Abstract
Purpose
Concomitant type 2 diabetes (T2D) and metabolic syndrome exacerbates mortality risk; yet, few studies have examined the effect of combining (AER+RES) aerobic (AER) and resistance (RES) training for individuals with T2D and metabolic syndrome.
Methods
We examined AER, RES, and AER+RES training (9-months) commensurate with physical activity guidelines in individuals with T2D (N=262, 63% female, 44% black). Primary outcomes were change in, and prevalence of, metabolic syndrome score at follow-up (mean, 95%CI). Secondary outcomes included maximal cardiorespiratory fitness (VO2peak and estimated METs from time-to-exhaustion (TTE), and exercise efficiency calculated as the slope of the line between ventilatory threshold, respiratory compensation, and maximal fitness. General linear models and bootstrapped Spearman correlations were used to examine changes in metabolic syndrome associated with training primary and secondary outcome variables.
Results
We observed a significant decrease in metabolic syndrome scores (P-for-trend, 0.003) for AER (−0.59, 95%CI, −1.00, −0.21) and AER+RES (−0.79, 95%CI, −1.40, −0.35), both being significant (P < 0.02) vs. Control (0.26, 95%CI, −0.58, 0.40) and RES (−0.13, 95%CI, −1.00, 0.24). This lead to a reduction in metabolic syndrome prevalence for the AER (56% vs. 43%) and AER+RES (55% vs. 46%) groups between baseline and follow-up. The observed decrease in metabolic syndrome was mediated by significant improvements in exercise efficiency for the AER and AER+RES training groups (P<0.05), which was more strongly related to TTE (25–30%; r= −0.38; 95% CI: −0.55, −0.19) than VO2peak (5–6%; r= −0.24; 95% CI: −0.45, −0.01).
Conclusion
Aerobic and AER+RES training significantly improves metabolic syndrome scores and prevalence in patients with T2D. These improvements appear to be associated with improved exercise efficiency and are more strongly related to improved TTE versus VO2peak.
Keywords: Exercise efficiency, metabolic syndrome, Metabolic Equivalents (METs), Aerobic and resistance training
INTRODUCTION
It is well recognized that the metabolic syndrome is an independent risk factor for cardiovascular disease, type 2 diabetes (T2D) cancer and all-cause mortality (1). Individuals with T2D who present with coexisting metabolic syndrome are not only at a higher risk for respective morbidities, but show additional risk for each accrued metabolic syndrome component feature than those without T2D (17, 27). Given the system-wide physiological benefits associated with exercise training the continued advocacy for exercise training is of paramount importance for individuals presenting with T2D and metabolic syndrome simultaneously.
Research continues to show that a low percentage of individuals meet recommended physical activity guidelines throughout the world and that these statistics deteriorate as one transitions from childhood through adulthood and ageing (24) These statistics worsen in the presence of various disease states (19, 24) Fundamental to most recommendation statements is the advocacy for aerobic (AER) and more recently, resistance (RES; (4). Resistance training is an important addition to healthcare as the combination of modalities (AER+RES) may be equally, if not more beneficial to health in some cases (10, 30). In 2007, Sigal et al. demonstrated in the DARE trial that AER+RES proved more beneficial for reducing haemoglobin A1C (HbA1c) and some components associated with metabolic syndrome than AER or RES alone (30). However, the time commitment was approximately 150 minutes for the AER and RES training groups, respectively, with AER+RES training in DARE for approximately 270 min/wk (30). This latter time commitment may be more than most individuals are willing to adopt given the low rates of exercise participation observed in most countries (7).
