Abstract
Perforation of a cardiac chamber is an infrequent but serious sequela of pacemaker lead implantation. An even rarer event is the perforation of the aorta by a protruding right atrial wire. We present here the first case in the medical literature of aortic perforation as a sequela to the implantation of a cardiac resynchronization therapy defibrillator.
The patient was a 54-year-old man with idiopathic dilated cardiomyopathy who underwent the implantation of a defibrillator, with no apparent sequelae. Six hours after the procedure, he experienced cardiac tamponade and required urgent open-chest surgery. The pericardial effusion was found to be caused by mechanical friction of a protruding right atrial wire on the aortic root. The aortic root and the atrial wall were both repaired with Prolene suture, which achieved complete control of the bleeding. There was no need to reposition the atrial wire. The patient had a good postoperative recovery.
Keywords: Aorta/injuries, iatrogenic; cardiac tamponade/etiology; cardioverter-defibrillator, implantable/adverse effects/complications; hemostasis, surgical; pacemaker, artificial/adverse effects/complications; pericardial effusion/etiology
Perforation of a cardiac chamber is an infrequent but severe complication/sequela* of pacemaker lead implantation. An even rarer event is perforation of the aorta by a protruding right atrial wire, which to the best of our knowledge has been described in only 3 prior case reports.1–3 Moreover, there is no evidence in the medical literature of this sequela after the implantation of a cardiac resynchronization therapy defibrillator.
Case Report
We describe the case of a 54-year-old man who presented with idiopathic dilated cardiomyopathy, left ventricular ejection fraction of 0.32, end-diastolic volume of 356 mL, severe functional mitral regurgitation, pulmonary artery systolic pressure of 63 mmHg, and severe dilation of both atria (minor axis of right atrium, 62 mm). The patient was in New York Heart Association (NYHA) functional class III and had complete left bundle branch block. He was scheduled for the implantation of a cardiac resynchronization therapy defibrillator.
We implanted an active-fixation OptiSense® 1999/52 Pacing Lead (St. Jude Medical, Inc.; St. Paul, Minn) in the right atrium, an active-fixation lead in the right ventricle, and a passive-fixation lead in the coronary sinus. The procedure was uncomplicated, and the patient was stable and asymptomatic at the end of it.
Six hours later, the patient reported the sudden onset of chest pain and profound dizziness. He was found to be pale, diaphoretic, and severely hypotensive (systolic blood pressure, 60 mmHg). An urgent echocardiogram showed severe pericardial effusion with signs of cardiac tamponade. Because of his hemodynamic instability, the patient underwent immediate sternotomy and a severe hemopericardium was drained. Inspection of the mediastinal space showed that the outflow of bright red blood arose from a very small perforation of the aortic root, in the region of the noncoronary sinus of Valsalva—just in front of a protruding right atrial pacemaker wire. This aortic ulcer was caused by mechanical friction from the atrial lead. We also observed a small erosion of the atrial wall, without active bleeding from the right atrium, and we could palpate the helix of the right atrial lead that protruded from the right atrium (Fig. 1). Thorough inspection of the pericardium and the 2 ventricular leads revealed no other bleeding sites. After extracorporeal circulation was established, both the aortic and atrial punctures were repaired with Prolene sutures reinforced by Teflon pled-gets (Fig. 2). Together with suturing the atrial puncture, we plicated the atrial wall above the atrial lead in order to cover the tip of the lead and prevent further damage to the atrial or aortic wall. There was no need to reposition the atrial lead, because it functioned correctly.
Fig. 1.
