or instability in relation to the outcomes of interest.
Conclusion
In conclusion, sensations of knee instability, slipping or shifting without the knee actually buckling are common, even more so than knee buckling. Both of these conditions are associated with increased fear of falling, low balance confidence, activity limitation, and poor physical function. Over 40% of the substantial number of persons with buckling or instability report limiting activities because of concerns about these symptoms. Having two or more buckling episodes appears to have a greater impact on these physical and psychosocial consequences than having one episode, and people who reported both sensations of instability without buckling and buckling episodes had a high risk of poor outcomes. Our findings of adverse consequence of knee instability underscore the need to address this problem in treatment and rehabilitation for knee OA.
Acknowledgments
Role of funding source
This study was supported by the NIH and NIA under the following grant numbers: AG18820, AG18832, AG18947, and AG19069. Funding was partly provided by the American College of Rheumatology Scientist Development Award, the NIH AR47785, and AG18393. The study sponsors, however, have no involvement in this study design, data analyses or interpretation of the data; or in the writing, review, and submission of this manuscript for publication.
Footnotes
- Substantial contributions to the conception and design, or acquisition of the data, or analysis and interpretation of the data: Nguyen US, Felson DT, Niu J, White DK, Segal N, Lewis CE, Rasmussen M, Nevitt MC.
- Drafting the article or revising it for important intellectual content: Nguyen US, Felson DT, Niu J, White DK, Segal N, Lewis CE, Rasmussen M, Nevitt MC.
- Final approval of the version to be published: Nguyen US, Felson DT, Niu J, White DK, Segal N, Lewis CE, Rasmussen M, Nevitt MC.
Conflict of interest
No authors declare financial or personal relationships with other people or organizations that could potentially inappropriately in-fluence (bias) their work and conclusions.
References
- 1.Felson D, Niu J, McClennan C, Sack B, Aliabadi P, Hunter D, et al. Knee buckling: prevalence, risk factors, and associated limitations in function. Ann Intern Med. 2007;147:534–40. doi: 10.7326/0003-4819-147-8-200710160-00005. [DOI] [PubMed] [Google Scholar]
- 2.Fitzgerald GK, Piva SR, Irrgang JJ. Reports of joint instability in knee osteoarthritis: its prevalence and relationship to physical function. Arthritis Rheum. 2004;51:941–6. doi: 10.1002/art.20825. [DOI] [PubMed] [Google Scholar]
- 3.Knoop J, van der Leeden M, van der Esch M, Thorstensson CA, Gerritsen M, Voorneman RE, et al. Association of lower muscle strength with self-reported knee instability in osteoarthritis of the knee: results from the Amsterdam Osteoarthritis cohort. Arthritis Care Res (Hoboken) 2012;64:38–45. doi: 10.1002/acr.20597. [DOI] [PubMed] [Google Scholar]
- 4.van der Esch M, Knoop J, van der Leeden M, Voorneman R, Gerritsen M, Reiding D, et al. Self-reported knee instability and activity limitations in patients with knee osteoarthritis: results of the Amsterdam osteoarthritis cohort. Clin Rheumatol. 2012;31:1505–10. doi: 10.1007/s10067-012-2025-1. [DOI] [PubMed] [Google Scholar]
- 5.Sharma L, Hayes KW, Felson DT, Buchanan TS, Kirwan-Mellis G, Lou C, et al. Does laxity alter the relationship between strength and physical function in knee osteoarthritis? Arthritis Rheum. 1999;42:25–32. doi: 10.1002/1529-0131(199901)42:1<25::AID-ANR3>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 6.Sharma L, Lou C, Felson DT, Dunlop DD, Kirwan-Mellis G, Hayes KW, et al. Laxity in healthy and osteoarthritic knees. Arthritis Rheum. 1999;42:861–70. doi: 10.1002/1529-0131(199905)42:5<861::AID-ANR4>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 7.Fitzgerald GK, Childs JD, Ridge TM, Irrgang JJ. Agility and perturbation training for a physically active individual with knee osteoarthritis. Phys Ther. 2002;82:372–82. [PubMed] [Google Scholar]
- 8.Hand CJ, Spalding TJ. Association between anatomical features and anterior knee pain in a “fit” service population. J R Nav Med Serv. 2004;90:125–34. [PubMed] [Google Scholar]
- 9.Steinitz DK, Harvey EJ, Berry GK, Reindl R, Correa JA. Knee joint laxity in a native Canadian Indian population. Can J Public Health. 2005;96:226–9. doi: 10.1007/BF03403696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Felson DT, Niu J, Guermazi A, Roemer F, Aliabadi P, Clancy M, et al. Correlation of the development of knee pain with enlarging bone marrow lesions on magnetic resonance imaging. Arthritis Rheum. 2007;56:2986–92. doi: 10.1002/art.22851. [DOI] [PubMed] [Google Scholar]
- 11.Segal NA, Torner JC, Felson D, Niu J, Sharma L, Lewis CE, et al. Effect of thigh strength on incident radiographic and symptomatic knee osteoarthritis in a longitudinal cohort. Arthritis Rheum. 2009;61:1210–7. doi: 10.1002/art.24541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Howland J, Peterson EW, Levin WC, Fried L, Pordon D, Bak S. Fear of falling among the community-dwelling elderly. J Aging Health. 1993;5:229–43. doi: 10.1177/089826439300500205. [DOI] [PubMed] [Google Scholar]