We recently reported in the HART-D trial that an exercise intervention using the same treatment strategy as DARE, yet modelled for time commitment according to current physical activity recommendations, also demonstrated a greater reduction in HBA1c and increased peak cardiorespiratory capacity (VO2peak) associated with AER+RES training (4, 10) We also showed that AER+RES training in HART-D significantly improved several aspects of skeletal muscle mitochondrial content and substrate oxidation (31). While the primary outcome reports from DARE and HART-D examined various components of metabolic syndrome, neither study has evaluated the effect of exercise training on the prevalence of metabolic syndrome when examined as a composite score of the respective components comprising metabolic syndrome. The analysis of metabolic syndrome is important given a recent report by Bateman et al. (2011) demonstrating that while RES training did not affect metabolic syndrome, AER and AER+RES training decreased metabolic syndrome scores similarly in individuals who were sedentary, overweight, and dyslipidemic (6). Collectively, the physiologic response to exercise training is of primary importance to patient care for individuals with T2D and concomitant metabolic syndrome. A secondary challenge to these types of investigations is the attempt to reconcile the modest, yet potentially important differences, between epidemiologic reports and clinical trial outcomes.
Epidemiology trials examining maximal cardiorespiratory fitness (fitness) often report fitness in terms of Metabolic Equivalent Tasks or METs calculated at time-to-exhaustion (TTE) due the inability to measure respiratory gas exchange in large trials. Based on epidemiology findings, it has been estimated that a 1 MET improvement carries with it a 13–19% reduction in all-cause and CVD mortality risk, respectively (20, 21). We have recently demonstrated a dose dependent decrease in metabolic syndrome associated with fitness from the Aerobics Center Longitudinal Study and more recently an improvement in metabolic syndrome in postmenopausal women exercising in accordance with physical activity guidelines (11, 14). Despite the protective effects of fitness found in epidemiology, clinical exercise trials show a smaller effect when equating fitness expressed as METs calculated directly from VO2peak despite a more pronounced improvement in METs measured from work output at TTE within the same trial (10, 11). This disparity is important to consider as the true impact of clinical trials using VO2peak as a “gold standard” may not be fully appreciated. While the differences between directly measured and estimated METs can be posited objectively to differences in actual versus estimated METs, it is also conceivable that the difference between changes in VO2peak and TTE/estimated METs could be explained by improvements in exercise efficiency. Based on the American College of Sports Medicine’s (ACSM) advocacy for “Exercise is Medicine,” we used an integrated approach aimed at reconciling laboratory measures with clinical outcomes and further examining their relationships to metabolic syndrome.
The primary aim of this analysis is to examine participants from the HART-D cohort to determine the relationship between AER, RES and AER+RES training and metabolic syndrome in participants with T2D (10). We hypothesize that metabolic syndrome prevalence will improve in a “dose-dependent” manner moving in order of effect from RES, to AER, to AER+RES training. Our secondary aim is to explore the relationship between metabolic syndrome and maximal fitness, whereby we propose that exercise efficiency will explain, at least in part, improvements in metabolic syndrome.
METHODS
The primary aim of the HART-D trial (N=262) was to examine the effect of 9-months AER, RES and AER+RES training on HbA1c in participants with T2D (10). Volunteers presented to HART-D as sedentary men and women (30–75 y) with T2D (HbA1C = 6.5% – 11.0%). We defined sedentary behavior as performing AER exercise < 20 minutes on < 3 days per week and not participating in RES. Individuals were excluded for the presence of or medical history of stroke, advanced neuropathy or retinopathy, or other serious medical condition contraindicated for exercise or that may prevent adherence to the study protocol. The Pennington Biomedical Research Center institutional review board approved the HART-D study, and written consent was obtained from all participants prior to study screening. All study procedures were performed in accordance with the Declaration of Helsinki.
Herein we present an ancillary, per-protocol report of 208 participants who completed the HART-D trial and were more than 70% compliant to the exercise protocol. No between group differences were noted for compliance. As previously reported by Church et al (2010), weekly exercise time did not differ significantly between the AER (140 min), RES (141 min) and AER (110 min) +RES (35 min) groups (total, 145 min). Moreover, no significant differences were noted for changes in body composition changes between groups relative body fat or lean body mass (10).
