Abstract
Among adolescents there is evidence that cognitive change partially mediates the effect of cognitive behavioral therapy (CBT) on depression outcome. However, prior studies have been limited by small samples, narrow measures of cognition, and failure to compare cognitive change following CBT to cognitive change following antidepressant medication. This study examined whether change in four cognitive constructs (cognitive distortions, cognitive avoidance, positive outlook, and solution-focused thinking) mediated change in depression severity in a sample of 291 adolescents who participated in the Treatment for Adolescents with Depression Study (TADS). TADS assessed the effects of CBT, fluoxetine, and their combination on depression severity. All three treatments were associated with change in the cognitive constructs and combination treatment produced the greatest change. Furthermore, change in the cognitive constructs partially mediated change in depression severity within all three treatments. Results implicated positive outlook as the construct most associated with change in depression severity over 36 weeks.
Keywords: depression, adolescence, cognitive behavioral therapy, cognition, mediation
Cognitive behavioral therapy (CBT) is the most extensively studied psychosocial treatment for depressed adolescents, with evidence from reviews and meta-analyses supporting its effectiveness (Compton et al., 2004; Curry & Becker, 2008; Klein, Jacobs, & Reinecke, 2007; Weisz, McCarty, & Valeri, 2006). CBT is based on the cognitive model of depression, which argues that inaccurate beliefs and maladaptive information processing have a causal role in the etiology and maintenance of depression (Beck, Rush, Shaw, & Emery, 1979). In line with this model, CBT is focused on alleviating symptoms of depression by targeting cognitive processes such as cognitive distortions, negative automatic thoughts, hopelessness, dysfunctional attitudes, and a negative attributional style. A basic question that has yet to be answered is whether CBT exerts its influence through change in these cognitive constructs, as theorized. Understanding therapeutic mechanisms of change is of critical importance to identify effective and essential elements of treatment packages for the purposes of disseminating these skills to clinicians in the community (Kazdin & Nock, 2003; Kraemer, Kiernan, Essex, & Kupfer, 2008; Kraemer, Wilson, Fairburn, & Agras, 2002).
Studies of treatment mechanisms among adult clinical samples have provided consistent evidence that CBT is associated with changes in cognition, although the evidence is mixed as to whether these changes are unique to CBT (as reviewed by Driessen and Hollon [2010]). For instance, several early studies found that antidepressant medication produced levels of cognitive change comparable to CBT (Imber et al., 1990; Simons, Garfield, & Murphy, 1984), causing some investigators to conclude that cognitive change is a nonspecific result of change in depression rather than a contributing factor. However, one early study by DeRubeis and colleagues (1990) found that CBT and antidepressant medication were associated with equivalent change in cognition but that the change in cognition was only predictive of symptom improvement in the CBT condition; thus, results from this study suggested that cognitive change mediated outcome for CBT but not for antidepressant medication.
Recent adult studies testing the relationship between cognitive change and relapse have provided further evidence of the causal role of cognition by demonstrating that cognitive change precedes rather than follows symptom change. Teasdale and colleagues (2001) found that CBT reduced negative thinking patterns and that this reduction was associated with reduced risk of relapse. Similarly, Strunk, DeRubeis, Chiu, and Alvarez (2007) found that patient competence in CBT coping skills predicted risk of relapse in the year following CBT termination. Finally, two studies of adults “at risk” for depression (who did not meet full diagnostic criteria) demonstrated that reductions in negative thinking significantly mediated CBT treatment outcome relative to alternate therapy conditions. Both of these studies found that reductions in negative thinking were stronger mediators of depression symptoms than measures of interpersonal functioning or behavioral activation (Allart-van Dam, Hosman, Hoogduin, & Schaap, 2003; Muñoz et al., 1995). In summary, the adult literature provides evidence that CBT has specific effects on cognition relative to alternative therapy models or antidepressant medication and that these specific effects of CBT partially account for change in depression symptoms.
Relative to the adult literature, the adolescent literature on CBT treatment mediators is more preliminary. To date, only two studies of clinically depressed adolescents and one study of adolescents “at risk” for depression have examined mediators of improvement in depressive symptoms. The first study by Kolko and colleagues (2000) evaluated whether cognitive distortions mediated the effects of CBT in a randomized trial comparing three psychotherapies for adolescent depression: CBT, systematic behavioral family therapy, and nondirective supportive therapy. Full mediation criteria were not met, but some evidence of treatment specificity was found such that adolescents who received CBT experienced greater reductions in cognitive distortions than did adolescents who received one of the other two psychotherapies.
The second investigation by Kaufman and colleagues (2005) evaluated several potential mediators of CBT outcome among depressed adolescents with comorbid conduct disorder. Variables tested as mediators included automatic negative cognitions, dysfunctional thoughts, social skills, pleasant activities, and problem solving. Results indicated that automatic negative cognitions mediated CBT treatment outcome, whereas none of the other variables fulfilled the criteria for mediation of treatment effects.
Finally, Stice and colleagues (2010) recently evaluated mediators of CBT outcome among adolescents at risk for depression. This longitudinal study found that reduced negative cognitions predicted change in adolescent depression following CBT and that the effects of CBT on adolescent depression were partially accounted for by change in negative cognitions.
Taken together, there is evidence from a small number of adolescent studies suggesting that cognitive change partially mediates the effects of CBT treatment outcome as well as some evidence that cognitive change is greater following CBT than following other active psychotherapy models. However, prior adolescent studies have been limited by small sample sizes and narrow measures of cognitive change.
Another critical limitation of prior adolescent literature has been that tests of CBT mediators have occurred independent of recent advances in antidepressant medication. To date, no prior studies have compared mediators of CBT outcome relative to antidepressant medication, despite a growing body of literature supporting the efficacy of antidepressant medication in treating depressed adolescents (Cheung, Emslie, & Mayes, 2005). Addressing this question is of significant importance to determine whether cognitive change is a unique mechanism underlying the effects of CBT among adolescents or whether cognitive change is a nonspecific result of effective depression treatment in this age group. This question also has theoretical and empirical value from a developmental perspective. Cognitive development and brain maturation continues throughout adolescence (Steinberg, 2004), suggesting that the cognitive processes that mediate CBT treatment among adults may not necessarily be the same among adolescents.
The Treatment for Adolescents with Depression Study (TADS) provides a valuable opportunity to compare the mechanisms of change for CBT and antidepressant medication among depressed teens (Treatment for Adolescents with Depression Study Team [TADS Team], 2003). Before TADS, a major limitation of CBT research was its isolation from developments in pharma-cotherapy research. The TADS study was therefore designed to evaluate the acute and long-term effectiveness of CBT, fluoxetine (FLX), and their combination (COMB) in treating moderate to severe depression. During the first 12 weeks of acute treatment, there was also a placebo control (PBO), and after 12 weeks, this group could elect one of the three active treatments. Results of TADS indicated that COMB was the most effective treatment for adolescent depression within the first 12 weeks in terms of the percentage of teens with clinical improvement (TADS Team, 2004). By week 36, COMB still had the highest response rate (86%), but all three active treatments had essentially converged (CBT and FLX response rates of 81% each; TADS Team, 2007).
