Abstract
Hereditary breast cancers have unique clinicopathological characteristics. Therefore, the objective of this study was to establish the relationship between self-reported family history of cancer and clinicopathological features in breast cancer patients from Washington, DC. Data on incident breast cancer cases from 2000 to 2010 were obtained from the Washington, DC Cancer Registry. Variables such as estrogen (ER), progesterone (PR), and human epidermal growth factor 2 (HER2) receptor status, as well as stage and grade, were analyzed in those that self-reported with (n = 1,734) and without a family history of cancer (n = 1,712). The breast cancer molecular subtypes were compared when ER, PR, and HER2 statuses were available. Furthermore, tumor characteristics were compared by race/ethnicity. Regression and chi-square analyses were performed. A report of family history was associated with age (OR = 1.27 95 % CI: 1.09–1.48; p < 0.0001), high grade tumors (OR = 1.29 95 % CI: 1.05–1.58; p = 0.02), and having ER and PR negative breast cancer (OR = 1.26 95 % CI: 1.02–1.57; p = 0.029). When tumor characteristics were compared by race/ethnicity, those that self-reported as African American with a family history had a higher frequency of ER negative tumors (OR = 1.51 95 % CI: 1.09–2.08; p = 0.008), PR negative tumors (OR = 1.46 95 % CI: 1.09–1.94; p = 0.028), grade 3 tumors (OR = 1.42 95 % CI: 1.05–1.93; p < 0.0001), and ER/PR negative tumors (OR = 1.5 95 % CI: 1.088–2.064; p = 0.01). These results suggest that a positive family history of cancer in African Americans should increase suspicions of hereditary cancer. Therefore, behavioral risk reduction activities, such as collecting a family history, may reduce late stage diagnosis and cancer mortality.
Introduction
The District of Columbia (DC) has the highest age-adjusted cancer mortality rate in the United States. According to the most recent cancer, 128.3 per 100,000 women were diagnosed with breast cancer between 2005 and 2009 in DC, and the city ranked 3rd overall in cancer mortality in the United States. Moreover, the city leads the nation in colorectal (23.3 per 100,000), prostate (41.3 per 100,000), breast (28.0 per 100,000), and pancreatic (16.3 per 100,000) cancer deaths. Of interest herein, the breast cancer incidence rate for women under the age of 50 in DC is one of the highest and surpasses the national average. Remarkably, one of the risk factors for hereditary or familial breast cancer is young age (50 or younger) at onset.
Another major risk factor for cancer and for familial cancer is history of a first-degree relative with breast cancer or a family history of cancer. Specifically, family history collection aims to identify the risk of selected single gene disorders for the purpose of offering appropriate specialist referral and management. Identifying individuals with a strong family history of cancer, providing genetic counseling, and testing as appropriate can provide patients with the tools necessary to reduce their risk of cancer in various ways. The family health history is one of the most powerful, but historically underutilized tools that helps to accurately predict breast cancer risk. Therefore, the collection of family health history, particularly as it relates to cancers, represents a valuable public health tool to assist individuals and their primary care providers (PCP) in accurately assessing risk and developing care plans accordingly.
For breast cancer, there is a two to threefold increased risk of breast cancer when at least one first-degree relative or two first-degree relatives have been affected with cancer (Butterworth 2007). The risk is substantially higher when family members are young (50 or younger) or premenopausal. Diagnosis of cancer at a younger age also increases suspicion that there is a hereditary BRCA1 or BRCA2 mutations in the family. Around 5–10 % of all breast cancers are associated with inherited mutations in BRCA1 and BRCA2. Individuals with mutations in BRCA1 and BRCA2 face the significant risks for breast cancer, 45–65 % by age 70, in addition to other cancers.
Notably, BRCA1 tumors appear to exhibit unique molecular characteristics, and recent studies indicate that triple negative or basal-like tumors are the most common subtypes exhibited by BRCA1 mutation carriers (Atchley et al. 2008; Lynch et al. 1998). The aggressive, triple negative molecular subtype is characterized by estrogen receptor (ER) negativity, progesterone receptor (PR) negativity, and human epidermal growth factor 2 (HER2) negativity and is associated with poor prognosis, unresponsiveness to typical endocrine therapy, and shortened survival. Women diagnosed with triple negative breast cancer also typically present at a younger age and with higher grade tumors.
Therefore, the objective of this study was to establish the relationship between self-reported family history of cancer and clinicopathological features in breast cancer patients from Washington, DC. A secondary aim is to determine if the characteristics were different by race/ethnicity. This study will provide further evidence that collection of family health history and tumor specific features can help us identify patients at risk for hereditary cancers. This study also highlights that family history is poorly collected because it is undervalued as genetic marker of breast cancer predisposition.
