Abstract
Background
DNA methyltransferase 3A (DNMT3A) mutations were considered to be independently associated with unfavorable prognosis in adults with de novo acute myeloid leukemia (AML), however, there are still debates on this topic. Here, we aim to further investigate the association between DNMT3A mutations and prognosis of patients with AML.
Methods
Eligible studies were identified from several data bases including PubMed, Embase, Web of Science, ClinicalTrials and the Cochrane Library (up to June 2013). The primary endpoint was overall survival (OS), while relapse-free survival (RFS) and event-free survival (EFS) were chosen as secondary endpoints. If possible, we would pool estimate effects (hazard ratio [HR] with 95% confidence interval[CI]) of outcomes in random and fixed effects models respectively.
Results
That twelve cohort studies with 6377 patients exploring the potential significance of DNMT3A mutations on prognosis were included. Patients with DNMT3A mutations had slightly shorter OS (HR = 1.60; 95% CI, 1.31–1.95; P<0.001), as compared to wild-type carriers. Among the patients younger than 60 years of age, DNMT3A mutations predicted a worse OS (HR = 1.84; 95% CI, 1.36–2.50; P<0.001). In addition, mutant DNMT3A predicted inferior OS (HR = 2.30; 95% CI, 1.78–2.97; P = 0.862) in patients with unfavorable genotype abnormalities. Similar results were also found in some other subgroups. However, no significant prognostic value was found on OS (HR = 1.40; 95% CI, 0.98–1.99; P = 0.798) in the favorable genotype subgroup. Similar results were found on RFS and EFS under different conditions.
Conclusions
DNMT3A mutations have slightly but significantly poor prognostic impact on OS, RFS and EFS of adults with de novo AML in total population and some specific subgroups.
Introduction
Acute myeloid leukemia (AML) are a group of heterogeneous diseases with respect to biological and clinical outcomes, which have been considered to be related to cytogenetic and gene lesions in hematopoietic stem or progenitor cells [1], [2], [3]. It is extremely important for patients with de novo AML to assess risk status based on cytogenetic and molecular abnormalities. Cytogenetic abnormalities have been utilized widely to evaluate the risk status of patients [3], [4], [5], [6]. However, only several molecular lesions were applied to risk stratification in clinical practice, such as FMS-like tyrosine kinase 3 (FLT3) [7], [8], Nucleophosmin1 (NPM1) [9], [10], CCAAT/enhancer-binding protein alpha (CEBPA) [11], [12]. Whereas DNMT3A [13], [14], [15], Isocitrate dehydrogenase1 (IDH1), IDH2 [16], [17] and TET2 [18], [19] have not been fully assessed. DNMT3A plays a role in de novo methylation of specific CpG islands in DNA, and DNMT3A mutations are implicated in the pathogenesis and prognosis of patients with AML [20]. Recurrent abnormities of the gene include missense, frameshift, nonsense, splice-site mutations and part deletion [13] as well. The most common type of missense mutations is predicted to affect the amino acid at R882, which accounts for more than half the population with DNMT3A mutations [13], [21], [22]. These mutations are highly enriched in the group of adults with an intermediate-risk cytogenetic profile or with cytogenetic normal AML (CN-AML) [13], [22], [23], [24], but they are absent or scarce in patients with a favorable-risk cytogenetic profile [21], [23], [24]. DNMT3A mutations having negative impact on OS of patients with AML were reported in several studies but not in the others [20], [22], [25], [26]. Similar discrepancies were observed in terms of RFS and EFS. Thus it is necessary to perform a systematic review and meta-analysis to further clarify the prognostic values of mutant DNMT3A in patients with de novo AML.
Materials and Methods
1 Literature search and search strategy
Literature search was conducted in several electronic databases including PubMed, Embase, Web of Science, ClinicalTrials and the Cochrane Library (up to June 26, 2013). We used the following search terms (medical subject headings [MeSH] or key words) limited in titles and abstracts: “acute myeloid leukemia”, “acute myeloblastic leukemia”, “acute myelocytic leukemia”, “acute granulocytic leukemia”, “Leukemia, Myeloid, Acute”, “AML”, and “DNA methyltransferase 3A”, “DNA (cytosine-5)-methyltransferase 3A”, “DNMT3A”. No other search terms were added in order to obtain more related studies.
2 Selection criteria
If meeting the following selection criteria, studies should be included: (1) studies published in English; (2) Cohort studies or meeting abstracts; (3) studies focusing on prognostic impact of DNMT3A mutations in adults with de novo AML; (4) data from time-to-event analysis in every study; (5) the latest version of multiple publications or overlap of some context from the same cohort should be selected, the older version should be used to clarify methodology or characteristics of patients.
Two investigators (R.-x.T. and T.-s.Z.) were asked to identify the eligible studies independently. Endnote ×6 were used for the management of the articles and for removing most of the duplicates. Unrelated articles and remaining duplicates were excluded by reading the abstracts carefully. The remaining full-text articles were retrieved and reviewed carefully to identify the eligible studies. Any divergency was resolved by asking a third author's opinion (H.-r.F.). The selection process was documented in a flow chart recommended in the PRISMA statement.
3 Risk of bias from included studies
The quality of eligible studies was assessed independently by two reviewers (R.-x.T. and T.-s.Z.) using the Newcastle-Ottawa-Scale (NOS) [27] for cohort studies. The NOS assigns a maximum of 4 points for selection, 2 points for comparability, and 3 points for exposure or outcome. According to the NOS, We classified the qualities of these studies into three groups: high (7–9 points), intermediate (4–6 points) and low (1–3 points) qualities [27].
4 Data extraction
Two independent researchers (R.-x.T. and T.-s.Z.) reviewed all of the articles that met the inclusion criteria. We selected OS as the primary endpoints, RFS and EFS as the secondary endpoints [6], [28]. We extracted characteristics of the studies, the corresponding HRs with 95% CIs from COX multivariable models. Unpublished data in some studies were obtained by contacting the authors. If the HRs with 95% CIs were not presented in some articles, we would extract the data from corresponding Kaplan-Meier curves using the methods described by Parmar and Tierney [29], [30].
5 Data synthesis and statistical analysis
We pooled the HRs and 95% CIs for OS, RFS and EFS respectively in total population and subgroups, using random-effect and fixed-effect models simultaneously [31], but only the estimates from random effects model was selected as the basis of our conclusion, because this approach could provide a more conservative assessment of the average effect size [32]. In the forest plots, pooled HR values>1 represented a positive association between mutant DNMT3A and prognosis of patients; while pooled HR values<1 represented a negative association.
6 Assessment of heterogeneity
We assessed statistical heterogeneity as to the pooled HR for OS in total population by visual inspection of the forests plots and by a formal statistical test using Chi-square test with a significance level at P<0. 1. I2 statistics was also used to quantitatively assess the possible heterogeneity (I2>30% represents moderate heterogeneity, I2>75% represents considerable heterogeneity) [33].