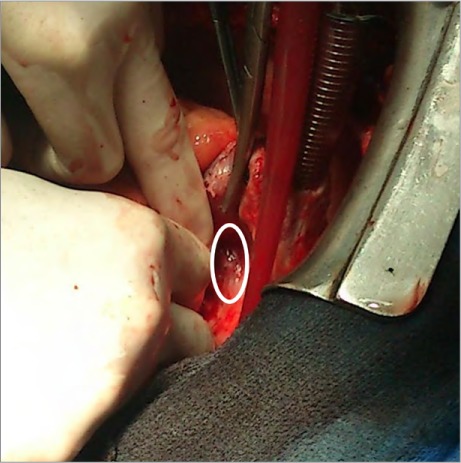
Intraoperative photograph shows the small puncture of the atrial wall caused by the helix of the atrial active-fixation lead (within the circle). Right atrial cannulation for extracorporeal circulation is also shown.
Fig. 2.
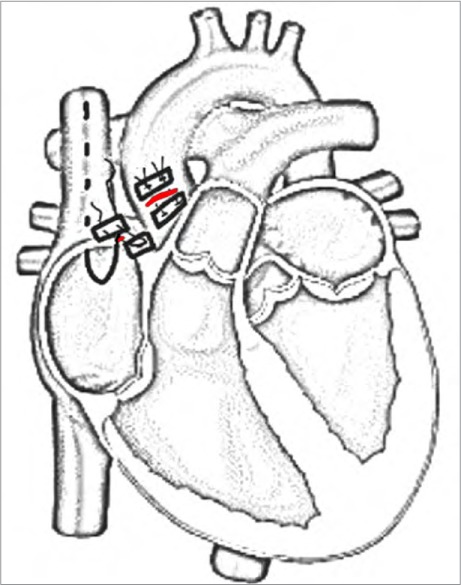
Anatomic sketch shows the close relationship between the atrial lead and the aorta. Note also the lesions (red) of the atrial and aortic walls and the Prolene sutures reinforced by Teflon pledgets, which were used to repair both wounds.
The patient's postoperative course was complicated by heart failure due to atrial fibrillation with rapid ventricular response, which required cardioversion; the patient was discharged from the hospital 30 days later in NYHA functional class II. Before that discharge, atrial lead function and position were checked and no abnormalities were found.
Discussion
Cardiac perforation associated with pacemaker or defibrillator implantation is a known occurrence that usually does not result in major sequelae; notwithstanding, cardiac tamponade can occur. Thoracic pain and hemodynamic instability after device implantation should always raise the clinical suspicion of tamponade, together with the possibility of aortic perforation.
Aortic perforation by a pacemaker lead is a very rare and life-threatening event. In the reports published up to the present time, its clinical presentation always took the form of cardiac tamponade. Immediate surgery is mandatory to diagnose and treat this severe sequela. In our patient, aortic perforation was undoubtedly due to the pacing lead's puncturing the right atrial wall and injuring the adjacent ascending aorta by mechanical friction. Moreover, this result was probably abetted by the severe dilation of the right atrium and by the increased right atrial pressure associated with the patient's advanced stage of heart failure.
Footnotes
*Although “complication” and “sequela” are often used interchangeably by physicians, it is useful to retain the distinction that a complication is a simultaneously existing condition aggravated by the primary condition or its treatment, whereas a sequela is a new condition caused by the primary condition or its treatment. – Ed.
References
- 1.Sticco CC, Barrett LO. Delayed cardiac tamponade by iatrogenic aortic perforation with pacemaker implantation. J Thorac Cardiovasc Surg. 2006;131(2):480–1. doi: 10.1016/j.jtcvs.2005.08.060. [DOI] [PubMed] [Google Scholar]
- 2.Kashani A, Mehdirad A, Fredman C, Barold SS. Aortic perforation by active-fixation atrial pacing lead. Pacing Clin Electrophysiol. 2004;27(3):417–8. doi: 10.1111/j.1540-8159.2004.00456.x. [DOI] [PubMed] [Google Scholar]
- 3.Kaljusto ML, Tonnessen T. Aortic perforation with cardiac tamponade two weeks after pacemaker implantation. J Thorac Cardiovasc Surg. 2007;134(2):502–3. doi: 10.1016/j.jtcvs.2007.03.037. [DOI] [PubMed] [Google Scholar]