Materials and methods
This study was based on data formally requested from the DC Department of Health (DCDOH) Cancer Registry and was approved by the DC Department of Health Internal Review Board; therefore experiments comply with the current laws of the US. Mandated under existing laws, the DC Cancer Registry (DCCR) collects, maintains, and reports cancer incidence on all cancers diagnosed and/or treated in DC and tracks information regarding malignant cancers and certain benign tumors gathered from hospitals, laboratories, and other reporting agencies in DC. One of the variables, family history, relative with cancer, and type of cancer, is abstracted by the tumor registrar from physicians’ notes and entered into the registry. DCDOH has also entered into reciprocal exchange agreements for cancer information with its neighboring states to capture all occurrences of cancer among DC residents. The DCCR is one of the DCDOH’s most successful surveillance programs. Collected data elements are subjected to stringent protocols of completeness, accuracy, and timeliness. Since 1997, DCCR data has been carefully reviewed by the North American Association of Central Cancer Registries (NAACCR) and the National Program of Cancer Registries (NPCR).
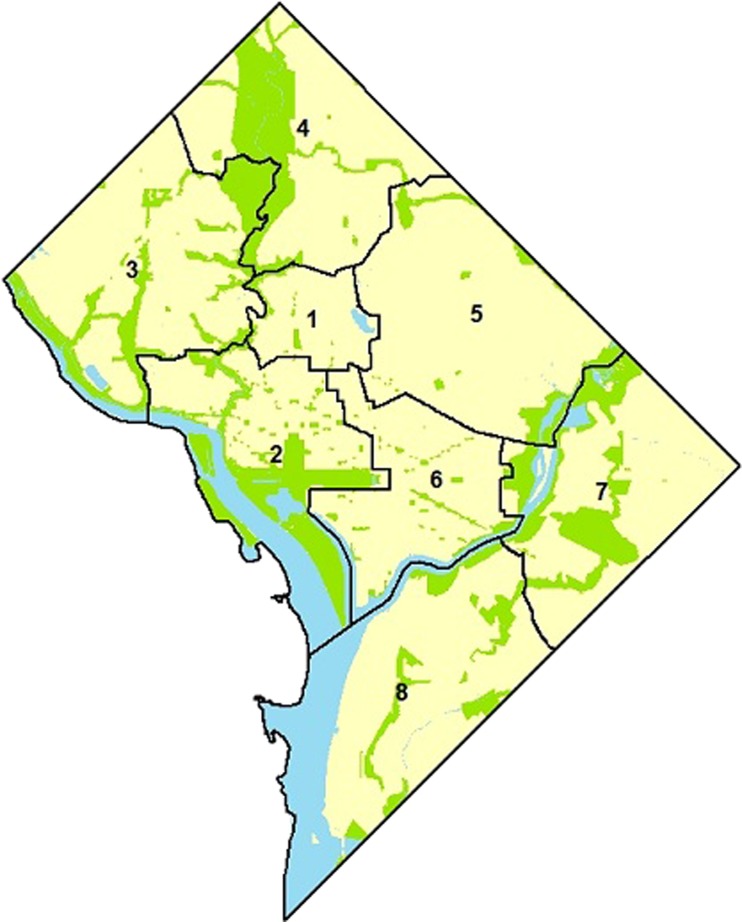
Eligibility criteria for the current study included all histologically confirmed malignant breast cancers in Washington, DC diagnosed between 2000 and 2010. All benign and stage 0 cases were excluded. Patients with duplicate records and multiple diagnoses were consolidated and coded as recurrences. Demographic variables (i.e., age at diagnosis, gender), tumor characteristics (i.e., size, stage, grade), treatment (i.e., surgery, radiation, chemotherapy, hormonal therapy), and socioeconomic variables (i.e., race, ward, marital status) were obtained from the cancer registry. Washington, DC is geographically divided into eight residential wards. Indicators of socioeconomic status and racial/ethnic diversity differ by ward (Fig. 1). Therefore, for this study, Ward was used as a proxy for socioeconomic status. In Ward 3, 77 % of residents are non-Hispanic EAs; the median income for these residents is >$97,000 per year with approximately 2 % of these residents living below the Federal Poverty Level. By contrast, in Ward 8, 93 % of the residents or more are AAs; their median income is less than $31,000 per year and more than 32 % of its residents live below the Federal Poverty Level (Price et al. 2012). Therefore, zip codes were categorized into Wards and Wards were stratified into two groups, namely Wards 7 and 8, which was compared to the group that included patients from Wards 1–6; 78.9 % of cases were located in wards 1 through 6.
Fig. 1.
Washington, DC geography, political structure, and demographics
Additionally hormone receptor (ER and PR) status and HER2/neu status were analyzed independently and together to determine the molecular subtype. ER and PR status was determined by immunohistochemistry, and HER2 was determined by fluorescence in situ hybridization (FISH). For this study, tumors that were ER and/or PR positive and HER2 negative were coded as luminal A; tumors that were ER and/or PR positive and HER2 positive were coded as luminal B; tumors that were ER and/or PR negative and HER2 positive were coded as HER2 overexpressing/amplified; and tumors negative for ER, PR, and HER2 were coded as triple negative.