Study Design and Intervention
Volunteers who met inclusion criteria were randomized to AER, RES, or AER+RES, or a non-exercise control group (Control). During the study, we maintained separate intervention and assessments teams and clinical testing and intervention laboratories were housed in separate buildings. During the course of the trial, participants met with a certified diabetes educator each month to track medication and health history changes and all exercise sessions were constantly monitored by trained study staff. The Control group was offered weekly stretching and relaxation classes. Participants randomized to the Control group were asked to maintain their normal daily physical activity level throughout the intervention. We confirmed physical activity levels outside of exercise training sessions using step counters. The stretching and relaxation classes were optional and considered light intensity physical activity insufficient to influence fitness or produce significant increases in strength. It should be noted, however, that during the course of the study, data safety monitoring procedures caused us to discontinue the Control group after a significant number of participants (~17%) had an increase in HbA1C > 1.0%, resulting in an unequal number of participants in the Control group.
The AER and AER+RES groups participated in treadmill walking 3 – 5 days per week at a moderate to vigorous intensity (65.4 ± 14.6% of VO2peak, mean ± SD). The exercise dose in the AER group was prescribed at 12 kcal per kg body weight per week (KKW), which was estimated to be equivalent to ~150 min/wk. Participants were weighed weekly to calculate the prescribed weekly caloric energy expenditure rate estimated from standard equations published by the ACSM (2, 4). The time required per session was calculated by dividing the weekly dose by the estimated caloric expenditure rate and the total number of sessions completed that week. The AER dose was lowered to 10 KKW in the AER+RES group to accommodate the RES component and ensure equal time commitment across all exercise groups.
The RES group completed 3 days of strength training exercises per week consisting of 2 sets of 4 upper body exercises (bench press, seated row, shoulder press, and lat pull down), 3 sets of 3 lower body exercises (leg press, extension, and flexion), and 2 sets of abdominal crunches and back extensions. Each set consisted of 10–12 repetitions and the amount of weight lifted was progressively increased once a participant was able to complete 12 repetitions on the final set of an exercise on 2 consecutive RES sessions. Participants in the AER+RES group completed 2 sessions of RES each week, each consisting of 1 set of 10–12 repetitions for all resistance exercises.
Measurements
Metabolic Syndrome and Cardiorespiratory Capacity
The primary outcome for our analysis is metabolic syndrome score as defined by NCEP ATP III guidelines (defined in Statistical section; (1). Cardiorespiratory fitness was evaluated using a standardized, ECG monitored, treadmill test while simultaneously collecting respiratory gases sampled from a True Max 2400 Metabolic Measurement Cart (ParvoMedics, Salt Lake City, Utah). From this test we measured METs from peak oxygen consumption (VO2peak; ml/kg/min ÷ 3.5) and (2) according to ACSM calculations based on speed and grade obtained at the end of exercise testing (3). Our rational for examining VO2peak and TTE is based on our desire to detail the clinical/physiologic changes surrounding VO2peak and the epidemiological index of time-to-exhaustion, as well as ascertaining exercise efficiency (detailed below).
To examine exercise efficiency we first calculated the ventilatory threshold (VT) using the V-slope method by plotting VO2 and VCO2 on the x- and y-axes, respectively, and visually examining the slope of the relationship for a breakpoint in linearity (32). We also calculated the respiratory compensation point attained during each test as an increase in the ventilatory equivalent of oxygen (VE/VO2) and end-tidal partial pressure of oxygen (PETO2) with no concomitant increase in the ventilatory equivalent of carbon dioxide (VE/VCO2) to confirm these findings (25). Of note, in the literature VT and RCP are sometimes referred to as ventilatory threshold 1 (VT1) and 2 (VT2), respectively] (8) For consistency we will use the abbreviations VT1 and VT2]. Thereafter, to determine exercise efficiency, we calculated the slope of the line between the time of onset of VT1, VT2, and TTE.
Blood Chemistries and Anthropometric Measures
Hemoglobin A1c was obtained by venipuncture after a 10-h fast and analyzed with a Beckman Coulter DXC600 Pro (Brea, CA). Weight was measured on a GSE 450 electronic scale (GSE Scale Systems, Novi, Michigan) and height was measured using a standard stadiometer. Body mass index (BMI) was calculated as follow: body weight (kg)/height (m2). Waist circumference was measured to the nearest 0.1 cm at the level of the iliac crest while the subject was at minimal expiration. Body composition was measured by dual-energy x-ray absorptiometry using the QDR 4500A whole-body scanner (Hologic Inc., Bedford, MA).
