ABSTRACT
Background:
Fatigue has been shown to affect performance of hop tests in patients after anterior cruciate ligament reconstruction (ACLR) compared to uninjured controls (CTRL). This may render the hop test less sensitive in detecting landing errors. The primary purpose of this study was to investigate the effect of lower extremity fatigue on landing performance assessed with the Landing Error Scoring System (LESS) in patients after ACLR compared to a CTRL group. It is plausible that fatigue would have an effect on confidence and risk appraisal in the ACLR group. The secondary purpose was to determine the relationship between psychological responses and LESS scores after fatigue.
Methods:
Twelve patients following ACLR (6 males, 6 females) who were tested at 10 ± 2.4 months after surgery participated in the current study and were compared to 10 subjects in the control group (5 males, 5 females). Subjects performed a jump‐landing task and the landing was assessed using the Landing Error Scoring System (LESS) both before and after fatigue. Digital video camcorders recorded frontal and sagittal plane views of the subject performing the task. The LESS was scored using video replay. Psychological responses in the ACLR group were assessed with the ACL‐RSI questionnaire.
Results:
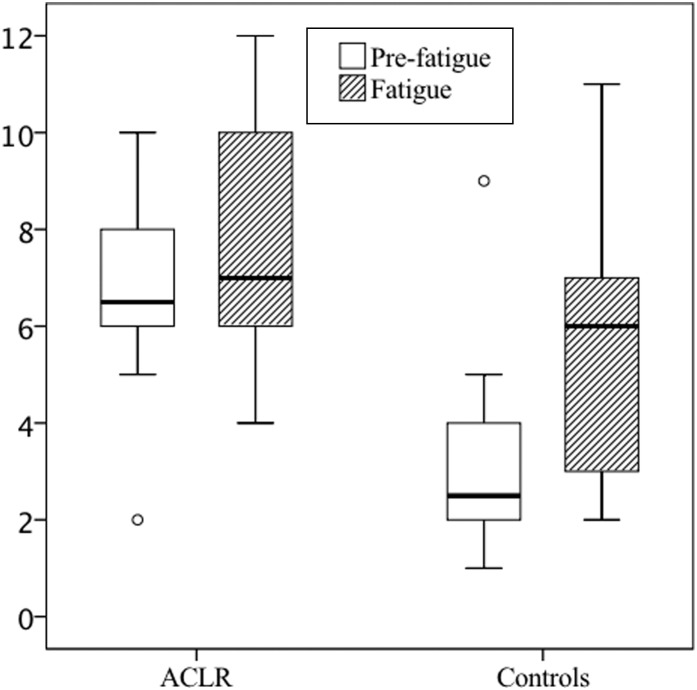
Patients after ACLR had a median LESS of 6.5 which reflects a poor result (LESS >6) in the pre‐fatigue condition compared to controls who had a LESS of 2.5 which is considered excellent (≤4). In the post‐fatigue condition, median LESS in patients after ACLR increased to 7.0 whereas in the control group the LESS increased to 6.0 both of which reflect a poor result. The median increase in LESS was larger in the control (2.0) group compared to patients after ACLR (1.0) but the difference was not significant (p=0.165).
Conclusions:
Patients after ACLR have higher LESS scores at baseline compared to a control group. Fatigue resulted in an increase in scores on the LESS in both groups.