A t test was performed to detect age differences between individuals who reported a family history compared to those who did not report a family history. To determine the association between categorical variables, bivariate or multivariate analysis was done using the χ2 test or Fisher’s exact test when appropriate (report of family history vs. race/ethnicity, ER, PR, HER2, molecular breast cancer subtype, grade, and age). The association between family health history and categorical variables was analyzed using multi-nominal logistic regression where odds ratios (ORs) and 95 % confidence intervals (CIs) were calculated with adjustment for potential confounders. Estimates were considered statistically significant for two-tailed values of p < 0.05. All analyses were carried out using the SPSS statistical program version 20 (SPSS Inc., Chicago, IL).
Results
Between 2000 and 2010, 5,932 breast cancers were diagnosed in 5,852 (98.7 %) women (Table 1). Of the cases, 1,762 (29.7 %) self-identified as white, 3,345 (56.4 %) self-identified as black, and 654 (11 %) self-identified as Hispanic. The mean age was 60.8 (±14.24), while patients under 50 comprised 25.6 % of cases. Stage I breast cancer had the highest incidence at 43.9 % followed by Stage II (35.9 %), Stage III (12.5 %), and Stage IV (7.7 %). In the reported cases, breast tumors tended to be of higher grade with 40.7 % being Grade II and 33.9 % being Grade III. ER, PR, and HER2 data were available for 2,936, 2,927, and 218 cases, respectively. Approximately 75 % were ER positive, 63.5 % PR positive, and 21.1 % HER2 positive/amplified. Subtypes were determined in patients whose ER, PR, and HER2 were known. Luminal A, luminal B, HER2 overexpressing/amplified breast cancer, and triple negative tumors comprised 60.6 %, 14.7 %, 6.4 %, and 18.3 % of the cancers, respectively. For those with ER and PR data, ER or PR positive tumors made up 75.8 % of all tumors. Recurrence was present in 17.4 % of cases. For this study, we used ward as a proxy for socioeconomic status; 78.9 % of cases were found in wards 1 through 6.
Table 1.
Characteristics of breast cancer cases in Washington, DC between 2000 and 2010 (n = 5,928)
| Frequency | % | |
|---|---|---|
| Gender | ||
| Female | 5,852 | 0.987 |
| Male | 76 | 0.013 |
| Race/ethnicity | ||
| Caucasian | 1,762 | 0.297 |
| African American | 3,345 | 0.564 |
| Hispanic | 654 | 0.11 |
| Age categories | ||
| <50 | 1,518 | 0.256 |
| >50 | 4,413 | 0.744 |
| Family history | ||
| None | 1,712 | 0.289 |
| Yes | 1,734 | 0.292 |
| Did not answer | 3,446 | 0.419 |
| Stage | ||
| I | 1,111 | 0.439 |
| II | 908 | 0.359 |
| III | 317 | 0.125 |
| IV | 195 | 0.077 |
| Grade | ||
| 1 | 705 | 0.154 |
| 2 | 1,868 | 0.407 |
| 3 | 2,013 | 0.339 |
| ER | ||
| Negative | 738 | 0.25 |
| Positive | 2,211 | 0.749 |
| PR | ||
| Negative | 1,071 | 0.364 |
| Positive | 1,869 | 0.635 |
| HER2 | ||
| Negative | 172 | 0.789 |
| Positive | 46 | 0.211 |
| Subtype | ||
| Luminal A | 132 | 0.606 |
| Luminal B | 32 | 0.147 |
| Her2 overexpressing | 14 | 0.064 |
| Triple negative | 40 | 0.183 |
| ER and PR negative | 709 | 0.242 |
| ER or PR positive | 2,226 | 0.758 |
| Recurrence | ||
| No | 4,848 | 0.817 |
| Yes | 1,023 | 0.174 |
| Vital status | ||
| Alive | 5,008 | 0.844 |
| Dead | 924 | 0.156 |
| DC wards | ||
| Wards 1–6 | 4,643 | 0.789 |
| Wards 7 and 8 | 1,245 | 0.211 |
When stratified by family history, differences in gender, age category, grade, PR status, and ER/PR negative status were found (Table 2). Specifically, those reporting a family history of cancer were younger (age = 59.10 ± 14.47 vs. 61.98 ± 13.33; p < 0.0001) and those categorized into the <50 age group were more likely to report a family history of cancer (OR = 1.27 95 % CI: 1.09–1.48; p < 0.0001); compared to females, males were less likely to report a family history of cancer (OR = 0.47 95 % CI: 0.26–0.88; p = 0.02). Additionally, those with a family history were more likely to have higher grade tumors (Grade 2 or 3 OR = 1.29 95 % CI: 1.05–1.58; p = 0.02). Furthermore, family history reporters had increased incidences of PR negative tumors (OR = 1.22 95 % CI: 1.01–1.47; p = 0.04) and ER/PR negative tumors (OR = 1.27 95 % CI: 1.02–1.57; p = 0.03). A report of family history was not associated with race/ethnicity, ER status or HER2 status (Table 2).
