Abstract
We investigated whether luteolin affects the gene expression, secretion and activity of matrix metalloproteinase-3 (MMP-3) in primary cultured rabbit articular chondrocytes, as well as production of MMP-3 in the rat knee to evaluate the potential chondro-protective effects of luteolin. Rabbit articular chondrocytes were cultured in a monolayer and IL-1β-induced gene expression levels of MMP-3, MMP-1, MMP-13, a disintegrin and metalloproteinase with thrombospondin motifs-4 (ADAMTS-4), ADAMTS-5 and type II collagen were measured by reverse transcription - polymerase chain reaction (RT-PCR). Effects of luteolin on interleukin-1β (IL-1β)-induced secretion and enzyme activity of MMP-3 in rabbit articular chondrocytes were investigated by western blot analysis and casein zymography, respectively. The effect of luteolin on MMP-3 protein production was also examined in vivo. The results were as follows: (1) luteolin inhibited the gene expression levels of MMP-3, MMP-1, MMP-13, ADAMTS-4 and ADAMTS-5. However, it increased the gene expression level of collagen in rabbit articular chondrocytes; (2) luteolin inhibited the secretion and activity of MMP-3; (3) luteolin inhibited in vivo production of MMP-3 protein. These results suggest that luteolin can regulate the gene expression, secretion and activity of MMP-3, by directly acting on articular chondrocytes.
Keywords: Osteoarthritis, Luteolin, Chondrocyte
INTRODUCTION
Osteoarthritis is the most common degenerative articular disease affecting millions of people, in particular the elderly. The synovial inflammation, formation of osteophyte, changes in subchondral bone and degeneration of articular cartilage are the major pathophysiologic features of osteoarthritis. The cause of osteoarthritis is unclear, and it involves multiple biochemical and mechanical factors. During the progression of osteoarthritis, the equilibrium between physiologic synthesis and degradation of articular cartilage is disrupted (Mankin, 1982; Aigner and McKenna, 2002).
It has been reported that the activation of degradative enzymes leads to the loss and degradation of proteoglycans and collagen in articular cartilage, and the matrix metalloproteinase (MMP) plays a pivotal role in the destruction of articular cartilage in patients who are suffering from osteoarthritis (Dean et al., 1989; Kullich et al., 2007). Among the various matrix metalloproteinase including collagenases (MMP-1, -8 and -13), gelatinases (MMP-2 and -9) and stromelysins (MMP-3, -7, -10 and -11) (Birkedal-Hansen et al., 1993; Burrage et al., 2006), MMP-3 degrades proteoglycans and activate procollagenase in articular cartilage (Garnero et al., 2000; Lin et al., 2004). In an experimental model of osteoarthritis, the role of MMP-3 in damage of articular cartilage was demonstrated. MMP-3 protein was reported to be expressed in the synovium and the surface of cartilage in the knee joints and in pannus-like tissue of patients with osteoarthritis (Okada et al., 1992; Shibakawa et al., 2003; Kobayashi et al., 2005; Blom et al., 2007).
Therefore, we suggest it is valuable to find the potential action of regulating (inhibiting) the activity, secretion and gene expression of MMP-3 by the natural products derived from medicinal plants used as empirical remedies for arthritis.
According to many reports, luteolin, a flavonoidal compound derived from diverse medicinal plants showing anti-inflammatory and anti-oxidative activities, has shown anti-inflammatory, anti-oxidative and anti-carcinogenic effects (Manju and Nalini, 2007; Jung et al., 2012; Sun et al., 2012). Luteolin and its analogues showed anti-arthritic effects in experimental models of rheumatoid arthritis and infectious arthritis (Lee and Kim, 2010; Lee and Han, 2011; Impellizzeri et al., 2013). Furthermore, luteolin has been reported to affect the proliferation and function of synovial fibroblasts in rats (Hou et al., 2009), and to suppress the activities of the other degradative enzymes, a disintegrin and metalloproteinase with thrombospondin motifs (ADAMTS)-4 & 5 (Moncada-Pazos et al., 2011). Choi and Lee reported that luteolin affected interleukin-1β (IL-1β)-induced production of MMPs and cytokines in the SW982 synovial sarcoma cell line (Choi and Lee, 2010).
However, to the best of our knowledge, there are no reports about the effects of luteolin on gene expression, secretion and activity of MMP-3, an articular cartilage-degradative enzyme that decomposes proteoglycans, in primary cultured rabbit articular chondrocytes or on production of MMP-3 in the rat knee. Therefore, we examined the effect of luteolin on IL-1β-induced gene expression, secretion and activity of MMP-3 in vitro and production of MMP-3 in vivo, in order to evaluate the potential chondroprotective effect of luteolin.
MATERIALS AND METHODS
Materials
All the chemicals and reagents used in this experiment including luteolin (purity: 95.0%) were purchased from Sigma (St. Louis, MO, USA) unless otherwise specified. Dulbecco’s Modified Eagle’s Medium (DMEM) was purchased from Gibco BRL (Grand Island, NY, USA) and recombinant human IL-1β was purchased from R&D Systems (Minneapolis, MN, USA).
Primary cultures of chondrocytes from rabbit articular cartilage
Male New Zealand White Rabbits (Daehan Biolink, Seoul, Korea) were obtained from at 2 weeks of age. Animals were housed one per cage and provided with distilled water and food ad libitum. They were kept under a 12 h light/dark cycle (lights on from 08:00 to 20:00) at constant temperature (22.5°C) and humidity (55%). Animals were cared through all of the experimental procedures in accordance with the Guide for the Care and Use of Laboratory Animals regulated by Chungnam National University, Daejeon, Korea. Rabbit articular chondrocytes were isolated from the tibial plateaus and femoral condyle in cartilage of the knee joints. Cartilage was washed in phosphate-buffered saline (PBS) and minced into pieces measuring about 2 mm3. Cartilage tissue was digested for 4 h with 0.2% type II collagenase at 37°C. After collection of individual cells by brief centrifugation, the cells were transferred to 100 mm culture dishes (seeding density: 105 cells/cm2) in 12 mL DMEM supplemented with 10% fetal bovine serum (FBS), in the presence of penicillin (100 units/mL) and streptomycin (100 μg/mL). Cells were cultured at 37°C in a humidified, 5% CO2/95% air, water-jacketed incubator (Sanyo, Tokyo, Japan). The medium was replaced every other day.