7 Subgroup analysis
We explored the possible causes of heterogeneity by subgroups analysis. We examined the following as important subgroups: (1) cytogenetic intermediate-risk subgroup; (2) cytogenetically normal subgroup; (3) patients younger than 60 years of age; (4) patients older than 60 years of age. (5) favorable risk genotype subgroup, namely low risk molecular group, which referred to the patients with mutant NPM1 and wild-type FLT3-ITD (NPM1+/FLT3-ITD−); (6) unfavorable risk genotype subgroup, also known as high risk molecular group, which included the patients (NPM1−/FLT3-ITD+, NPM1−FLT3-ITD− or NPM1+/FLT3-ITD+); (7) patients with DNMT3A mutations at R882; and (8) patients with DNMT3A mutations at Non-R882. Of note, NPM1/FLT3-ITD risk genotype groups were all belong to CN-AML.
8 Assessment of reporting biases and sensitivity analysis
Sensitivity analysis was performed to detect the robustness of pooled HR for OS of all patients. Firstly, to test for publication bias, We selected OS of total population to form a funnel plot [34], [35] and contour enhanced funnel plot [36], and undertook the Egger test as well. Different types of funnel plots were presented in a similar form of scatter plots of study effect sizes (x axis) against estimated standard errors (y axis). Contour enhanced funnel plots display areas of statistical significance on a funnel plot. Contour lines represent different levels of statistical significance (e. g. 5%, 10%). If studies seemed to be missing in areas of non-significance (P>10%), the asymmetry of the funnel plot might be due to publication bias, although other explanations should still be considered. Meanwhile, we attempted to find other reporting biases such as outcome reporting bias, language bias, citation bias and location bias and so on.
In addition, we tried to figure out “missing” studies and assessed the robustness of pooled HR for OS of the overall population by combining contour enhanced funnel plots with the trim and fill adjustment method(random and fixed effects linear estimator) [37], [38], [39], All statistical analyses were performed by the software STATA (version 12. 0).
Results
1 Search results
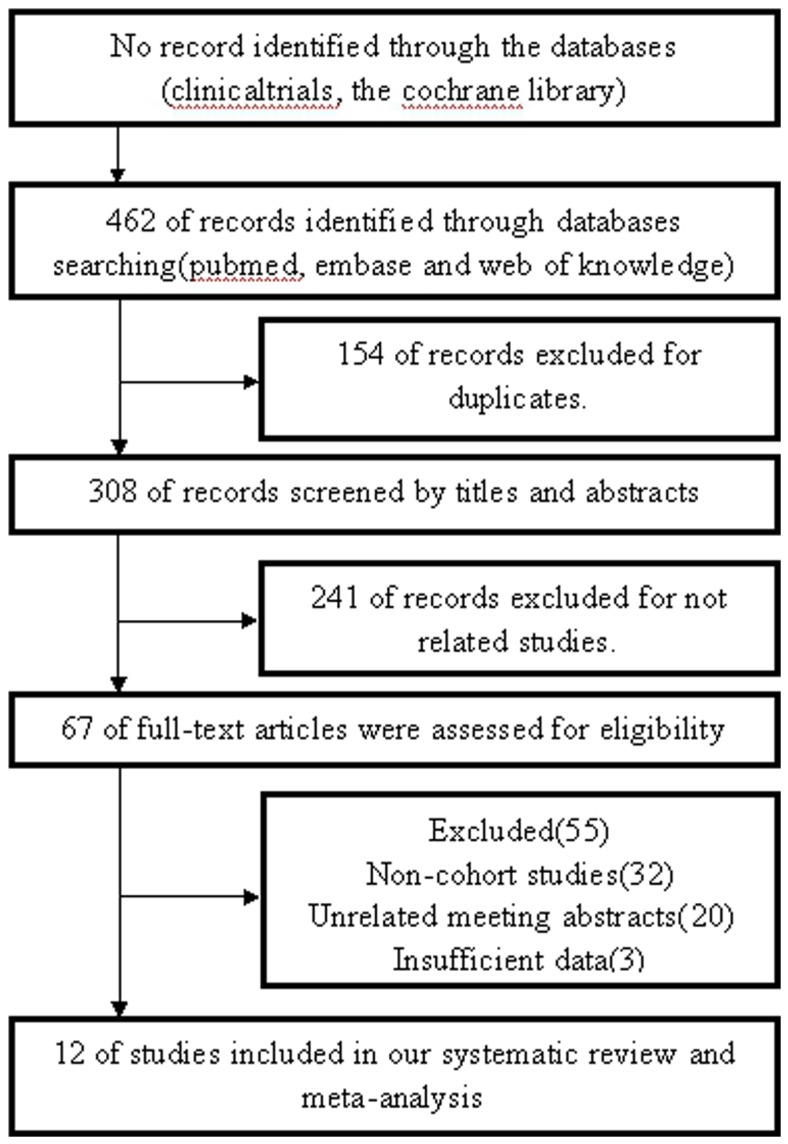
As shown in Figure 1 , 462 records were obtained by searching the databases. After exclusion of 154 duplicates, 308 records were further screened by reading their titles and abstracts, and then 241 records were excluded, in which DNMT3A mutations were not regarded as the primary research problems. The full texts of the remaining 67 studies were read carefully, and 55 of them including 32 non-cohort studies, 20 unrelated meeting abstracts and 3 studies having no sufficient data were further excluded. Eventually, 12 studies met the predefined selection criteria, which included 2 meeting abstract [40] and 10 original articles [13], [20], [21], [22], [23], [24], [25], [41], [42], [43].
Figure 1. PRISMA flow diagram for study review and inclusion.
2 Risk of bias in the included studies
We assessed risk of bias (see methodological quality domains), according to nine items of NOS. The qualities of 9 (75%) studies were considered high, and the remaining 3 (25%) studies were thought moderate. More details were shown in Table 1 and Table 2 .
Table 1. Clinical and laboratory characteristics of patients with AML with DNMT3A mutations from the 12 included studies.