Level of Evidence:
3b
Keywords: Anterior cruciate ligament, jump landing, fatigue, jump landing, psychology, return to sport
INTRODUCTION
Return to sport (RTS) after ACL reconstruction (ACLR) is a frequent subject of debate and patients are usually allowed to return to regular athletic participation approximately six months post‐surgery.1,2 The release to full activity is a potential sensitive landmark for the athlete who wants to return to high‐level sport participation. Unfortunately, many questions exist and there is a lack of consensus regarding the appropriate criteria for releasing patients to unrestricted sports activities postoperatively.3
Recently, Sward et al suggested that return to a high activity level after an unilateral ACLR was the most important risk factor for sustaining a contralateral ACL injury.4 Injury rates for a second injury exceed 20% for young highly active athletes returning to sports within the first year after surgery.5 Data from the Swedish National Anterior Cruciate Ligament Register indicate that 22% of the 15‐ to 18‐year‐old female soccer players underwent a revision or contralateral ACLR during a 5‐year period.6 Risk factors acquired secondary to the ACL injury, such as altered neuromuscular function, that affect both the injured and the contralateral leg, most likely further increase the risk of a contralateral ACL injury.4,5
It is common practice to use hop tests in late phase of rehabilitation to ensure safe RTS.7,8 However, hop tests may not be sensitive enough to detect biomechanical deficits, and, typically, kinematics and kinetics are not measured in the clinical setting. As biomechanical changes play an important role in risk for secondary injury, there is a need to develop objective, performance‐based assessments designed to identify potential lower extremity biomechanical deficits in the late stage of rehabilitation following ACLR prior to release of the athlete to the high demands of sports. Identification of altered movement patterns post‐ACLR may be critical to maximize functional recovery following surgery and reduce risk for a second ACL injury. Based on kinematic and kinetic measurements from jump‐landing movement strategies, Padua et al9 developed the Landing Error Scoring System (LESS). The LESS has been shown to possess good criterion validity and reliability as a field‐based assessment tool used to identify individuals who exhibit faulty jump‐landing biomechanics or high‐risk movement patterns during jump‐landing. It has commonly been assumed that athletes participating in higher levels of competition are more physically fit and have better movement patterns, and that more novice (lower levels of participation) athletes are less fit and poorer movers. Supporting this assumption are data showing that high school athletes demonstrated significantly poorer LESS scores (e.g., higher‐risk movement patterns) when compared with college student‐athletes.10 More recently, higher level athletes have been shown to have better physical fitness as measured by the Army Physical Fitness Test but as a group did not exhibit better landing technique.11 The implications of this research suggest that “high‐risk” movement patterns are prevalent in all levels of athletes. A recent longitudinal study demonstrated that ACL injury and ACLR altered lower extremity biomechanics, demonstrated by increases in frontal plane movement (increased hip adduction and knee valgus). The injured leg of patients after ACLR also exhibited decreased sagittal plane loading (decreased anterior tibial shear force, knee extension moment and hip flexion moment).12 The LESS has not been used in a group of patients after ACLR.
Of all the risk factors associated with ACL injury, neuromuscular control is altered further when the effects of fatigue are combined with unanticipated movements are present.13 A recently published systematic review that investigated effects of fatigue on landing kinematics in a healthy, uninjured population found that neuromuscular fatigue causes various biomechanical alterations that may increase the risk of a noncontact ACL injury during landing.14 Fatigue has been found to increase peak proximal tibial anterior shear force,15 increase peak knee valgus angle,13,16 decrease knee flexion angle,15 decrease hip flexion angle,13 and increase knee internal rotation17 during various tasks. The effect of fatigue has also been studied in patients after ACLR, indicating that 68% of the patients after ACLR showed abnormal hop limb symmetry index (LSI) when tested in a fatigued condition.18
The primary purpose of this study was to investigate the effect of lower extremity fatigue on landing performance assessed with the Landing Error Scoring System (LESS) in patients after ACLR compared to a CTRL group. The authors’ hypothesis was that patients after ACLR would demonstrate a higher LESS score than those in the CTRL group. In addition, the authors expected that fatigue would result in higher LESS scores in the ACLR group compared to CTRL group.
Besides the relationship between physical impairments and RTS, evidence is emerging that psychological responses are strong predictors associated with RTS rate following athletic injury.19,20 The ACL‐Return to Sport after Injury (ACL‐RSI) scale has been shown to be a valid tool to predict athletes’ emotions, confidence and risk appraisal when returning to sport after ACLR.21 As was reported in a systematic review, ground reaction forces and hip and knee flexion moments were reduced when fatigued,14 which may contribute to an adaptive strategy to ensure a safe landing.22 Therefore, it seems plausible that confidence and risk appraisal in the ACLR group would have an effect on the ACL‐RSI when performing a jump‐landing task during fatigue and the change in LESS as determined by non‐fatigue condition and the fatigue condition. Thus, the secondary purpose of this study was to determine the relationship between ACL‐RSI and LESS scores after fatigue. It was hypothesized that a correlation exists between the ACL‐RSI and LESS scores after fatigue.
METHODS
Participants
Twelve patients following ACLR (6 males, 6 females) who were tested at 10 ± 2.4 months after surgery participated in the current pilot study. Patients were operated by one of two experienced orthopaedic surgeons from the same hospital. Briefly, a transtibial technique was used and in all cases a hamstring tendon graft was used. All patients completed their rehabilitation at the same rehabilitation center and were cleared to return to sports by the orthopaedic surgeons and physical therapists. In addition 10 active healthy subjects (5 males, 5 females) recruited from the local university served as the CTRL group. These CTRL subjects had no history of previous knee injury or surgery and had no other injuries in the six months prior to participating in the study. The characteristics of both groups are presented Table 1. Sample size estimations were performed a priori using the Statistical Solutions toolkit (http://www.statisticalsolutions.net/pss_calc.php). Means and standard deviations from previous reported data were entered for the LESS.9 Clinically meaningful differences of two normalized units of LESS were used. Based on statistical power to detect clinically meaningful differences, eight subjects were needed per group to compare functional differences between the experimental conditions. The Institutional Review Board approved the study and prior to participating in this study, all subjects read and signed an informed consent form.
