Abstract
Objective
To examine the hypothesis that the influence of physical activity capacity on participation is mediated through activity performance.
Design
Secondary analysis of a prospective cross-sectional study sample.
Setting
Regional pediatric specialty care hospital.
Participants
Children (N = 128; 59% boys; age range, 2–9y) with cerebral palsy with Gross Motor Function Classification System levels I to III; 49% had hemiplegia, and 72% had spasticity.
Interventions
Not applicable.
Main Outcome Measures
Activity capacity was measured with the Gross Motor Function Measure-66, performance was measured with the Activities Scale for Kids, and participation was measured with the Assessment of Life Habits. Children’s Assessment of Participation and Enjoyment and the Assessment of Preschool Children’s Participation assessed diversity participation. Regression equations and Sobel z test were used to examine the mediated effect via performance.
Results
Physical activity performance mediates 74.9% (β=.83, P<.001) of the effect of activity capacity on total participation levels and 52.8% (β=.47, P=.001) of the effect of capacity on diversity participation.
Conclusions
The relation between what an ambulatory child with cerebral palsy is able to perform in a clinical setting and their participation in life is significantly mediated by what they actually do motorically in day-to-day life. Results suggest that interventions focusing on improving what they actually do every day, regardless of their capacity to perform (what they can do when tested), may positively influence participation.
Keywords: Cerebral palsy, Motor activity, Rehabilitation
Discussions of assessment, goal setting, and treatment within pediatric disability are increasingly being framed within the International Classification of Functioning, Disability and Health (ICF) model (fig 1).1,2 Dynamic reciprocal relations between the levels of function (body function/structure, activity, participation) and contextual factors (personal, environmental) are proposed in the ICF. However, there is limited empirical testing of these relations. Application of the ICF framework in the context of therapy goals and intervention is difficult without an understanding of the relations among the qualifiers, domains, and contextual factors. For example, if walking skill improves in a clinical setting (activity capacity), to what extent does day-to-day walking change (activity performance)? Does this change in walking performance subsequently influence the child’s ability to participate in activities of daily life, such as walking to the school bus (participation), within context of the individual body function/structure, personal, and environmental factors of that child and family?
Fig 1.
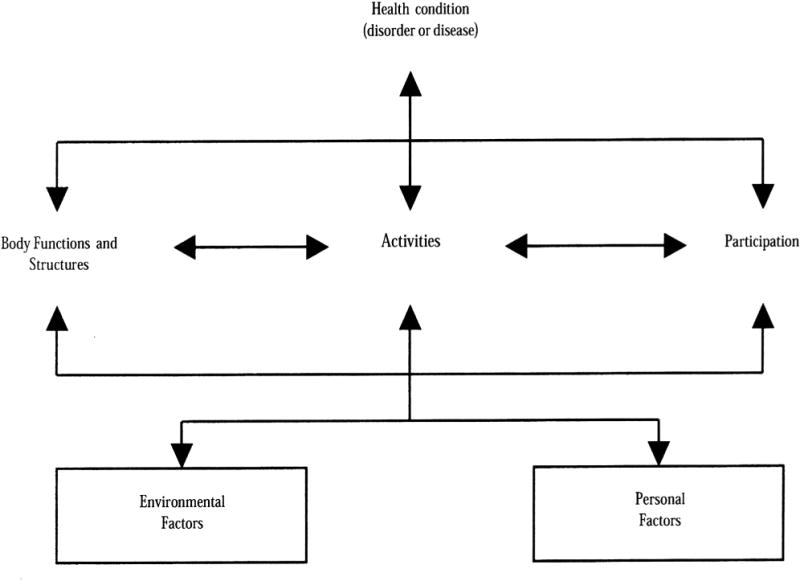
ICF (adapted from World Health Organization. Towards a Common Language for Functioning, Disability and Health: ICF. Geneva: World Health Organization; 2002.).
From the ICF perspective, activity is defined as the execution of a task or action by an individual, whereas participation is considered involvement in a life situation or habits of daily life in a social context. The domain of activity can be separately measured through the qualifiers of capacity and performance. Capacity is the execution of a task in a controlled environment, such as the standardized gross motor function tests administered by clinicians and therapists in the clinic. These measures tell us what a child can do or is capable of doing when asked to perform in a structured or idealized clinical setting. Performance is the execution of a task in the natural environment, or what the child really does when out on the playground at school, at home, or in the community.2 Activity, as defined by the ICF, is included in the most recently published definition of cerebral palsy (CP): a group of disorders of the development of movement and posture, causing activity limitations that are attributed to non-progressive disturbances that occurred in the developing fetal or infant brain.3
Prior evidence has established the strong negative association between capacity and participation (both quantity and diversity). In studies4,5,8 of school-based activity performance and participation in Israel, children with CP had significantly lower physical activity performance, as measured by the School Function Assessment. Children with CP and lower activity performance participated significantly less often than their typically developing peers in daily school activities (ie, playground games and moving to other areas of the school).4 Motor function has also been shown to be predictive of less participation in mobility, education, and social relations for children with CP.5 Morris et al,6 using the family reported Lifestyle Assessment Questionnaire, demonstrated that movement, manual, and intellectual abilities predicted physical independence, but other domains of activity and participation did not. Voorman et al7 described the activity and participation of 100 children with CP (age range, 9–13y) across all Gross Motor Function Classification System (GMFCS) levels. Mobility performance level, as defined by the GMFCS, was strongly associated with self-care and domestic life activities and participation.
