This Special Issue commemorates the formation of an important partnership that began almost 25 years ago between the fields of neurologic rehabilitation and motor learning. At the time that this partnership began to develop, the assumption was made that the principles of motor learning gleaned through research with healthy subjects would be similar to those for patients with orthopedic and neurologic disorders, and as such would be highly relevant to the science and practice of physical therapy. Presently, the collaborative partnership between rehabilitation and motor learning research continues to grow. In fact, motor learning research targeting rehabilitation interventions has grown exponentially in recent years, as depicted in the figure below. This new research is providing our best evidence yet knowledge of motor learning will directly impact patient care.
The expansion of motor learning-associated rehabilitation research is also linked to a parallel expansion in basic research in neuroplasticity. We now understand that brain plasticity underlies all learning, and that the potential for neuroplastic change exists over the entire lifespan and in both healthy and dysfunctional brains.1 Numerous specific mechanisms for neuroplasticity have been revealed, ranging from very small changes in the molecular responses of individual neurons and synapses to major alterations in the functioning of local and global brain circuits. A major effort of the motor learning-based rehabilitation research community has been to determine practice parameters that will induce these basic mechanisms of neuroplasticity and maximize skill learning in the clinical setting.
Twenty-five years of translating principles of motor learning to clinical populations has informed the interventions we choose and how we deliver them. Our expanded knowledge of motor learning has made physical therapists mindful of ways to set up practice to promote motor learning in individuals with neuropathology. For example, we now recognize that individuals with early to moderate Parkinson Disease demonstrate a relatively preserved motor learning capability but may require more repetition due to slower learning rates compared to non-disabled controls.2 Likewise, preliminary evidence now exists that learning is promoted when individuals poststroke receive reduced feedback frequency3 and external focus instructions,4, 5 similar to that seen in healthy, young adults. Conversely, individuals with visuospatial working memory deficits following stroke better learn multiple motor tasks by practicing in a blocked compared with random practice order; a result that diverges from the well-established contextual interference effect in healthy populations.6 Thus, translation from principles to practice is complex.
In the current issue, five articles represent different stages of work along the spectrum of translational motor learning research. Borich et al. show us that the changes in motor behavior associated with short-term motor learning in individuals with chronic stroke are related to measures of corticospinal tract integrity, suggesting that learning capacity may be linked to the functioning of specific brain pathways. Siengsukon and Al-Sharman demonstrate that sleep is likely an important contributor to consolidation, which is a time-dependent process in which a motor behavior becomes relatively more permanent. Vasudevan et al. show that the capability of individuals with traumatic brain injury to perform a short-term locomotor adaptation on a split-belt treadmill is altered, but in a way that is distinct from other patient types, such as patients with cerebral stroke or cerebellar damage. In a case study from Kesar et al., motor learning-driven changes in functional performance post-stroke are compared longitudinally within and between sessions. Finally, Winstein et al. provide a timely historical review of motor learning research and the motivation for and clinical examples of a novel approach to clinical care, featuring patient-centered motor learning principles.
While these studies demonstrate that considerable progress has been made, the direct application of motor learning research into physical therapy practice is far from complete. Several basic principles of motor learning established in healthy populations have not been studied in the context of pathology. Principles that have been applied to clinical populations such as the studies described above have yet to be put to the test in large-scale clinical trials. Many questions remain, including: What is the impact of practice schedule and structure on long-term retention? What dosage of task practice is sufficient to induce relatively permanent skill acquisition and better outcomes? How do the magnitude, form and timing of feedback influence performance and retention? Do different patient populations respond differently to different motor learning approaches? In a similar vein, several areas of emerging motor learning-based rehabilitation research will play an important role in improving physical therapy practice. These include: (1) understanding the role of cognition, attention, motivation, and active participation in motor learning; (2) utilizing patient-specific and individualized approaches to achieve optimal motor learning; and (3) incorporating technology-based learning devices, such as point-of-care home monitoring devices. Ideally, all clients’ plans of care would take into account the motor learning mechanisms that are intact and can therefore be capitalized upon, as well as those that are deficient and will therefore require additional training or alternative strategies.
As it is a primary goal of the physical therapist to maximize a patient’s capability to perform and retain skilled action, the partnership between the fields of motor learning and neurorehabilitation continues to flourish. There is little doubt that as more knowledge is gained, the application of these principles will continue to drive practice.
Figure 1.
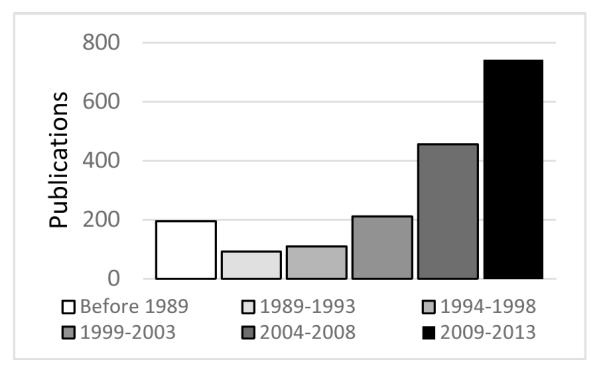
Exponential rise in the number of research articles found in PubMed that contained the search terms “motor learning” and “rehabilitation” and limiting the results to studies in human subjects.
References
- 1.Pascual-Leone A, Amedi A, Fregni F, Merabet LB. The plastic human brain cortex. Annual review of neuroscience. 2005;28:377–401. doi: 10.1146/annurev.neuro.27.070203.144216. [DOI] [PubMed] [Google Scholar]
- 2.Nieuwboer A, Rochester L, Muncks L, Swinnen SP. Motor learning in parkinson’s disease: Limitations and potential for rehabilitation. Parkinsonism Relat Disord. 2009;15(Suppl 3):S53–58. doi: 10.1016/S1353-8020(09)70781-3. [DOI] [PubMed] [Google Scholar]
- 3.Winstein CJ, Merians AS, Sullivan KJ. Motor learning after unilateral brain damage. Neuropsychologia. 1999;37:975–987. doi: 10.1016/s0028-3932(98)00145-6. [DOI] [PubMed] [Google Scholar]
- 4.Fasoli SE, Trombly CA, Tickle-Degnen L, Verfaellie MH. Effect of instructions on functional reach in persons with and without cerebrovascular accident. Am J Occup Ther. 2002;56:380–390. doi: 10.5014/ajot.56.4.380. [DOI] [PubMed] [Google Scholar]
- 5.van Vliet PM, Wulf G. Extrinsic feedback for motor learning after stroke: What is the evidence? Disabil Rehabil. 2006;28:831–840. doi: 10.1080/09638280500534937. [DOI] [PubMed] [Google Scholar]
- 6.Schweighofer N, Lee JY, Goh HT, Choi Y, Kim SS, Stewart JC, et al. Mechanisms of the contextual interference effect in individuals poststroke. J Neurophysiol. 2011;106:2632–2641. doi: 10.1152/jn.00399.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]


