ABSTRACT
Background:
Training guidelines for novice runners are needed to reduce the risk of injury. The purpose of this study was to investigate whether the risk of injury varied in obese and non‐obese individuals initiating a running program at different weekly distances.
Methods:
A volunteer sample of 749 of 1532 eligible healthy novice runners was included in a 3‐week observational explorative prospective cohort study. Runners were categorized into one of six strata based on their body mass index (BMI) (≤30=low; >30=high) and running distance after 1 week (<3 km = low; 3 to 6 km = medium; >6 km = high). Data was collected for three weeks for the six strata. The main outcome measure was running‐related injury.
Results:
Fifty‐six runners sustained a running‐related injury during the 3‐week data collection. A significantly greater number of individuals with BMI>30 sustained injuries if they ran between 3 to 6 km (cumulative risk difference (CRD) = 14.3% [95%CI: 3.3% to 25.3%], p<0.01) or more than 6 km (CRD = 16.2% [95%CI: 4.4% to 28.0%], p<0.01) the first week than individuals in the reference group (low distance and low BMI). The effect‐measure modification between high running distance and BMI on additive scale was positive (11.7% [‐3.6% to 27.0%], p=0.13). The number of obese individuals needed to change their running distance from high to low to avoid one injury was 8.5 [95%CI: 4.6 to 52].
Conclusions:
Obese individuals were at greater risk of injury if they exceeded 3 km during the first week of their running program. Because of a considerable injury risk compared with their non‐obese peers, individuals with a BMI>30 may be well advised to begin running training with an initial running distance of less than 3 km (1.9 miles) the first week of their running regime. Large‐scale trials are needed to further describe and document this relationship.
Level of Evidence:
Level 2b
Keywords: Body mass index, distance, injury risk, Running
INTRODUCTION
Running as a leisure‐time activity has increased in popularity during the past decades,1 and as a consequence, millions of novice runners around the world begin running each year. They may start their running career by using training schedules found on the Internet; by using advice from a friend, a coach or a clinician; or by simply using a self‐structured approach. Unfortunately, none of these approaches relies on evidence‐based knowledge on how training schedules should be designed in order to reduce the risk of running‐related injuries.2
Running‐related injuries are common among novice runners,2 affecting approximately 30 runners per 1000 hours of running.3‐5 Because of the high incidence, interventions to reduce the number of injuries are greatly needed.6 Training errors are believed to be the primary risk factor for injury because training, pragmatically, must be a part of the causal chain leading to injury.2,7,8 Randomized controlled trials have been conducted,5,9 but despite adequate designs, these studies fail to identify training‐related mechanisms leading to injury in novice runners. In contrast, studies have identified high body mass index (BMI) to be associated with increased risk of injury.10,11 In novice runners enrolled in a prospective study, Buist et al10 found 25% (82 of 334) of the novice runners with BMI above 25 sustained a running‐related injury (RRI) during follow‐up compared to 15% (76 of 514) in the group of participants with BMI below 25 (p=0.03). Importantly, the mean exposure time (time spent running) was equal in both groups. This may lead to the assumption, that increasing BMI exposes the lower extremity to increased load while running which ultimately increase the injury risk. Still, a BMI > 26 has been suggested to be protective for injury.12 But importantly, this observation did not take into account the running exposure. If the overweight persons ran less, the statement presented that high BMI is protective, may be caused by a reduced training stimulus which reduces the risk of injury. In order to identify the role of BMI in the development of injury, it is important to take into account the exposure to running and to question if an obese individual is able to tolerate the same training load as a non‐obese individual.
Since no studies have investigated the association between weekly distance during the first week of a running regimen and the risk of running‐related injuries, the purpose of this study was to investigate whether the risk of injury varied in obese and non‐obese individuals initiating a running program at different weekly distances. The risk of injury was hypothesized to be more pronounced in novice runners with a BMI greater than 30.
METHODS
Study design
An observational 3‐week prospective cohort study was designed based on the Danish Novice Running (DANO‐RUN) study. The original purpose of the DANO‐RUN study is presented elsewhere.13 Because the study was explorative, several other papers have been published from the same dataset. 14‐16 The study design, the study procedures, and the informed consent procedure were presented to the Ethics Committee of Central Denmark Region (M‐20110114). The committee waived the request of ethics approval because the study design was observational. According to Danish law, observational studies do not need to be approved by an ethics committee. The Danish data protection agency approved the study.