Relative to prior studies that have tested CBT mediators, strengths of the TADS study include the large sample size and the administration of multiple measures of depression symptoms and depression-relevant cognition. Building on these strengths, our research group recently sought to identify higher order cognitive constructs from several self-report measures of cognition among youth who received one of the three active TADS treatments (n = 390; Ginsburg et al., 2009). Using factor analysis, we identified four cognitive constructs: cognitive distortions, cognitive avoidance, positive outlook, and solution-focused thinking. Cognitive distortions represented a perfectionistic and unrealistic need for social approval as well as specific cognitive distortions such as over-generalization. Cognitive avoidance reflected a tendency to avoid problems and use an impulsive approach when problem solving. By contrast, positive outlook reflected positive views of the self, world, and future, whereas solution-focused thinking reflected a positive approach to problem solving. Although these constructs were correlated with clinician-rated depression scores, the pattern of loadings did not change when depression scores were included in the factor analysis, indicating that the constructs were associated with depression symptoms but distinguishable from them. Baseline scores on three of the four constructs (cognitive distortions, cognitive avoidance, and positive outlook) were associated with depression symptom severity and predicted acute treatment response, such that higher levels of maladaptive cognitions and lower levels of adaptive cognitions were associated with less symptom reduction after 12 weeks of treatment.
In the current study, we build on our prior work to examine whether change in these cognitive constructs mediates improvement in the level of depression severity following CBT and whether this change occurs only in CBT or across treatment conditions. We had three specific hypotheses. First, based on cognitive theory, we hypothesized that CBT, alone or in combination with fluoxetine (COMB), would be associated with reductions in maladaptive cognition (cognitive distortions and cognitive avoidance) and increases in adaptive cognition (positive outlook and solution-focused thinking). Second, we expected that change in the cognitive constructs would be greater in the CBT and COMB conditions than in the FLX condition. Finally, we hypothesized that change in cognition would mediate decreases in depression severity within the CBT and COMB arms but not within the FLX arm. TADS was not originally designed with adequate statistical power to examine mediators of treatment response; hence, this study was designed to be exploratory in nature with the goal of informing future examinations of mediation among adolescent populations.
Methods
Study Participants
Original Treatment for Adolescents with Depression Study Sample
Four hundred and thirty-nine clinically depressed adolescents were originally enrolled in TADS. Details of TADS’s participant characteristics have been described in previous reports (TADS Team, 2004, 2005). Adolescents in TADS were all age 12–17 years at the time of the initial screening and met full criteria for current Major Depressive Disorder (MDD) in accordance with the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (American Psychiatric Association, 2000). As noted previously, participants in TADS were randomized to one of four interventions: CBT, FLX, COMB, or PBO.
Current Study
We examined only those 291 youth who had complete data on cognitive measures at baseline and who had been randomized to one of the three active treatment arms. Within this sample (n = 291), 56% of adolescents were females. The average age at the beginning of the trial was 14.57 years (SD = 1.53). Seventy-three percent of participants classified their race/ethnicity status as White; 11% as African American; 8% as Hispanic White; 3% as Hispanic Black; 1% as Asian; and 4% as other. The modal family income was $50,000 to $74,000, with a range of less than $5,000 to more than $200,000. Importantly, the current sample of 291 did not differ significantly from the sample of 390 youth reported by Ginsburg and colleagues (2009) on age, gender, depression severity, or baseline values on any of the four cognitive constructs (all p > .05).
Measures
Children’s Depression Rating Scale–Revised (CDRS-R; Poznanski & Mokros, 1996)
The CDRS-R is a well-validated 17-item clinician-rated depression severity measure. The CDRS-R total score served as the primary outcome measure for the study. Scores on the CDRS-R were based on interviews with the adolescent and parent and could range from 17 to 113, with higher scores representing more severe depression. The reliability, validity, and sensitivity to change of the CDRS-R are well documented (Brooks & Kutcher, 2001). Interrater reliability (intraclass correlations [ICCs]) on the CDRS-R was excellent (TADS Team, 2005).
Cognitive Measures
Depression-relevant cognition was measured using the four cognitive constructs identified by Ginsburg and colleagues (2009): cognitive distortions, cognitive avoidance, positive outlook, and solution-focused thinking. These constructs were derived from a principal axis factor analysis with oblique rotation on scores from five self-report cognitive questionnaires administered during the baseline assessment. Parallel analysis was used to determine the number of factors to extract and rotate. This approach was used (as opposed to confirmatory factor analysis) because of the lack of firm expectations regarding the number of factors or the pattern of factor loadings. The loadings of individual scales on each of the four cognitive constructs, as reported in the initial analysis, are presented in Table 1. The specific scales that comprised each of these constructs are briefly described in the following text.
TABLE 1.
Rotated Factor Pattern From Principal Axes Factoring and Oblique Rotation
| Instrument | Scale | Factor 1 | Factor 2 | Factor 3 | Factor 4 |
|---|---|---|---|---|---|
| DAS | Perfectionism | .83 | −.01 | .02 | −.01 |
| DAS | Need for Social Approval | .76 | .00 | −.01 | .01 |
| CNCEQ | Total Score | .63 | .08 | −.10 | .02 |
| SPSI-R | Impulsivity/Carelessness | −.01 | .82 | .11 | −.06 |
| SPSI-R | Avoidance Style | .01 | .78 | −.06 | −.02 |
| SPSI-R | Negative Problem Orientation | .10 | .67 | −.20 | .08 |
| CTI-C | View of the World | .08 | −.01 | .84 | −.05 |
| CTI-C | View of the Self | −.16 | −.04 | .73 | .04 |
| BHS | Total Score | .14 | −.01 | −.61 | −.06 |
| SPSI-R | Rational Problem Solving | .04 | −.06 | −.13 | .85 |
| SPSI-R | Positive Problem Orientation | −.04 | .04 | .22 | .75 |
Notes. Bolded text denotes factor loadings. DAS = Dysfunctional Attitudes Scale; CNCEQ = Children’s Negative Cognitive Errors Questionnaire; SPSI-R = Social Problem-Solving Inventory–Revised; CTI-C = Cognitive Triad Inventory for Children; BHS = Beck Hopelessness Scale. Copied with permission from Ginsburg, G. S., Silva, S. G., Jacobs, R. H., Tonev, S., Hoyle, R. H., Kingery, J. N., … March, J. S. (2009). Cognitive measures of adolescent depression: Unique or unitary constructs? Journal of Clinical Child and Adolescent Psychology, 38(6), 790–802. http://dx.doi.org/10.1080/15374410903259015.