Treatment of cells with luteolin and the other natural products
Chondrocytes were seeded on 6-well culture plates at a density of 105 cells/cm2. After 2 days in monolayer culture, the cells were incubated for 2 h in growth medium with 1, 10, 50, or100 μM of luteolin, fisetin, quercetin or ferulic acid, respectively, followed by incubation in the presence or absence of IL-1β (10 ng/mL) for 24 h. Luteolin, fisetin, quercetin or ferulic acid was dissolved in dimethylsulfoxide (DMSO), diluted in PBS, and administerted in culture medium (final concentrations of DMSO were 0.5%). The final pH values of these solutions were between 7.0 and 7.4. Culture medium and 0.5% DMSO in medium did not affect gene expression, secretion and activity of MMP-3 in primary cultured chondrocytes. The supernatant was collected, centrifuged, and both cell and supernatant fractions were stored at −80°C until use.
Cytotoxicity assay
Chondrocytes were seeded at a density of 2×105/mL (0.1 mL/well) in a 96-well microtiter plate, and allowed to attach for 24 h to keep the log phase growth at the time of drug treatment. Luteolin, fisetin, quercetin or ferulic acid was dissolved in DMSO, and administered in DMEM supplemented with 10% FBS (final concentrations of DMSO were under 0.5%). 0.5% DMSO alone did not affect the proliferation of chondrocytes. After incubation with the indicated drug concentrations for 72 h, cell proliferation was determined using the sulforhodamine B (SRB) assay (Skehan et al., 1990).
Isolation of total RNA and RT-PCR
Total RNA was isolated from chondrocytes using Easy-BLUE Extraction Kit (INTRON Biotechnology, Kyung-ki-do, Korea) and reverse transcribed by using AccuPower RT Premix (BIONEER Corporation, Daejeon, Korea) according to the manufacturer’s instructions. 2 μg of total RNA was primed with 1 μg of oligo (dT) in a final volume of 30 μL (RT reaction). 2 μL of RT reaction product was PCR amplified in 20 μL using Thermoprime Plus DNA Polymerase (ABgene, Rochester, NY, USA). PCR was performed with the following primers: MMP-3 (5′ATG GAC CTT CTT CAG CAA 3′; 5′TCA TTA TGT CAG CCT CTC 3′); MMP-13 (5′AGG AGC ATG GCG ACT TCT AC 3′; 5′TAA AAA CAG CTC CGC ATC AA 3′); MMP-1 (5′TCA GTT CGT CCT CAC TCC AG 3′; 5′TTG GTC CAC CTG TCA TCT TC 3′); ADAMTS-4 (5′CAA GGT CCC ATG TGC AAC GT 3′; 5′CAT CTG CCA CCA CCA GTG TCT 3′); ADAMTS-5 (5′TGT CCT GCCAGC GGATGT 3′; 5′ACG GAA TTA CTG TAC GGC CTA CA 3′); type II collagen (5′AAC ACT GCC AAC GTC CAG AT 3′; 5′CTG ACG CAC GGT ATA GGT GA 3′). As quantitative controls, primers for GAPDH (5′ACT GGC GTC TTC ACC ACC AT 3′; 5′AAG GCC ATG CCA GTG AGC TT 3′) were used. The PCR products increased as the concentration of RNA increased. The amplified fragment sizes were 350 base pairs (bp) for MMP-3, 458 bp for MMP-13, 300 bp for MMP-1, 90 bp for ADAMTS-4, 110 bp for ADAMTS-5, 220 bp for type II collagen and 400 bp for GAPDH. After PCR, 15 μL of PCR products were subjected to 2% agarose gel electrophoresis and visualized with ethidium bromide under a transilluminator (Moon et al., 2011).
Western blot analysis for measuring secretion level of MMP-3 in culture supernatant
The Bradford assay was used to measure protein concentrations in culture supernatants to ensure consistent weight of protein samples subjected to electrophoresis. Culture supernatant samples containing MMP-3 proteins (50 μg each) were subjected to 10% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and then transferred onto a polyvinylidene difluoride (PVDF) membrane. Blots were blocked using 5% skim milk in Tris-buffered saline /Tween 20 (TBS-T) and probed overnight with MMP-3 antibody in blocking buffer at 4°C. Antibody against MMP-3 was purchased from Santa Cruz Biotechnology (Santa Cruz, CA, USA). Membranes were washed with TBS-T and then probed for 1 h with a secondary antibody conjugated with horseradish peroxidase (Calbiochem, La Jolla, CA, USA). After 4 intensive washes with TBS-T, immunoreactive bands were detected using an enhanced chemiluminescence kit (Pierce ECL western blotting substrate, Thermo Scientific, Waltham, MA, USA).
Casein zymography to measure the activity of MMP-3
A modified casein-substrate zymography was carried out using culture supernatants from chondrocytes pretreated for 2 h with luteolin and stimulated for 24 h with IL-1β in DMEM containing 0.5% FBS. The Bradford assay was used to measure protein concentrations in culture media to ensure consistency across samples. Samples were electrophoresed at 4°C in a 10% SDS gel containing 0.1% casein. After the electrophoresis, gels were washed with 10 mM Tris-HCl (pH 8.0) containing 2.5 % Triton X-100. Next, the gels were incubated at 37°C for 48 h in 50 mM Tris-HCl (pH 8.0) containing 1% Triton X-100, 0.2 M NaCl and 5 mM CaCl2. Finally, gels were stained with 1% Coomassie Brilliant Blue, destained, and photographs were taken (Moon et al., 2011).