- 13.Scheffer AC, Schuurmans MJ, van Dijk N, van der Hooft T, de Rooij SE. Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing. 2008;37:19–24. doi: 10.1093/ageing/afm169. [DOI] [PubMed] [Google Scholar]
- 14.Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci. 1995;50A:M28–34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- 15.Myers AM, Fletcher PC, Myers AH, Sherk W. Discriminative and evaluative properties of the Activities-specific Balance Confidence (ABC) scale. J Gerontol Med Sci. 1998;53:M287–94. doi: 10.1093/gerona/53a.4.m287. [DOI] [PubMed] [Google Scholar]
- 16.Jorstad EC, Hauer K, Becker C, Lamb SE. Measuring the psychological outcomes of falling: a systematic review. J Am Geriatr Soc. 2005;53:501–10. doi: 10.1111/j.1532-5415.2005.53172.x. [DOI] [PubMed] [Google Scholar]
- 17.Filiatrault J, Gauvin L, Fournier M, Parisien M, Robitaille Y, Laforest S, et al. Evidence of the psychometric qualities of a simplified version of the Activities-specific Balance Confidence scale for community-dwelling seniors. Arch Phys Med Rehabil. 2007;88:664–72. doi: 10.1016/j.apmr.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 18.Hill K. Activities-specific and Balance Confidence (ABC) Scale. Aust J Physiother. 2005;51:197. doi: 10.1016/s0004-9514(05)70033-7. [DOI] [PubMed] [Google Scholar]
- 19.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–40. [PubMed] [Google Scholar]
- 20.Sharma L, Cahue S, Song J, Hayes K, Pai YC, Dunlop D. Physical functioning over three years in knee osteoarthritis: role of psychosocial, local mechanical, and neuromuscular factors. Arthritis Rheum. 2003;48:3359–70. doi: 10.1002/art.11420. [DOI] [PubMed] [Google Scholar]
- 21.McHugh GA, Luker KA, Campbell M, Kay PR, Silman AJ. Pain, physical functioning and quality of life of individuals awaiting total joint replacement: a longitudinal study. J Eval Clin Pract. 2008;14:19–26. doi: 10.1111/j.1365-2753.2007.00777.x. [DOI] [PubMed] [Google Scholar]
- 22.Terwee CB, van der Slikke RM, van Lummel RC, Benink RJ, Meijers WG, de Vet HC. Self-reported physical functioning was more influenced by pain than performance-based physical functioning in knee-osteoarthritis patients. J Clin Epidemiol. 2006;59:724–31. doi: 10.1016/j.jclinepi.2005.11.019. [DOI] [PubMed] [Google Scholar]
- 23.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can co-morbidity be measured by questionnaire rather than medical record review? Med Care. 1996;34:73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Sangha O, Stucki G, Liang MH, Fossel AH, Katz JN. The Self-Administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 2003;49:156–63. doi: 10.1002/art.10993. [DOI] [PubMed] [Google Scholar]
- 25.Felson D, Naimark A, Anderson J, Kazis L, Castelli W, Meenan R. The prevalence of knee osteoarthritis in the elderly: the Framingham Osteoarthritis Study. Arthritis Rheum. 1987;30:914–8. doi: 10.1002/art.1780300811. [DOI] [PubMed] [Google Scholar]
- 26.Segal NA, Glass NA, Torner J, Yang M, Felson DT, Sharma L, et al. Quadriceps weakness predicts risk for knee joint space narrowing in women in the MOST cohort. Osteoarthr Cartil. 2010;18:769–75. doi: 10.1016/j.joca.2010.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.White DK, Felson DT, Niu J, Nevitt MC, Lewis CE, Torner JC, et al. Reasons for functional decline despite reductions in knee pain: the Multicenter Osteoarthritis Study. Phys Ther. 2011;91:1849–56. doi: 10.2522/ptj.20100385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162:199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- 29.Zou GA. Modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 30.Friedman SM, Munoz B, West SK, Rubin GS, Fried LP. Falls and fear of falling: which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. J Am Geriatr Soc. 2002;50:1329–35. doi: 10.1046/j.1532-5415.2002.50352.x. [DOI] [PubMed] [Google Scholar]
- 31.Cumming RG, Salkeld G, Thomas M, Szonyi G. Prospective study of the impact of fear of falling on activities of daily living, SF-36 scores, and nursing home admission. J Gerontol A Biol Sci Med Sci. 2000;55:M299–305. doi: 10.1093/gerona/55.5.m299. [DOI] [PubMed] [Google Scholar]
- 32.Irrgang JJ, Snyder-Mackler L, Wainner RS, Fu FH, Harner CD. Development of a patient-reported measure of function of the knee. J Bone Jt Surg Am. 1998;80:1132–45. doi: 10.2106/00004623-199808000-00006. [DOI] [PubMed] [Google Scholar]
- 33.Steiner ME, Brown C, Zarins B, Brownstein B, Koval PS, Stone P. Measurement of anterior-posterior displacement of the knee. A comparison of the results with instrumented devices and with clinical examination. J Bone Jt Surg Am. 1990;72:1307–15. [PubMed] [Google Scholar]
- 34.Kupper JC, Loitz-Ramage B, Corr DT, Hart DA, Ronsky JL. Measuring knee joint laxity: a review of applicable models and the need for new approaches to minimize variability. Clin Biomech (Bristol, Avon) 2007;22:1–13. doi: 10.1016/j.clinbiomech.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 35.Schmitt LC, Fitzgerald GK, Reisman AS, Rudolph KS. Instability, laxity, and physical function in patients with medial knee osteoarthritis. Phys Ther. 2008;88:1506–16. doi: 10.2522/ptj.20060223. [DOI] [PMC free article] [PubMed] [Google Scholar]