Table 2.
Association of report of family history of cancer with demographic and pathological markers
| No | Yes | |||||||
|---|---|---|---|---|---|---|---|---|
| n = 1,712 | % | n = 1,734 | % | p value | ||||
| Age | 61.98 ± 14.47 | 59.10 ± 13.33 | <0.0001a | |||||
| Age category | ||||||||
| >50 | 1,304 | 0.76 | 1,241 | 0.72 | ||||
| <50 | 408 | 0.24 | 493 | 0.28 | 0.00 | 1.27 | 1.09 | 1.48 |
| Gender | ||||||||
| Female | 1,679 | 0.98 | 1,717 | 0.99 | 1.00 | |||
| Male | 31 | 1.80 | 15 | 0.09 | 0.02 | 0.47 | 0.26 | 0.88 |
| Race | ||||||||
| Caucasian | 508 | 547 | 1.00 | |||||
| African American | 1,042 | 1,022 | 0.22 | 1.10 | 0.95 | 1.27 | ||
| Hispanic | 111 | 124 | 0.80 | 0.96 | 0.73 | 1.28 | ||
| Grade | ||||||||
| 1 | 234 | 0.17 | 198 | 0.13 | 1.00 | |||
| 2 | 545 | 0.39 | 618 | 0.42 | 0.01 | 0.75 | 0.60 | 0.93 |
| 3 | 634 | 0.45 | 666 | 0.45 | 0.05 | 0.81 | 0.66 | 1.00 |
| Grade 1 vs. 2/3 | 1,179 | 0.83 | 1,284 | 0.87 | 0.02 | 1.29 | 1.05 | 1.58 |
| ER | ||||||||
| Positive | 689 | 0.77 | 721 | 0.74 | 1.00 | |||
| Negative | 210 | 0.23 | 258 | 0.26 | 0.13 | 1.17 | 0.95 | 1.45 |
| PR | ||||||||
| Positive | 587 | 0.65 | 594 | 0.61 | 1.00 | |||
| Negative | 310 | 0.35 | 382 | 0.39 | 0.04 | 1.22 | 1.01 | 1.47 |
| HER2 | ||||||||
| Positive | 3 | 0.19 | 6 | 0.18 | 1.00 | |||
| Negative | 13 | 0.81 | 28 | 0.82 | 0.93 | 0.93 | 0.20 | 4.31 |
| ER/PR | ||||||||
| Positive | 701 | 0.78 | 720 | 0.74 | 1.00 | |||
| Both negative | 195 | 0.22 | 254 | 0.26 | 0.03 | 1.27 | 1.02 | 1.57 |
aIndependent t test F = 16.87, t = 6.08
Next, an analysis of only family history reported by race/ethnicity was performed to determine populations with increased incidences of hereditary features (Tables 3 and 4). Hispanics reporting a family history tended to be younger (OR = 1.44 95 % CI: 0.96–2.17; p = 0.08); African Americans appeared to have increased incidences of ER negative (OR = 1.51 95 % CI: 1.51–2.08; p = 0.01), PR negative (OR = 1.46 95 % CI: 1.10–1.94; p = 0.03), and ER negative/PR negative (OR = 1.50 95 % CI: 1.09–2.07; p = 0.01) tumors. Compared to Caucasians, African Americans, and Hispanics both appeared to have higher grade disease (OR [AAs] = 2.26 95 % CI: 1.65–3.11; p < 0.0001 and OR [Hispanics] = 2.41 95 % CI: 1.21–4.81; p = 0.01). Race/ethnicity was not associated with HER2 status in individuals who report a family history (Table 3).
Table 3.