Statistical Methods
The primary outcome for our analysis is metabolic syndrome prevalence and score. Metabolic syndrome is defined as presenting with three of the following features: (1) increased waist circumference (>102 cm [>40 in] for men, >88 cm [>35 in] for women); (2) elevated triglycerides (≥150 mg/dl); (3) low HDL cholesterol (<40 mg/dl in men, <50 mg/dl in women); (4) hypertension (systolic blood pressure ≥130and and/or diastolic blood pressure ≥85 mmHg); (5) impaired fasting glucose (≥110 mg/dl).
For secondary outcomes we examined changes in respective metabolic syndrome component versus changes between the components features of metabolic syndrome and METs calculated from VO2peak and estimated from TTE. For exploratory purposes, we also examined the relationship between exercise efficiency and metabolic syndrome.
For our primary and secondary analyses we used a generalized linear model to analyse the influences of the differing regimens of exercise training on metabolic syndrome (SPSS version 21.0, Somers, NY). Relationships for our tertiary analysis were performed using a Spearman correlation analysis for changes in metabolic syndrome versus changes cardiorespiratory fitness, metabolic syndrome components, and anthropometry indices as independent variables. For this latter analysis, we performed a bootstrap analysis of our data using 1,000 imputations. Bootstrapping was used in order to improve the accuracy of confidence intervals surrounding various correlations as we reasoned that (1) our cohort continued their medication use during the study and (2) owing to our original report, the participants in our study reduced medication use concurrent with exercise training (10). Subsequently, any change in medication use surrounding metabolic syndrome components would likely influence our analysis effectively reducing the magnitude of changes in metabolic syndrome.
Based on our primary outcome paper, all of our analyses were covaried for age, ethnicity, duration of T2D, baseline HbA1c and baseline and follow-up medications used for T2D, blood pressure, and cholesterol. We also included baseline metabolic syndrome score within this analysis. Within group differences between baseline and follow-up are reported as mean and 95% confidence intervals (95% CI). When we observed significant trends, we further explored our findings using a priori comparisons between each exercise training group vs. the Control group via Dunnett-Hsu post-hoc assessments. All reported P-values are two-sided (P<0.05) and our analyses accounts for Dunnett-Hsu adjustments when reported. Data are presented as Mean ± SD or mean change from baseline and 95% confidence intervals as appropriate.
RESULTS
The demographic characteristics and clinical features of our cohort (N = 262) are presented in Table 1. For our exploratory analyses of exercise efficiency, we successfully examined 207 participants who had complete data for each variable examined. No significant differences were observed for maximal fitness characteristics or percentage presenting with metabolic syndrome between the entire cohort and our tertiary assessment so we have presented all fitness characteristics in Table 2. Overall, participants presented with an average age of 56 ± 9 y and T2D duration of 7.1 ± 5.5 y and 59% of our cohort presented with metabolic syndrome. Based on BMI (34.9 ± 5.9 kg/m2) participants in our study ranged from class I to class III obese.
Table 1.