In vivo experiments
Male Sprague-Dawley rats (Daehan Biolink, Seoul, Korea) weighing 200-210 g were used to investigate the effect of luteolin on production of MMP-3 in articular cartilage in vivo. Animals were housed 5 per cage, and provided with distilled water and food ad libitum, and kept under a 12 h light/dark cycle (lights on from 08:00 to 20:00) at constant temperature (22.5°C) and humidity (55%). Animals were cared through all of the experimental procedures in accordance with the Guide for the Care and Use of Laboratory Animals regulated by Chungnam National University, Daejeon, Korea. Rats were randomly divided into 4 groups as follows: control, IL-1β only, 50 μM luteolin plus IL-1β, or 100 μM luteolin plus IL-1β. Rats were anesthetized with vaporized diethyl ether, and those from the 50 μM luteolin plus IL-1β and 100 μM luteolin plus IL-1β treatment groups received a 30 μL injection of 50 μM or 100 μM luteolin, respectively, into the right knee joint. After 3 h, rats from the IL-1β only group, the 50 μM luteolin plus IL-1β group and the 100 μM luteolin plus IL-1β group received a 30 μL injection of 20 ng IL-1β in sterile PBS into the right knee joint. Rats from the control group were injected with 30 μL of sterile PBS (Hu et al., 2011). Rats were euthanized with CO2 asphyxiation72 h after injections. Articular cartilage (tibial plateau and femoral condyle) was isolated from each animal, homogenized, and prepared for measuring the level of production of MMP-3 protein by western blot analysis. Tissue ly-sates from articular cartilage homogenates containing MMP-3 protein (50 μg each) were subjected to 10% SDS-PAGE and transferred onto a PVDF membrane. Blots were blocked with 5% skim milk in Tris-buffered saline/Tween 20 (TBS-T) and probed with MMP-3 antibody (Santa Cruz Biotechnology, Santa Cruz, CA, USA) in blocking buffer overnight at 4°C. Membranes were washed with TBS-T and probed for 1 h with a secondary antibody conjugated with horseradish peroxidase (Calbiochem, La Jolla, CA, USA). After 4 intensive washes with TBS-T, immunoreactive bands were detected using an enhanced chemiluminescence kit (Pierce ECL western blotting substrate, Thermo Scientific, Waltham, MA, USA).
RESULTS
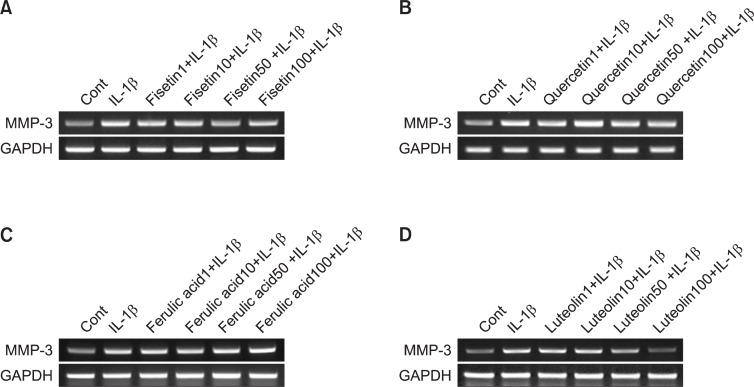
Effect of luteolin, quercetin, fisetin, or ferulic acid on MMP-3 gene expression in rabbit chondrocytes
To compare the potency of activity on MMP-3 gene expression, effect on MMP-3 gene expression was examined by pre-treatment of quercetin, fisetin or ferulic acid - similar flavonoidal and related compounds with luteolin - in addition to luteolin (Fig. 1). As shown in Fig. 2, luteolin inhibited IL-1β-induced MMP-3 gene expression. However, quercetin, fisetin, or ferulic acid did not affect MMP-3 gene expression.
Fig. 1.
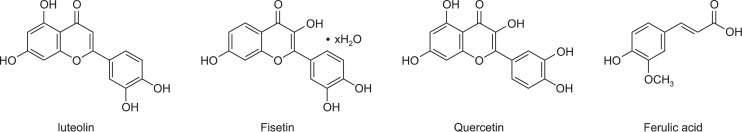
Chemical structure of luteolin and luteolin-related natural products.
Fig. 2.
Effect of luteolin, quercetin, fisetin, or ferulic acid on MMP-3 gene expression in rabbit chondrocytes. Primary cultured rabbit articular chondrocytes were pretreated with varying concentrations (1, 10, 50, and 100 μM) of luteolin, quercetin, fisetin or ferulic acid for 2 h and then stimulated with IL-1β (10 ng/mL) for 24 h. MMP-3 gene expression level was measured by RT-PCR. Three independent experiments were performed and representative data were shown (cont: control, concentration unit is μM).
Effect of luteolin, quercetin, fisetin or ferulic acid on proliferation of rabbit chondrocytes (cytotoxicity assay)
As can be seen in Fig. 3, luteolin, quercetin, fisetin or ferulic acid showed no significant cytotoxicity at the concentrations of 1, 10, 50, and 100 μM. The numbers of cells in luteolin-treated cultures were 100 ± 0%, 97 ± 9%, 98 ± 13%, 105 ± 7%, and 89 ± 14% for control, 1, 10, 50, and 100 μM luteolin, respectively. The numbers of cells in fisetin-treated cultures were 100 ± 13%, 86 ± 19%, 90 ± 16%, 94 ± 17%, and 92 ± 8% for control, 1, 10, 50, and 100 μM fisetin, respectively. The numbers of cells in quercetin-treated cultures were 100 ± 8%, 109 ± 10%, 85 ± 18%, 88 ± 12%, and 103 ± 11% for control, 1, 10, 50, and 100 μM quercetin, respectively. The numbers of cells in ferulic acid-treated cultures were 100 ± 11%, 83 ± 19%, 104 ± 8%, 106 ± 11%, and 85 ± 13% for control, 1, 10, 50, and 100 μM ferulic acid, respectively.
Fig. 3.