Association of race with pathological markers in those reporting a family history of cancer
| Caucasian | % | African American | % | Hispanic | % | p valuea | |
|---|---|---|---|---|---|---|---|
| Age category | |||||||
| >50 | 388 | 0.71 | 753 | 0.74 | 78 | 0.63 | |
| <50 | 159 | 0.29 | 269 | 0.26 | 46 | 0.37 | 0.03 |
| Grade | |||||||
| 1 | 93 | 0.20 | 91 | 0.10 | 10 | 0.10 | |
| 2 | 214 | 0.47 | 336 | 0.38 | 53 | 0.51 | |
| 3 | 148 | 0.33 | 466 | 0.52 | 41 | 0.39 | <0.0001 |
| Grade 1 vs. 2/3 | 362 | 0.80 | 802 | 0.90 | 94 | 0.90 | <0.0001 |
| ER | |||||||
| Positive | 249 | 0.78 | 392 | 0.70 | 64 | 0.82 | |
| Negative | 71 | 0.22 | 169 | 0.30 | 14 | 0.18 | 0.01 |
| PR | |||||||
| Positive | 211 | 0.66 | 320 | 0.57 | 50 | 0.64 | |
| Negative | 108 | 0.34 | 239 | 0.43 | 28 | 0.36 | 0.03 |
| HER2 | |||||||
| Positive | 1 | 0.11 | 4 | 0.22 | 1 | 0.14 | |
| Negative | 8 | 0.89 | 14 | 0.78 | 6 | 0.86 | 0.75 |
| ER/PR | |||||||
| Either positive | 248 | 0.78 | 392 | 0.70 | 64 | 0.82 | |
| Both negative | 70 | 0.22 | 166 | 0.30 | 14 | 0.18 | 0.01 |
aFor African Americans vs. Caucasians
Table 4.
Logistic regression analysis of tumor characteristics by race in those reporting a family history of cancer
| Age <50 | p value | ER negative | p value | PR negative | p value | ER and PR | p value | Grade | p value | |
|---|---|---|---|---|---|---|---|---|---|---|
| Caucasian | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| African American | 0.87 (0.69–1.09) |
0.25 | 1.51 (1.09–2.08) |
0.01 | 1.46 (1.10–1.94) |
0.03 | 1.50 (1.09–2.07) |
0.01 | 2.26 (1.65–3.11) |
<0.0001 |
| Hispanic | 1.44 (0.96–2.17) |
0.08 | 0.77 (0.41–1.45) |
0.41 | 1.08 (0.64–1.82) |
0.77 | 0.77 (0.41–1.46) |
0.43 | 2.41 (1.21–4.81) |
0.01 |
Discussion
The objective of this study was to establish the relationship between self-reported family history of cancer and clinicopathological features in breast cancer patients from Washington, DC. We found that report of family history of cancer was associated with ER and PR negative breast cancer status and breast cancer diagnosis under the age of 50. A secondary aim is to determine if the characteristics were different by race/ethnicity. When tumor characteristics were compared by race/ethnicity, those who self-reported as African American with a family history had a higher frequency of ER negative tumors, PR negative tumors, grade 3 tumors, and ER/PR negative tumors. This study confirms that clinicopathological characteristics of patients reporting a family history are consistent with clinicopathological characteristics in patients with hereditary and familial cancer syndromes.
It is well established that patients with BRCA1 mutation have distinct characteristics (Atchley et al. 2008; Lynch et al. 1998; Musolino et al. 2005) and BRCA1 tumors are more aggressive, have a tendency towards ER negative/PR negative, and the triple negative (estrogen receptor (ER) negative, progesterone receptor (PR) negative, and HER2/neu negative) subtype. Triple negative (TN) breast cancers have no targeted therapies available to them and have a worse survival compared with ER+ and PR+ breast cancer. Pre-menopausal African American, British black, Hispanic, and African have a higher prevalence of TN breast cancer compared to post-menopausal and Caucasian women (Bauer et al. 2007; Bowen et al. 2008; Carey et al. 2006; Olopade et al. 2003). In fact, the TN subtype has also been shown to be the most prominent in African American women under 35 years of age (Ihemelandu et al. 2007a). Further, in Washington, DC, African American (AA) women show increased incidences of triple negative and ER/PR negative breast cancer (data not shown) and some increased lethality from triple negative breast cancer (Ihemelandu et al. 2007a, b) compared to Caucasian women (Morris et al. 2007). However, the actual prevalence of hereditary or BRCA1/2 breast cancer in AAs and other ethnically diverse populations is unknown.
Still the US Preventive Services and Task Force (USPTF) recommends that women with a family history of breast cancer should be referred for genetic testing and counseling (GCT) (2005). They determined that these women would benefit from genetic counseling that allows informed decision-making about testing and further prophylactic treatment. For example, women with BRCA1/2 genetic mutations have choices that range from prophylactic surgery to prevent breast and ovarian cancer to surveillance or watchful waiting. However, lack of awareness of family health history by patients and their providers diminishes these important opportunities for intervention.
There are also several reasons for the underutilization of GCT. One issue is lack of awareness of the availability of genetic testing for cancer predisposition. For example, the results of a survey of genetic tests for cancer risk indicated that about half the US population was aware of genetic testing in the clinical setting (Wideroff et al. 2003). On the other hand, several studies have shown disparities in awareness between Whites and AAs. This has dire implications in AAs, because our study shows that they have an increased likelihood of features related to hereditary breast cancer. In fact, AAs are less likely to report awareness of genetic testing, discuss cancer related issues with family members, and generally underestimate their risk of breast cancer (Matthews et al. 2000; Wideroff et al. 2003).