The cognitive distortions and maladaptive beliefs construct was composed of the Dysfunctional Attitudes Scale (DAS; Weissman & Beck, 1978) and the Children’s Negative Cognitive Error Questionnaire (CNCEQ; Leitenberg, Yost, & Carroll-Wilson, 1986). The cognitive avoidance construct was composed of three subscales of the Social Problem-Solving Inventory–Revised (SPSI-R; D’Zurilla, Nezu, & Maydeu-Olivares, 2002): impulsivity/carelessness, avoidant style, and negative problem orientation. The positive outlook construct consisted of the Cognitive Triad Inventory for Children (CTI-C; Kaslow, Stark, Printz, Livingston, & Tsai, 2002) and the Beck Hopelessness Scale (BHS; Beck & Steer, 1988). The solution-focused thinking construct was composed of the rational problem solving and positive problem orientation subscales of the SPSI-R. For further detail on the component measures, please refer to Ginsburg et al. (2009).
Procedure
All of the aforementioned measures were administered during a baseline assessment that was conducted after informed consent and assent were obtained and immediately prior to randomization. The measure of depression severity (CDRS-R) was administered by trained independent evaluators (IEs) who were blind to treatment condition at baseline and again at 6-, 12-, 18-, 24-, 30-, and 36-week assessments. Adolescents completed the self-report cognitive measures at baseline, 12, 24, and 36 weeks. We use data from baseline, 12, 24, and 36 weeks to allow us to test for mediation across the entire treatment period (both acute and maintenance).
Statistical Analyses
Random regression models (RRMs) were used to test change in the cognitive constructs and change in depression severity over time. Models included both fixed (treatment, time, treatment-by-time interactions, and site) and random (patient and patient-by-time interactions) effects. Analyses assessed both linear and quadratic effects of time. Trajectories of self-reported cognitions were estimated across the full 36-week treatment period.
We tested for mediation using the criteria of Kraemer and colleagues (2002). Specifically, Criterion 1 evaluates the effect of treatment and requires that treatment leads to a significant reduction in depression severity over time. Within an RRM, satisfaction of this criterion would be indicated by a significant effect of time (e.g., indication of depression severity changing over time) and/or a significant treatment-by-time interaction (e.g., indication of treatment effects on depression over time). This criterion has previously been tested within the full TADS sample (TADS Team, 2007) and replicated this primary finding among the 291 adolescents included in the current sample. Replication of the TADS primary finding was necessary to allow us to move forward with the following mediation criteria.
Criterion 2 assesses the effect of treatment on the four cognitive constructs and requires that treatment lead to change in these cognitive constructs. This criterion allowed us to test our hypotheses regarding how different treatments change cognition over 36 weeks. Within an RRM, we would expect there to be either a significant treatment effect or a significant treatment-by-time interaction predicting each of the cognitive constructs. Evidence of a significant effect would then allow us to conduct a posteriori pairwise comparisons to test our hypotheses and determine which treatment condition was associated with the greatest level of cognitive change.
Criterion 3 evaluates the effect of treatment on depression severity when accounting for change in the cognitive constructs. This criterion allowed us to test whether changes in cognition led to differential depression outcomes across conditions. According to Kraemer et al. (2002), a mediator can demonstrate an effect on treatment outcome through either a main effect (e.g., cognitive construct predicts depression severity) or an interaction of the proposed mediator with treatment (e.g., cognitive construct by treatment interaction predicts depression severity). In the current longitudinal analysis, these terms include both linear and quadratic interactions with time. For this criterion to be satisfied, we would therefore expect one of the following four terms to significantly predict depression severity: (a) cognitive construct, (b) cognitive construct by treatment interaction (two-way interaction), (c) cognitive construct by treatment-by-time interaction (linear effect of time, three-way interaction), or (d) cognitive construct by treatment-by-time interaction (quadratic effect of time, four-way interaction). In the case of mediation, we would expect the inclusion of these terms to significantly reduce the influence of treatment on depression severity. This would be indicated by a reduction in the strength of the treatment-by-time linear or quadratic interaction.
To calculate the proportion of outcome variation accounted for by change in the cognitive constructs, we used the pseudo-R2 recommended by Singer and Willett (2003).
All analyses were conducted using the MIXED procedure in SAS 9.3. The level of significance was set at p < .05 for each statistical test. Because these analyses were considered exploratory, no adjustments were made for the number of statistical tests.
Results
Criterion 1
To test Criterion 1, we examined the effect of treatment on depression. As illustrated in Figure 1, we replicated the TADS Week 36 analysis using an RRM for the 291 adolescents randomized to active treatment. Results confirmed that significant treatment differences were present at Week 12 (acute treatment outcome; TADS Team, 2004) and that all active treatments converged at Week 36 (continuation phase outcome; TADS Team, 2007). There was a significant effect for time (F = 45.91, p < .01), a treatment-by-time effect (F = 11.31, p < .01), and a site effect (F = 2.02, p < .04). In addition, there were significant quadratic terms for the time main effect (quadratic time term; F = 8.36, p < .01) and for the time by treatment interaction (quadratic time by treatment term: F = 8.60, p < .01). The effects of time (including the quadratic term) indicated that depression symptoms changed over time. The treatment-by-time interaction (including the quadratic term) indicated that change in depression symptoms over time varied by the type of treatment. These results indicated that Criterion 1 for mediation was satisfied within our subsample, allowing us to proceed with mediation Criterion 2.
Figure 1.
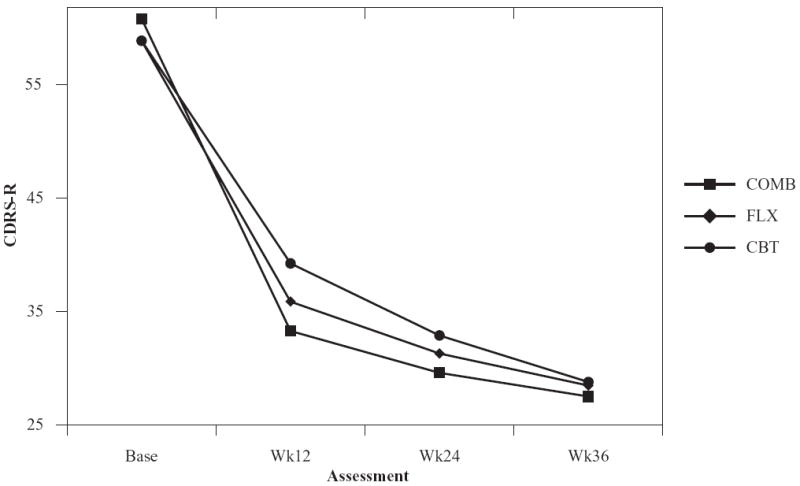
Mean Children’s Depression Rating Scale–Revised (CDRS-R) predicted scores over 36 weeks of treatment. COMB = combination of FLX and CBT; FLX = fluoxetine; CBT = cognitive behavioral therapy.