Baseline characteristics of study participants
| All (N = 262) |
Control (n = 41) |
Aerobic (n = 72) |
Resistance (n = 73) |
Aerobic + Resistance (n = 76) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Characteristics | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD |
| Age (y) | 56 | 9 | 59 | 8 | 54 | 9 | 57 | 9 | 55 | 8 |
| Gender (N, %) | ||||||||||
| Male | 97 | 37% | 13 | 5% | 27 | 10% | 30 | 11% | 27 | 10% |
| Female | 165 | 63% | 28 | 11% | 45 | 17% | 43 | 16% | 49 | 19% |
| Race (N, %) | ||||||||||
| White | 138 | 53% | 22 | 8% | 39 | 15% | 41 | 16% | 36 | 14% |
| Black | 114 | 44% | 17 | 7% | 33 | 13% | 30 | 12% | 34 | 13% |
| Hispanic | 1 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | 1 | 0% |
| Asian | 8 | 3% | 2 | 1% | 0 | 0% | 2 | 1% | 4 | 2% |
| Other | 1 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | 1 | 0% |
| Duration of Diabetes (y) | 7.1 | 5.5 | 7.2 | 5.2 | 7.4 | 6.0 | 7.2 | 5.5 | 6.7 | 5.4 |
| Metabolic Syndrome | ||||||||||
| Metabolic Syndrome Score | 2.77 | 0.93 | 2.63 | 0.86 | 2.99 | 0.91 | 2.7 | 0.88 | 2.72 | 1.03 |
| Presenting (%) | 59% | 56% | 56% | 56% | 55% | |||||
| Follow-up (%) | 49% a | 54% | 43% a | 53% | 46% a | |||||
| Anthropometry | ||||||||||
| Height (cm) | 167.78 | 9.2 | 166.78 | 9.9 | 167.89 | 10.1 | 168.72 | 9 | 167.31 | 8 |
| BMI (kg/m2) † | 34.86 | 5.9 | 34.84 | 6.2 | 34.65 | 6.1 | 34.07 | 5.4 | 35.82 | 6.2 |
| Weight (kg) | 98.18 | 18.8 | 97.03 | 20 | 97.54 | 18.6 | 96.92 | 16.6 | 100.61 | 20.4 |
| Body fat (%) | 37.81 | 7.3 | 38.48 | 7 | 37.12 | 7.7 | 37.04 | 7.6 | 38.84 | 6.8 |
| Waist Circumference (cm) * | 112.11 | 13.8 | 110.56 | 14.4 | 111.29 | 14.2 | 110.9 | 12.2 | 114.89 | 14.5 |
| Haematology †† | ||||||||||
| HBA1C (%) | 7.33 | 1.2 | 7.71 | 1.5 | 7.3 | 1.2 | 7.18 | 1 | 7.3 | 1.2 |
| Glucose (mg/dL) * | 151.02 | 36.4 | 158.44 | 40.7 | 146.36 | 30.6 | 153.77 | 39.3 | 148.77 | 35.9 |
| Insulin (pmol/L) | 21.89 | 32.5 | 17.65 | 14.7 | 18.46 | 16.5 | 20.37 | 14.7 | 28.9 | 54.9 |
| Triglycerides (mg/dL) * | 147.11 | 78.2 | 162.88 | 86.3 | 136.25 | 66.5 | 152.99 | 77.6 | 143.24 | 83.9 |
| Total cholesterol (mg/dL) | 174.08 | 34.6 | 184.71 | 31.2 | 168.82 | 32.2 | 174.39 | 34.1 | 172.96 | 38.2 |
| HDL (mg/dL) * | 49.35 | 11.5 | 50.39 | 9.5 | 48.95 | 13.4 | 49.43 | 12.1 | 49.07 | 10 |
| LDL cholesterol (mg/dL) | 95.48 | 29.4 | 102.6 | 25.8 | 92.45 | 28.3 | 94.09 | 30.4 | 95.88 | 31.1 |
| Blood Pressure (mmHg) | ||||||||||
| Systolic (mmHg) * | 126.2 | 13.1 | 127.1 | 13.9 | 124.4 | 12.5 | 124.1 | 12.5 | 129.4 | 13.5 |
| Diastolic (mmHg) * | 75.6 | 8.5 | 76.4 | 8 | 75.8 | 9.4 | 75.1 | 8.2 | 75.34 | 8.3 |
Metabolic Syndrome according to NCEP ATP III criteria
Calculated as weight in kilograms divided by height in meters squared
SI conversions: To convert total, low-density lipoprotein, and high-density lipoprotein cholesterol to mmol/L, multiply by 0.0259; triglycerides to mmol/L, multiply by 0.0113; and fasting glucose to mmol/L, multiply by 0.0555, insulin to uU/mL multiply by 0.144.