Table 1.
Characteristics of patients after ACL reconstruction (ACLR) and healthy controls (CTRL)
| ACLR (n=12) | CTRL (n=10) | |
|---|---|---|
| Gender (male/female) | 6/6 | 5/5 |
| Age (years) | 27.4 ± 9.6 | 21.0 ± 0.8 |
| Time post surgery (months) | 10.0 ± 2.4 | NA |
| Height (centimeters) | 177.7 ± 7.4 | 179.1 ± 9.4 |
| Weight (KG) | 77.3 ± 12.5 | 72.6 ± 8.7 |
All descriptive data are reported as mean +/− standard deviation.
Procedure
After informed consent was obtained the subject then changed into athletic clothing. One investigator placed 14 mm reflective markers on the following anatomical landmarks of both legs: 1) greater trochanter, 2) lateral epicondyle and 3) tibial tuberosity to enhance video analysis for the LESS. Prior to the start of the experiment, each subject performed a standard sub‐maximal 15‐minute warm‐up consisting of running, agility drills and stretching of the quadriceps, hamstrings and calf muscles. The same investigator instructed subjects in performing the LESS and demonstrated its performance. Each subject was allowed to practice the jump‐landing task sub‐maximally 3 times prior to data collection.
Double‐Legged Drop Jump (LESS)
The double legged jump‐landing task incorporated vertical and horizontal movements as subjects jumped from a 30‐centimeter high box to a distance of 50% of subjects’ body‐height away from the box, down to the ground, and immediately rebounded for a maximum vertical jump.9 During task instruction, emphasis was placed on subjects jumping as high as they could once they landed from the box. Subjects were not provided any feedback or coaching on their landing technique. A successful jump was characterized by 1) jumping off of both feet from the box; 2) jumping forward, but not vertically, 3) immediately jumping vertically after landing and 4) completing the task in a fluid motion.
Two standard 60 HZ video cameras (Sony; DSR‐hc62, Tokyo, Japan) captured frontal plane and sagittal plane view as each subject performed the jump landing procedures. Each jump was videotaped and scored at a later date using the pause and rewind functions. The LESS is a count 17 items of landing technique “errors” on a range of readily observable items. A higher LESS (>6) indicates poor technique in landing from the jump; a lower LESS (≤4) indicates better jump‐landing technique.9 The authors used the following criteria for evaluating individual LESS items according to DiStefano et al where subjects were scored with an “error” if the subject demonstrated the specific landing characteristic error during two or more of the three trials; otherwise, that individual item was coded as “no error.”23
The LESS of the involved leg of individuals in the ACLR group was compared to the non‐dominant leg of individuals in the CTRL group which has been shown to be able to accurately detect differences between groups.24 Leg dominance was defined as the leg with which the subject would kick a ball.
Fatigue Protocol
The LESS was used to assess landing movement patterns under two conditions: pre‐fatigue and post‐fatigue. The pre‐fatigue protocol consisted of the above‐mentioned test, and was considered a non‐fatigue baseline. After the baseline condition the fatigue protocol was executed. Subjects first performed a maximum counter movement jump (CMJ), which was marked for jump height. For this study fatigue was operationally defined as the point where jump height fell below 70% of the maximum jump height of that person which is similar to protocols used in previous studies.13,22 The fatigue protocol consisted of ten double‐legged squats until 90 degrees of knee flexion followed by two repetitions of the CMJ. This scheme was conducted until subjects were no longer able to reach 70% of their maximum CMJ height for 2 consecutive trials (the operational definition of fatigue).
The subjects were asked to give a rating of perceived exertion (RPE) for the local fatigue in the lower extremities. The RPE is a subjective scale of ranging from 6 to 20, where 6 means “no exertion at all” and 20 means “maximal exertion”. The RPE scale is commonly used to gauge activity intensity, and is designed to estimate a subject's heart rate based on how the subject feels.25 To ensure that fatigue was indeed present during the post‐fatigue assessment, the authors’ ensured this post‐fatigue assessment started within 30 seconds after the fatigue protocol. After the patients in the ACLR group finished the LESS, they filled out the ACL‐RSI questionnaire.26 The ACL‐RSI is a 12‐item scale designed to measure psychological factors associated with RTS following ACLR. The scale items are created around three specific psychological responses related to sport resumption; emotions, confidence, and risk appraisal.26
Statistical analysis
All data were analyzed using SPSS (version 18.0 for Windows, SPSS Inc., Chicago, Illinois), with an a priori alpha level of p<0.05. Due to the limited sample size and skewed distribution of the data, the authors choose to apply non‐parametric analyses. Changes in LESS between pre‐fatigue and post‐fatigue conditions for all participants were analyzed using the Wilcoxon signed ranks test. Differences in changes in LESS between ACLR and CTRL were analyzed using a Mann‐Whitney U test. The non‐parametric correlation of the association between ACL‐RSI score of the ACLR group and the change in LESS due to fatigue was explored.