The diversity of participation in daily life for children with CP was described by Imms et al8 with the Children’s Assessment of Participation and Enjoyment (CAPE). Children with CP participated in a broad range of diverse activities, but with lower participation in formal compared with informal activities. Diversity was the lowest for skill-based and active physical activities. Children with quadriplegia participated in fewer activities with less intensity than other topographic groups. Children with spastic diplegia CP have limitations in upright mobility skills, are physically less active, and walk fewer steps each day.9,10 These activity limitations appear to restrict day-to-day participation in education, social relations, and mobility.
Jette et al11 documented activity and participation as distinct dimensions, as proposed by the ICF framework, within a cross-sectional survey of 150 community-dwelling adults ≥60 years. Kerr et al12 described the relation between walking energy efficiency (body structure/function) and measures of activity limitation, participation restriction, and health status in a longitudinal study of 184 ambulatory children with CP between 4 and 17 years of age. Energy efficiency with walking was significantly related to clinic-based activity limitations but not to daily life participation and health status. Clinic-assessed measures of energy efficiency were correlated with clinic-assessed measures of activity but were not correlated with those of community life experiences or participation. The absence of a relation with daily life experiences (participation) may be because of the measurement of energy consumption within a clinical setting versus the community. The relations between body functions and structure, activity, and participation within a botulinum toxin intervention trial for children with CP was examined by Wright et al.13 The Gross Motor Function Measure (GMFM) and Pediatric Evaluation of Disability Inventory were used to describe activity levels, whereas the Pediatric Outcome Database Collection Instrument characterized participation in daily life. Baseline relations between these measures were moderate to strong, whereas the change scores relations were no more than fair.
Presently, mobility interventions for children with CP focus on the body/function structure or activity capacity levels of the ICF. It is proposed that enhanced activity (usually measured by capacity) will have the desired outcome of higher levels and diversity of participation in daily life. These interventions have varying levels of cost, burden to the family, and invasiveness (eg, orthoses, botulinum toxin injections, body-weight-supported or robotic treadmill training, and orthopedic or neurosurgery). A better understanding of the relation between activity capacity and performance and participation in the habits of day-to-day life in ambulatory children with CP is needed. As room for improvement in activity capacity is often limited in children with CP, we hypothesize that improving performance, even within the limits of their capacity, would have significant positive impact on their participation in life. Such knowledge has the potential to inform more cost-effective rehabilitation strategies and intervention research to optimize the day-to-day life experience of ambulatory children with CP. Thus, we examined the hypothesis that the relation between what ambulatory children with CP are able or capable of doing in a structured environment or clinical setting (activity capacity) and completion of the habits of daily life (participation) is mediated through what they really do regularly (activity performance). We also explored whether the influence of walking skills in a clinical setting (walking capacity) on mobility-related life habits (participation) is mediated through the actual walking levels (activity performance) in day-to-day life.
Methods
The research protocol was approved by the Seattle Children’s Institutional Review Board. Directed approach letters were mailed from 2 specialty care pediatric facilities in the Pacific Northwest United States to potential participants and their families. Inclusion criteria were (1) 2 to < 10 years of age, (2) diagnosis of CP, and (3) GMFCS levels of I to III. Exclusion criteria included (1) lower extremity botulinum toxin injections in the last 3 months, (2) visual impairment-limiting physical activity levels per parental/therapist report, (3) uncontrolled seizure disorder impacting mobility skills, and (4) orthopedic or neurosurgery in the last 6 months. Once informed consent was obtained, measures of walking and physical activity capacity, performance, and participation were collected within a larger cross-sectional descriptive project examining the relation between walking activity performance and participation. Demographic information was collected by interview of the parent with GMFCS level confirmed by in-person observation of motor skills by the first author during a single research visit. The anthropometric measurements of triceps and subscapular skinfolds, knee height, and weight were collected to calculate the height-adjusted lean mass using techniques and algorithms validated for children with CP.14–17 Triceps and subscapular skinfold thicknesses were used to determine percent body fat with corrections for CP. Reported as kilograms per centimeter, height-adjusted lean mass was then calculated as (100 − percent body fat × weight) ÷ by knee segment height.