Participants
A sample of 933 healthy novice runners was included in the DANO‐RUN study. Informed written consent was obtained from all participants prior to inclusion. A novice runner was defined as a person who had not run regularly during the preceding year. The cut‐off to define regularly was set at 10 km of total running distance the year prior to inclusion. Thus, persons running 4 times 2 km the past year were eligible to participate, whereas persons running a total of 3 times 6 km the past year were excluded. A flow‐chart of those excluded prior to or at baseline is presented in another paper.16 Exclusion criteria were: age below 18 or above 65, injury in the lower extremities or back three months preceding a baseline investigation, no e‐mail address or access to the internet, participation in other sports for more than four hours per week, use of insoles while running, pregnancy, previous strokes, heart diseases, pain in the chest during training, or unwilling to run in a neutral running shoe or use a global positioning system (GPS) watch to quantify training characteristics.
Assessment of running distance
At baseline, all participants received the same neutral running shoe (Supernova Glide 3 Male/Female, Adidas, Herzogenaurach, Germany) and were instructed to use the shoe in all running sessions. Participants were then instructed to run as much as they wanted during the 3‐week follow‐up period. Their running regime was considered self‐structured because no prescriptions or guidelines regarding the training distance, duration, intensity, or frequency were given. Participants were thus allowed to run any distance of their choice (for example, 500 meters, or a greater distance of 15 km) during the first week of the study period.
The running distance was measured in km using a global positioning system (GPS) watch (Forerunner 110 M, Garmin International Inc., Olathe, KS, USA). The GPS method to objectively measure training distance among runners has previously been proven as valid, with a measurement error of ≤ 6.2% compared with a gold standard.11,17 Participants were instructed to upload training data to a web‐based training diary (http://www.vilober.dk/). If a problem with the GPS device occurred during follow‐up, participants were instructed to upload the missing training session(s) manually by reporting running distance and time spent running. Participants were also instructed to contact the DANO‐RUN study group through their diary to solve any technical problems in particular if the GPS device did not work correctly. During and after follow‐up, data quality control was performed. If suspicious data occurred, the participant was contacted to verify that the data uploaded to the diary was correct. If the participant did not respond to this contact, they were censored at the time the suspicious data was uploaded for the first time. As an example of suspicious data, a person was contacted if he or she ran with an average speed of 50 km per hour.
Definition of exposure
The main exposure of interest was the cumulative running distance (measured in km) during the first week (7 days) after the beginning of the running assessment (first time the participant ran after being included in the study). The beginning of the first week (day 1) was defined as the moment the participant completed the first running session, and the end of week 1 was defined as six days after day 1. Participants were then categorized into exposure strata based on their cumulative running distance the first week. The categorization was performed using two cut offs. By doing so, a more or less equal number of subjects (approximately 33%) were assigned to one of the following strata: less than 3 km (n = 258), 3 to 6 km (n= 225), and finally more than 6 km (n = 266). In addition to the categorization of running distance into three categories, analysis were stratified based on BMI (dichotomized based on BMI≤30 or BMI>30) because a high BMI has been shown to be associated with increased risk of injury among novice runners.10,11 The authors hypothesized that BMI would be related to the association between running distance the first week and risk of injury as an effect‐measure modifier. Because running distance was categorized into three categories and analysis was stratified based on BMI into two groups, a total of six strata were identified (Table 1).
Table 1.
The categorization and number of the participants in the six strata
| BMI category | Running distance the first week | Number of participants |
|---|---|---|
| BMI≤30 | <3 km | n=200* |
| 3 to 6 km | n=180 | |
| >6 km | n=228 | |
| BMI>30 | <3 km | n=58 |
| 3 to 6 km | n=45 | |
| >6 km | n=38 |
= the reference strata. BMI = Body mass index. Km = kilometers.
The follow‐up of three weeks was chosen because it was hypothesized that injuries occurring after three weeks are related to the weekly change in running distance rather than the absolute distance covered from the beginning of the running program.