Criterion 2
To test Criterion 2 and examine whether treatments changed cognition, we analyzed the effect of treatment on the four cognitive constructs. Quadratic terms were not significant and were removed from the models for parsimony. As demonstrated in Table 2, the treatment-by-time interaction significantly predicted each of the four cognitive variables, indicating that this criterion was satisfied.
TABLE 2.
Fixed Effects in Predicting Cognitive Constructs
| F | p | |
|---|---|---|
| Cognitive distortions | ||
| Treatment | 1.42 | .24 |
| Time | 166.82 | <.01 |
| Treatment × Time | 5.11 | .01 |
| Site | 3.11 | <.01 |
| Cognitive avoidance | ||
| Treatment | 1.28 | .28 |
| Time | 84.33 | <.01 |
| Treatment × Time | 3.89 | .02 |
| Site | 1.83 | .06 |
| Positive outlook | ||
| Treatment | 2.59 | .08 |
| Time | 258.43 | <.01 |
| Treatment × Time | 8.15 | <.01 |
| Site | 3.58 | <.01 |
| Solution-focused thinking | ||
| Treatment | 2.15 | .12 |
| Time | 8.24 | <.01 |
| Treatment × Time | 5.39 | .01 |
| Site | 2.93 | <.01 |
We then compared the level of cognitive change by treatment condition. As illustrated in Figures 2 to 4, the rate of change in cognitive distortions, positive outlook, and solution-focused thinking was greater in COMB than in FLX and CBT, which did not differ from one another. As illustrated in Figure 5, the rate of change in cognitive avoidance was greater in COMB than in FLX. COMB did not outperform CBT on this construct.
Figure 2.
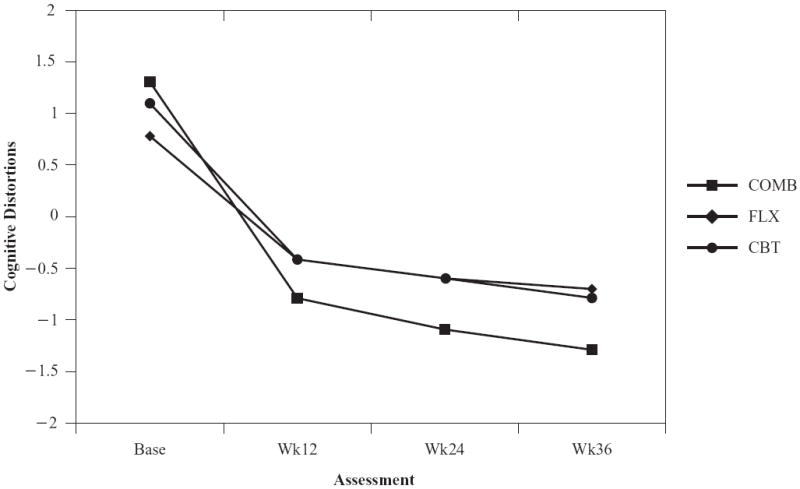
Mean cognitive distortions over 36 weeks of treatment. COMB = combination of FLX and CBT; FLX = fluoxetine; CBT = cognitive behavioral therapy.
Figure 4.
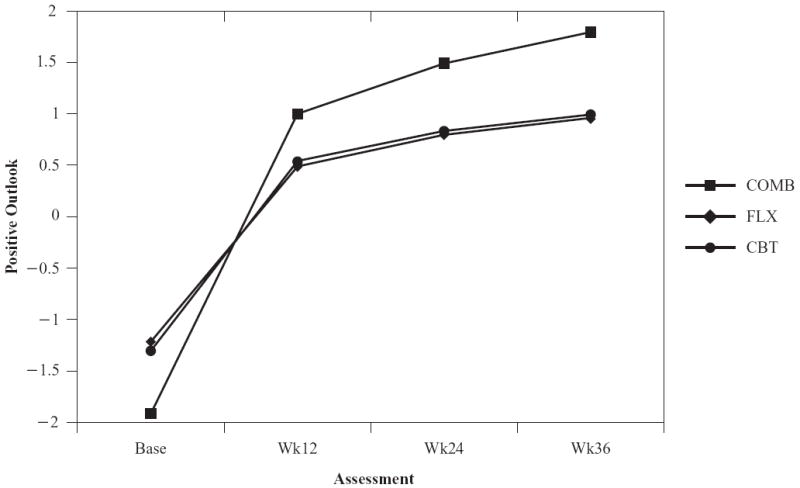
Mean positive outlook over 36 weeks of treatment. COMB = combination of FLX and CBT; FLX = fluoxetine; CBT = cognitive behavioral therapy.
Figure 5.
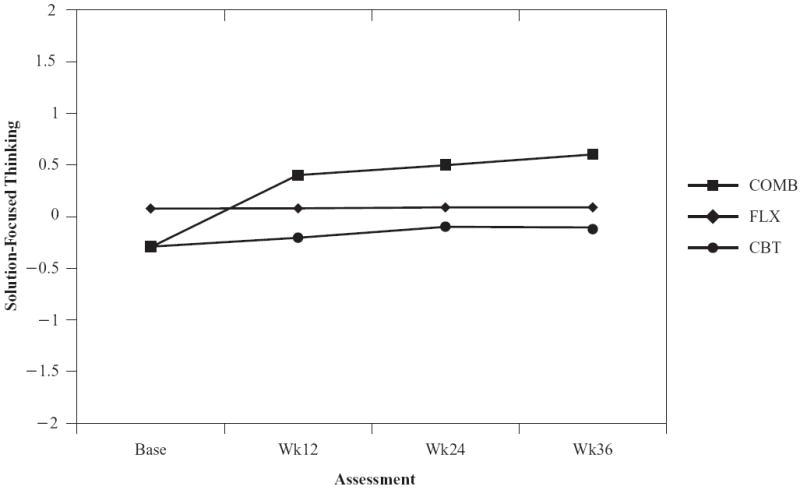
Solution-focused thinking over 36 weeks of treatment. COMB = combination of FLX and CBT; FLX = fluoxetine; CBT = cognitive behavioral therapy.
Note. N = 291. All figures represent predicted scores generated from random regression models.