The Gross Motor Function Measure-66-Item Set (GMFM-66-IS) was administered by the first author to measure physical activity capacity.18 The GMFM-66-IS was developed to allow valid measurement of the GMFM-66 score from a subset of items, thus decreasing the burden of administering all 66 items. Three decision items were used to determine which of the 4 item sets to administer with the GMFM-66 score then calculated using the Gross Motor Ability Estimator software.19 Walking activity capacity was examined with the 1-minute walk test (1MWT),20,21 and was chosen to ensure that walking capacity could be obtained across all ambulatory GMFCS levels. The 1MWT was performed on a flat, nonslippery surface over a 10-m oval track. Children were instructed to walk around the oval track as fast as they could (no running) for 1 minute. The number of meters walked in 1 minute was recorded to the nearest meter.
Physical activity performance was sampled by parental report of the Activity Scale for Kids. The Activity Scale for Kids is a self- and parental-report measure of childhood physical performance for children ages 5 to 15 years.22 The Activity Scale for Kids, performance version–30 items (ASKp-30) was developed to query what a child usually does, taking into account day-to-day life experiences and the environment in which the child has functioned over the past 7 days. The ASKp-30 was completed by the parents after their child had worn a StepWatch monitora for 7 days, per the protocol of a larger study, and returned to the investigators by mail. The ASKp-30 total summary score and locomotion subdomain score were computed to sample physical activity and walking performance, respectively.
Participation in daily life was quantified by parental report of 2 valid measures of pediatric participation: the CAPE and the Assessment of Life Habits (LIFE-H) for children.23,24 These 2 measures were chosen because they were developed from different theoretical models, were validated with different methodology, and measure participation from complementary perspectives. The CAPE was designed to document the intensity and diversity of participation in day-to-day activities, whereas the LIFE-H for children is intended to describe the accomplishment of a group of life habits that are characteristic of children in their environment (home, school, and neighborhood).
The CAPE is a 55-item questionnaire designed to examine how children and young adults (ages 6–21y) participate in everyday activities outside of the school setting.25 Participation is documented across 5 dimensions, including diversity (number of activities done), intensity (frequency of participation measured as a function of the number of possible activities within a category), and enjoyment of activities. The CAPE was administered via interview format by the first author to the child (as able) and parent at the same time. Participants age <6 years had the Assessment of Preschool Children’s Participation (APCP) completed by their parents.26,27 Overall diversity and intensity of participation were sampled with the CAPE or APCP total scores. In order to examine locomotor-related participation, the active physical activity type intensity score was calculated.
The LIFE-H for children was designed and validated to assess the social participation of children with disabilities with versions for parental report of children ages 0 to 4 years and 5 to 13 years.23 The LIFE-H for children was developed from the disability creation process model, which proposes that the accomplishment of life habits is an interaction of individual identities, choices, impairment of body organs, abilities, disabilities, and the characteristics of the environment in which we live. For this analysis, the total, mobility, and fitness categories of the LIFE-H for children were examined to capture overall physical activity and life habits related to locomotor-related participation. Each question was scored relative to the level of accomplishment and type of assistance with a weighted single score from 0 to 9. Parents completed the appropriate LIFE-H for children based on the chronological age of the child at the research visit.
Statistical analysis
We used means and SDs to summarize continuous variables, counts, and frequencies of categorical variables. Following the framework of Baron and Kenny,28 we applied regression equations to estimate and examine how the effect of activity capacity on life participation was mediated by performance, as depicted in the following equations:
Participation ~c Capacity+β Covariates
Participation ~c′ Capacity + b Performance + β Covariates
Performance~a Capacity + β Covariates
Under this framework, the product of the a and b parameters, ab, is the mediated effect, sometimes also referred to as the indirect effect. The estimated mediated effect using Sobel z test.29 Age, sex, GMFCS level, and body composition (ratio of lean body mass/knee height) were included as covariates in the previous regression equations. Participation or accomplishment of life habits was measured with the LIFE-H for children total, mobility, and fitness scores. The CAPE/APCP total intensity and diversity scores documented intensity and diversity of participation. For activity capacity we collected the GMFM-66-IS total scores, and for walking capacity we used the 1MWT. The ASKp-30 summary and locomotion subscales represented activity and walking performance in day-to-day life. The mediation analyses and other statistical analyses were conducted using SPSS version 17.0.b
Results
A direct mail or personal approach by health care providers was completed for 686 potential participants previously screened for ambulatory CP and age. Of the 214 eligible participants, 128 children with CP completed the study protocol (fig 2, table 1). Five enrolled participants did not complete data collection, with 4 monitors unreturned. The study sample had an average age of 6.2 years (range, 2.2–9.9y; 82% white; 41% women). GMFCS levels I, II, and III were represented by 44, 54, and 30 participants, respectively, and were primarily spastic (72%). Topographically, 49% had unilateral involvement or hemiplegia, with 36% having diplegia. Communication abilities of the sample, as measured by the Communication Function Classification System,30 were primarily level I (57%), with fine motor skills classified with the Manual Abilities Classifications System,31 and predominately level II (45%). Home ownership was reported by 73% of the parents, and 31% of the mothers had attended vocational school or some college.