Another reason for decreased use of GCT in minorities is access. Whites compared to Blacks in the US have more frequent access to genetic testing for predisposition to cancer (Gramling et al. 2009). For example, Armstrong et al. found that the odds ratio (ORs) for AAs undergoing genetic counseling was 0.22 (0.12–0.40) compared to their White counterparts (Armstrong et al. 2005). Additionally, genetic testing is very expensive and may be inaccessible to individuals with fewer financial resources. Moreover, health insurance may not cover its use or may cover its use under very stringent conditions. As indicated by our research, these stringent conditions may not be sensitive enough to detect a significant number of individuals who may be BRCA1/2 positive in ethnically diverse populations. Therefore, the use of genetic counseling and testing (GCT) for primary cancer prevention is yet another area of medicine in which disparities occur.
Another barrier to utilization of GCT lies with the referring physician. The role of the physician in identifying and referring high-risk patients for genetic counseling cannot be underestimated. Advances in the field has necessitated that healthcare providers integrate genetics into the risk assessment and management of families with cancer. However, most PCPs have little experience or training relevant to genetic testing, and many lack confidence and skill in this area of practice. Additionally, research has shown that minority-serving physicians were less likely to have ever ordered a genetic test to assess breast cancer risk (18 % vs. 29 %) compared to those serving fewer minority patients and were also less likely to have ever referred a patient for genetic testing to a genetics center or counselor (52 % vs. 64 %) (Shields et al. 2008). Additionally, they found that physicians serving a disproportionate share of Medicaid patients were also significantly less likely to have ever referred a patient to a counselor. Notably, in the District of Columbia, Medicare and not Medicaid, covers genetic counseling and testing, leaving a large proportion of the population unable to receive access to genetic resources. This could be why physicians with patients with high socioeconomic status are more likely to make referrals for GCT.
Despite the aforementioned disparities, when presented with a list of possible advantages of cancer genetic risk assessment, AAs have repeatedly agreed with the benefits of genetic testing (Kinney et al. 2001; Matthews et al. 2000; Thompson et al. 2002). More specifically, AAs have reported that cancer genetic risk assessment would help: (a) motivate them to perform breast self-examinations and/or mammograms more regularly; (b) inform family members about their potential risk of developing cancer; (c) improve decision-making regarding preventive care; (d) increase emotional reassurance; (e) possibly reduce feelings of uncertainty and increase a sense of control; and (f) contribute to finding a cure (Kinney et al. 2001; Matthews et al. 2000; Thompson et al. 2002). These findings support the benefit of GCT awareness campaigns in communities of color like Washington, DC where the population is one of the most diverse in the Nation.
There were several limitations to the study presented herein. First, although tumor registrars systematically abstract family history data from physicians’ notes, it is not known if physicians systematically collect such information. Other studies have found that while most family physicians consider family history as an important clinical tool, there are several barriers that prevent the collection of such information (Flynn et al. 2010; Wood et al. 2008; Yoon et al. 2002). These barriers include lack of time (Burke et al. 2002; Fuller et al. 2010; Rich et al. 2004; Williams et al. 2011); because of lack of accurate information provided by the patient (Flynn et al. 2010; Rich et al. 2004; Suther and Goodson 2004; Williams et al. 2011; Wood et al. 2008); and lack of clear guidelines and recommendations for the collection and interpretation of the family history, risk assessment, and any subsequent referrals to secondary care (Fuller et al. 2010; Suther and Goodson 2004; Washington 2006; Wood et al. 2008). In the US, 63 % of family physicians report to know the family history of at least three quarters of their patients (Acton et al. 2000). Lower collection rates have also been published (Daelemans et al. 2013; Flynn et al. 2010). In a more recent study, approximately half of the surveyed physicians confirmed knowing the family history of at least 50 % of their patients (Daelemans et al. 2013). This is consistent with the DC registry’s collection of family health history in approximately 50 % of their patients.
Another limitation was that a family history of all cancers and not just breast cancer was entered into the registry. That could be the reason why the rate of those who reported a positive family history was high (∼50 %) among those who reported a positive and negative family history. In general, 30 % of breast cancer patients report a family history of breast cancer. It’s important to note that the National Comprehensive Cancer Network guidelines for hereditary breast and ovarian cancer (HBOC) list additional component cancers such as fallopian tube, pancreatic, and prostate cancer. Therefore, information on other cancers should be collected although for HBOC.