Post hoc comparisons for the cognitive distortions construct indicated that there were no specific differences between COMB and the other treatment groups at any of the time points. For the positive outlook construct, those in the COMB group had significantly higher scores than those in the FLX and CBT groups at Week 24 (FLX vs. COMB, F = 4.39, p = .04; CBT vs. COMB, F = 4.09, p = .04) and Week 36 (FLX vs. COMB, F = 5.47, p =.02; CBT vs. COMB, F = 4.97, p = .03). Similarly, for solution-focused thinking, those in the COMB group had higher scores than those in the CBT group at Weeks 12 (F = 5.44, p = .02), 24 (F = 6.27, p = .01), and 36 (F = 6.64, p = .01). Finally, for cognitive avoidance, there was a trend for those in the COMB group to have lower scores than those in FLX (F = 3.20, p = .08) at Week 36. These results demonstrate that all three active treatments changed cognition and that COMB outperformed other treatments.
Criterion 3
To test the third criterion, we examined the effect of treatment on depression when accounting for each of the cognitive constructs. In this analysis, both linear and quadratic effects of time were significant and needed to be included in the model. Results of these analyses are presented in Table 3.
TABLE 3.
F Statistics for Fixed Effects in Predicting Depression: Assessing Mediation
| Cognitive Factor
| ||||
|---|---|---|---|---|
| Model Term | Cognitive Distortions | Cognitive Avoidance | Positive Outlook | Solution-Focused Thinking |
| Time effect | ||||
| Linear | 11.92** | 13.67** | 12.1** | 13.45** |
| Quadratic | 8.37** | 6.44* | 6.90* | 8.45** |
| Treatment effect | ||||
| Treatment × Time Interaction | ||||
| Linear | 5.13* | 6.31** | 5.88** | 5.83** |
| Quadratic | 4.03* | 4.93* | 5.23* | 4.96* |
| Cognitive construct effect | 11.48* | 6.89* | 26.95** | 3.38 |
| Cognitive Construct × Time Interaction | ||||
| Linear | 9.61** | 4.46* | 27.07** | 2.04 |
| Quadratic | 8.6** | 4.77* | 20.97** | 1.62 |
| Cognitive Construct × Treatment Interaction | 1.05 | 0.15 | 0.17 | 1.92 |
| Cognitive Construct × Treatment × Time Interaction | ||||
| Linear | 1.05 | 1.49 | 1.83 | 0.52 |
| Quadratic | 0.74 | 1.53 | 1.78 | 0.43 |
| Site effect | 1.59 | 2.35* | 1.40 | 2.35* |
Note. Model includes linear and quadratic effects of time.
p < .05.
p < .01.
Main effects of the cognitive constructs were detected for cognitive distortions, cognitive avoidance, and positive outlook, whereas a significant effect was not identified for solution-focused thinking. However, none of the cognitive constructs by treatment terms (two-way interactions) or cognitive constructs by treatment-by-time terms (three-way or four-way interactions) were significant.
Next, we tested whether including the significant main effects of the cognitive constructs reduced the effect of treatment on depression severity over the 36-week period. Taking change in cognitive distortions into account reduced the previous effect of treatment (linear treatment-by-time effect F = 11.31 to F = 5.13; quadratic treatment-by-time effect F= 8.60 to F = 4.03). Taking change in cognitive avoidance into account also reduced the effect of treatment (linear treatment-by-time effect F = 11.31 to F = 6.31, both p < .01; quadratic treatment-by-time effect F= 8.60 to F = 4.93, both p < .01). Similarly, change in positive outlook over 36 weeks reduced the effect of treatment (linear treatment-by-time effect F = 11.31 reduced to F = 5.88, both p < .01; quadratic treatment-by-time effect F = 8.60 to F = 5.23, both p < .01). Thus, change in cognitive distortions, cognitive avoidance, and positive outlook statistically contributed to change in depression over time. However, the fact that we did not detect any significant cognitive construct by treatment interactions indicates that inclusion of the cognitive constructs did not change the ordering of treatment outcomes. In other words, taking change in cognition into account does not explain why one treatment works better than another.
To assess which of these cognitive constructs was contributing the most to our final model of depression change, we ran another RRM including all the cognitive constructs that partially mediated depression severity (cognitive constructs 1–3). In this model, cognitive construct 3, positive outlook, was the only construct that remained significant as displayed in Table 4. The pseudo-R2 value for the difference between models with and without cognitive distortions, cognitive avoidance, and positive outlook suggested that approximately 45% of change in depression severity was accounted for by change in positive outlook.
TABLE 4.
The Effect of Cognitive Constructs on Depression Severity
| F | p | |
|---|---|---|
| Treatment | 0.48 | .61 |
| Time | 11.92 | <.01 |
| Time × Time | 5.88 | .02 |
| Treatment × Time | 5.87 | .01 |
| Treatment × Time × Time | 5.29 | .01 |
| Cognitive distortions (Factor 1) | 0.49 | .48 |
| Factor 1 × Time | 0.04 | .84 |
| Factor 1 × Time × Time | 0.08 | .78 |
| Cognitive avoidance (Factor 2) | .01 | .94 |
| Factor 2 × Time | 1.99 | .16 |
| Factor 2 × Time × Time | 1.93 | .17 |
| Positive outlook (Factor 3) | 14.98 | <.01 |
| Factor 3 × Time | 13.24 | <.01 |
| Factor 3 × Time × Time | 9.83 | <.01 |
| Site | 1.32 | .22 |
Discussion
This study examined whether change in cognitive constructs mediated change in depression severity across 36 weeks of treatment and whether cognitive change was a specific mechanism underlying CBT relative to antidepressant medication. Consistent with our hypotheses, we found that CBT both delivered alone and in combination with FLX was associated with decreased maladaptive cognitions and increased adaptive cognitions. Also in line with our hypotheses, we found evidence of mediation for the cognitive distortions, cognitive avoidance, and positive outlook constructs.
Of the three cognitive constructs, positive outlook was the most influential in predicting change in depression severity. The positive outlook construct was captured through items such as “I look forward to the future with hope and enthusiasm” and “The important people in my life are helpful and nice to me.” Because our positive outlook variable derives from a factor analysis, it is somewhat difficult to compare our construct with other studies examining adaptive cognition. In this study, this construct broadly captures a more adaptive and positive frame of mind (as assessed by the Cognitive Triad Inventory for Children) and a more hopeful perspective (as assessed by lower hopelessness on the Beck Hopelessness Scale). Thus, this study suggests that increasing more adaptive and hopeful cognitive sets may be more important than decreasing negative cognitive constructs among depressed adolescents.