| First author | Year | Source | NOS | n/N | Median follow-up, mo (range) | Median age, y (range) | FAB classification | Cytogenetic risk group | HR estimation |
| Timothy J. Ley | 2010 | USA | 9 | 62/281 | 34.1 (0.2–129.3) | 53.1 (39.4–66.8) | M0, 2; M1, 15; M2, 11; M3, 1; M4, 20; M5, 12; M6, 0; M7, 1; RAEB, 0; Unknown, 0 | Favorable, 0; Intermediate, 56; Adverse, 4; Unknown, 2 | HR |
| Yang Shen | 2011 | China | 7 | 75/1141 | — | 38–69 | — | — | HR |
| Felicitas Thol | 2011 | Germany | 9 | 87/489 | 61.2 (0.624–140.4) | 52 (30–60) | M0, 3; M1, 15; M2, 8; M3, 0; M4, 37; M5, 22; M6, 1; M7, 0; RAEB, —; Unknown, 1 | Favorable, 1; Intermediate, 82; Adverse, 4; Unknown, 0 | HR |
| Hsin-An Hou | 2011 | Taiwan | 8 | 70/500 | 55 (1.0–160) | 61 (16–87) | M0, 2; M1, 14; M2, 13; M3, 0; M4, 28; M5, 12; M6, 0; M7, —; RAEB, —; Unknown, 1 | Favorable, 0; Intermediate, 62; Adverse, 4; Unknown, 4 | HR |
| Jana Markova | 2011 | Czech Republic | 5 | 67/226 | 11.6 (0–202) | 54.9 (18.2–81.7) | M0, 0; M1, 18; M2, 22; M3, —; M4, 17; M5, 5; M6, —; M7, —; RAEB, —; Unknown, 5 | Favorable, 0; Intermediate, 67; Adverse, 0; Unknown, 0 | Survival curve |
| A Renneville | 2012 | France | 7 | 36/123 | 46.8 | 47 (23–58) | M0, 0; M1, 6; M2, 10; M3, 0; M4, 11; M5, 9; M6, 0; M7, 0; RAEB, 0; Unknown, 0 | Favorable, 0; Intermediate, 36; Adverse, 0; Unknown, 0 | HR |
| Guido Marcucci | 2012 | USA | 9 | 142/415 | 90 (27.6–488) | 61 (22–82) | M0, 1; M1, 29; M2, 18; M3, 0; M4, 33; M5, 26; M6, 0; M7, —; RAEB, —; Unknown, 35 | Favorable, 0; Intermediate, 142; Adverse, 0; Unknown, 0 | HR |
| Jay P. Patel | 2012 | USA | 9 | 88/384 | — | 48 (17–60) | — | — | HR |
| Ana Flávia Tibúrcio Ribeiro | 2012 | USA | 9 | 96/415 | 115.7 (7.2–224.1) | 50.5 (18–60) | M0, 1; M1, 15; M2, 23; M3, —; M4, 15; M5, 36; M6, 1; M7, —; RAEB, 3; Unknown, 2 | Favorable, 0; Intermediate, 85; Adverse, 6; Unknown, 5 | HR |
| Xu, Y | 2012 | China | 5 | 31/442 | — | 40 (16–60) | — | — | HR |
| Ostronoff, F | 2013 | USA | 6 | 37/191 | 101.6 | 68 (57–81) | M0, 2; M1, 9; M2, 6; M3, 0; M4, 10; M5, 7; M6, 0; M7, 0; RAEB, 0; Unknown, 3 | Favorable, 0; Intermediate, 24; Adverse, 1; Unknown, 12 | HR |
| Verena I. Gaidzik | 2013 | Germany | 9 | 370/1770 | 59.28 | 50.5 (18–60) | — | Favorable, 4; Intermediate, 309; Adverse, 33; Unknown, 24 | HR |
NOS, Newcastle-ottawa quality assessment scale; n, number of patients with DNMT3A mutations; N, number of patients in total; —, indicates there is no related data presented.
Table 2. Clinical and laboratory characteristics of patients with AML without DNMT3A mutations from the 12 included studies.
| First author | Year | Source | NOS | (N-n)/N | Median follow-up, mo (range) | Median age, y (range) | FAB classification | Cytogenetic risk group | HR estimation |
| Timothy J. Ley | 2010 | USA | 9 | 219/281 | 34.1 (0.2–129.3) | 47.8 (31.2–64.4) | M0, 19; M1, 44; M2, 54; M3, 47; M4, 41; M5, 9; M6, 3; M7, 2; RAEB, 0; Unknown, 0 | Favorable, 79; Intermediate, 110; Adverse, 26; Unknown, 4 | HR |
| Yang Shen | 2011 | China | 7 | 1066/1141 | — | 18.6–59.4 | — | — | HR |
| Felicitas Thol | 2011 | Germany | 9 | 402/489 | 61.2 (0.624–140.4) | 45 (17–60) | M0, 7; M1, 74; M2, 113; M3, 0; M4, 130; M5, 44; M6, 11; M7, 3; RAEB, —; Unknown, 20 | Favorable, 78; Intermediate, 262; Adverse, 57; Unknown, 5 | HR |
| Hsin-An Hou | 2011 | Taiwan | 8 | 430/500 | 55 (1.0–160) | 49 (15–90) | M0, 8; M1, 98; M2, 158; M3, 38; M4, 96; M5, 12; M6, 12; M7, —; RAEB, —; Unknown, 8 | Favorable, 99; Intermediate, 256; Adverse, 61; Unknown, 14 | HR |
| Jana Markova | 2011 | Czech Republic | 5 | 159/226 | 11.6 (0–202) | 54.9 (18.2–81.7) | M0, 7; M1, 29; M2, 46; M3, —; M4, 33; M5, —; M6, 12; M7, —; RAEB, —; Unknown, 32 | Favorable, 0; Intermediate, 159; Adverse, 0; Unknown, 0 | Survival curve |
| A Renneville | 2012 | France | 7 | 87/123 | 46.8 | 48 (16–59) | M0, 5; M1, 24; M2, 27; M3, —; M4, 11; M5, 7; M6, 7; M7, —; RAEB, —; Unknown, 6 | Favorable, 0; Intermediate, 87; Adverse, 0; Unknown, 0 | HR |
| Guido Marcucci | 2012 | USA | 9 | 273/415 | 90 (27.6–488) | 62 (18–83) | M0, 7; M1, 54; M2, 71; M3, 0; M4, 41; M5, 21; M6, 3; M7, —; RAEB, —; Unknown, 76 | Favorable, 0; Intermediate, 273; Adverse, 0; Unknown, 0 | HR |
| Jay P. Patel | 2012 | USA | 9 | 296/384 | — | 48 (17–60) | — | — | HR |
| Ana Flávia Tibúrcio Ribeiro | 2012 | USA | 9 | 319/415 | 115.7 (7.2–224.1) | 41 (15–60) | M0, 15; M1, 72; M2, 81; M3, —; M4, 64; M5, 64; M6, 5; M7, —; RAEB, 13; Unknown, 5 | Favorable, 57; Intermediate, 191; Adverse, 64; Unknown, 7 | HR |
| Xu, Y | 2012 | China | 5 | 411/442 | — | 40 (16–60) | — | — | HR |
| Ostronoff, F | 2013 | USA | 6 | 154/191 | 101.6 | 68 (56–89) | M0, 3; M1, 35; M2, 55; M3, 1; M4, 38; M5, 13; M6, 2; M7, 5; RAEB, 0; Unknown, 3 | Favorable, 12; Intermediate, 54; Adverse, 32; Unknown, 56 | HR |
| Verena I. Gaidzik | 2013 | Germany | 9 | 1400/1770 | 59.28 | 47.6 (18–60) | — | Favorable, 252; Intermediate, 751; Adverse, 287; Unknown, 110 | HR |
NOS, Newcastle-ottawa quality assessment scale; n, number of patients with DNMT3A mutations; N, number of patients in total; —, indicates there is no related data presented.
3 Characteristics of the included studies
The main characteristics of the patients with or without DNMT3A mutations in 12 included studies were presented in Table 1 and Table 2 respectively, additional characteristics of the patients were shown in Tables S1 and S2. Of these studies, 5 originated from America, 4 from Europe and 3 from Asia.
4 Data extracting
We obtained directly most of data from the included studies except for one set of data [25], which were extracted indirectly from the corresponding Kaplan-Meier curves related to mutant DNMT3A. Additionally, we managed to obtain some unpublished data by contacting the authors. Hou et al. offered the HRs with 95% CIs for OS and RFS in unfavorable and favorable risk genotype subgroups with AML. Fabiana et al. offered the HRs with 95% CIs for OS, EFS and RFS in subgroups as mentioned above.