Fig 2.

Summary of the recruitment of participants.
Table 1.
Combined sample characteristics (N = 128)
| Characteristic | Value |
|---|---|
| Age | 6.2±2.3 (2.2–9.9) |
| Age group | |
| 2–3y | 24 (19) |
| 4–5y | 34 (27) |
| 6–7y | 39 (30) |
| 8–9y | 31 (24) |
| Sex, female | 52 (41) |
| GMFCS | |
| Level I | 44 (35) |
| Level II | 54 (42) |
| Level III | 30 (23 |
| Topography of CP | |
| Diplegia | 46 (36) |
| Hemiplegia | 63 (49) |
| Quadriplegia | 12 (9) |
| Triplegia | 6 (5) |
| Monoplegia | 1 (1) |
| Primary movement disorder | |
| Spasticity | 91 (72) |
| Dystonia | 8 (6) |
| Mixed | 13 (10) |
| Ataxia | 3 (2) |
| Hypotonia/low tone | 12 (10) |
| Manual Abilities Classification System | |
| Level I | 46 (36) |
| Level II | 58 (45) |
| Level III | 24 (19) |
| Communication Function Classification System | |
| Level I | 73 (57) |
| Level II | 25 (20) |
| Level III | 18 (14) |
| Level IV | 12 (9) |
| Hispanic | 19 (15) |
| Race | |
| White | 105 (82) |
| Black | 5 (4) |
| Asian/Pacific Islander | 10 (8) |
| Native American | 2 (2) |
| Mixed | 3 (2) |
| Other | 3 (2) |
| Parental characteristics | |
| Maternal vocational school/some college | 39 (31) |
| Home ownership | 94 (73) |
NOTE. Values are mean ± SD (range) or n (%).
The mediation analysis examining the direct and indirect effects via what they are capable of doing physically in a structured test situation (capacity) and what a child actually does (performance) to overall accomplishment, diversity, and intensity of daily life habits (participation) is summarized in Table 2. Approximately 75% of the total effect of what a child is capable of doing in a clinical setting (activity capacity, GMFM-66-IS) on accomplishment of total daily life habits (participation) levels, as measured by the LIFE-H total score, was mediated by what he or she actually does (activity performance, ASKp-30 total score) (fig 3). For diversity of daily life habits accomplished (participation, CAPE/APCP total diversity), what a child actually does in day-to-day life (activity performance) mediates 52.8% ( =.47, P=.001) of the total effect of what he or she is capable of doing in a structured setting or clinic (capacity). What a child actually does (activity performance) mediates 94.5% ( =.32, P=.03) of the total effect of his or her gross motor performance in a clinical setting (GMFM-66-IS) on the intensity of daily life habits (participation, CAPE/APCP total intensity).
Table 2.
Direct and indirect effects of variables testing whether physical activity performance mediates the relationship of physical activity capacity to overall total, diversity, and intensity of participation
| Dependent Variables | Predictor Variables | c (P) | c′ (P) | ab (P) | R2 | % Mediated Effect |
|---|---|---|---|---|---|---|
| Total | GMFM-66-IS | .66 (<.001) | .43 | |||
| ASKp-30 | GMFM-66-IS | .59 (<.001) | .69 | |||
| Total | GMFM-66-IS and ASKp-30 | .13 (.22) | .83 (<.001) | .66 | 74.9 | |
| Diversity | GMFM-66-IS | .52 (<.001) | .21 | |||
| ASKp-30 | GMFM-66-IS | .59 (<.001) | .69 | |||
| Diversity | GMFM-66-IS and ASKp-30 | .24 (.13) | .47 (.001) | .27 | 52.8 | |
| Intensity | GMFM-66-IS | .19 (.170) | .24 | |||
| ASKp-30 | GMFM-66-IS | .56 (<.001) | .69 | |||
| Intensity | GMFM-66-IS and ASKp-30 | .02 (.99) | .32 (.030) | .26 | 94.5 |
NOTE. Model controlled for the confounders of age, sex, GMFCS level, and ratio of lean body mass/knee height.
Physical activity capacity = GMFM-66-IS Total
Physical Activity Performance = Activities Scale for Kids (ASKp-30).
Abbreviations: Diversity, CAPE total diversity score; Intensity, CAPE total intensity score; Total, LIFE-H total weighted score.