Assessment of outcome: Running‐related injury
At baseline, participants were presented with the injury definition; “An injury is defined as any musculoskeletal complaint of the lower extremity or back causing a restriction of running for at least one week”. This injury definition was a modified version of a definition used by Buist et al.5
If a running‐related injury was sustained, participants were instructed to use their personal web–based training diary to contact the medical team. The injured participant was contacted by telephone and an appointment for a clinical examination was made, preferably no later than 1 week after initial contact. After thorough examination by a physiotherapist with experience in diagnosing running‐related injuries, a diagnosis was made. In most cases, the diagnosis was made without the use of diagnostic imaging, as suggested by Khan et al,18 but if further examination including diagnostic imaging was needed, the participant was referred to an extensive medical examination at the Division of Sports Traumatology, Aarhus University Hospital.
Importantly, only injuries occurring during the first 3 weeks from the first day in the study were included in the analyses. Of the 933 participants originally included in the DANO‐RUN study, 183 sustained injuries. Of these, three were included by mistake because they were injured just before inclusion in the study. The remaining 180 injuries occurred after the end of the study period of three weeks used for the present paper (the total follow‐up in the DANO‐RUN study was 1 year). The 183 injured individuals may have influenced the results regarding the risk of injury during the first three weeks and were, therefore, excluded from the analysis in the present study. In addition, one participant was excluded because data from the first seven running sessions were uploaded manually. Thus, the sub‐sample included in the present study comprised 749 individuals.
Assessment of confounders
Prior to analyses, the authors hypothesized that the following variables would be the major factors possibly confounding the association between running distance during the first week of a running regime and risk of running‐related injury during the following three weeks: distance covered in week two, distance covered in week three, frequency and intensity of training sessions in weeks one to three, and progression in running distance from weeks one to three.2 In addition, more variables than BMI may be considered as effect‐measure modifiers on the association between running distance and risk of injury, mainly previous running‐related injuries and age.19
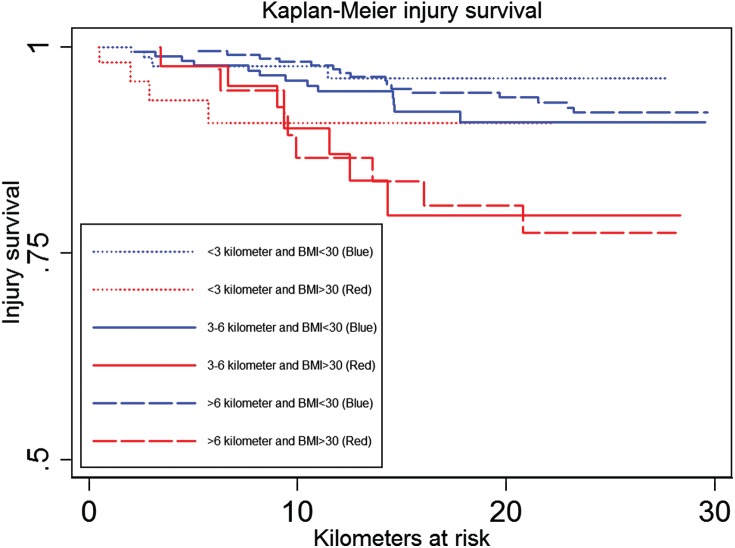
Statistical analyses
The injury proportion as a function of distance was estimated using the Kaplan‐Meier curve. Time to injury at 10 and 20 km was analyzed using the cumulative running distance as time scale. The cumulated injury risk difference was analyzed across the six exposure groups by performing a generalized linear regression using the pseudo values method.20,21 In all analyses, the reference group was persons with a BMI less than 30 running less than 3 km the first week. This group was selected as reference because it was hypothesized that these individuals would have the lowest injury risk. When estimating risk differences by the pseudo values method, at least 10 injuries are needed per parameter (number of parameters = number of categories per variable – 1) to avoid violation of the statistical assumptions.22 Participants were categorized into six groups based on their BMI (≤ 30 and > 30) and based on the distance covered after 1 week of running (< 3 km, 3 km to 6 km and > 6 km). Based on this, at least 50 running‐related injuries were needed to perform a valid analysis stratified by BMI. In addition, the remaining injuries above the 50 needed for the crude analysis did only allow for one confounder (distance covered in week 2) to be included in the adjusted analysis. Participants were right‐censored in case of pregnancy, disease, lack of motivation, non‐running‐related injury causing a permanent stop of running, unwillingness to attend clinical examination in case of injury, if a different shoe was used than the neutral shoe, or end of follow‐up after 1‐year, whichever came first. The number needed (equal to number needed to treat [NNT]) to convert their running distance from more than 3 km to less than 3 km in order to avoid one RRI was based on the equation: NNT = ‐1 / cumulative risk difference. The absolute excess risk was used to measure the size of effect‐measure modification. Differences were considered statistically significant at p<.05, and estimates are presented with 95% confidence intervals (CI). Results were presented according to the guidelines suggested by Knol and VanderWeele.23 All analyses were performed using STATA/SE version 12 (StataCorp LP, 2011, College Station, Texas, USA).