5 Association of DNMT3A mutations with pretreatment clinical and molecular characteristics
More patients with DNMT3A mutations were found with mutations in NPM1, FLT3-ITD and IDH1/2 [13], [20], [21], [22], [23], [24], [42], whereas CEBPA mutations hardly coexisted in the patients with DNMT3A mutations [20], [21], [22], [42], [43]. DNMT3A mutations were mainly enriched in the patients with CN-AML or with intermediate-risk AML. Patients with favorable-risk cytogenetics had scarcely DNMT3A mutations. Comparing with wild-type DNMT3A patients, DNMT3A mutated patients were older, with higher median WBC counts and percentage of bone marrow blasts at diagnosis. Whereas, platelet counts of patients were not considered to be associated with DNMT3A mutations in most of the included studies [21], [22], [23], [24].
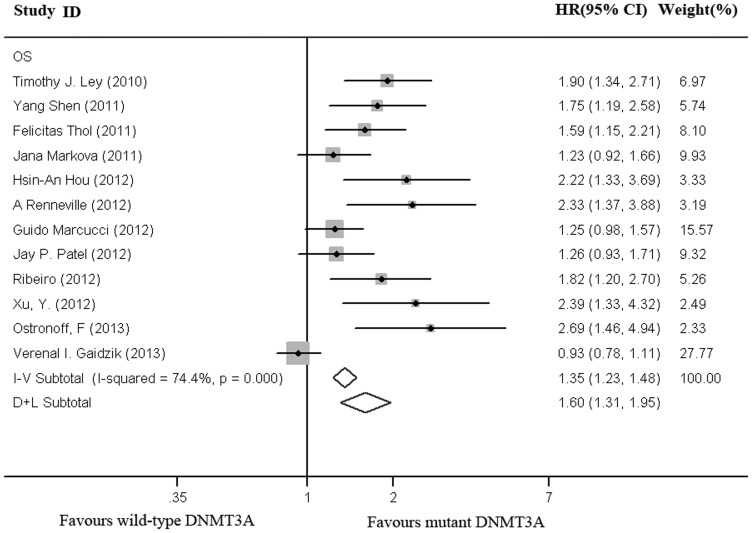
6 Association of DNMT3A mutations with clinical outcomes in total population
As shown in Figure 2 , data were extracted from 12 studies, with a total of 6377 patients, including 1161 patients with DNMT3A mutation. In the total population, the patients with DNMT3A mutations had a shorter OS as compared to those with wild-type DNMT3A (HR = 1.60, 95% CI, 1.31–1.95). There was considerable heterogeneity as shown by I2 testing (I2 = 74.4%, P<0. 001).
Figure 2. Forest plot of the HR for overall survival of all AML patients.
DNMT3A mutations versus wild-type DNMT3A. I–V Overall: the pooled HR with 95% CI using a fixed effects model; D+L Overall: the pooled HR with 95% CI using a random effects model.
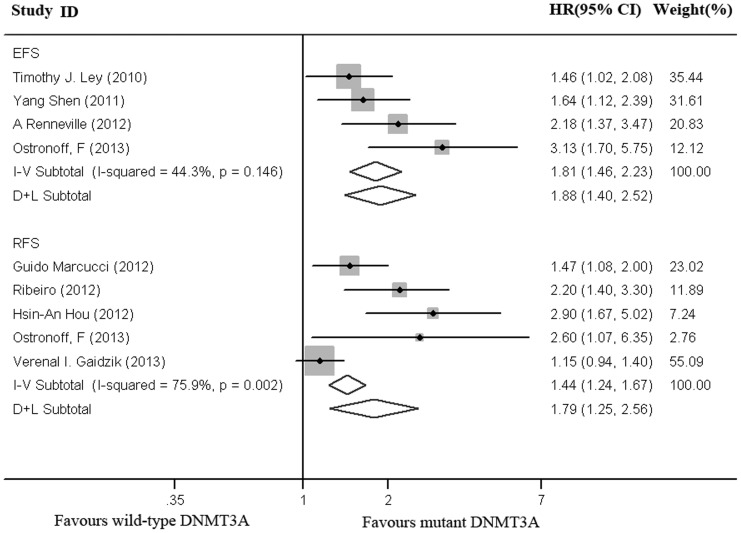
As shown in Figure 3 , data were extractable from 5 out of 12 studies, with a total of 3291 patients, including 715 DNMT3A mutated patients. In this population, patients with DNMT3A mutations had a shorter RFS as compared to those with wild-type DNMT3A (HR = 1.79, 95% CI, 1.25–2.56). There was considerable heterogeneity by I2 testing (I2 = 75.9%, P = 0.002).
Figure 3. Forest plot of the HRs for relapse-free or event-free survival of AML patients.
DNMT3A mutations versus wild-type DNMT3A. I–V Subtotal represented the pooled HRs with 95% CIs using a fixed effects model; D+L Subtotal represented the pooled HR with 95% CI using a random effects model.
As shown in Figure 3 , data were extractable from 4 out of 12 studies, with a total of 1736 patients, including 210 DNMT3A mutated patients. In this population, patients with DNMT3A mutations had a shorter EFS as compared to them with wild-type DNMT3A (HR = 1.88, 95% CI, 1.40–2.52). There was moderate heterogeneity by I2 testing (I2 = 44.3%, P = 0.146).
7 Association of DNMT3A mutations with clinical outcomes in different subgroups
We pooled the HRs in fixed- and random-effect models simultaneously, which were shown in Table 3 and Table 4 respectively, corresponding forest plots were presented in Figures S1 to S8. In the favorable risk genotype subgroup, mutant DNMT3A had no prognostic impact on OS or RFS other than EFS. And in the non-R882-DNMT3A mutations subgroup, mutant DNMT3A had no prognostic value for OS. However, DNMT3A mutations were independently prognostic factors for OS, RFS and EFS of patients in the remaining 6 subgroups. There was considerable statistical heterogeneity detected by I2 test in most of these subgroups.
Table 3. Outcome of subgroups in a random effects model.