Fig 3.
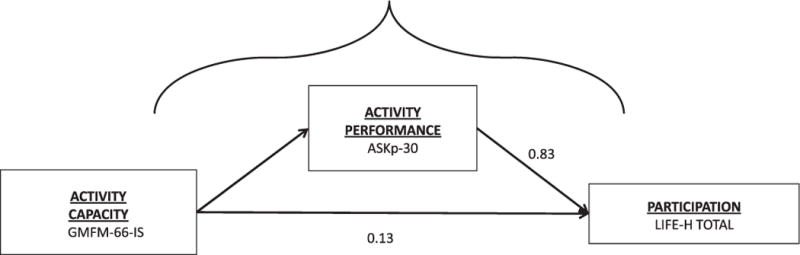
Relationship of physical activity capacity and performance to total participation levels. Of the total effect of capacity on participation, 74.9% was mediated through performance (direct effect: β=.13, mediation effect: β=.83).
Table 3 displays the direct and indirect effects of walking skill in a clinical testing environment (walking capacity) on daily locomotor life habits (participation, LIFE-H fitness and mobility, CAPE/APCP active physical). Actual walking activity in daily life (walking performance, ASKp-30 locomotor) mediates 44% ( =.35, P=.001) of the total effect of the distance walked at a self-selected rate in a clinical setting (walking capacity, 1MWT) on accomplishment of life habits, such as getting in/out of bed, sleeping, physical activity to maintain fitness, and relaxing quiet activities (fitness LIFE-H category). For life habits related to mobility (ie, moving around on sidewalks/streets, riding a bike or passenger in a vehicle), the walking a child really does in day-to-day life (walking performance) mediates 51.5% ( =.50, P<.001) of the total effect of the walking distance exhibited during a clinical test (walking capacity, 1MWT). However, the walking a child really does in day-to-day life (walking performance) does not appear to significantly mediate the effect of the walking he or she can do in a test environment (walking capacity, 2.2%, =.02, P=.90) on intensity of active physical life habits (CAPE, active physical intensity).
Table 3.
Direct and indirect effects of variables testing whether walking activity performance mediates the relationship of walking capacity to locomotion in daily life (fitness, mobility, and active physical activity)
| Dependent Variables | Predictor Variables | c (P) | c′ (P) | ab (P) | R2 | % Mediated Effect |
|---|---|---|---|---|---|---|
| Fitness | 1MWT | .27 (.009) | .29 | |||
| ASKp-30-Loco | 1MWT | .34 (<.001) | .51 | |||
| Fitness | 1MWT and ASKp-30-Loco | .15 (.15) | .35 (.001) | .35 | 44.0 | |
| Mobility | 1MWT | .33 (.002) | .33 | |||
| ASKp-30-Loco | 1MWT | .34 (<.001) | .51 | |||
| Mobility | 1MWT and ASKp-30-Loco | .15 (.10) | .50 (<.001) | .45 | 51.5 | |
| ActPhys | 1MWT | .33 (.001) | .33 | |||
| ASKp-30-Loco | 1MWT | .32 (<.001) | .54 | |||
| ActPhys | 1MWT and ASKp-30-Loco | .21 (.08) | .02 (.900) | .22 | 2.2 |
NOTE. The model controlled for the confounders of age, sex, GMFCS level, and ratio of lean body mass/knee height.
Walking Capacity = 1MWT, Walking Activity Performance = Activities Scale for Kids (ASKp-30).
Abbreviations: ActPhys, CAPE active physical intensity; ASKp-30-Loco, Activities Scale for Kids-locomotor subscale; Fitness, LIFE-H fitness category; Mobility, LIFE-H mobility category.
Discussion
To our knowledge, this is the first article to examine the relative relations between the ICF activity domain qualifiers of capacity and performance and participation in ambulatory children with CP. The effect of what gross motor skills a child can perform in a structured/clinical setting (activity capacity) on overall frequency and diversity of participation in ambulatory children with CP is significantly mediated through what they really do in day-to-day life (activity performance). Similarly, the effect of walking capacity on life habits related to getting around the environment, maintaining physical fitness, and sleep in daily life (mobility and fitness participation) is mediated by their actual day-to-day walking performance. In contrast, walking performance does not appear to mediate the relation between walking capacity and intensity of participation in daily activities that require active gross motor skills. This conflicting finding may be a function of differing measures of intensity of participation (CAPE vs LIFE-H).