RESULTS
The mean RPE during the fatigue protocol was 18.7 ± 1.4 in ACLR and 18.7 ± 1.0 in CTRL group. Two of the 12 patients after ACLR only performed the LESS in the pre‐fatigued condition. They declined to repeat the LESS after the fatigue protocol due to a lack of confidence in the stability of the knee. Subsequently, the analysis was performed on the remaining 10 patients. The results of the LESS in the two experimental conditions are presented in Table 2.
Table 2.
Median and Inter Quartile Range (IQR 25th, 75th Percentiles) of the Landing Error Scoring System (LESS) Scores before (Pre‐fatigue) and after the fatigue protocol (Fatigue) in patients after ACL reconstruction (ACLR) and healthy controls (CTRL)
| ACLR | CTRL | |||
|---|---|---|---|---|
| Median | IQR | Median | IQR | |
| Pre‐fatigue | 6.5 | (5.5, 7.5) | 2.5 | (2.0, 4.0) |
| Fatigue | 7.0 | (6.0, 10.0) | 6.0 | (3.0, 7.0) |
| Changea | 1.0 | (0.0, 2.0) | 2.0 | (1.0, 3.0) |
IQR=Inter Quartile Range
The median change of the LESS between pre‐fatigue and fatigue conditions was not statistically significant different between the groups (p=0.165).
The LESS score increased significantly after fatigue conditions (Wilcoxon signed rank test p=0.001). The median (interquartile range) LESS scores for all participants increased from 5.0 (2.0; 7.0) for pre–fatigue condition to 7.0 (4.3; 7.8) for post‐fatigue condition (p=0.001). The median increase in LESS was larger in the CTRL (2.0) group compared to patients after ACLR (1.0) but the difference was not significant (Mann‐Whitney U test, p=0.165, Table 2). Box plots are presented of the LESS scores in pre‐fatigue and fatigue conditions for both groups. (Figure 1)
Figure 1.
Box plot of the Landing Error Scoring System (LESS) scores (median) for patients after ACLR and the healthy CTRL group. The box signifies the upper and lower quartiles, and the median is represented by a short black line within the box.
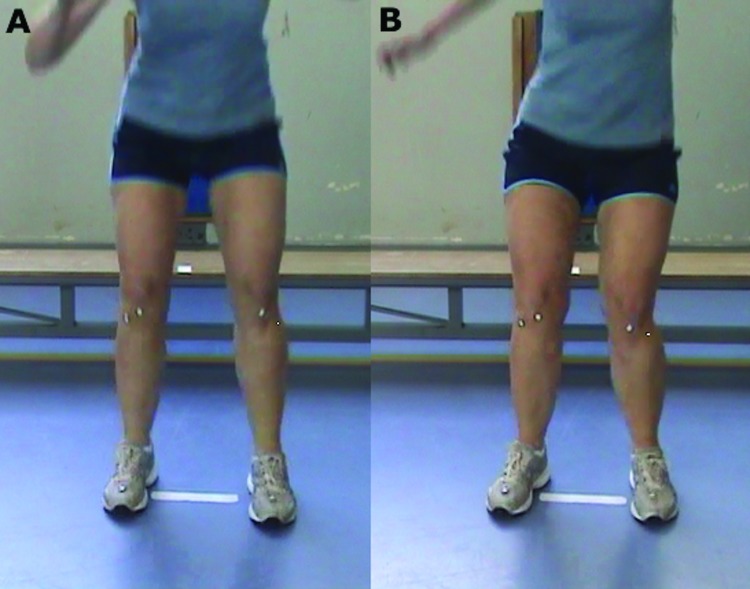
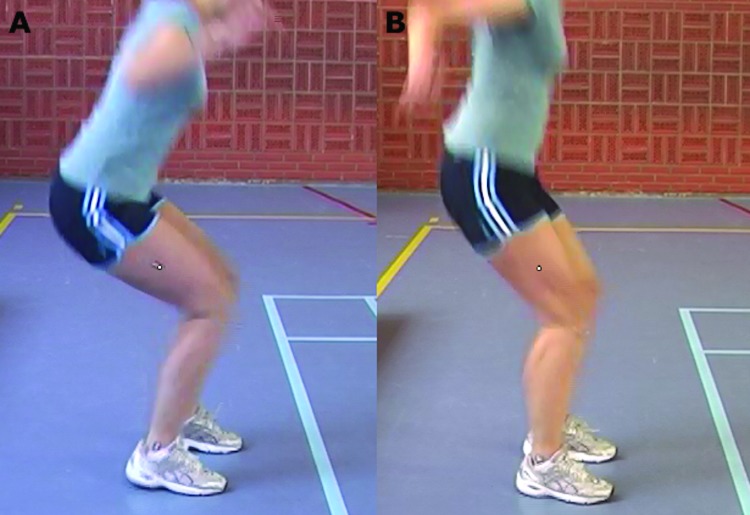
The frequency of errors was counted as the number of patients that had a specific error divided by the total group multiplied by 100. In the post‐fatigue condition, the most noticeable landing errors were knee flexion at initial contact (ACLR 90%, CTRL 30%), extension on the hips (ACLR 60%, CTRL 20%), knee valgus at initial contact (ACLR 70%, CTRL 90%), lateral trunk flexion (50% ACLR, CTRL 0%), asymmetrical foot contact (ACLR 60%, CTRL 10%), maximal knee valgus (ACLR 90%, CTRL 100%). A representative landing style of a patient after ACLR showing the difference between pre‐fatigued and post‐fatigued state is depicted in Figures 2 and 3. The mean ACL‐RSI of the ACLR group was 49.68 ± 3.62 and there was no relationship (r=0.1, p=0.777) between the ACL‐RSI and the change in LESS as determined between the non‐fatigue and the fatigue conditions.
Figure 2.
Example of a representative patient after ACLR during the double‐legged drop jump analyzed in the frontal view, A) pre‐fatigued and B) post‐fatigued states. An asymmetrical loading pattern in the post‐fatigued state is observed with lateral trunk lean and increased valgus of the left knee. Of particular interest is the fact that the right leg is the ACLR leg, indicating that the patient was unloading her involved leg after fatigue, potentially putting her uninvolved leg at greater risk of sustaining an injury.
Figure 3.