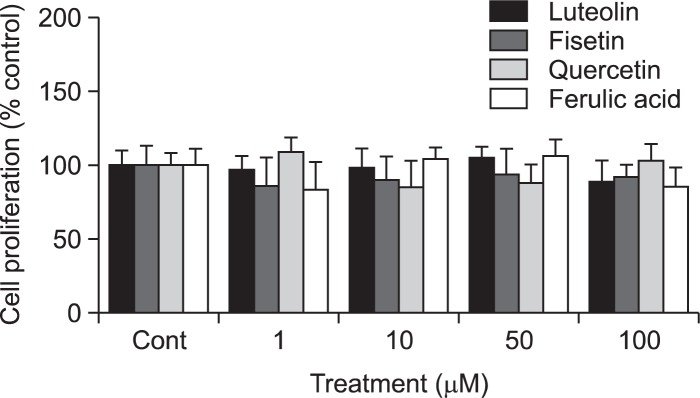
Effect of luteolin, quercetin, fisetin, or ferulic acid on proliferation of rabbit chondrocytes. Chondrocytes were incubated for 72 h in the presence of varying concentrations of luteolin, quercetin, fisetin or ferulic acid. Cell viability was determined using SRB assay as described in Materials and methods. Each bar represents a mean ± S.E.M. of three independent experiments in comparison with that of the control set at 100%.
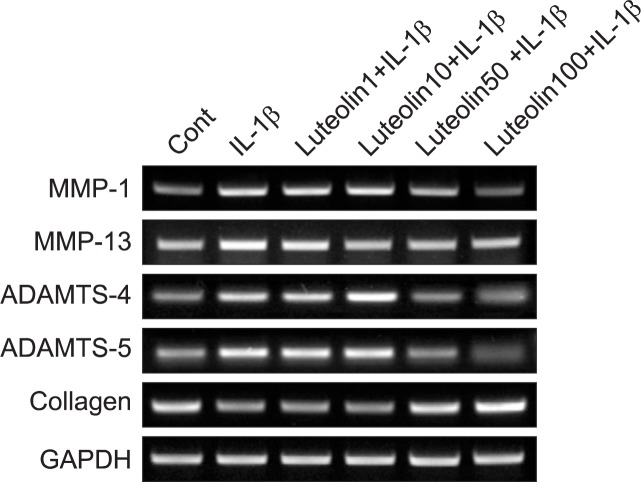
Effect of luteolin on gene expression of MMP-1, MMP-13, ADAMTS-4, ADAMTS-5, or type II collagen in rabbit chondrocytes
As shown in Fig. 4, luteolin also inhibited IL-1β-induced gene expression of MMP-1, MMP-13, ADAMTS-4, or ADAMTS-5, the other degradative enzymes related to the destruction of articular cartilage. Furthermore, luteolin showed the possible chondroprotective effect by abolishing IL-1β-induced deficits in type II collagen gene expression, in rabbit chondrocytes.
Fig. 4.
Effect of luteolin on gene expression of MMP-1, MMP-13, ADAMTS-4, ADAMTS-5, or type II collagen in rabbit chondrocytes. Primary cultured rabbit articular chondrocytes were pretreated with varying concentrations (1, 10, 50, and 100 μM) of luteolin for 2 h and then stimulated with IL-1β (10 ng/mL) for 24 h. The gene expression level of MMP-1, MMP-13, ADAMTS-4, ADAMTS-5 or collagen type II was measured by RT-PCR. Three independent experiments were performed and representative data were shown (cont: control, concentration unit is μM).
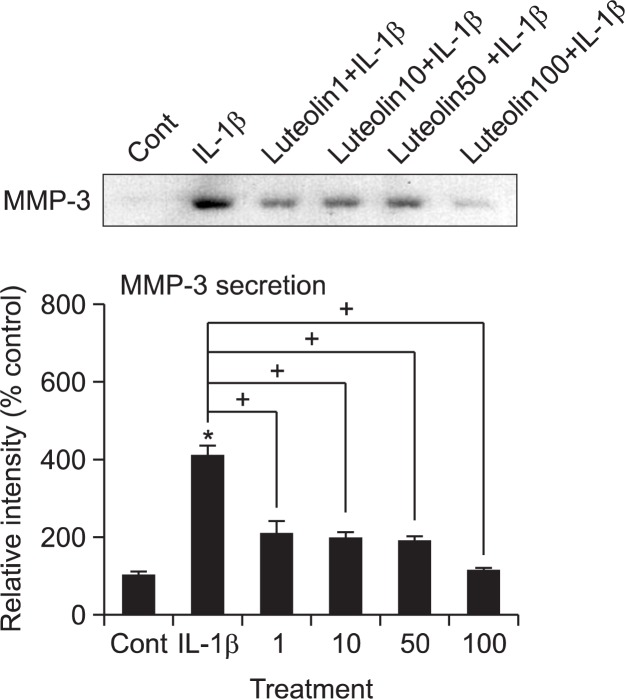
Effect of luteolin on IL-1β-induced secretion of MMP-3 from rabbit articular chondrocytes
If luteolin can affect the MMP-3 gene expression at the transcriptional level, it should be investigated whether luteolin affects IL-1β-induced secretion of MMP-3 proteins from rabbit articular chondrocytes. As can be seen in Fig. 5, stimulation with IL-1β (10 ng/mL) increased secretion level of MMP-3 from chondrocytes. Luteolin inhibited IL-1β-induced secretion of MMP-3. This result means that luteolin can control the steps of protein synthesis and secretion of MMP-3.
Fig. 5.
Effect of luteolin on IL-1β-induced secretion of MMP-3 in rabbit articular chondrocytes. Primary cultured rabbit articular chondrocytes were pretreated with varying concentrations (1, 10, 50, and 100 μM) of luteolin for 2 h and then stimulated with IL-1β (10 ng/mL) for 24 h. Culture supernatants were collected for measurement of the levels of produced and secreted MMP-3 by western blot analysis. Three independent experiments were performed and representative data were shown (cont: control, concentration unit is μM).