Previous research has confirmed the relation between activity capacity and measures of participation in children with CP. Ostensjo et al32 reported a strong relation between GMFM-66 and the Pediatric Evaluation of Disability Inventory functional skills. Similarly, Smits et al33 documented that the GMFM-66 scores explained 90% and 84%, respectively, of the variance of Pediatric Evaluation of Disability Inventory functional skills and caregiver assistance scales in 116 children with CP across all GMFCS levels. The mediation analysis presented here suggests that for ambulatory children the relation between activity capacity (what they do in a structured setting) and day-to-day participation is mediated largely through activity performance (what a child actually does in day-to-day life). This has implications for the development and testing of strategies to enhance the participation and physical activity in daily life of children with CP. Based on these findings, rehabilitation strategies tested and implemented within the personal and environmental context of a patient’s daily life (activity performance) may have greater influence on their participation in life. Outcomes to document effectiveness should also include performance-based outcomes, thus capturing what a patient actually does in daily life.
Cost-effective and translatable public health strategies used to enhance physical activity and overall health in the general population have yet to be examined in persons with physical disability. For example, would a daily walking program for children with CP (similar to the 10,000 steps per day for optimal health in adults without disability34) enhance overall activity and participation better than a clinic-based treadmill program? Likewise, embracing the bidirectionality of the ICF component relations, increased opportunities to participate in physical activities (participation) or accessible playgrounds, adaptive sports equipment (environment), endurance/strength (body structure/function), and desire to be active (personal factors) all may influence overall activity performance.
These results suggest that interventions should focus on what a child actually does motorically (performance) in day-to-day life regardless of what he or she is capable of performing in a structured testing environment/clinic (capacity levels) to positively influence participation. This may be analogous to athletic training programs of runners. Although resistive exercise, treadmill, and/or stationary biking are important aspects of the training, actual mileage road running is essential to achieve best outcomes in a road race. Thus, strategies to enhance daily walking performance of children using assistive devices while at school may also then enhance their ability to participate in recreational sports outside of the school setting. Meaningful, valid, and sensitive measures of activity performance (what they really do) and participation (life habits) within day-to-day life are needed. Knowledge generated from this project lays the conceptual groundwork for the refinement of current knowledge. For example, previous interventions found to be ineffective with clinic-based outcomes (capacity level) may have potential intervention effect when examined with outcomes which sample what they really do in day-to-day life (performance) and/or may have potential effect on the ability to live the kind of life they want (participation).
Study limitations
A limitation is that the analysis presented here only examined ambulatory children at 1 point in time. These relations may differ relative to developmental age, diagnosis, mobility, and functional mobility status (ie, independent walker, nonwalker). This work needs to be replicated longitudinally and in association with interventions. A measurement limitation is that the ASKp-30 has not been validated for parental report of children <5 years of age. The walking capacity to performance mediation analysis should be interpreted with caution because the ASKp-30 locomotor subscale is composed of only 7 items and has not been confirmed as a unique construct psychometrically.
Conclusions
Further exploration of how all the ICF components/factors interact is needed. The recent examination of some of the ICF component relations at population level by Colver et al35 builds the foundation for clinical translation of this knowledge to support children with CP and their families.36 Verschuren et al37 have also identified various key personal and environmental factors that influence the level of participation in physical activity for children with CP in a qualitative investigation. This knowledge has the potential to support the development of novel rehabilitation strategies that are not based on traditional approaches of changing the body structure/function of the child but are directed toward the potentially modifiable ICF components of activity performance, participation, environment, and personal factors.
Acknowledgments
Supported by the National Institutes of Health (grant no. K23 HD060764) and the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health (grant no. UL1RR025014).
List of abbreviations
- APCP
Assessment of Preschool Children’s Participation
- ASKp-30
Activity Scale for Kids, performance version–30 items
- CAPE
Children’s Assessment of Participation and Enjoyment
- CP
cerebral palsy
- GMFCS
Gross Motor Function Classification System
- GMFM
Gross Motor Function Measure
- GMFM-66-IS
Gross Motor Function Measure-66 Item Set
- ICF
International Classification of Functioning, Disability and Health
- LIFE-H
Assessment of Life Habits
- 1MWT
1-minute walk test
Footnotes
Presented to the American Academy of Cerebral Palsy and Developmental Medicine, September 13, 2012, Toronto, ON, Canada; and International Cerebral Palsy Conference, October 10, 2012, Pisa, Italy.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Clinical Trial Registration No.: NCT01217242.
No commercial party having a direct financial interest in the results of the research supporting this article has conferred or will confer a benefit on the authors or on any organization with which the authors are associated.
- StepWatch; Orthocare Innovations, 6405 218 St SW, #301, Mountlake Ter, WA 98043.
- SPSS Inc, 233 S Wacker Dr, 11th Fl, Chicago, IL 60606.