The finding that positive outlook was the strongest mediator of depression symptoms is consistent with research, indicating that optimism is a significant predictor of depression symptoms among youth (Wong & Lim, 2009). Several interventions, such as the Penn Resiliency Program, have been designed to prevent depression and anxiety specifically by increasing resiliency and promoting hope (Gillham & Reivich, 2004; Reivich, Gillham, Chaplin, & Seligman, 2005). Recent studies examining mindfulness interventions with youth have also highlighted the efficacy of promoting well-being, as opposed to reducing suffering, among samples of clinical adolescents (e.g., Biegel, Brown, Shapiro, & Schubert, 2009). It is noteworthy, however, that the other positive construct—solution-focused thinking—was not a significant predictor of change in depression symptoms. The solution-focused thinking construct was based on a problem solving scale and a problem orientation scale. It is possible that our lack of findings for this construct may reflect developmental considerations such as ongoing improvements in problem-solving abilities across adolescence.
Counter to our expectations, we found that adolescents who received CBT alone experienced comparable cognitive change to those who received medication alone (FLX). In addition, we found that change in the FLX condition was mediated by change in cognition, and that adolescents who received the combination of CBT and FLX experienced the greatest change in cognition. Taken together, these results suggest that change in cognitive constructs may be a non-specific outcome following effective treatment of depressed adolescents and not necessarily a specific outcome following CBT. These results are consistent with some of the earlier studies of depressed adults, which found that antidepressant medication and CBT produced comparable change in cognition. Our pattern of results is also consistent with the TADS primary outcomes, suggesting that among adolescents with moderate to severe depression, the combination of FLX and CBT is the most effective treatment in reducing depression severity, decreasing negative cognitions, and increasing adaptive cognitions.
One potential explanation for our inability to find treatment-specific effects of CBT on cognition is that CBT with depressed youth exerts its effect through other mechanisms such as behavioral activation (e.g., Jacobson, Martell, & Dimidjian, 2001), cognitive measures we did not assess (i.e., rumination, autobiographical memory), or common therapeutic factors. In the adult depression literature, there is evidence that behavioral activation may be a key component of CBT; dismantling studies have found that behavioral activation produced equivalent outcomes to antidepressant medication and superior outcomes to cognitive therapy (emphasizing cognitive modification) in treating severe depression (Dimidjian et al., 2006). Current trials of behavioral activation as a treatment for depressed adolescents are underway and are needed to assess whether a behavioral intervention would be sufficient to produce significant change in cognitive constructs and depressive symptoms.
A paper by Longmore and Worrell (2007) entitled “Do We Need to Challenge Thoughts in Cognitive Behavior Therapy?” refers to the “empirical anomaly” in the CBT research literature that cognitive mediators often fail to explain the full impact of CBT (p. 182). The authors note that even though CBT has proven efficacious in the treatment of depression, it remains unclear whether or not changes in key cognitive processes represent the primary mechanism by which CBT diminishes depression. When interpreting studies such as this one that fail to find treatment-specific effects of CBT on cognition, it is important to consider two issues. First, as noted by Hollon, Stewart, and Strunk (2006), it is possible that CBT and medication exert different mechanisms of change even if they lead to similar cognitive changes. For instance, cognition and emotion could be conceptualized as reciprocal aspects of the same process, making it feasible that intervening in one domain would affect the other (Hollon et al., 1987). Second, as noted by Haaga (2007), there may be individual differences in how a treatment’s effects are mediated, further clouding the picture. Just as depression is multiply determined, so might improvement be multiply determined.
Limitations
Results of our study should be interpreted in the context of several potential limitations. First, cognition is a broad term encompassing many aspects of human experience. The self-report questionnaires that were used to derive the cognitive constructs measure what Ingram and Kendall (1986) have labeled cognitive products. Cognitive products may not be the most appropriate form of cognition to measure when examining potential mechanisms of change in depression severity. Priming mechanisms, such as mood induction techniques, may be one way of more sensitively measuring cognitive constructs. Additionally, cognitive change that occurs within individual sessions or from session to session can potentially be measured by coding client verbalizations (e.g., McNamara & Horan, 1986). These alternative approaches may offer a promising avenue for future investigation into mechanisms of change.
Second, it is possible that the assessment schedule used in TADS may have masked shorter term effects of cognitive change on symptom reduction. Furthermore, the assessment of depression and cognition at simultaneous points makes it difficult to establish which changed first, depression or cognition. As such, the TADS was not specifically designed to test mediators; however, we believe the current secondary analyses offer valuable preliminary evidence that change in cognition is related to treatment outcomes. For instance, future studies could seek to build on the current findings by leveraging technology, such as ecological momentary assessment, to measure the hypothesized mediators more frequently and more thoroughly evaluate the temporal ordering of change (Shiffman, Stone, & Hufford, 2008).
Last, it is important to note that the current results do not indicate which component of CBT led to changes in cognition. Dismantling studies that attempt to isolate the effects of specific CBT skills such as cognitive restructuring or behavioral activation are needed to address this question.
Clinical Implications
Notwithstanding the aforementioned limitations, we believe our study represents an important addition to the prior literature on mediators of CBT treatment for depressed youth. Specifically, the longitudinal nature of the study and extended 36-week follow-up period as well as broad assessment of cognition represent extensions of previous research. This study provides evidence that improvement in positive outlook mediates improvement in depression symptoms among moderately to severely depressed adolescents, but suggests that this improvement in positive outlook is not necessarily specific to CBT. Clinically, our results have two primary implications. First, our findings suggest that a teenager with high levels of maladaptive cognitions may respond more quickly to COMB as opposed to FLX or CBT alone and that monitoring an adolescent’s cognitive constructs, particularly their positive outlook, may offer an important additional indicator of improvement. Second, our results suggest that attempts to improve an adolescent’s level of positive and hopeful thinking may be more effective in reducing depression symptoms than attempts to reduce an adolescent’s level of negative thinking.
Figure 3.
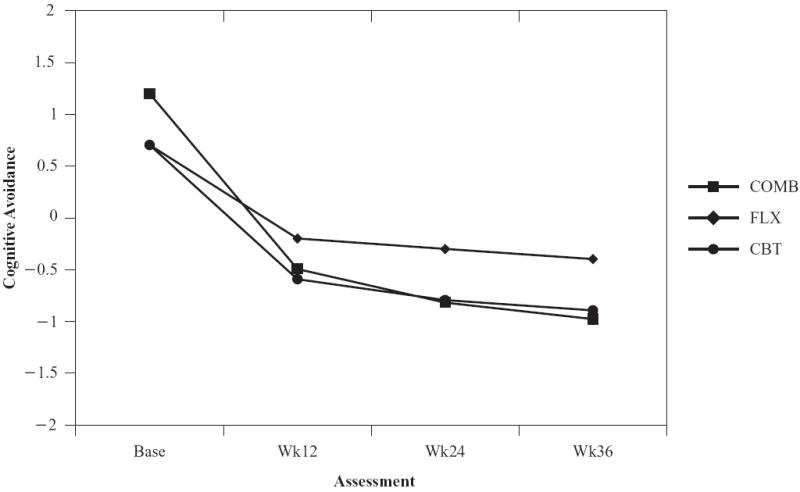
Mean cognitive avoidance over 36 weeks of treatment. COMB = combination of FLX and CBT; FLX = fluoxetine; CBT = cognitive behavioral therapy.
