Abstract
Benign cardiac fibroma is rarely reported in adults. Its clinical symptoms are related to outflow obstruction or dysrhythmias. We present the case of a 70-year-old woman who had a syncopal episode from ventricular tachycardia caused by cardiac fibroma. Because of unfavorable tumor anatomy, the patient was not a candidate for surgical excision, and she declined orthotopic heart transplantation. To prevent sudden cardiac death, we placed an implantable cardioverter-defibrillator, and the patient remained well throughout the 2-year follow-up period. To our knowledge, this is the first report of implantable cardioverter-defibrillator therapy to treat an adult patient's unresectable cardiac fibroma.
Keywords: Adult; cardioverter-defibrillators, implantable/therapy/utilization; fibroma/diagnosis/pathology; tachycardia, ventricular/etiology; treatment outcome
Cardiac fibroma is rarely reported in adults. Children who survive this benign tumor of the heart might present during adulthood with arrhythmias or mechanical complications. Surgical excision or orthotopic heart transplantation (OHT) is the treatment of choice. Adult patients with unresectable tumors who present with syncope or survive cardiac arrest from ventricular arrhythmias might benefit from implantable cardioverter-defibrillator (ICD) therapy. We present the case of an adult woman whose fibroma-induced ventricular tachycardia (VT) was treated with an ICD.
Case Report
In September 2011, a 70-year-old woman emergently presented with a single syncopal episode, from which she recovered spontaneously. Her heart rate was 94 beats/min, her blood pressure was 130/68 mmHg, and her oxygen saturation was 100% on room air. Physical examination revealed nothing unusual. The results of laboratory tests, chest radiography, and 12-lead electrocardiography were normal. A transthoracic echocardiogram showed a noncontractile, solid, 4.4 × 2.9-cm intramyocardial mass in the basal interventricular septum (Fig. 1A). Computed tomograms (CT) of the chest showed a 3.8 × 3.3-cm calcified mass in the basal portion of the interventricular septum; the mass extended into the inferior wall of the left ventricle (LV) and bulged into the LV cavity without evident LV outflow obstruction (Fig. 1B). Cardiac magnetic resonance (CMR) images revealed a 3.8 × 3.38-cm mass, isodense on T1 weighting and hyperdense on T2 weighting. Triple-inversion sequences better characterized the mass (Fig. 1C), and gadolinium contrast showed delayed enhancement (Fig. 1D). The noncontractility on echocardiography, the presence of calcium on CT, and the delayed gadolinium enhancement on CMR strongly suggested a benign cardiac fibroma.1 The location and extent of the tumor precluded surgical resection. The option of OHT was presented; however, the patient declined surgical intervention. Because of the known predisposition of cardiac fibroma to generate malignant ventricular arrhythmias and because of the risk of sudden cardiac death (SCD), we performed electrophysiologic studies to further evaluate the patient's syncope. We induced VT during the study (Fig. 2). During the longest period of VT (2 min), the patient lost consciousness and became hypotensive; she was successfully treated with a 150-J direct-current shock. A dual-chamber ICD was implanted for the prevention of SCD. During the 2-year follow-up period, the patient had no further episodes of sustained VT, and she remained well.
Fig. 1.
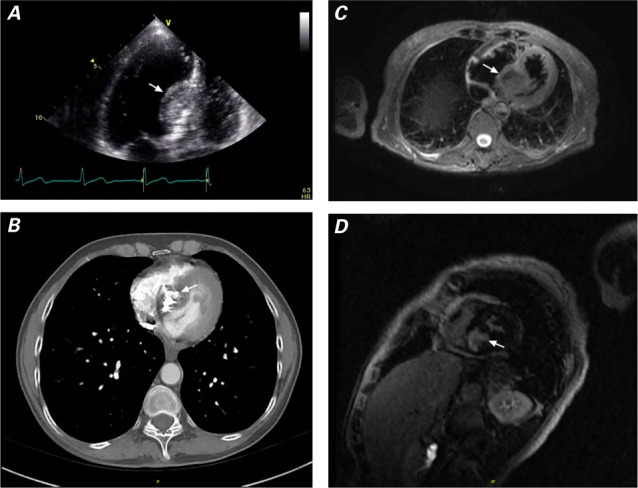
A) Transthoracic echocardiogram (apical 4-chamber view) shows a solid mass in the basal intraventricular septum. B) Cardiac computed tomogram shows a heavily calcified mass in the basal septum. Cardiac magnetic resonance images show the mass C) with isodensity similar to that of the myocardium (triple-inversion cardiac sequence) and D) by delayed gadolinium enhancement.