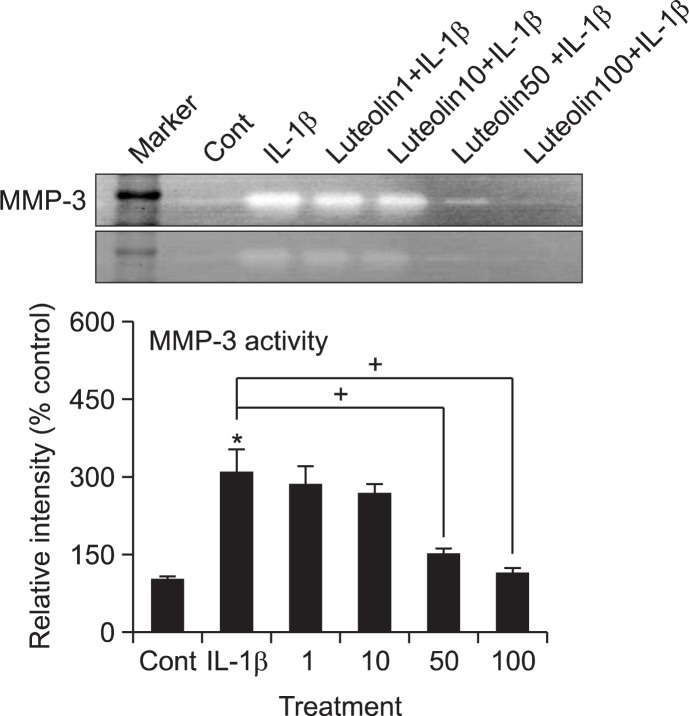
Effect of luteolin on MMP-3 activity in rabbit articular chondrocytes
After treatment with IL-1β for 24 h, culture supernatants from rabbit articular chondrocytes were analyzed for caseinase activity by casein zymography, to investigate the effect of luteolin on the activity of MMP-3, which is known to degrade proteoglycans, one of the two major matrix components of cartilage. As can be seen in Fig. 6, IL-1β increased the activity of MMP-3 in rabbit articular chondrocytes, and this effect was inhibited by pretreatment with luteolin.
Fig. 6.
Effect of luteolin on the enzyme activity of MMP-3 in rabbit articular chondrocytes. Primary cultured rabbit articular chondrocytes were pretreated with varying concentrations (1, 10, 50, and 100 μM) of luteolin for 2 h and then stimulated with IL-1β (10 ng/mL) for 24 h. Culture supernatants were collected for measurement of the enzyme activity of MMP-3 by casein zymography. Three independent experiments were performed and representative data were shown (cont: control, concentration unit is μM).
Effect of luteolin on production of MMP-3 in vivo
To examine whether luteolin shows the potential effect in vivo, we checked the effect of intraarticular injection of luteolin into the knee joint of rats on in vivo IL-1β-stimulated production of MMP-3 from articular cartilage tissues. As can be seen in Fig. 7, stimulation with IL-1β (20 ng/30 μL) increased the level of MMP-3 production from articular cartilage tissues. However, luteolin inhibited IL-1β-induced production level of MMP-3 in vivo, at the highest concentration tested.
Fig. 7.
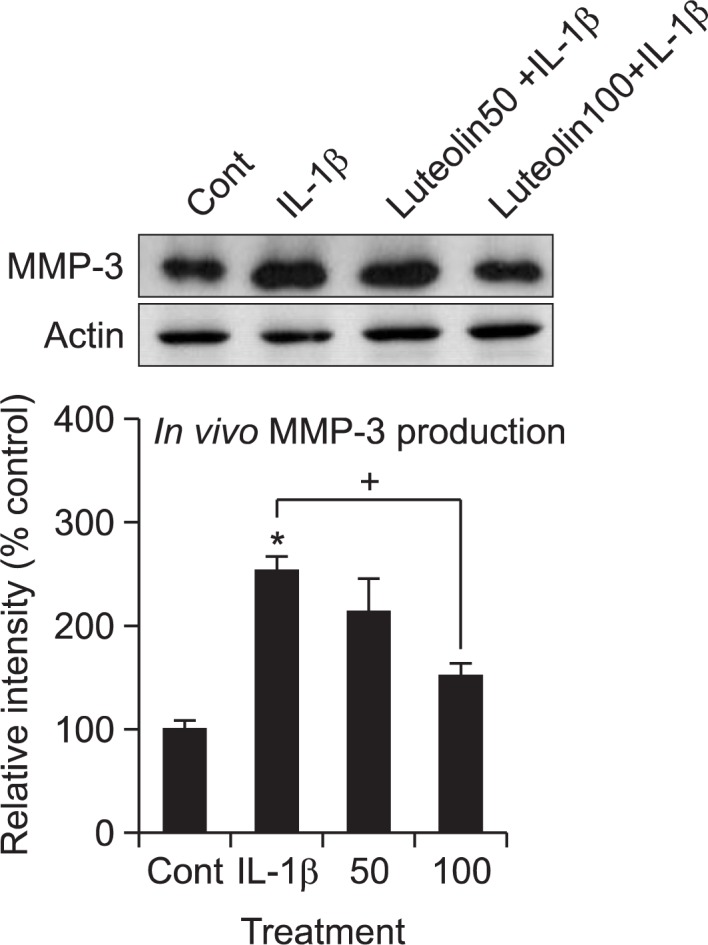
Effect of luteolin on production of MMP-3 in vivo. The knee joint of rats were pretreated with 50 μM or 100 μM of luteolin for 3 h and stimulated with IL-1β (20 ng/30 μL) for 72 h, by intraarticular injection. Tissue lysates from articular cartilage homogenates were collected for measurement of the level of produced MMP-3 in vivo, by western blot analysis. Equal protein loading was evaluated by β-actin levels, and representative data were shown (cont: control, concentration unit is μM).