RESULTS
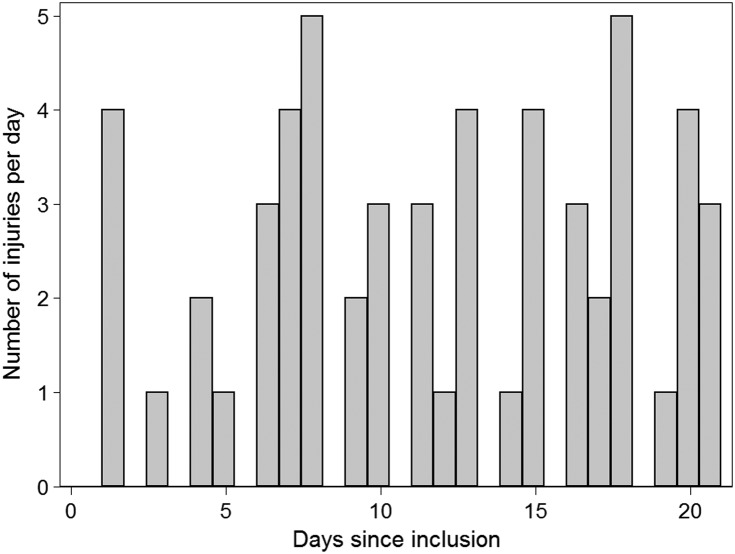
Of the 749 participants (381 males/368 females; mean age 36.7 ± 10.2; mean BMI 26.2 ± 4.4 kg/m2) included in the analyses, a total of 56 sustained a running‐related injury during the three week follow‐up, with 15 injuries occurring in week one, 19 injuries occurring in week two, and finally 22 injuries occurring in week three. The numbers of injured participants, non‐injured participants, and censored participants after week one, after week two, and after week three stratified by BMI status are presented in Table 2. In addition, the numbers of injuries per day during the first 21 days of the study are presented in Figure 1. One of the injuries occurred on a traumatic basis while the rest were considered overuse. The most frequent diagnoses were medial tibial stress syndrome n=13; medial meniscus injury n=8; patellofemoral pain n=7; and achilles tendinopathy n=7. During the first week, the median running distance was 4.46 km, ranging from a minimum of 413 meters to a maximum exceeding 30 km (n = 2).
Table 2.
The flow of the included participants. Number (counts) of injured, non‐injured, and censored participants are presented after week 1, week 2, and week 3 stratified by BMI status. In addition, the median distances in kilometer (km) the participants covered during each of the 3 weeks are presented.
| Subgroup | Week 1 | Week 2 | Week 3 | |
|---|---|---|---|---|
| All participants | All | 749 | 715 | 693 |
| Injured | All | 15 | 18 | 22 |
| BMI ≤ 30 | 10 | 9 | 18 | |
| BMI > 30 | 5 | 10 | 4 | |
| Non‐injured | All | 715 | 693 | 668 |
| BMI ≤ 30 | 587 | 575 | 554 | |
| BMI > 30 | 128 | 118 | 114 | |
| Censored | All | 19 | 3 | 3 |
| BMI ≤ 30 | 11 | 3 | 3 | |
| BMI > 30 | 8 | 0 | 0 | |
| Median distance | All | 4.47 | 4.11 | 3.82 |
| BMI ≤ 30 | 4.66 | 4.26 | 3.90 | |
| BMI > 30 | 3.58 | 3.77 | 3.33 |
BMI = body mass index.
Figure 1.
Number of injuries per day during the 3‐week (21 days) follow‐up.
The novice runners included in the analyses ran a total of 14,767 km until injury, until censoring, or until the end of the 3‐week follow‐up. The Kaplan‐Meier curve for the six exposure groups, visualizing the injury proportion as a function of km, is presented in Figure 2. In Table 3, results from the generalized linear regression model for the cumulative risk of running‐related injury at 10 and 20 km are presented.