Still, our study was consistent with others in that the types of tumor characteristics found in BRCA1/2 cancers were found in those self-reporting family histories of cancer. Our data shows that the tumor characteristics of familial breast cancer are more highly pronounced in African Americans compared to Caucasians and Hispanics and warrant early detection and behavioral risk reduction activities, such as collecting a family health history, which may greatly reduce late stage diagnosis and cancer mortality. Developing tailored behavioral prevention messages aimed at risk reduction, improving utilization of cancer screening, increasing the use of chemopreventive options, and surgical intervention for inherited cancers may have an additional impact on the District’s cancer mortality rate.
Acknowledgments
Compliance and ethics
Experiments comply with the current laws of the US.
Financial support
This project has been funded in whole or in part with Federal funds from the National Center for Research Resources (NCRR-UL1RR031975), National Institutes of Health, through the Clinical and Translational Science Awards Program (CTSA), a trademark of DHHS, part of the Roadmap Initiative, “Re-Engineering the Clinical Research Enterprise”; from the RCMI Program at Howard University, Division of Research Infrastructure, National Center for Research Resources, NIH (NCRR-G12 RR003048) and the Howard University Cancer Center/Johns Hopkins Cancer Center Partnership, National Cancer Institute (NCI-U54 CA091431).
Disclosures
None.
References
- (2005) Risk Assessment, Genetic Counseling, and Genetic Testing for BRCA-Related Cancer in Women, Topic Page. U.S. Preventive Services Task Force. http://www.uspreventiveservicestaskforce.org/uspstf/uspsbrgen.htm [DOI] [PubMed]
- Acton RT, Burst NM, Casebeer L, Ferguson SM, Greene P, Laird BL, Leviton L. Knowledge, attitudes, and behaviors of Alabama’s primary care physicians regarding cancer genetics. Acad Med. 2000;75(8):850–852. doi: 10.1097/00001888-200008000-00021. [DOI] [PubMed] [Google Scholar]
- Armstrong K, Micco E, Carney A, Stopfer J, Putt M. Racial differences in the use of BRCA1/2 testing among women with a family history of breast or ovarian cancer. JAMA. 2005;293(14):1729–1736. doi: 10.1001/jama.293.14.1729. [DOI] [PubMed] [Google Scholar]
- Atchley DP, Albarracin CT, Lopez A, Valero V, Amos CI, Gonzalez-Angulo AM, Hortobagyi GN, Arun BK. Clinical and pathologic characteristics of patients with BRCA-positive and BRCA-negative breast cancer. J Clin Oncol. 2008;26(26):4282–4288. doi: 10.1200/JCO.2008.16.6231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer KR, Brown M, Cress RD, Parise CA, Caggiano V. Descriptive analysis of estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, and HER2-negative invasive breast cancer, the so-called triple-negative phenotype: a population-based study from the California cancer Registry. Cancer. 2007;109(9):1721–1728. doi: 10.1002/cncr.22618. [DOI] [PubMed] [Google Scholar]
- Bowen RL, Duffy SW, Ryan DA, Hart IR, Jones JL. Early onset of breast cancer in a group of British black women. Br J Cancer. 2008;98(2):277–281. doi: 10.1038/sj.bjc.6604174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke W, et al. Genetics in primary care: a USA faculty development initiative. Community Genet. 2002;5(no. 2):138–146. doi: 10.1159/000065165. [DOI] [PubMed] [Google Scholar]
- Butterworth A (2007) Family history as a risk factor for common, complex disease. Public Health Genet
- Carey LA, et al. Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA. 2006;295(21):2492–2502. doi: 10.1001/jama.295.21.2492. [DOI] [PubMed] [Google Scholar]
- Daelemans S, Vandevoorde J, Vansintejan J, Borgermans L, Devroey D. The use of family history in primary health care: a qualitative study. Adv Prev Med. 2013;2013 doi: 10.1155/2013/695763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flynn BS, Wood ME, Ashikaga T, Stockdale A, Dana GS, Naud S. Primary care physicians’ use of family history for cancer risk assessment. BMC Fam Pract. 2010;11:45. doi: 10.1186/1471-2296-11-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller M, Myers M, Webb T, Tabangin M, Prows C. Primary care providers’ responses to patient-generated family history. J Genet Couns. 2010;19(1):84–96. doi: 10.1007/s10897-009-9264-6. [DOI] [PubMed] [Google Scholar]
- Gramling R, Clarke J, Simmons E. Racial distribution of patient population and family physician endorsed importance of screening patients for inherited predisposition to cancer. J Health Care Poor Underserved. 2009;20(1):50–54. doi: 10.1353/hpu.0.0107. [DOI] [PubMed] [Google Scholar]