Example of a representative patient after ACLR during the double‐legged drop jump analyzed in the sagittal view, A) pre‐fatigued and B) post‐fatigued states. A change in loading pattern is observed during the post‐fatigued state demonstrated by decreased trunk, hip, and knee flexion.
DISCUSSION
The most important findings of this study were that the LESS was higher in patients at a mean 10 ± 2.4 months after ACLR at baseline as well as after fatigue compared to CTRL. All patients after ACLR had a high LESS (>6) indicating poor landing technique. In the current study, a series of CMJ were used to induce a generalized fatigue in subjects. These activities were selected to also induce a localized fatigue of the quadriceps, with the assumption that an amount of localized quadriceps fatigue in addition to general fatigue may result in biomechanical changes at the knee during landing.22 It seems that this series of activities was successful in inducing changing landing mechanics as assessed with the LESS. Overall, the results from the current study showed that fatigue induced changes in landing the ACLR group. However, increased LESS were also noted in the CTRL after fatigue. In fact, the changes in the LESS were more pronounced in the CTRL compared to the ACLR group. This may be attributed to the difference in pre‐fatigue LESS scores between groups. Since the ACLR group had a higher LESS score, they may have decreased room for an increase in their LESS score, thus sort of a ceiling effect. Conversely, the CTRL group with lower pre‐fatigue LESS scores had more room for increasing their LESS score.
The LESS items in the ACLR group showed more asymmetrical landing compared with the CTRL group typically with smaller knee flexion angle at initial contact, increased valgus at initial contact, more lateral trunk flexion, smaller hip flexion angle, asymmetrical foot contact and increased valgus displacement. Fatigue led to a substantial increase in LESS in the CTRL group as 90% of the subjects were classified as having a landing error due to an increase in knee valgus both at initial contact and maximal valgus angle. A systematic review of fatigue exercise on single‐limb landing biomechanics revealed various biomechanical alterations that may increase the risk of a noncontact ACL injury.14 More specifically, repetitive exercise has also been shown to alter lower extremity biomechanics during double‐leg landing tasks.15,16 Recently, Schmitz et al found sagittal plane lower extremity joint biomechanics from a drop jump were altered toward the end of a 90‐minute intermittent exercise protocol designed to simulate a soccer match. Subjects performed landing with less hip flexion and this more erect landing style has been associated with ACL injury mechanisms27 and has been characterized as a reduction in shock‐attenuating ability of the lower extremity.28 In the current study an increase in knee valgus was observed in the fatigued condition and is consistent with other studies.13,16 The mechanism of increased valgus may in part be attributed to a an alteration in hip kinematics. Pollard and co‐workers showed that limited hip and knee flexion during landing is associated with increased valgus angles and moments.29
The authors of the current study analyzed the involved leg of the ACLR group, but the asymmetrical landing patterns were also seen in the uninvolved leg. The authors are currently working on a revision of the LESS that includes a comparative analysis of both limbs to assess side‐to‐side symmetry.