| Subgroups | OS | RFS | EFS | ||||||||||||
| N. of S. | D+/− | I2 (%) | HR (95% CI) | P | N. of S. | D+/− | I2 (%) | HR (95% CI) | P | N. of S. | D+/− | I2 (%) | HR (95% CI) | P | |
| CN-AML | 7 | 760/2321 | 74.4 | 1.60 (1.20–2.13) | 0.001 | 5 | 562/1582 | 67.3 | 1.68 (1.20–2.36) | 0.016 | 2 | 99/373 | 62.1 | 2.43 (1.18–5.00) | 0.104 |
| Intermediate-risk cytogenetics | 3 | 225/697 | 67.2 | 1.51 (1.08–2.11) | 0.047 | 2 | 183/721 | 0.0 | 1.52 (1.19–1.93) | 0.937 | 0 | — | — | — | — |
| Younger than 60 years of age | 10 | 1054/4836 | 80.7 | 1.84 (1.36–2.50) | <0.001 | 4 | 597/1971 | 84.3 | 2.10 (1.20–3.69) | <0.001 | 3 | 173/1372 | 0.0 | 2.32 (1.78–3.02) | 0.949 |
| Unfavorable risk genotype | 4 | 230/1073 | 0.0 | 2.30 (1.78–2.97) | 0.862 | 3 | 194/986 | 0.0 | 2.38 (1.69–3.36) | 0.726 | 2 | 73/241 | 0.0 | 1.74 (1.17–2.60) | 0.78 |
| Favorable risk genotype | 6 | 388/1611 | 0.0 | 1.40 (0.98–1.99) | 0.798 | 4 | 290/1305 | 41.1 | 1.18 (0.62–2.24) | 0.165 | 2 | 73/241 | 0.0 | 1.99 (1.09–3.61) | 0.432 |
| Older than 60 years of age | 2 | 204/492 | 0.0 | 1.71 (1.27–2.31) | 0.759 | 0 | — | — | — | — | 0 | — | — | — | — |
| R882-DNMT3A-mt/DNMT3A-wt | 4 | 539/2144 | 74.5 | 1.41 (1.06–1.88) | 0.008 | 3 | 432/1541 | 0.0 | 1.36 (1.16–1.61) | 0.757 | 0 | — | — | — | — |
| Non-R882-DNMT3A-mt/DNMT3A-wt | 3 | 332/1825 | 89 | 1.25 (0.69–2.25) | <0.001 | 0 | — | — | — | — | 0 | — | — | — | — |
N.of S., number of studies;
D+/−, indicates ratio of number of patients with mutant DNMT3A to patients with wild-type DNMT3A;
—, reflects there is no corresponding data presented; Abbreviations: mt, mutation; wt, wild type.
Table 4. Outcome of subgroups in a fixed effects model.
| Subgroups | OS | RFS | EFS | ||||||||||||
| N. of S. | D+/− | I2 (%) | HR (95% CI) | P | N. of S. | D+/− | I2 (%) | HR (95% CI) | P | N. of S. | D+/− | I2 (%) | HR (95% CI) | P | |
| CN-AML | 7 | 760/2321 | 74.4 | 1.33 (1.17–1.52) | 0.001 | 5 | 562/1582 | 67.3 | 1.44 (1.22–1.71) | 0.016 | 2 | 99/373 | 62.1 | 2.19 (1.46–3.27) | 0.104 |
| Intermediate-risk cytogenetics | 3 | 225/697 | 67.2 | 1.45 (1.20–1.75) | 0.047 | 2 | 183/721 | 0.0 | 1.52 (1.19–1.93) | 0.937 | 0 | — | — | — | — |
| Younger than 60 years of age | 10 | 1054/4836 | 80.7 | 1.40 (1.25–1.58) | <0.001 | 4 | 597/1971 | 84.3 | 1.44 (1.22–1.71) | <0.001 | 3 | 173/1372 | 0.0 | 2.32 (1.78–3.02) | 0.949 |
| Unfavorable risk genotype | 4 | 230/1073 | 0.0 | 2.30 (1.78–2.97) | 0.862 | 3 | 194/986 | 0.0 | 2.38 (1.69–3.36) | 0.726 | 2 | 73/241 | 0.0 | 1.74 (1.17–2.60) | 0.78 |
| Favorable risk genotype | 6 | 388/1611 | 0.0 | 1.40 (0.98–1.99) | 0.798 | 4 | 290/1305 | 41.1 | 1.19 (0.75–1.88) | 0.165 | 2 | 73/241 | 0.0 | 1.99 (1.09–3.61) | 0.432 |
| Older than 60 years of age | 2 | 204/492 | 0.0 | 1.71 (1.27–2.31) | 0.759 | 0 | — | — | — | — | 0 | — | — | — | — |
| R882-DNMT3A-mt/DNMT3A-wt | 4 | 539/2144 | 74.5 | 1.30 (1.14–1.50) | 0.008 | 3 | 432/1541 | 0.0 | 1.36 (1.16–1.61) | 0.757 | 0 | — | — | — | — |
| Non-R882-DNMT3A-mt/DNMT3A-wt | 3 | 332/1825 | 89 | 1.08 (0.90–1.31) | <0.001 | 0 | — | — | — | — | 0 | — | — | — | — |
N.of S., number of studies;
D+/−, indicates ratio of number of patients with mutant DNMT3A to patients with wild-type DNMT3A;
—, reflects there is no corresponding data presented; Abbreviations: mt, mutation; wt, wild type.
8 Publication bias and sensitive analysis
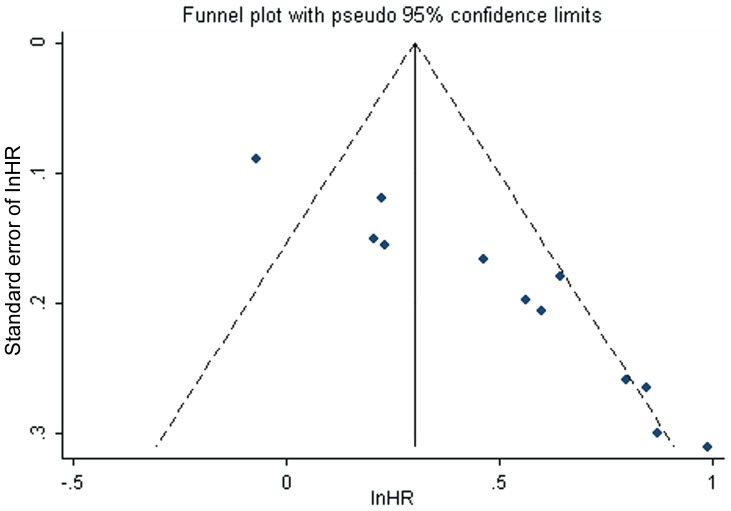
We utilized the data about OS of total population to search publication bias and do sensitive analysis.
As shown in Figure 4 , there was a strong suggestion of asymmetry in the funnel plot (Egger's test P<0. 001).
Figure 4. Funnel plots illustrated significant asymmetry on HR for overall survival of all patients.
Studies were distributed asymmetrically and suggested biases exist.
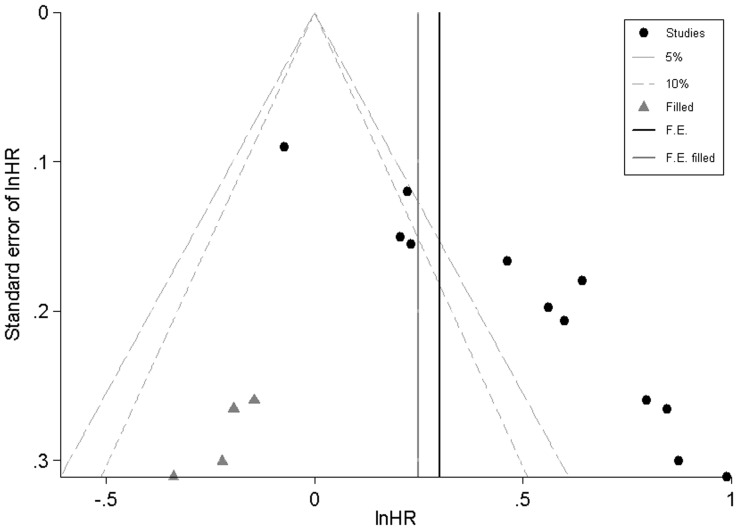
Figure 5 demonstrated the distribution of 12 real studies and 4 filled studies. Of the 12 real studies, 8 studies lay above the right 5% significant contour line, and 4 studies located below the 5% significant contour line. Only one study distributed on the left-hand side of the plot, which also implied asymmetry of the plot. Secondly, the trim and fill method imputed a total of 4 “missing” studies in a random effects model, which were presented in the form of gray triangles located in the region of statistical non-significance (P>10%), and the vertical black line showed the pooled log HR as to OS in 12 studies, while the vertical gray line showed the pooled log HR including the filled studies. After adding the “missing” studies to the contour-enhanced funnel plot, the pooled fixed-effects HR was 1.282 (95% CI, 1.174–1.400), and the pooled random-effects HR was 1.394 (95% CI, 1.161–1.674), which implied DNMT3A mutations had a slightly negative impact on OS in total population.