DISCUSSION
Trial to develop a useful pharmacological tool for regulating the broken equilibrium between synthesis and degradation of articular cartilage during the progression of osteoarthritis can be a promising approach to the effective control of osteoarthritis. As aforementioned in introduction, luteolin, a flavonoidal compound derived from diverse medicinal plants showing anti-inflammatory and anti-oxidative activities, has shown anti-inflammatory, anti-oxidative, anti-carcinogenic and anti-arthritic effects in experimental models of rheumatoid arthritis and infectious arthritis (Manju and Nalini, 2007; Hou et al., 2009; Lee and Kim, 2010; Choi and Lee, 2010; Lee and Han, 2011; Moncada-Pazos et al., 2011; Sun et al., 2012; Jung et al., 2012; Impellizzeri et al., 2013).
However, to the best of our knowledge, there have been no reports on the effects of luteolin on gene expression, secretion, and activity of MMP-3, which is an articular cartilage-degradative enzyme that decomposes proteoglycans, in primary cultured rabbit articular chondrocytes and production of MMP-3 in the rat knee.
Although osteoarthritis can be defined as a non-inflammatory disease in general, its development and progression is attributed to low-grade inflammation in intraarticular site, as well as to various inflammatory cytokines in articular tissues and fluids that are produced by chondrocytes and/or interact with chondrocytes (Bonnet and Walsh, 2005; Kobayashi et al., 2005; Loeser, 2006; Goldring et al., 2008). IL-1β, an inflammatory cytokine produced by the cells in articular tissues including chondrocytes, can increase the gene expression level of MMPs and stimulate the progression of osteoarthritis. IL-1β plays a pivotal role in the initiation and progression of destruction of articular cartilage by inhibiting synthesis of collagen and stimulating MMPs expressions (Aida et al., 2005; Kobayashi et al., 2005; Pantsulaia et al., 2010).
Among multiple MMPs in articluar tissues, MMP-3 has been reported to play an important pathophysiological role in osteo-arthritis, by degrading components of the extracellular matrix, such as proteoglycans. MMP-3 levels were increased more than MMP-1 levels in patients suffering from osteoarthritis in knee joints compared to the control group (Garnero et al., 2000; Lijnen, 2002).
As can be seen in results, we found that luteolin inhibited IL-1β-induced MMP-3 gene expression. However, quercetin, fisetin, or ferulic acid-similar flavonoidal and/or related compounds with luteolin-did not affect MMP-3 gene expression (Fig. 1, 2). This result suggests that luteolin suppresses the gene expression of MMP-3 at the transcriptional level.
In addition to MMP-3, MMP-1 and MMP-13 have been reported to play important roles in the destruction of cartilage in osteoarthritis. MMP-1 is a commonly detected metalloproteinase in synovial fluid from patients suffering from osteoarthritis (Freemont et al., 1997; Goupille et al., 1998; Kanyama et al., 2000; Yoshihara et al., 2000; Neuhold et al., 2001; Jo et al., 2003; Little et al., 2009). Another degradative enzyme, ADAMTS-4, was reported to be a major aggrecanase in cartilage of mouse and ADAMTS-5 was known to be important in cartilage matrix destruction during osteoarthritis (Stanton et al., 2005; Echtermeyer et al., 2009).
Therefore, we examined the effect of luteolin on gene expression of MMP-1, MMP-13, ADAMTS-4, or ADAMTS-5. As can be seen in Fig. 4, luteolin inhibited IL-1β-induced gene expression of MMP-1, MMP-13, ADAMTS-4 or ADAMTS-5. At the same time, luteolin restored the gene expression of type II collagen that had been inhibited by IL-1β, in rabbit chondrocytes. Thus, the chondroprotective effect of luteolin are supported by its regulation of the gene expression of diverse proteases involved in the destruction of articular cartilage in osteoarthritis, as well as by its promotion of the expression of type II collagen at the transcriptional level.
Next, if luteolin can affect the MMP-3 gene expression at the transcriptional level, it should be investigated whether luteolin affects IL-1β-induced secretion of MMP-3 protein from rabbit articular chondrocytes. As can be seen in Fig. 5, stimulation with IL-1β increased the secretion level of MMP-3 from chondrocytes. Luteolin inhibited IL-1β-induced secretion level of MMP-3. This result shows that luteolin can control the steps of protein synthesis and secretion of MMP-3.
To investigate the regulatory effect of luteolin on the enzyme activity of MMP-3 secreted, culture supernatants from rabbit articular chondrocytes stimulated with IL-1β for 24 h were analyzed for caseinase activity by casein zymography. As shown in Fig. 6, when rabbit articular chondrocytes were stimulated with IL-1β, the enzyme activity of MMP-3 was increased. This effect was inhibited by pretreatment with luteolin. This result suggests that luteolin can suppress the proteolytic activity of MMP-3, in osteoarthritic articular cartilage tissues.
Finally, we examined the effect of intraarticular injection of luteolin into the knee joint of rats on in vivo IL-1β-stimulated production of MMP-3 in articular cartilage tissue. As shown in Fig. 7, luteolin inhibited IL-1β-stimulated production level of MMP-3 in articular cartilage tissue. This result shows that, in addition to its in vitro effects, luteolin exerts chondroprotective effects in vivo when administered via intraarticular injection.
Taken together, luteolin showed the chondroprotective effect by regulating the gene expression, secretion and activity of MMP-3, directly acting on articular chondrocytes. It can be developed as a novel agent for controlling cartilage damage in osteoarthritis via intraarticular administration, through future studies.