- Ihemelandu CU, Leffall LD, Jr, Dewitty RL, Naab TJ, Mezghebe HM, Makambi KH, Adams-Campbell L, Frederick WA. Molecular breast cancer subtypes in premenopausal African-American women, tumor biologic factors and clinical outcome. Ann Surg Oncol. 2007a;14(10):2994–3003. doi: 10.1245/s10434-007-9477-6. [DOI] [PubMed] [Google Scholar]
- Ihemelandu CU, Leffall LD, Jr, Dewitty RL, Naab TJ, Mezghebe HM, Makambi KH, Adams-Campbell L, Frederick WA. Molecular breast cancer subtypes in premenopausal and postmenopausal African-American women: age-specific prevalence and survival. J Surg Res. 2007b;143(1):109–118. doi: 10.1016/j.jss.2007.03.085. [DOI] [PubMed] [Google Scholar]
- Kinney AY, Croyle RT, Dudley WN, Bailey CA, Pelias MK, Neuhausen SL. Knowledge, attitudes, and interest in breast–ovarian cancer gene testing: a survey of a large African-American kindred with a BRCA1 mutation. Prev Med. 2001;33(6):543–551. doi: 10.1006/pmed.2001.0920. [DOI] [PubMed] [Google Scholar]
- Lynch BJ, Holden JA, Buys SS, Neuhausen SL, Gaffney DK. Pathobiologic characteristics of hereditary breast cancer. Hum Pathol. 1998;29(10):1140–1144. doi: 10.1016/S0046-8177(98)90427-0. [DOI] [PubMed] [Google Scholar]
- Matthews AK, Cummings S, Thompson S. Genetic testing of African Americans for susceptibility to inherited cancers. J Psycological Oncol. 2000;18:1–13. doi: 10.1300/J077v18n02_01. [DOI] [Google Scholar]
- Morris GJ, et al. Differences in breast carcinoma characteristics in newly diagnosed African-American and Caucasian patients: a single-institution compilation compared with the National Cancer Institute’s Surveillance, Epidemiology, and End Results database. Cancer. 2007;110(4):876–884. doi: 10.1002/cncr.22836. [DOI] [PubMed] [Google Scholar]
- Musolino A, et al. Molecular profile and clinical variables in BRCA1-positive breast cancers. A population-based study. Tumori. 2005;91(6):505–512. doi: 10.1177/030089160509100611. [DOI] [PubMed] [Google Scholar]
- Olopade OI, Fackenthal JD, Dunston G, Tainsky MA, Collins F, Whitfield-Broome C. Breast cancer genetics in African Americans. Cancer. 2003;97(1 Suppl):236–245. doi: 10.1002/cncr.11019. [DOI] [PubMed] [Google Scholar]
- Price RA, Blanchard JC, Harris RJ, Ruder T, Gresenz CR (2012) Monitoring cancer outcomes across the continuum: data synthesis and analysis for the District of Columbia. Technical Report. RAND Corporation [PMC free article] [PubMed]
- Rich EC, Burke W, Heaton CJ, Haga S, Pinsky L, Short MP, Acheson L. Reconsidering the family history in primary care. J Gen Intern Med. 2004;19(3):273–280. doi: 10.1111/j.1525-1497.2004.30401.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shields AE, Burke W, Levy DE. Differential use of available genetic tests among primary care physicians in the United States: results of a national survey. Genet Med. 2008;10(6):404–414. doi: 10.1097/GIM.0b013e3181770184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suther SG, Goodson P. Texas physicians’ perceptions of genomic medicine as an innovation. Clin Genet. 2004;65(5):368–377. doi: 10.1111/j.0009-9163.2004.00253.x. [DOI] [PubMed] [Google Scholar]
- Thompson HS, et al. Psychosocial predictors of BRCA counseling and testing decisions among urban African-American women. Cancer Epidemiol Biomarkers Prev. 2002;11(12):1579–1585. [PubMed] [Google Scholar]
- Washington H (2006) Medical Apartheid: the dark history of medical experimentation on Black Americans from colonial times to the present. Doubleday Books
- Wideroff L, Vadaparampil ST, Breen N, Croyle RT, Freedman AN. Awareness of genetic testing for increased cancer risk in the year 2000 National Health Interview Survey. Community Genet. 2003;6(no. 3):147–156. doi: 10.1159/000078162. [DOI] [PubMed] [Google Scholar]
- Williams JL, Collingridge DS, Williams MS. Primary care physicians’ experience with family history: an exploratory qualitative study. Genet Med. 2011;13(1):21–25. doi: 10.1097/GIM.0b013e3181f928fc. [DOI] [PubMed] [Google Scholar]
- Wood ME, Stockdale A, Flynn BS. Interviews with primary care physicians regarding taking and interpreting the cancer family history. Fam Pract. 2008;25(5):334–340. doi: 10.1093/fampra/cmn053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon PW, Scheuner MT, Peterson-Oehlke KL, Gwinn M, Faucett A, Khoury MJ. Can family history be used as a tool for public health and preventive medicine? Genet Med. 2002;4(4):304–310. doi: 10.1097/00125817-200207000-00009. [DOI] [PubMed] [Google Scholar]