Figure 5. Confunnel with filled studies from metatrim:
mutant DNMT3A versus wild-type DNMT3A in a random effects model. The pooled HR on overall survival from 12 published studies is robust and the heterogeneity mainly results from unpublished studies.
Discussion
We have performed a systematic review and meta-analysis in an effort to figure out the association between DNMT3A mutations and poor prognosis of patients with de novo AML.
So far, the 12 published studies have addressed the prognostic value of mutant DNMT3A in AML patients. According to the rules of NOS, the majority of included studies belonged to high quality, only 3 of the studies had moderate quality. A total of 6377 patients of the 12 included studies, where there were 1161 patients with mutant DNMT3A.
The primary end point was OS. DNMT3A mutations had slightly prognostic impact on OS in total population, which was consistent with the pooled outcomes in the meta-analysis by Shivarov et al [44]. And the conclusion was suitable for the majority of subgroups except for the favorable risk genotype and non-R882 DNMT3A mutation subgroups. The second endpoints were RFS and EFS. First of all, mutant DNMT3A had poor prognostic impact on RFS in nearly all of the mentioned groups other than favorable risk genotype subgroup. As for EFS, DNMT3A mutations were associated with poor prognosis of patients in all of the mentioned groups above. However, most of the included studies showed neither type of DNMT3A mutation had an impact on the probability of achieving CR in multivariate analyses [21], [22], [23], [24], [41], [42].
There were significant correlation of DNMT3A mutations with patient characteristics, including age of patients and WBC in peripheral blood at diagnosis, the mutations of NPM1, FLT3 or other genes (IDH1, IDH2, TET2, WT1 and CEBPA), regardless of the types of mutation. In addition, only one study mentioned the association between DNMT3A mutations and expression of CD molecules on leukemic initiating cells, such as CD14, CD13 and CD34 [24].
We observed considerable or moderate between-study heterogeneity in total population and subgroups, unlike that in the meta-analysis by Shivarov et al [44].
The heterogeneity mainly came from one study lately published [26]. It was worth noting that we did not conduct a meta-regression analysis because of fewer studies included. So we explored subjectively the clinical heterogeneity as follows: firstly, with respect to FAB classification, patients' years of age, cytogenetic and molecular abnormalities, the constituent ratio of patients were various in each study, for instance, 7 studies only included patients younger than 60 years of age [20], [21], [23], [40], [41], [42], 2 studies only included cytogenetic normal patients [22], [42], 1 study included patients belonging to cytogenetic intermediate risk group [22]; secondly, most of the included studies did not presented the ECOG performance status of patients except for two of them [23], [43], so we could not further assess the status of patients when they were included, which might be one of the sources of heterogeneity; thirdly, the treatment programs such as induced chemotherapy and hematopoietic stem cell transplantation were diverse in individual studies, even intensities of the same induced chemotherapy drug were various in different studies, so the selection of different treatment programs might lead to the heterogeneity of clinical outcomes; eventually, there were much between-study heterogeneity in other aspects such as the time of follow up, percentages of bone marrow blasts, races of patients, types of DNMT3A mutations, the methods of gene sequencing, and the number of adjusted covariates among the 12 studies and so on.
We found the asymmetry in a usual funnel plot. Subsequently, we adjusted pooled HR for OS in total population by combining the trim and fill method with contour enhanced funnel plot, and found that the asymmetry was probably caused by unpublished “missing” studies, so publication bias was a major threat to the validity of our estimate outcomes, although other explanations should still be considered. Meanwhile, we verified the robustness of the pooled random-effect and fixed-effect outcomes of 16 studies consistent with the pooled outcomes of 12 original studies, which was extremely important for our eventual conclusion.
We did not find any methodological issues in the preparation of the review which could put it at risk for bias.
There are the following aspects of main limitation in our review. Firstly, the “missing” studies have been relatively absent to date. Secondly, selective reporting were seen in some studies, for instance, the pooled HRs for RFS and EFS were shown in relatively fewer studies as compared to them for OS, and some subgroups such as older patients were not analyzed in most studies, which resulted in losses of valuable information. Thirdly, two studies were published as meeting abstracts, so we could not assess its potential risk of bias in detail. Fourthly, the included studies were all published in English, so language bias existed. Fifthly, we could not access the association between mutant DNMT3A and prognosis of secondary AML because of the lack of efficient data. Finally, if these trials could offer individual patient data, our analysis would have been much more perfect.
In conclusion, using some advanced statistical methods and high quality evidences, we confirmed objectively the robustness of association between mutant DNMT3A and prognosis of adults with de novo AML, although there are considerable heterogeneity in many conditions. Combining other important genetic biomarkers, DNMT3A mutations would contribute to a more precise clinical risk stratification and decision of treatment. More cohort studies concerning DNMT3A mutations are needed in an effort to further verify or modify the pooled estimates to a certain extent, especially for the patients with CN-AML or with cytogenetic intermediate risk abnormalities. It is meaningful to clarify the mechanism that mutant DNMT3A function as a epigenetic regulator in adult AML. And more studies will be needed to determine whether dose-intensified induction chemotherapy improves the survival outcomes in patients with DNMT3A mutations.
Supporting Information
Forest plot of the HRs with 95% CIs for OS, RFS and EFS of CN-AML patients (mutant DNMT3A versus wild-type DNMT3A).
(TIF)
Forest plot of the HRs with 95% CIs for OS and RFS of AML patients with intermediate-risk cytogenetics (mutant DNMT3A versus wild-type DNMT3A).
(TIF)
Forest plot of the HRs with 95% CIs for OS, RFS and EFS of patients younger than 60 years of age (mutant DNMT3A versus wild-type DNMT3A).
(TIF)
Forest plot of the HRs with 95% CIs for OS, RFS and EFS of patients with unfavorable risk genotype (mutant DNMT3A versus wild-type DNMT3A).
(TIF)
Forest plot of the HRs with 95% CIs for OS, RFS and EFS of patients with favorable risk genotype (mutant DNMT3A versus wild-type DNMT3A).
(TIF)
Forest plot of the HR with 95% CI for OS of patients older than 60 years of age (mutant DNMT3A versus wild-type DNMT3A).