References
- 1.Steiner WA, Ryser L, Huber E, Uebelhart D, Aeschlimann A, Stucki G. Use of the ICF model as a clinical problem-solving tool in physical therapy and rehabilitation medicine. Phys Ther. 2002;82:1098–107. [PubMed] [Google Scholar]
- 2.World Health Organization. International Classification of Functioning, Disability and Health (ICF) Geneva: World Health Organization; 2002. [Google Scholar]
- 3.Rosenbaum P, Paneth N, Leviton A, et al. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl. 2007;109:8–14. [PubMed] [Google Scholar]
- 4.Schenker R, Coster W, Parush S. Participation and activity performance of students with cerebral palsy within the school environment. Disabil Rehabil. 2005;27:539–52. doi: 10.1080/09638280400018437. [DOI] [PubMed] [Google Scholar]
- 5.Beckung E, Hagberg G. Neuroimpairments, activity limitations, and participation restrictions in children with cerebral palsy. Dev Med Child Neurol. 2002;44:309–16. doi: 10.1017/s0012162201002134. [DOI] [PubMed] [Google Scholar]
- 6.Morris C, Kurinczuk JJ, Fitzpatrick R, Rosenbaum PL. Do the abilities of children with cerebral palsy explain their activities and participation? Dev Med Child Neurol. 2006;48:954–61. doi: 10.1017/S0012162206002106. [DOI] [PubMed] [Google Scholar]
- 7.Voorman JM, Dallmeijer AJ, Schuengel C, Knol DL, Lankhorst G, Becher JG. Activities and participation of 9- to 13-year-old children with cerebral palsy. Clin Rehabil. 2006;20:937–48. doi: 10.1177/0269215506069673. [DOI] [PubMed] [Google Scholar]
- 8.Imms C, Reilly S, Carlin J, Dodd K. Diversity of participation in children with cerebral palsy. Dev Med Child Neurol. 2008;50:363–9. doi: 10.1111/j.1469-8749.2008.02051.x. [DOI] [PubMed] [Google Scholar]
- 9.van den Berg-Emons HJ, Saris WH, de Barbanson DC, Westerterp KR, Huson A, van Baak MA. Daily physical activity of schoolchildren with spastic diplegia and of healthy control subjects. J Pediatr. 1995;127:578–84. doi: 10.1016/s0022-3476(95)70115-x. [DOI] [PubMed] [Google Scholar]
- 10.Bjornson KF, Belza B, Kartin D, Logsdon R, McLaughlin JF. Ambulatory physical activity performance in youth with cerebral palsy and youth who are developing typically. Phys Ther. 2007;87:248–57. doi: 10.2522/ptj.20060157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jette AM, Haley SM, Kooyoomajian JT. Are the ICF activity and participation dimensions distinct? J Rehabil Med. 2003;35:145–9. doi: 10.1080/16501970310010501. [DOI] [PubMed] [Google Scholar]
- 12.Kerr C, Parkes J, Stevenson M, Cosgrove AP, McDowell BC. Energy efficiency in gait, activity, participation and health status in children wtih cerebral palsy. Dev Med Child Neurol. 2008;50:204–10. doi: 10.1111/j.1469-8749.2008.02030.x. [DOI] [PubMed] [Google Scholar]
- 13.Wright FV, Rosenbaum PL, Goldsmith CH, Law M, Fehlings D. How do changes in body functions and structures, activity and participation relate in children with cerebral palsy? Dev Med Child Neurol. 2008;50:283–9. doi: 10.1111/j.1469-8749.2008.02037.x. [DOI] [PubMed] [Google Scholar]
- 14.Stevenson R, Conaway M, Chumlea C, et al. Growth and health in children with moderate-to-severe cerebral palsy. Pediatrics. 2006;118:1010–8. doi: 10.1542/peds.2006-0298. [DOI] [PubMed] [Google Scholar]
- 15.Gurka MJ, Kuperminc MN, Busby MG, et al. Assessment and correction of skinfold thickness equations in estimating body fat in children with cerebral palsy. Dev Med Child Neurol. 2010;52:e35–41. doi: 10.1111/j.1469-8749.2009.03474.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Spender QW, Cronk CE, Charney EB. Assessment of linear growth of children in cerebral palsy. Dev Med Child Neurol. 1989;31:206–14. doi: 10.1111/j.1469-8749.1989.tb03980.x. [DOI] [PubMed] [Google Scholar]
- 17.Stevenson R. Measurement of growth in children with developmental disabilities. Dev Med Child Neurol. 1996;38:855–60. doi: 10.1111/j.1469-8749.1996.tb15121.x. [DOI] [PubMed] [Google Scholar]
- 18.Russell DJ, Avery LM, Walter SD, et al. Development and validation of item sets to improve efficiency of administration of the 66-item Gross Motor Function Measure in children with cerebral palsy. Dev Med Child Neurol. 2010;52:e48–54. doi: 10.1111/j.1469-8749.2009.03481.x. [DOI] [PubMed] [Google Scholar]
- 19.Russell D, Rosenbaum P, Avery L, Lane M. Gross Motor Function Measure (GMFM-66 and GMFM-88) User’s manual. 2002 [Google Scholar]