REFERENCES
- Aida Y, Maeno M, Suzuki N, Shiratsuchi H, Motohashi M, Matsumura H. The effect of IL-1beta on the expression of matrix metalloproteinases and tissue inhibitors of matrix metalloproteinases in human chondrocytes. Life Sci. 2005;77:3210–3221. doi: 10.1016/j.lfs.2005.05.052. [DOI] [PubMed] [Google Scholar]
- Aigner T, McKenna L. Molecular pathology and pathobiology of osteoarthritic cartilage. Cell Mol Life Sci. 2002;59:5–18. doi: 10.1007/s00018-002-8400-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birkedal-Hansen H, Moore WG, Bodden MK, Windsor LJ, Birkedal-Hansen B, DeCarlo A, Engler JA. Matrix metalloproteinases: a review. Crit Rev Oral Biol Med. 1993;4:197–250. doi: 10.1177/10454411930040020401. [DOI] [PubMed] [Google Scholar]
- Blom AB, van Lent PL, Libregts S, Holthuysen AE, van der Kraan PM, van Rooijen N, van den Berg WB. Crucial role of macrophages in matrix metalloproteinase-mediated cartilage destruction during experimental osteoarthritis: involvement of matrix metalloproteinase-3. Arthritis Rheum. 2007;56:147–157. doi: 10.1002/art.22337. [DOI] [PubMed] [Google Scholar]
- Bonnet CS, Walsh DA. Osteoarthritis, angiogenesis and inflammation. Rheumatology (Oxford) 2005;44:7–16. doi: 10.1093/rheumatology/keh344. [DOI] [PubMed] [Google Scholar]
- Burrage PS, Mix KS, Brinckerhoff CE. Matrix metal-loproteinases: role in arthritis. Front Biosci. 2006;11:529–543. doi: 10.2741/1817. [DOI] [PubMed] [Google Scholar]
- Choi EM, Lee YS. Luteolin suppresses IL-1beta-induced cytokines and MMPs production via p38 MAPK, JNK, NF-kappaB and AP-1 activation in human synovial sarcoma cell line, SW982. Food Chem Toxicol. 2010;48:2607–2611. doi: 10.1016/j.fct.2010.06.029. [DOI] [PubMed] [Google Scholar]
- Dean DD, Martel-Pelletier J, Pelletier JP, Howell DS, Woessner JF., Jr Evidence for metalloproteinase and metalloproteinase inhibitor imbalance in human osteoarthritic cartilage. J Clin Invest. 1989;84:678–685. doi: 10.1172/JCI114215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Echtermeyer F, Bertrand J, Dreier R, Meinecke I, Neugebauer K, Fuerst M, Lee YJ, Song YW, Herzog C, Theilmeier G, Pap T. Syndecan-4 regulates ADAMTS-5 activation and cartilage breakdown in osteoarthritis. Nat Med. 2009;15:1072–1076. doi: 10.1038/nm.1998. [DOI] [PubMed] [Google Scholar]
- Freemont AJ, Hampson V, Tilman R, Goupille P, Taiwo Y, Hoyland JA. Gene expression of matrix metalloproteinases 1, 3, and 9 by chondrocytes in osteoarthritic human knee articular cartilage is zone and grade specific. Ann Rheum Dis. 1997;56:542–549. doi: 10.1136/ard.56.9.542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garnero P, Rousseau JC, Delmas PD. Molecular basis and clinical use of biochemical markers of bone, cartilage, and synovium in joint diseases. Arthritis Rheum. 2000;43:953–968. doi: 10.1002/1529-0131(200005)43:5<953::AID-ANR1>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- Goldring MB, Otero M, Tsuchimochi K, Ijiri K, Li Y. Defining the roles of inflammatory and anabolic cytokines in cartilage metabolism. Ann. Rheum. Dis. 2008;67(Suppl 3):iii75–iii82. doi: 10.1136/ard.2008.098764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goupille P, Jayson MI, Valat JP, Freemont AJ. Matrix metalloproteinases: the clue to intervertebral disc degeneration. Spine (Phila Pa 1976) 1998;23:1612–1626. doi: 10.1097/00007632-199807150-00021. [DOI] [PubMed] [Google Scholar]
- Hou Y, Wu J, Huang Q, Guo L. Luteolin inhibits proliferation and affects the function of stimulated rat synovial fibroblasts. Cell Biol Int. 2009;33:135–147. doi: 10.1016/j.cellbi.2008.10.005. [DOI] [PubMed] [Google Scholar]
- Hu PF, Chen WP, Tang JL, Bao JP, Wu LD. Protective effects of berberine in an experimental rat osteoarthritis model. Phytother Res. 2011;25:878–885. doi: 10.1002/ptr.3359. [DOI] [PubMed] [Google Scholar]
- Impellizzeri D, Esposito E, Paola R, Di, Ahmad A, Campolo M, Pel i A, Morittu VM, Britti D, Cuzzocrea S. Palmitoylethanolamide and luteolin ameliorate development of arthritis caused by injection of collagen type II in mice. Arthritis ResTher. 2013;15:R192. doi: 10.1186/ar4382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jo H, Park JS, Kim EM, Jung MY, Lee SH, Seong SC, Park SC, Kim HJ, Lee MC. The in vitro effects of dehydroepiandrosterone on human osteoarthritic chondrocytes. Osteoarthritis Cartilage. 2003;11:585–594. doi: 10.1016/s1063-4584(03)00094-3. [DOI] [PubMed] [Google Scholar]
- Jung HA, Jin SE, Min BS, Kim BW, Choi JS. Anti-inflammatory activity of Korean thistle Cirsium maackii and its major flavonoid, luteolin 5-O-glucoside. Food Chem Toxicol. 2012;50:2171–2179. doi: 10.1016/j.fct.2012.04.011. [DOI] [PubMed] [Google Scholar]
- Kanyama M, Kuboki T, Kojima S, Fujisawa T, Hattori T, Takigawa M, Yamashita A. Matrix metalloproteinases and tissue inhibitors of metalloproteinases in synovial fluids of patients with temporomandibular joint osteoarthritis. J. Orofac. Pain. 2000;14:20–30. [PubMed] [Google Scholar]