Figure 2.
Visualizing the injury proportion as a function of km in the six exposure groups. All red lines represent individuals with a BMI > 30, while the blue lines represent individuals with a BMI ≤ 30.
Table 3.
Cumulative risk differences (cRD) for running‐related injury*.
| Running distance the first week | cRDs [95%CI] for > 3 to ≤ 6 km within strata of BMI | cRDs [95%CI] for > 6 km within strata of BMI | |||||||
|---|---|---|---|---|---|---|---|---|---|
| ≤ 3km | > 3 to ≤ 6 km | > 6 km | |||||||
| Injury/ no injury | cRD [95%CI] | Injury/ no injury | cRD [95%CI] | Injury/ no injury | cRD [95%CI] | ||||
| After 10km: | Low BMI [≤30] | 4/196 | Reference | 7/173 | 1.0% [−3.4%; 5.3%] p=0.67 | 4/224 | −1.6% [−5.8%; 2.5%] p=0.44 | 1.0% [−3.4%; 5.3%] p=0.67 | −1.6% [−5.8%; 2.5%] p=0.44 |
| High BMI [>30] | 4/54 | 5.8% [−0.5%; 12.2%] p=0.07 | 4/38 | 7.3% [0.2%; 14.3%] p=0.04 | 5/33 | 12.7% [5.2%; 20.2%] p<0.01 | 1.5% [−7.0%; 9.9%] p=0.74 | 6.9% [−2.0%; 15.8%] p=0.13 | |
| After 20km: | Low BMI [≤30] | 5/195 | Reference | 13/167 | 2.5% [−4.3%; 9.4%] p=0.47 | 13/215 | −1.0% [−7.4%; 5.5%] p=0.78 | 2.5% [−4.3%; 9.4%] p=0.47 | −1.0% [−7.4%; 5.5%] p=0.78 |
| High BMI [>30] | 4/54 | 5.4% [−4.5%; 15.4%] p=0.28 | 7/38 | 14.3% [3.3%; 25.3%] p=0.01 | 7/31 | 16.2% [4.4%; 28.0%] p<0.01 | 8.8% [−4.4%; 22.1] p=0.19 | 10.8% [−3.1%; 24.7%] p=0.13 | |
CI = confidence interval. Km = kilometer. BMI = body mass index
Chi2 tests for difference between all six groups were performed after 10 km and 20 km revealing a significant difference across all six groups (p<0.01).
Two analyses are presented: after 10 km and after 20 km. The reference risks for the runners with a BMI ≤ 30 and running less than 3 km during the first week were 3.1% [0.1% to 6.1%] after 10 km and 6.5% [1.7% to 11.2%] after 20 km. Kilometers at risk for the 749 novice runners were 14,676 km. Measure of effect modification on additive scale (Absolute Excess Risk): 11.7% [−3.6% to 27.0%], p=0.13 (BMI>30 and >6km after 20 km) and 6.3% [−8.6% to 21.2%], p=0.41 (BMI>30 and >3 to ≤ 6 km after 20 km).
Results revealed significant differences in cumulative risk between individuals with a BMI above 30 running more than 3 km the first week compared with individuals with a BMI less than 30 and running less than 3 km the first week (p < 0.01). Among the obese individuals, those running more than 6 km during the first week faced a greater, although non‐significant risk (risk difference = 10.8% [95% CI: ‐3.1% to 24.7%], p=0.13) after 20 km of running compared with those running less than 3 km the first week. Based on this, the number of obese individuals needed to change their running distance from more than 6 km to less than 3 km the first week in order to avoid one running‐related injury was 8.5 [95% CI: 4.6 to 52]. In addition to this, if the obese individuals running more than 6 km reduced their BMI and started by running less than 3 km the first week, the number needed to treat to avoid one injury was 6.17 [95% CI: 4 to 13]. In addition to the stratified analyses, adjusted analyses were performed. The analyses adjusted for the running distance in week two revealed no significant changes in any of the estimates from the crude analyses presented.
DISCUSSION
This is the first study to provide insight into the initial running distance completed by novice runners and their risk of injury during the first 3 weeks of their running regime. Importantly, individuals with a BMI greater than 30 may be well advised to take‐up running but refraining from running more than 3 km during the first week in order to reduce the risk of injury. If they do so, the risk of injury declines from 22.7% to 11.9% after 20 km of running. Although more time‐consuming, another approach that may be effective in reducing the risk of injury may be to reduce the BMI before initiating a running program: Among those running more than 6 km the first week, obese individuals faced a 17.2% greater risk of injury than those with a BMI less than 30. Thus, a weight‐loss intervention targeted individuals with a BMI greater than 30 prior to the start of a running regime may also be an injury‐reducing approach.