Contributor Information
Rachel H. Jacobs, University of Illinois at Chicago, Illinois.
Sara J. Becker, Brown Alpert Medical School, Providence, RI.
John F. Curry, Duke University, Durham, North Carolina.
Susan G. Silva, Duke University, Durham, North Carolina.
Golda S. Ginsburg, Johns Hopkins University School of Medicine, Baltimore, Maryland.
David B. Henry, University of Illinois at Chicago, Illinois.
Mark A. Reinecke, Northwestern University Feinberg School of Medicine, Chicago, Illinois.
References
- Allart-van Dam E, Hosman C, Hoogduin C, Schaap CP. The coping with depression course: Short-term outcomes and mediating effects of a randomized controlled trial in the treatment of subclinical depression. Behavior Therapy. 2003;34:381–396. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. text rev. [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. New York, NY: Guilford Press; 1979. [Google Scholar]
- Beck AT, Steer RA. Manual for the Beck Hopelessness Scale. San Antonio, TX: Psychological Corporation; 1988. [Google Scholar]
- Biegel GM, Brown KW, Shapiro SL, Schubert CM. Mindfulness-based stress reduction for the treatment of adolescent psychiatric outpatients: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2009;77(5):855–866. doi: 10.1037/a0016241. [DOI] [PubMed] [Google Scholar]
- Brooks SJ, Kutcher S. Diagnosis and measurement of adolescent depression: A review of commonly utilized instruments. Journal of Child and Adolescent Psychopharmacology. 2001;11(4):341–376. doi: 10.1089/104454601317261546. [DOI] [PubMed] [Google Scholar]
- Cheung AH, Emslie GJ, Mayes TL. Review of the efficacy and safety of antidepressants in youth depression. Journal of Child Psychology and Psychiatry. 2005;46(7):735–754. doi: 10.1111/j.1469-7610.2005.01467.x. http://dx.doi.org/10.1111/j.1469-7610.2005.01467.x. [DOI] [PubMed] [Google Scholar]
- Compton SN, March JS, Brent D, Albano AM, Weersing R, Curry J. Cognitive-behavioral psychotherapy for anxiety and depressive disorders in children and adolescents: An evidence-based medicine review. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43(8):930–959. doi: 10.1097/01.chi.0000127589.57468.bf. [DOI] [PubMed] [Google Scholar]
- Curry JF, Becker SJ. Empirically supported treatments for adolescent mood disorders. In: Steele R, Roberts M, Elkin D, editors. Handbook of evidence based therapies for children and adolescents. New York, NY: Springer Publishing; 2008. [Google Scholar]
- D’Zurilla TJ, Nezu AM, Maydeu-Olivares A. The social problem-solving inventory-revised (SPSI-R): Technical manual. North Tonawanda, NY: Multi-Health Systems; 2002. [Google Scholar]
- DeRubeis RJ, Evans MD, Hollon SD, Garvey MJ, Grove WM, Tuason VB. How does cognitive therapy work? Cognitive change and symptom change in cognitive therapy and pharmacotherapy for depression. Journal of Consulting and Clinical Psychology. 1990;58(6):862–869. doi: 10.1037//0022-006x.58.6.862. [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Hollon SD, Dobson KS, Schmaling KB, Kohlenberg RJ, Addis ME, Jacobson NS, et al. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. Journal of Consulting and Clinical Psychology. 2006;74(4):658–670. doi: 10.1037/0022-006X.74.4.658. http://dx.doi.org/10.1037/0022-006X.74.4.658. [DOI] [PubMed] [Google Scholar]
- Driessen E, Hollon SD. Cognitive behavioral therapy for mood disorders: Efficacy, moderators and mediators. The Psychiatric Clinics of North America. 2010;33(3):537–555. doi: 10.1016/j.psc.2010.04.005. http://dx.doi.org/10.1016/j.psc.2010.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillham JE, Reivich KJ. Cultivating optimism in childhood and adolescence. Annals of Political and Social Science. 2004;591:146–163. [Google Scholar]
- Ginsburg GS, Silva SG, Jacobs RH, Tonev S, Hoyle RH, Kingery JN, March JS, et al. Cognitive measures of adolescent depression: Unique or unitary constructs? Journal of Clinical Child and Adolescent Psychology. 2009;38(6):790–802. doi: 10.1080/15374410903259015. http://dx.doi.org/10.1080/15374410903259015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haaga DA. Could we speed this up? Accelerating progress in research on mechanisms of change in cognitive therapy of depression. Clinical Psychology: Science and Practice. 2007;14(3):240–243. [Google Scholar]
- Hollon SD, Stewart MO, Strunk D. Enduring effects for cognitive behavior therapy in the treatment of depression and anxiety. Annual Review of Psychology. 2006;57:285–315. doi: 10.1146/annurev.psych.57.102904.190044. http://dx.doi.org/10.1146/annurev.psych.57.102904.190044. [DOI] [PubMed] [Google Scholar]
- Hollon SD, DeRubeis RJ, Evans MD. Causal mediation of change in treatment for depression: Discriminating between nonspecificity and noncausality. Psychological Bulletin. 1987;102(1):139–149. http://dx.doi.org/10.1037/0033-2909.102.1.139. [PubMed] [Google Scholar]
- Imber SD, Pilkonis PA, Sotsky SM, Elkin I, Watkins JT, Collins JF, Glass DR, et al. Mode-specific effects among three treatments for depression. Journal of Consulting and Clinical Psychology. 1990;58(3):352–359. doi: 10.1037//0022-006x.58.3.352. [DOI] [PubMed] [Google Scholar]
- Ingram RE, Kendall PC. Cognitive clinical psychology: Implications of an information processing perspective. San Diego, CA: Academic Press; 1986. [Google Scholar]
- Jacobson NS, Martell CR, Dimidjian S. Behavioral activation (BA) treatment for depression: Returning to contextual roots. Clinical Psychology: Science and Practice. 2001;8(3):255–270. [Google Scholar]
- Kaslow NJ, Stark KD, Printz B, Livingston R, Tsai SL. Cognitive triad inventory for children: Development and relation to depression and anxiety. Journal of Clinical Child Psychology. 2002;21:339–347. [Google Scholar]
- Kaufman NK, Rohde P, Seeley JR, Clarke GN, Stice E. Potential mediators of cognitive-behavioral therapy for adolescents with comorbid major depression and conduct disorder. Journal of Consulting and Clinical Psychology. 2005;73(1):38–46. doi: 10.1037/0022-006X.73.1.38. http://dx.doi.org/10.1037/0022-006X.73.1.38. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Nock MK. Delineating mechanisms of change in child and adolescent therapy: methodological issues and research recommendations. Journal of Child Psychology and Psychiatry. 2003;44(8):1116–1129. doi: 10.1111/1469-7610.00195. [DOI] [PubMed] [Google Scholar]