(TIF)
Forest plot of the HRs with 95% CIs for OS and RFS of patients with R882-mutant DNMT3A as compared to patients with wild-type DNMT3A.
(TIF)
Forest plot of the HR with 95% CI for OS of patients with Non-R882-mutant DNMT3A as compared to patients with wild-type DNMT3A.
(TIF)
Clinical and laboratory characteristics of patients with AML with DNMT3A mutations from the 12 included studies.
(DOCX)
Clinical and laboratory characteristics of patients with AML without DNMT3A mutations from the 12 included studies.
(DOCX)
The PRISMA 2009 checklist.
(DOC)
Acknowledgments
Xiaoyu Lai and Jimin Shi contributed to the revisions of the manuscript during the peer review process and were included as co-authors after the original submission.
Funding Statement
The research article was supported by the National Natural Science Foundation of China (No: 81170526), the National Natural Science Foundation for Distinguished Young Scholars of China (No: 81100364), the Zhejiang Province Natural Science Major Foundation (No: Z2100097), the Zhejiang Province Natural Science Foundation (No: Y2110152) and the Public Welfare Research Subproject from National Ministry of Health (No: 201202017). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Becker H, Maharry K, Radmacher MD, Margeson D, Mrozek K, et al. (2010) Sole trisomy 8 in patients (pts) with de novo Acute Myeloid Leukemia (AML) is associated with age-independent poor outcome that is modified by molecular markers and with unique gene- and microrna (miR)-signatures: A Cancer and Leukemia Group B (CALGB) study. Blood 116: 255–5. [Google Scholar]
- 2. Byrd JC, Mrozek K, Dodge RK, Carroll AJ, Edwards CG, et al. (2002) Pretreatment cytogenetic abnormalities are predictive of induction success, cumulative incidence of relapse, and overall survival in adult patients with de novo acute myeloid leukemia: results from Cancer and Leukemia Group B (CALGB 8461). Blood 100: 4325–36. [DOI] [PubMed] [Google Scholar]
- 3. Grimwade D, Hills RK, Moorman AV, Walker H, Chatters S, et al. (2010) Refinement of cytogenetic classification in acute myeloid leukemia: determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials. Blood 116: 354–65. [DOI] [PubMed] [Google Scholar]
- 4. Grimwade D, Walker H, Oliver F, Wheatley K, Harrison C, et al. (1998) The importance of diagnostic cytogenetics on outcome in AML: analysis of 1,612 patients entered into the MRC AML 10 trial. The Medical Research Council Adult and Children's Leukaemia Working Parties. Blood 92: 2322–33. [PubMed] [Google Scholar]
- 5. Slovak ML, Kopecky KJ, Cassileth PA, Harrington DH, Theil KS, et al. (2000) Karyotypic analysis predicts outcome of preremission and postremission therapy in adult acute myeloid leukemia: a Southwest Oncology Group/Eastern Cooperative Oncology Group Study. Blood 96: 4075–83. [PubMed] [Google Scholar]
- 6. Dohner H, Estey EH, Amadori S, Appelbaum FR, Buchner T, et al. (2010) Diagnosis and management of acute myeloid leukemia in adults: recommendations from an international expert panel, on behalf of the European LeukemiaNet. Blood 115: 453–74. [DOI] [PubMed] [Google Scholar]
- 7. Whitman SP, Maharry K, Radmacher MD, Becker H, Mrozek K, et al. (2010) FLT3 internal tandem duplication associates with adverse outcome and gene- and microRNA-expression signatures in patients 60 years of age or older with primary cytogenetically normal acute myeloid leukemia: a Cancer and Leukemia Group B study. Blood 116: 3622–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Thiede C, Steudel C, Mohr B, Schaich M, Schakel U, et al. (2002) Analysis of FLT3-activating mutations in 979 patients with acute myelogenous leukemia: association with FAB subtypes and identification of subgroups with poor prognosis. Blood 99: 4326–35. [DOI] [PubMed] [Google Scholar]
- 9. Becker H, Marcucci G, Maharry K, Radmacher MD, Mrozek K, et al. (2010) Favorable prognostic impact of NPM1 mutations in older patients with cytogenetically normal de novo acute myeloid leukemia and associated gene- and microRNA-expression signatures: a Cancer and Leukemia Group B study. J Clin Oncol 28: 596–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Falini B, Mecucci C, Tiacci E, Alcalay M, Rosati R, et al. (2005) Cytoplasmic nucleophosmin in acute myelogenous leukemia with a normal karyotype. N Engl J Med 352: 254–66. [DOI] [PubMed] [Google Scholar]
- 11. Marcucci G, Maharry K, Radmacher MD, Mrozek K, Vukosavljevic T, et al. (2008) Prognostic significance of, and gene and microRNA expression signatures associated with, CEBPA mutations in cytogenetically normal acute myeloid leukemia with high-risk molecular features: a Cancer and Leukemia Group B Study. J Clin Oncol 26: 5078–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Taskesen E, Bullinger L, Corbacioglu A, Sanders MA, Erpelinck CA, et al. (2011) Prognostic impact, concurrent genetic mutations, and gene expression features of AML with CEBPA mutations in a cohort of 1182 cytogenetically normal AML patients: further evidence for CEBPA double mutant AML as a distinctive disease entity. Blood 117: 2469–75. [DOI] [PubMed] [Google Scholar]
- 13. Ley TJ, Ding L, Walter MJ, McLellan MD, Lamprecht T, et al. (2010) DNMT3A Mutations in Acute Myeloid Leukemia. New England Journal of Medicine 363: 2424–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yan XJ, Xu J, Gu ZH, Pan CM, Lu G, et al. (2011) Exome sequencing identifies somatic mutations of DNA methyltransferase gene DNMT3A in acute monocytic leukemia. Nature Genetics 43: 309–U351. [DOI] [PubMed] [Google Scholar]
- 15. Yamashita Y, Yuan J, Suetake I, Suzuki H, Ishikawa Y, et al. (2010) Array-based genomic resequencing of human leukemia. Oncogene 29: 3723–31. [DOI] [PubMed] [Google Scholar]
- 16. Mardis ER, Ding L, Dooling DJ, Larson DE, McLellan MD, et al. (2009) Recurring mutations found by sequencing an acute myeloid leukemia genome. N Engl J Med 361: 1058–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Marcucci G, Maharry K, Wu YZ, Radmacher MD, Mrozek K, et al. (2010) IDH1 and IDH2 gene mutations identify novel molecular subsets within de novo cytogenetically normal acute myeloid leukemia: a Cancer and Leukemia Group B study. J Clin Oncol 28: 2348–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Abdel-Wahab O (2012) Molecular genetics of acute myeloid leukemia: clinical implications and opportunities for integrating genomics into clinical practice. Hematology 17: S39–S42. [DOI] [PubMed] [Google Scholar]
- 19. Delhommeau F, Dupont S, Della Valle V, James C, Trannoy S, et al. (2009) Mutation in TET2 in myeloid cancers. N Engl J Med 360: 2289–301. [DOI] [PubMed] [Google Scholar]