Biomechanical and neuromuscular risk factors for injury to the ipsilateral and contralateral knee have recently been established for both male and female patients after ACLR with high sensitivity and specificity.5 Regression analyses indicated four predictive factors for secondary injury risk with excellent specificity (88%) and sensitivity (92%): uninvolved hip rotation net moment impulse during landing, frontal‐plane knee motion during landing, sagittal plane knee moment asymmetries at initial contact, and deficits in postural stability on the reconstructed leg. The highly predictive model of second injury risk underscores the importance of targeted return‐to‐sport rehabilitation, as all predictors are modifiable in nature.30 Although the authors performed a different jump task analysis and did not examine postural deficits there are similarities with the current findings and those of Paterno et al.5 The asymmetrical LESS items (knee flexion, knee valgus, extension the hips, trunk lean) may indicate similar landing strategies as found by Paterno and co‐workers. Given that the authors of the current study observed a greater frequency of asymmetrical landings in those with ACLR following fatigue, this may indicate greater relative loading on the uninvolved leg of the patients after ACLR as they are trying to compensate by unloading the involved leg. It could be speculated that this pattern of asymmetrical loading where the athlete initially loads their uninvolved leg more frequently post‐fatigue may result in the type of loading pattern reported by Paterno et al.5 However, future research is needed to investigate the effects of asymmetrical loading on these specific variables.
The authors of the current paper emphasize the need to use objective tools that are sensitive to detect limb‐to‐limb deficits. There is a growing body of literature that supports the current study that put forward the assessment of the quality of movement patterns after ACLR.31‐34 Subsequently rehabilitation protocols can de developed that are targeted to minimize limb asymmetries to prevent second ACL injury.35
Whilst this study only assessed subjects when they were at maximum fatigue, it is possible that the effects of fatigue are seen at a much earlier time point during a fatigue protocol. Previous studies have, for example, shown significant increases in initial contact hip extension and internal rotation, and in peak knee valgus and internal rotation when participants were only partially fatigued.13,22 Effects of fatigue may also induce task specific effects. Webster and colleagues used a series of squats, bilateral jumps and single leg landings to induce fatigue.22 Only hip flexion at initial contact was significantly larger in the ACLR leg compared to the contralateral or control group values. The greater hip flexion was suggested to be a compensatory strategy for patients to reduce the demand for knee control when landing from a height.22 The greater hip flexion is not in agreement with a previous study that showed that patients after ACLR with a hamstring graft utilized reduced hip flexion at initial contact and had lower peak hip flexion compared to a ACLR group who had a patellar tendon graft and CTRL.36 The differences in outcomes between these studies may be attributed to differences in jump tasks, kinematic analysis, time after surgery, and type of surgery.
The ACL‐RSI provides preliminary evidence that the scale may be a relevant screening tool to identify athletes who may be at risk of not returning to their preinjury level of sport by 12 months after surgery.21 A score of less than 56 points on the ACL‐RSI for the ACLR group may indicate an increased risk of not returning to the preinjury level and may help clinicians to identify at‐risk athletes.21 In the current study the mean ACL‐RSI was 49.6 points. Although the authors did not find a relationship between the ACL‐RSI and the change in LESS scores in the subjects with ACLR, patients after ACLR had abnormal scores on both the ACL‐RSI and LESS which in turn may be used for development of RTS criteria in future studies.
Limitations
A number of study limitations must be considered. The patient population in the current study consisted of young patients recruited from the same hospital, which may reduce generalizability of the results. Although the current results showed that fatigue influenced landing strategies, a more precise determination of fatigue should be developed. Only the involved leg in the ACLR group was analyzed and a small sample size was studied. Given the high LESS scores in patients after ACLR and the effect fatigue induced asymmetrical landing patterns putting also the uninvolved leg at risk, future researchers should employ bilateral LESS analysis. The effect of fatigue was only examined directly after the fatigue protocol was completed and it is unknown how long the effects last. Very importantly, it is unknown if LESS scores would improve in the course of time after ACLR, and as such a longitudinal study would be valuable.