- 20.Wade DT. Measurement in neurological rehabilitation. Oxford: Oxford Univ Pr; 1992. Timed walking tests. [Google Scholar]
- 21.Scholtes VA, Dallmeijer AJ, Rameckers EA, Verschuren O, Tempelaars E, Hensen M. Lower limb strength training in children with cerebral palsy–a randomized controlled trial protocol for functional strength training based on progressive resistance exercise principles. BMC Pediatr. 2008;8:41. doi: 10.1186/1471-2431-8-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Young N, Williams JI, Yoshida KK, Wright JG. Measurement properties of the Activities Scale for Kids. J Clin Epidemiol. 2000;53:125–37. doi: 10.1016/s0895-4356(99)00113-4. [DOI] [PubMed] [Google Scholar]
- 23.Noreau L, Lepage C, Boissiere L, et al. Measuring participation in children with disabilities using the Assessment of Life Habits. Dev Med Child Neurol. 2007;49:666–71. doi: 10.1111/j.1469-8749.2007.00666.x. [DOI] [PubMed] [Google Scholar]
- 24.King G, Law M, King SM, et al. CAPE/PAC Children’s Assessment of Participation and Enjoyment & Preferences for Activities of Children. San Antonio: PsychCorp; 2004. [Google Scholar]
- 25.King GA, Law M, King S, Hurley P, Hanna S, Kertoy M. Measuring children’s participation in recreation and leisure activities: construct validation of the CAPE and PAC. Child Care Health Dev. 2007;33:28–39. doi: 10.1111/j.1365-2214.2006.00613.x. [DOI] [PubMed] [Google Scholar]
- 26.Law M, King G, Petrenchik T, Kertoy M, Anaby D. The assessment of preschool children’s participation: internal consistency and construct validity. Phys Occup Ther Pediatr. 2012;32:272–87. doi: 10.3109/01942638.2012.662584. [DOI] [PubMed] [Google Scholar]
- 27.Coster W, Law M, Bedell G, Khetani M, Cousins M, Teplicky R. Development of the participation and environment measure for children and youth: conceptual basis. Disabil Rehabil. 2012;34:238–46. doi: 10.3109/09638288.2011.603017. [DOI] [PubMed] [Google Scholar]
- 28.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 29.Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. Sociol Methods. 1982;13:290–312. [Google Scholar]
- 30.Hidecker MJ, Paneth N, Rosenbaum PL, et al. Developing and validating the Communication Function Classification System for individuals with cerebral palsy. Dev Med Child Neurol. 2011;53:704–10. doi: 10.1111/j.1469-8749.2011.03996.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Eliasson AC, Krumlinde-Sundholm L, Rösblad B, et al. The Manual Ability Classification System (MACS) for children with cerebral palsy: scale development and evidence of validity and reliability. Dev Med Child Neurol. 2006;48:549–54. doi: 10.1017/S0012162206001162. [DOI] [PubMed] [Google Scholar]
- 32.Ostensjo S, Brogren E, Vollestad NK. Motor impairments in young children with cerebral palsy: relationship to gross motor function and everyday activities. Dev Med Child Neurol. 2004;46:580–9. doi: 10.1017/s0012162204000994. [DOI] [PubMed] [Google Scholar]
- 33.Smits DW, Gorter JW, Ketelaar M, et al. Relationship between gross motor capacity and daily-life mobility in children with cerebral palsy. Dev Med Child Neurol. 2010;52:e60–6. doi: 10.1111/j.1469-8749.2009.03525.x. [DOI] [PubMed] [Google Scholar]
- 34.Tudor-Locke C, Bassett DR., Jr How many steps/day are enough? Preliminary pedometer indices for public health. Sports Med. 2004;34:1–8. doi: 10.2165/00007256-200434010-00001. [DOI] [PubMed] [Google Scholar]
- 35.Colver A, Thyen U, Arnaud C, et al. Association between participation in life situations of children with cerebral palsy and their physical, social, and attitudinal environment: a cross-sectional multicenter European study. Arch Phys Med Rehabil. 2012;93:2154–64. doi: 10.1016/j.apmr.2012.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fauconnier J, Dickinson HO, Beckung E, et al. Participation in life situations of 8–12 year old children with cerebral palsy: cross sectional European study. BMJ. 2009;338:b1458. doi: 10.1136/bmj.b1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Verschuren O, Wiart L, Hermans D, Ketelaar M. Identification of facilitators and barriers to physical activity in children and adolescents with cerebral palsy. J Pediatr. 2012;161:488–94. doi: 10.1016/j.jpeds.2012.02.042. [DOI] [PubMed] [Google Scholar]