- 20. Patel JP, Gonen M, Figueroa ME, Fernandez H, Sun ZX, et al. (2012) Prognostic Relevance of Integrated Genetic Profiling in Acute Myeloid Leukemia. New England Journal of Medicine 366: 1079–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ribeiro AFT, Pratcorona M, Erpelinck-Verschueren C, Rockova V, Sanders M, et al. (2012) Mutant DNMT3A: a marker of poor prognosis in acute myeloid leukemia. Blood 119: 5824–31. [DOI] [PubMed] [Google Scholar]
- 22. Marcucci G, Metzeler KH, Schwind S, Becker H, Maharry K, et al. (2012) Age-Related Prognostic Impact of Different Types of DNMT3A Mutations in Adults With Primary Cytogenetically Normal Acute Myeloid Leukemia. Journal of Clinical Oncology 30: 742–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Thol F, Damm F, Ludeking A, Winschel C, Wagner K, et al. (2011) Incidence and Prognostic Influence of DNMT3A Mutations in Acute Myeloid Leukemia. Journal of Clinical Oncology 29: 2889–96. [DOI] [PubMed] [Google Scholar]
- 24. Hou HA, Kuo YY, Liu CY, Chou WC, Lee MC, et al. (2012) DNMT3A mutations in acute myeloid leukemia: stability during disease evolution and clinical implications. Blood 119: 559–68. [DOI] [PubMed] [Google Scholar]
- 25. Markova J, Michkova P, Burckova K, Brezinova J, Michalova K, et al. (2012) Prognostic impact of DNMT3A mutations in patients with intermediate cytogenetic risk profile acute myeloid leukemia. European Journal of Haematology 88: 128–35. [DOI] [PubMed] [Google Scholar]
- 26. Gaidzik VI, Schlenk RF, Paschka P, Stölzle A, Späth D, et al. (2013) Clinical impact of DNMT3A mutations in younger adult patients with acute myeloid leukemia: results of the AML Study Group (AMLSG). Blood 121: 4769–77. [DOI] [PubMed] [Google Scholar]
- 27. Wells GA, Shea B, O'Connell D, Peterson J, Welch V, et al. (2012) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Hospital Research Institute Available: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 2013 Jun 23. [Google Scholar]
- 28. Cheson BD, Bennett JM, Kopecky KJ, Buchner T, Willman CL, et al. (2003) Revised recommendations of the International Working Group for Diagnosis, Standardization of Response Criteria, Treatment Outcomes, and Reporting Standards for Therapeutic Trials in Acute Myeloid Leukemia. J Clin Oncol 21: 4642–9. [DOI] [PubMed] [Google Scholar]
- 29. Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR (2007) Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 8: 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Parmar MK, Torri V, Stewart L (1998) Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med 17: 2815–34. [DOI] [PubMed] [Google Scholar]
- 31. DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3): 177–88. [DOI] [PubMed] [Google Scholar]
- 32. Sattar N, Preiss D, Murray HM, Welsh P, Buckley BM, et al. (2010) Statins and risk of incident diabetes: a collaborative meta-analysis of randomised statin trials. Lancet 375: 735–42. [DOI] [PubMed] [Google Scholar]
- 33. Deeks JJ, Higgins JPT, Altman DG (2011) Chapter 9: Analysing data and undertaking meta-analyses. Cochrane Hand book for Systematic reviews of Interventions Available: http://handbook.cochrane.org/. Accessed 25 June 2013. [Google Scholar]
- 34. Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50: 1088–101. [PubMed] [Google Scholar]
- 35. Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315: 629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L (2008) Contour-enhanced meta-analysis funnel plots help distinguish publication bias from other causes of asymmetry. J Clin Epidemiol 61: 991–6. [DOI] [PubMed] [Google Scholar]
- 37. Moreno SG, Sutton AJ, Turner EH, Abrams KR, Cooper NJ, et al. (2009) Novel methods to deal with publication biases: secondary analysis of antidepressant trials in the FDA trial registry database and related journal publications. BMJ 339: b2981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Duval S, Tweedie R (2000) Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56: 455–63. [DOI] [PubMed] [Google Scholar]
- 39. Palmer TM, Peters JL, Sutton AJ, Moreno SG (2008) Contour-enhanced funnel plots for meta-analysis. Stata Journal 8: 242–54. [Google Scholar]
- 40. Xu Y, Yang Z, Tian H, Qiu H, Sun A, et al. (2012) Hematopoietic stem cell transplantation (HSCT) benefits the survival of acute myeloid leukemia (AML) patients with IDH1, NRAS and DNMT3A mutations. Blood 120. [Google Scholar]
- 41. Shen Y, Zhu YM, Fan X, Shi JY, Wang QR, et al. (2011) Gene mutation patterns and their prognostic impact in a cohort of 1185 patients with acute myeloid leukemia. Blood 118: 5593–603. [DOI] [PubMed] [Google Scholar]
- 42. Renneville A, Boissel N, Nibourel O, Berthon C, Helevaut N, et al. (2012) Prognostic significance of DNA methyltransferase 3A mutations in cytogenetically normal acute myeloid leukemia: a study by the Acute Leukemia French Association. Leukemia 26: 1247–54. [DOI] [PubMed] [Google Scholar]
- 43. Ostronoff F, Othus M, Ho PA, Kutny M, Geraghty DE, et al. (2013) Mutations in the DNMT3A exon 23 independently predict poor outcome in older patients with acute myeloid leukemia: a SWOG report. Leukemia 27: 238–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Shivarov V, Gueorguieva R, Stoimenov A, Tiu R (2013) DNMT3A mutation is a poor prognosis biomarker in AML: Results of a meta-analysis of 4500 AML patients. Leukemia Research 37: 1445–50. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Forest plot of the HRs with 95% CIs for OS, RFS and EFS of CN-AML patients (mutant DNMT3A versus wild-type DNMT3A).
(TIF)
Forest plot of the HRs with 95% CIs for OS and RFS of AML patients with intermediate-risk cytogenetics (mutant DNMT3A versus wild-type DNMT3A).
(TIF)
Forest plot of the HRs with 95% CIs for OS, RFS and EFS of patients younger than 60 years of age (mutant DNMT3A versus wild-type DNMT3A).
(TIF)
Forest plot of the HRs with 95% CIs for OS, RFS and EFS of patients with unfavorable risk genotype (mutant DNMT3A versus wild-type DNMT3A).
(TIF)
Forest plot of the HRs with 95% CIs for OS, RFS and EFS of patients with favorable risk genotype (mutant DNMT3A versus wild-type DNMT3A).
(TIF)
Forest plot of the HR with 95% CI for OS of patients older than 60 years of age (mutant DNMT3A versus wild-type DNMT3A).
(TIF)
Forest plot of the HRs with 95% CIs for OS and RFS of patients with R882-mutant DNMT3A as compared to patients with wild-type DNMT3A.
(TIF)
Forest plot of the HR with 95% CI for OS of patients with Non-R882-mutant DNMT3A as compared to patients with wild-type DNMT3A.
(TIF)
Clinical and laboratory characteristics of patients with AML with DNMT3A mutations from the 12 included studies.
(DOCX)
Clinical and laboratory characteristics of patients with AML without DNMT3A mutations from the 12 included studies.
(DOCX)
The PRISMA 2009 checklist.
(DOC)