CONCLUSION
This pilot study showed different movement patterns between ACLR and CTRL groups in both fatigue and non‐fatigue conditions during jump landing. Significant differences in both groups were found between pre‐fatigue vs. post‐fatigue LESS scores. The ACLR group showed smaller knee flexion angles at initial contact, increased valgus at initial contact, more lateral trunk flexion, smaller hip flexion angle, asymmetrical foot contact and increased maximal valgus. Fatigue resulted in an increase of the LESS scores in both groups. The authors of the current paper emphasize the need to use valid and objective tools that are sensitive to detect limb‐to‐limb deficits and to develop rehabilitation protocols that are targeted to eliminate limb asymmetries. Individualized rehabilitation programs that consider specific neuromuscular characteristics with and without fatigue should be developed in rehabilitation after ACLR.
Acknowledgements
The authors would like to thank Laura Huinink for her invaluable contributions to the development of this study.
REFERENCES
- 1.Simoneau GG Wilk KE The challenge of return to sports for patients post‐ACL reconstruction. J Orthop Sports Phys Ther. 2012;42:300‐301. [DOI] [PubMed] [Google Scholar]
- 2.Wilk KE Macrina LC Cain EL Dugas JR Andrews JR Recent advances in the rehabilitation of anterior cruciate ligament injuries. J Orthop Sports Phys Ther. 2012;42:153‐171. [DOI] [PubMed] [Google Scholar]
- 3.Barber‐Westin SD Noyes FR Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:1697‐1705. [DOI] [PubMed] [Google Scholar]
- 4.Sward P Kostogiannis I Roos H Risk factors for a contralateral anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2010;18:277‐291. [DOI] [PubMed] [Google Scholar]
- 5.Paterno MV Schmitt LC Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38:1968‐1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ahlden M Samuelsson K Sernert N Forssblad M Karlsson J Kartus J The Swedish National Anterior Cruciate Ligament Register: a report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med. 2012;40:2230‐2235. [DOI] [PubMed] [Google Scholar]
- 7.Jang SH Kim JG Ha JK Wang BG Yang SJ Functional performance tests as indicators of returning to sports after anterior cruciate ligament reconstruction. Knee. 2014;21:95‐101. [DOI] [PubMed] [Google Scholar]
- 8.Logerstedt D Grindem H Lynch A, et al. Single‐legged Hop Tests as Predictors of Self‐reported Knee Function After Anterior Cruciate Ligament Reconstruction: The Delaware‐Oslo ACL Cohort Study. Am J Sports Med. 2012;40:2348‐2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Padua DA Marshall SW Boling MC Thigpen CA Garrett WE Beutler AI The Landing Error Scoring System (LESS) Is a Valid and Reliable Clinical Assessment Tool of Jump‐Landing Biomechanics The JUMP‐ACL Study. Am J Sports Med. 2009;37:1996‐2002. [DOI] [PubMed] [Google Scholar]
- 10.Smith HC Johnson RJ Shultz SJ, et al. A Prospective Evaluation of the Landing Error Scoring System (LESS) as a Screening Tool for Anterior Cruciate Ligament Injury Risk. Am J Sports Med. 2012;40:521‐526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Theiss JL Gerber JP Cameron KL, et al. Jump‐Landing Differences Between Varsity, Club, and Intramural Athletes: The Jump‐ACL Study. J Strength Cond Res. 2014;28:1164‐1171. [DOI] [PubMed] [Google Scholar]
- 12.Goerger BM Marshall SW Beutler AI Blackburn JT Wilckens JH Padua DA Anterior cruciate ligament injury alters preinjury lower extremity biomechanics in the injured and uninjured leg: the JUMP‐ACL study. Br J Sports Med. 2014. Feb 21. 10.1136/bjsports‐2013‐092982. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 13.Borotikar BS Newcomer R Koppes R McLean SG Combined effects of fatigue and decision making on female lower limb landing postures: central and peripheral contributions to ACL injury risk. Clin Biomech. 2008;23:81‐92. [DOI] [PubMed] [Google Scholar]
- 14.Santamaria LJ Webster KE The effect of fatigue on lower‐limb biomechanics during single‐limb landings: a systematic review. J Orthop Sports Phys Ther. 2010;40:464‐473. [DOI] [PubMed] [Google Scholar]
- 15.Chappell JD Herman DC Knight BS Kirkendall DT Garrett WE Yu B Effect of fatigue on knee kinetics and kinematics in stop‐jump tasks. Am J Sports Med. 2005;33:1022‐1029. [DOI] [PubMed] [Google Scholar]
- 16.McLean SG Fellin RE Suedekum N Calabrese G Passerallo A Joy S Impact of fatigue on gender‐based high‐risk landing strategies. Med Sci Sports Exerc. 2007;39:502‐514. [DOI] [PubMed] [Google Scholar]