The effect‐measure modification on additive scale was positive and close to significant (11.7% [‐3.6% to 27.0%], p=0.13). This means that there were some indications that the estimated joint effect on the additive scale of running more than 6 km with a BMI greater than 30 was larger than the estimated effect of BMI and running distance, so there is positive effect modification of increasing running distance the first week across strata of BMI. Based on this, individuals with a BMI greater than 30 should ideally lose weight and take‐up running with a distance below 3 kilometers the first week.
One major strength of the present paper was the approach used to categorize participants into six different strata. BMI was considered to be an effect‐measure modifier on the association between running distance the first week and development of injury. As described by Meeuwisse,19 it is very important to distinguish between stratified analysis (using effect‐measure modification) and adjusted analysis (using confounders). In a majority of the previous studies on novice runners,3‐5,9 other variables have been included as confounders. But the findings in the present paper suggest that BMI should be included as an effect‐measure modifier because the effect of the running distance is different across BMI strata. The authors therefore suggest that more work should be devoted to distinguish between confounders and effect‐measure modifiers in studies on running‐related injuries.
It is very important to stress that the results of the present study should be interpreted with caution. Owing to the prospective design of the present study, the risk of the results being biased by confounding is noteworthy, and it is, indeed, possible that the estimates presented in the present article are highly biased. One variable (cumulative running distance in week two) was adjusted for and we had the data to undertake further adjustments. But the number of events per parameter included in a pseudo‐values approach with cumulative risk difference as measure of association is at least 10. In the present study, 56 runners sustained a running‐related injury of whom 28 sustained the injury before completing a total of 10 kilometers of running and 49 before completing a total of 20 kilometers. Then, one categorical variable with three groups (running volume the first week categorized into three groups) further stratified by BMI as a dichotomous variable (BMI≤30 or BMI>30) and one continuous variable (cumulative running distance in week 2) was the upper limit of variables to be included in the adjusted/stratified analysis to avoid violation of the assumptions behind the statistical model. Instead of including more variables, which the model allows for, the authors chose to strictly follow the assumption behind the statistical model. As a consequence, possible confounders like the running frequency, running pace, or how rapidly the runners changed their training distance over time were not adjusted for.2 In addition, it was not possible to further stratify the results based on previous injuries. It may be very likely that individuals with a high BMI who ran more than 3 km the first week may face an even more pronounced risk of injury if they had a previous injury, whereas the risk may have been smaller among the obese individuals who had not had any severe injuries previously. Unfortunately, at least 200 injuries were needed to perform such detailed analysis. The problem presented highlights the need for further prospective studies that include more individuals than the 933 originally included in the present study. Still, the results from the present study provide a foundation for designing future randomized controlled trials in this field of research.
CONCLUSION
Individuals with a BMI greater than 30 had an increased risk of RRI in the first three weeks of training, and may be well advised to begin running with an initial total running distance of less than 3 km during the first week of their running regimen. More large‐scale randomized studies are needed to further describe and document this relationship.