- Kobayashi M, Squires GR, Mousa A, Tanzer M, Zukor DJ, Antoniou J, Feige U, Poole AR. Role of interleukin-1 and tumor necrosis factor alpha in matrix degradation of human osteoarthritic cartilage. Arthritis Rheum. 2005;52:128–135. doi: 10.1002/art.20776. [DOI] [PubMed] [Google Scholar]
- Kullich W, Fagerer N, Schwann H. Effect of the NSAID nimesulide on the radical scavenger glutathione S-transferase in patients with osteoarthritis of the knee. Curr Med Res Opin. 2007;23:1981–1986. doi: 10.1185/030079907X223486. [DOI] [PubMed] [Google Scholar]
- Lee JH, Han Y. Antiarthritic effect of lonicerin on Candida albicans arthritis in mice. Arch Pharm Res. 2011;34:853–859. doi: 10.1007/s12272-011-0520-6. [DOI] [PubMed] [Google Scholar]
- Lee JH, Kim GH. Evaluation of antioxidant and inhibitory activities for different subclasses flavonoids on enzymes for rheumatoid arthritis. J Food Sci. 2010;75:H212–H217. doi: 10.1111/j.1750-3841.2010.01755.x. [DOI] [PubMed] [Google Scholar]
- Lijnen HR. Matrix metalloproteinases and cellular fibrinolytic activity. Biochemistry (Mosc) 2002;67:92–98. doi: 10.1023/a:1013908332232. [DOI] [PubMed] [Google Scholar]
- Lin PM, Chen CT, Torzilli PA. Increased stromelysin-1 (MMP-3), proteoglycan degradation (3B3- and 7D4) and collagen damage in cyclically load-injured articular cartilage. Osteoarthritis Cartilage. 2004;12:485–496. doi: 10.1016/j.joca.2004.02.012. [DOI] [PubMed] [Google Scholar]
- Little CB, Barai A, Burkhardt D, Smith SM, Fosang AJ, Werb Z, Shah M, Thompson EW. Matrix metalloproteinase 13-deficient mice are resistant to osteoarthritic cartilage erosion but not chondrocyte hypertrophy or osteophyte development. Arthritis Rheum. 2009;60:3723–3733. doi: 10.1002/art.25002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeser RF. Molecular mechanisms of cartilage destruction: mechanics, inflammatory mediators and aging collide. Arthritis Rheum. 2006;54:1357–1360. doi: 10.1002/art.21813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manju V, Nalini N. Protective role of luteolin in 1,2-dimethylhydrazine induced experimental colon carcinogenesis. Cell Biochem Funct. 2007;25:189–194. doi: 10.1002/cbf.1305. [DOI] [PubMed] [Google Scholar]
- Mankin HJ. The response for articular cartilage to mechanical injury. J Bone Joint Surg Am. 1982;64:460–466. [PubMed] [Google Scholar]
- Moncada-Pazos A, Obaya AJ, Viloria CG, López-Otín C, Cal S. The nutraceutical flavonoid luteolin inhibits ADAMTS-4 and ADAMTS-5 aggrecanase activities. J Mol Med (Berl) 2011;89:611–619. doi: 10.1007/s00109-011-0741-7. [DOI] [PubMed] [Google Scholar]
- Moon PD, Jeong HS, Chun CS, Kim HM. Baekjeolyusin-tang and its active component berberine block the release of collagen and proteoglycan from IL-1β-stimulated rabbit cartilage and down-regulate matrix metalloproteinases in rabbit chondrocytes. Phytother Res. 2011;25:844–850. doi: 10.1002/ptr.3353. [DOI] [PubMed] [Google Scholar]
- Neuhold LA, Killar L, Zhao W, Sung ML, Warner L, Kulik J, Turner J, Wu W, Billinghurst C, Meijers T, Poole AR, Babij P, DeGennaro LJ. Postnatal expression in hyaline cartilage of constitutively active human collagenase-3 (MMP-13) induces osteoarthritis in mice. J Clin Invest. 2001;107:35–44. doi: 10.1172/JCI10564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okada Y, Shinmei M, Tanaka O, Naka K, Kimura A, Nakanishi I, Bayliss MT, Iwata K, Nagase H. Localization of matrix metalloproteinase 3 (stromelysin) in osteoarthritic cartilage and synovium. Lab Invest. 1992;66:680–690. [PubMed] [Google Scholar]
- Pantsulaia I, Kalichman L, Kobyliansky E. Association between radiographic hand osteoarthritis and RANKL, OPG and inflammatory markers. Osteoarthritis Cartilage. 2010;18:1448–1453. doi: 10.1016/j.joca.2010.06.009. [DOI] [PubMed] [Google Scholar]
- Shibakawa A, Aoki H, Masuko-Hongo K, Kato T, Tanaka M, Nishioka K, Nakamura H. Presence of pannus-like tissue on osteoarthritic cartilage and its histological character. Osteo-arthritis Cartilage. 2003;11:133–140. doi: 10.1053/joca.2002.0871. [DOI] [PubMed] [Google Scholar]
- Skehan P, Storeng R, Scudiero D, Monks A, McMahon J, Vistica D, Warren JT, Bokesch H, Kenney S, Boyd MR. New colorimetric cytotoxicity assay for anticancer-drug screening. J Natl Cancer Inst. 1990;82:1107–1112. doi: 10.1093/jnci/82.13.1107. [DOI] [PubMed] [Google Scholar]
- Stanton H, Rogerson FM, East CJ, Golub SB, Lawlor KE, Meeker CT, Little CB, Last K, Farmer PJ, Campbell IK, Fourie AM, Fosang AJ. ADAMTS-5 is the major aggrecanase in mouse cartilage in vivo and in vitro. Nature. 2005;434:648–652. doi: 10.1038/nature03417. [DOI] [PubMed] [Google Scholar]
- Sun GB, Sun X, Wang M, Ye JX, Si JY, Xu HB, Meng XB, Qin M, Sun J, Wang HW, Sun XB. Oxidative stress suppression by luteolin-induced heme oxygenase-1 expression. Toxicol Appl Pharmacol. 2012;265:229–240. doi: 10.1016/j.taap.2012.10.002. [DOI] [PubMed] [Google Scholar]
- Yoshihara Y, Nakamura H, bata K, Yamada H, Hayakawa T, Fujikawa K, Okada Y. Matrix metalloproteinases and tissue inhibitors of metalloproteinases in synovial fluids from patients with rheumatoid arthritis or osteoarthritis. Ann Rheum Dis. 2000;59:455–461. doi: 10.1136/ard.59.6.455. [DOI] [PMC free article] [PubMed] [Google Scholar]