Fig. 2.
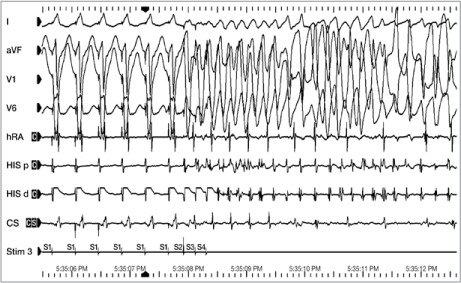
Electrocardiogram shows ventricular tachycardia induced during electrophysiologic testing.
CS = coronary sinus; HIS d = His distal; HIS p = His proximal; hRA = high right atrium; Stim 3 = pacing train (S1) and extra-stimuli (S2, S3, and S4).
Discussion
Cardiac fibroma, a benign neoplasm of the myocardium, is typically seen in children (median age upon diagnosis, 13 yr).2 This tumor is rarely reported in adults. Most cardiac fibromas originate in the LV free wall. The clinical manifestations depend on the location and extent of the tumor. Small, localized tumors might cause no symptoms, whereas large ones can cause ventricular arrhythmias, congestive heart failure, conduction abnormalities, and LV inflow or outflow obstruction. In a review of 38 patients,3 ventricular arrhythmias were reported in 9 patients. Seven had documented VT, and 2 of the 7 presented with syncope. According to that review, patients with small tumors underwent completely curative surgical excision, and those with large, unresectable tumors underwent OHT.4 Patients who were not surgical candidates for OHT underwent partial resection of the tumor, to relieve symptoms caused by obstruction or chamber compression. Our patient declined OHT, and the unfavorable anatomy of the tumor precluded surgical resection, so an ICD was implanted for the prevention of SCD. Children with unresectable cardiac fibroma have been given ICDs for this purpose5; however, to our knowledge, ours is the first report of ICD therapy to treat an unresectable fibroma in an adult.
The long-term outcome in patients with unresectable cardiac fibromas in the absence of conduction abnormalities or LV outflow obstruction is not known. On the basis of the pediatric medical literature, even asymptomatic untreated cardiac fibroma increases the risk of death, chiefly because of malignant ventricular arrhythmias. To prevent SCD, ICD placement can be considered in patients who have unresectable cardiac fibromas and who are not candidates for OHT. Class III or Ic antiarrhythmic medications or a β-blocker can be prescribed if the patient has recurrent VT after ICD placement. The role of catheter-based ablation in the management of VT in patients with cardiac fibroma is not known.
References
- 1.Araoz PA, Mulvagh SL, Tazelaar HD, Julsrud P, Breen JF. CT and MR imaging of benign primary cardiac neoplasms with echocardiographic correlation. Radiographics. 2000;20(5):1303–19. doi: 10.1148/radiographics.20.5.g00se121303. [DOI] [PubMed] [Google Scholar]
- 2.Burke A, Virmani R. Pediatric heart tumors. Cardiovasc Pathol. 2008;17(4):193–8. doi: 10.1016/j.carpath.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 3.Nwachukwu H, Li A, Nair V, Nguyen E, David TE, Butany J. Cardiac fibroma in adults. Cardiovasc Pathol. 2011;20(4):e146–52. doi: 10.1016/j.carpath.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 4.Goldstein DJ, Oz MC, Rose EA, Fisher P, Michler RE. Experience with heart transplantation for cardiac tumors. J Heart Lung Transplant. 1995;14(2):382–6. [PubMed] [Google Scholar]
- 5.Kusano KF, Ohe T. Cardiac tumors that cause arrhythmias. Card Electrophysiol Rev. 2002;6(1–2):174–7. doi: 10.1023/a:1017936622990. [DOI] [PubMed] [Google Scholar]