- 17.Sanna G O’Connor KM Fatigue‐related changes in stance leg mechanics during sidestep cutting maneuvers. Clin Biomech. 2008;23:946‐954. [DOI] [PubMed] [Google Scholar]
- 18.Augustsson J Thomee R Karlsson J Ability of a new hop test to determine functional deficits after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2004;12:350‐356. [DOI] [PubMed] [Google Scholar]
- 19.Ardern CL Taylor NF Feller JA Webster KE A systematic review of the psychological factors associated with returning to sport following injury. Br J Sports Med. 2013;47:1120‐1126. [DOI] [PubMed] [Google Scholar]
- 20.Ardern CL Taylor NF Feller JA Webster KE Fear of re‐injury in people who have returned to sport following anterior cruciate ligament reconstruction surgery. J Sci Med Sport. 2012;15:488‐495. [DOI] [PubMed] [Google Scholar]
- 21.Ardern CL Taylor NF Feller JA Whitehead TS Webster KE Psychological Responses Matter in Returning to Preinjury Level of Sport After Anterior Cruciate Ligament Reconstruction Surgery. Am J Sports Med. 2013;41:1549‐1558. [DOI] [PubMed] [Google Scholar]
- 22.Webster KE Santamaria LJ McClelland JA Feller JA Effect of fatigue on landing biomechanics after anterior cruciate ligament reconstruction surgery. Med Sci Sports Exerc. 2012;44:910‐916. [DOI] [PubMed] [Google Scholar]
- 23.DiStefano LJ Padua DA DiStefano MJ Marshall SW Influence of Age, Sex, Technique, and Exercise Program on Movement Patterns After an Anterior Cruciate Ligament Injury Prevention Program in Youth Soccer Players. Am J Sports Med. 2009;37:495‐505. [DOI] [PubMed] [Google Scholar]
- 24.Myer GD Schmitt LC Brent JL, et al. Utilization of Modified NFL Combine Testing to Identify Functional Deficits in Athletes Following ACL Reconstruction. J Orthop Sports Phys Ther. 2011;41:377‐387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brazen DM Todd MK Ambegaonkar JP Wunderlich R Peterson C The effect of fatigue on landing biomechanics in single‐leg drop landings. Clin J Sport Med. 2010;20:286‐292. [DOI] [PubMed] [Google Scholar]
- 26.Webster KE Feller JA Lambros C Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys Ther Sport. 2008;9:9‐15. [DOI] [PubMed] [Google Scholar]
- 27.Boden BP Dean GS Feagin JA Jr. Garrett WE Jr. Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23:573‐578. [DOI] [PubMed] [Google Scholar]
- 28.Blackburn JT Padua DA Influence of trunk flexion on hip and knee joint kinematics during a controlled drop landing. Clin Biomech. 2008;23:313‐319. [DOI] [PubMed] [Google Scholar]
- 29.Pollard CD Sigward SM Powers CM Limited hip and knee flexion during landing is associated with increased frontal plane knee motion and moments. Clin Biomech. 2010;25:142‐146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Myer GD Martin L Jr. Ford KR, et al. No association of time from surgery with functional deficits in athletes after anterior cruciate ligament reconstruction: evidence for objective return‐to‐sport criteria. Am J Sports Med. 2012;40:2256‐2263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pairot de Fontenay B Argaud S Blache Y Monteil K Asymmetries in joint work during multi‐joint movement after anterior cruciate ligament reconstruction: A pilot study. Scand J Med Sci Sports. 2014.Mar 20. 10.1111/sms.12207. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 32.Xergia SA Pappas E Zampeli F Georgiou S Georgoulis AD Asymmetries in functional hop tests, lower extremity kinematics, and isokinetic strength persist 6 to 9 months following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2013;43:154‐162. [DOI] [PubMed] [Google Scholar]
- 33.Castanharo R da Luz BS Bitar AC D’Elia CO Castropil W Duarte M Males still have limb asymmetries in multijoint movement tasks more than 2 years following anterior cruciate ligament reconstruction. J Orthop Sci. 2011;16:531‐535. [DOI] [PubMed] [Google Scholar]
- 34.Orishimo KF Kremenic IJ Mullaney MJ McHugh MP Nicholas SJ Adaptations in single‐leg hop biomechanics following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18:1587‐1593. [DOI] [PubMed] [Google Scholar]
- 35.Gokeler A Benjaminse A Hewett TE, et al. Feedback Techniques to Target Functional Deficits Following Anterior Cruciate Ligament Reconstruction: Implications for Motor Control and Reduction of Second Injury Risk. Sports Med. 2013;43:1065‐1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Decker M Torry M Sterett W Functional adaptations affect landing performance after ACL reconstruction. Biomechanics. 2000:29‐40. [Google Scholar]