- Klein JB, Jacobs RH, Reinecke MA. Cognitive-behavioral therapy for adolescent depression: A meta-analytic investigation of changes in effect-size estimates. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46(11):1403–1413. doi: 10.1097/chi.0b013e3180592aaa. http://dx.doi.org/10.1097/chi.0b013e3180592aaa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolko DJ, Brent DA, Baugher M, Bridge J, Birmaher B. Cognitive and family therapies for adolescent depression: Treatment specificity, mediation, and moderation. Journal of Consulting and Clinical Psychology. 2000;68(4):603–614. [PubMed] [Google Scholar]
- Kraemer HC, Kiernan M, Essex M, Kupfer DJ. How and why criteria defining moderators and mediators differ between the Baron & Kenny and MacArthur approaches. Health Psychology. 2008;27(2, Suppl):S101–108. doi: 10.1037/0278-6133.27.2(Suppl.).S101. http://dx.doi.org/10.1037/0278-6133.27.2(Suppl.).S101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59(10):877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Leitenberg H, Yost LW, Carroll-Wilson M. Negative cognitive errors in children: Questionnaire development, normative data, and comparisons between children with and without self-reported symptoms of depression, low self-esteem, and evaluation anxiety. Journal of Consulting and Clinical Psychology. 1986;54(4):528–536. doi: 10.1037//0022-006x.54.4.528. [DOI] [PubMed] [Google Scholar]
- Longmore RJ, Worrell M. Do we need to challenge thoughts in cognitive behavior therapy? Clinical Psychology Review. 2007;27(2):173–187. doi: 10.1016/j.cpr.2006.08.001. [DOI] [PubMed] [Google Scholar]
- McNamara K, Horan JJ. Experimental construct validity in the evaluation of cognitive and behavioral treatments for depression. Journal of Counseling Psychology. 1986;33:23–30. [Google Scholar]
- Muñoz RF, Ying YW, Bernal G, Pérez-Stable EJ, Sorensen JL, Hargreaves WA, Miller LS, et al. Prevention of depression with primary care patients: A randomized controlled trial. American Journal of Community Psychology. 1995;23(2):199–222. doi: 10.1007/BF02506936. [DOI] [PubMed] [Google Scholar]
- Poznanski EO, Mokros HB. Children’s Depression Rating Scale-Revised: Manual. Los Angeles, CA: Western Psychological Services; 1996. [Google Scholar]
- Reivich K, Gillham JE, Chaplin TM, Seligman MEP. From helplessness to optimism: The role of resilience in treating and preventing depression in youth. In: Goldstein S, Brooks RB, editors. Handbook of resilience in children. New York, NY: Kluwer Academic/Plenum; 2005. pp. 223–237. [Google Scholar]
- Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annual Review of Clinical Psychology. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- Simons AD, Garfield SL, Murphy GE. The process of change in cognitive therapy and pharmacotherapy for depression. Changes in mood and cognition. Archives of General Psychiatry. 1984;41(1):45–51. doi: 10.1001/archpsyc.1984.01790120049007. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. New York, NY: Oxford University Press; 2003. [Google Scholar]
- Steinberg L. Risk taking in adolescence: What changes, and why? Annals of the New York Academy of Sciences. 2004;1021:51–58. doi: 10.1196/annals.1308.005. [DOI] [PubMed] [Google Scholar]
- Stice E, Rohde P, Seeley JR, Gau JM. Testing mediators of intervention effects in randomized controlled trials: An evaluation of three depression prevention programs. Journal of Consulting and Clinical Psychology. 2010;78(2):273–280. doi: 10.1037/a0018396. http://dx.doi.org/10.1037/a0018396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strunk DR, DeRubeis RJ, Chiu AW, Alvarez J. Patients’ competence in and performance of cognitive therapy skills: Relation to the reduction of relapse risk following treatment for depression. Journal of Consulting and Clinical Psychology. 2007;75(4):523–530. doi: 10.1037/0022-006X.75.4.523. http://dx.doi.org/10.1037/0022-006X.75.4.523. [DOI] [PubMed] [Google Scholar]
- Teasdale JD, Scott J, Moore RG, Hayhurst H, Pope M, Paykel ES. How does cognitive therapy prevent relapse in residual depression? Evidence from a controlled trial. Journal of Consulting and Clinical Psychology. 2001;69(3):347–357. doi: 10.1037//0022-006x.69.3.347. [DOI] [PubMed] [Google Scholar]
- Treatment for Adolescents with Depression Study Team. Treatment for Adolescents With Depression Study (TADS): Rationale, design, and methods. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:531–542. doi: 10.1097/01.CHI.0000046839.90931.0D. [DOI] [PubMed] [Google Scholar]
- Treatment for Adolescents with Depression Study Team. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial. Journal of the American Medical Association. 2004;292(7):807–820. doi: 10.1001/jama.292.7.807. http://dx.doi.org/10.1001/jama.292.7.807. [DOI] [PubMed] [Google Scholar]
- Treatment for Adolescents with Depression Study Team. The Treatment for Adolescents With Depression Study (TADS): Demographic and clinical characteristics. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44(1):28–40. doi: 10.1097/01.chi.0000145807.09027.82. [DOI] [PubMed] [Google Scholar]
- Treatment for Adolescents with Depression Study Team. The Treatment for Adolescents With Depression Study (TADS): Long-term effectiveness and safety outcomes. Archives of General Psychiatry. 2007;64(10):1132–1143. doi: 10.1001/archpsyc.64.10.1132. http://dx.doi.org/10.1001/archpsyc.64.10.1132. [DOI] [PubMed] [Google Scholar]
- Weissman AN, Beck AT. Development and validation of the Dysfunctional Attitude Scale: A preliminary investigation; Paper presented at the 86th Annual Convention of the American Psychological Association; Toronto, Ontario, Canada. 1978. Sep, [Google Scholar]
- Wong SS, Lim T. Hope versus optimism in Singaporean adolescents: Contributions to depression and life satisfaction. Personality and Individual Differences. 2009;46:648–652. [Google Scholar]
- Weisz JR, McCarty CA, Valeri SM. Effects of psychotherapy for depression in children and adolescents: A meta-analysis. Psychological Bulletin. 2006;132(1):132–149. doi: 10.1037/0033-2909.132.1.132. http://dx.doi.org/10.1037/0033-2909.132.1.132. [DOI] [PMC free article] [PubMed] [Google Scholar]