REFERENCES
- 1.Laub TB Pilgaard M Sports participation in Denmark 2011. Copenhagen, Denmark: Danish Institute for Sports Studies; 2013. [Google Scholar]
- 2.Nielsen RO Buist I Sorensen H Lind M Rasmussen S Training errors and running related injuries: A systematic review. Int J Sports Phys Ther. 2012;7(1):58‐75. [PMC free article] [PubMed] [Google Scholar]
- 3.Buist I Bredeweg SW Bessem B van Mechelen W Lemmink KA Diercks RL Incidence and risk factors of running‐related injuries during preparation for a 4‐mile recreational running event. Br J Sports Med. 2010;44(8):598‐604. [DOI] [PubMed] [Google Scholar]
- 4.Buist I Bredeweg SW Lemmink KA van Mechelen W Diercks RL Predictors of running‐related injuries in novice runners enrolled in a systematic training program: A prospective cohort study. Am J Sports Med. 2010;38(2):273‐280. [DOI] [PubMed] [Google Scholar]
- 5.Buist I Bredeweg SW van Mechelen W Lemmink KA Pepping GJ Diercks RL No effect of a graded training program on the number of running‐related injuries in novice runners: A randomized controlled trial. Am J Sports Med. 2008;36(1):33‐39. [DOI] [PubMed] [Google Scholar]
- 6.Finch C A new framework for research leading to sports injury prevention. J Sci Med Sport. 2006;9(1‐2):3‐9. [DOI] [PubMed] [Google Scholar]
- 7.Meeuwisse WH Tyreman H Hagel B Emery C A dynamic model of etiology in sport injury: The recursive nature of risk and causation. Clin J Sport Med. 2007;17(3):215‐219. [DOI] [PubMed] [Google Scholar]
- 8.Hreljac A Etiology, prevention, and early intervention of overuse injuries in runners: A biomechanical perspective. Phys Med Rehabil Clin N Am. 2005;16(3):651‐67, vi. [DOI] [PubMed] [Google Scholar]
- 9.Bredeweg SW Zijlstra S Buist I The GRONORUN 2 study: Effectiveness of a preconditioning program on preventing running related injuries in novice runners. the design of a randomized controlled trial. BMC Musculoskelet Disord. 2010;11:196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buist I Bredeweg SW Higher risk of injury in overweight novice runners. Br J Sports Med. 2011;45(4):338. [Google Scholar]
- 11.Nielsen RO Cederholm P Buist I Sorensen H Lind M Rasmussen S Can GPS be used to detect deleterious progression in training volume among runners? J Strength Cond Res. 2013;27(6):1471‐1478. [DOI] [PubMed] [Google Scholar]
- 12.Taunton JE Ryan MB Clement DB McKenzie DC Lloyd‐Smith DR Zumbo BD A prospective study of running injuries: The vancouver sun run “in training” clinics. Br J Sports Med. 2003;37(3):239‐244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nielsen RO Ramskov D Sørensen H Lind M Rasmussen S Buist I Protocol for the dano‐run study: A 1‐year observational follow up study on running related injuries in 1000 novice runners. Br J Sports Med. 2011;45(4):365. [Google Scholar]
- 14.Bertelsen ML Jensen JF Nielsen MH Nielsen RO Rasmussen S Footstrike patterns among novice runners wearing a conventional, neutral running shoe. Gait Posture. 2013;38(2):354‐356. [DOI] [PubMed] [Google Scholar]
- 15.Nielsen RO Buist I Parner ET, et al. Predictors of running‐related injuries among 930 novice runners: A 1‐year prospective follow‐up study. OJSM. 2013;1(1):1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nielsen RO Buist I Parner ET, et al. Foot pronation is not associated with increased injury risk in novice runners wearing a neutral shoe: A 1‐year prospective cohort study. Br J Sports Med. 2014;48(6):440‐447. [DOI] [PubMed] [Google Scholar]
- 17.Townshend AD Worringham CJ Stewart IB Assessment of speed and position during human locomotion using nondifferential GPS. Med Sci Sports Exerc. 2008;40(1):124‐132. [DOI] [PubMed] [Google Scholar]
- 18.Khan KM Tress BW Hare WS Wark JD Treat the patient, not the x‐ray: Advances in diagnostic imaging do not replace the need for clinical interpretation. Clin J Sport Med. 1998;8(1):1‐4. [PubMed] [Google Scholar]
- 19.Meeuwisse WH Athletic injury etiology: Distinguishing between interaction and confounding. Clin J Sport Med. 1994;4(3):171‐175. [Google Scholar]
- 20.Parner ET Andersen PK Regression analysis of censored data using pseudo‐observations. Stata Journal. 2010;10(3):408. [Google Scholar]
- 21.Klein JP Logan B Harhoff M Andersen PK Analyzing survival curves at a fixed point in time. Stat Med. 2007;26(24):4505‐4519. [DOI] [PubMed] [Google Scholar]
- 22.Hansen SN Andersen PK Parner ET Events per variable for risk differences and relative risks using pseudo‐observations. Lifetime Data Anal. 2014: In press. [DOI] [PubMed] [Google Scholar]
- 23.Knol MJ VanderWeele TJ Recommendations for presenting analyses of effect modification and interaction. Int J Epidemiol. 2012;41(2):514‐520. [DOI] [PMC free article] [PubMed] [Google Scholar]