Significantly different than baseline (P<0.05)
Table 2.
Baseline cardiorespiratory fitness characteristics of HART-D study participants
| Treatment Group | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| All (N = 207) | Control (n = 33) | Aerobic (n = 54) |
Resistance (n = 59) |
Aer + Res (n = 61) | ||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Ventilatory Threshold (VT1) | ||||||||||
| Time-of-onset (sec) | 169.73 | 75.6 | 160.50 | 118.0 | 165.69 | 61.3 | 181.72 | 70.6 | 166.89 | 62.7 |
| Respiratory Compensation (VT2) | ||||||||||
| Time-of-onset (sec) | 460.75 | 134.9 | 433.85 | 123.5 | 465.30 | 151.0 | 470.52 | 130.8 | 463.56 | 131.3 |
| Maximal Cardiorespiratory Fitness | ||||||||||
| Maximal oxygen uptake (L/min) | 1.92 | .5 | 1.88 | .5 | 2.03 | .5 | 1.92 | .5 | 1.81 | .5 |
| Maximal oxygen uptake (ml/lg/min) | 20.12 | 4.3 | 19.66 | 3.2 | 21.18 | 5.3 | 20.41 | 4.5 | 18.94 | 3.3 |
| Maximal METs from maximal oxygen uptake * | 5.75 | 1.2 | 5.62 | .9 | 6.05 | 1.5 | 5.83 | 1.3 | 5.41 | .9 |
| Maximal METs from speed and grade | 8.57 | 1.3 | 8.47 | 1.2 | 8.66 | 1.5 | 8.62 | 1.3 | 8.48 | 1.3 |
| Time-to-exhaustion (sec) | 641.42 | 150.6 | 638.68 | 128.4 | 645.82 | 166.5 | 640.34 | 148.2 | 639.75 | 151.1 |
Maximal oxygen uptake (ml/kg/min) divided by 3.5; significant from calculated METs from speed and grade (P< 0.05).
Calculated METs derived from treadmill speed and grade.(ref ACSM)
Based on VO2peak (20.1 ± 4.3 ml/kg/min), participants in HART-D were low fit, ranking in the lower 15th percentile for maximal cardiorespiratory capacity achieved during exercise testing (3, 28). These VO2peak levels correspond to the Class I/II fitness levels as defined by the New York Heart Association (15). Fifty-nine percent of our cohort presented with metabolic syndrome at baseline. Sixty three percent of our cohort were women, 44% black, 3% Asian and 0.5% Hispanic. Ninety-seven percent of our cohort used diabetes medications, 79% blood pressure medications and 64% cholesterol medications at baseline.
Metabolic Syndrome
We have presented the results for our change in metabolic syndrome score analysis in Figure 1 where we observed a significant trend (P = 0.003) for a decrease in metabolic syndrome within the AER (−0.49; 95% CI: −0.77, −0.21) and AER+RES (−0.64; 95% CI: −0.92, −0.35) groups. Both of these changes were significant (P < 0.02) vs. Control (0.03; 95% CI: −0.33, 0.40) and RES (−0.03; 95% CI: −0.30, 0.24). These changes lead to a significant decrease in the percentage of participants presenting at baseline vs. follow-up with metabolic syndrome for the AER (56% vs. 43%) and AER+RES (55% vs. 45%) groups (both, P<0.05, Table 1). For our analysis of metabolic syndrome components, we observed a significant trend (P = 0.03) for reduced waist circumference improvement for all treatment groups: RES (−1.91 cm; 95% CI: −3.03, −0.78), AER (−1.58 cm; 95% CI: −2.76, −0.39), and AER+RES (−2.80 cm; 95% CI: −3.93, −1.67), with all treatment groups being significant vs. Control (0.67 cm; 95% CI: −0.82, 2.15), P < 0.05). We also observed a significant reduction in systolic blood pressure for the AER group (−6.61 mmHg; 95% CI: −6.00, −0.22), also significant vs. Control (P < 0.05). No other metabolic syndrome features changes were found to be statistically significant.
Figure 1.
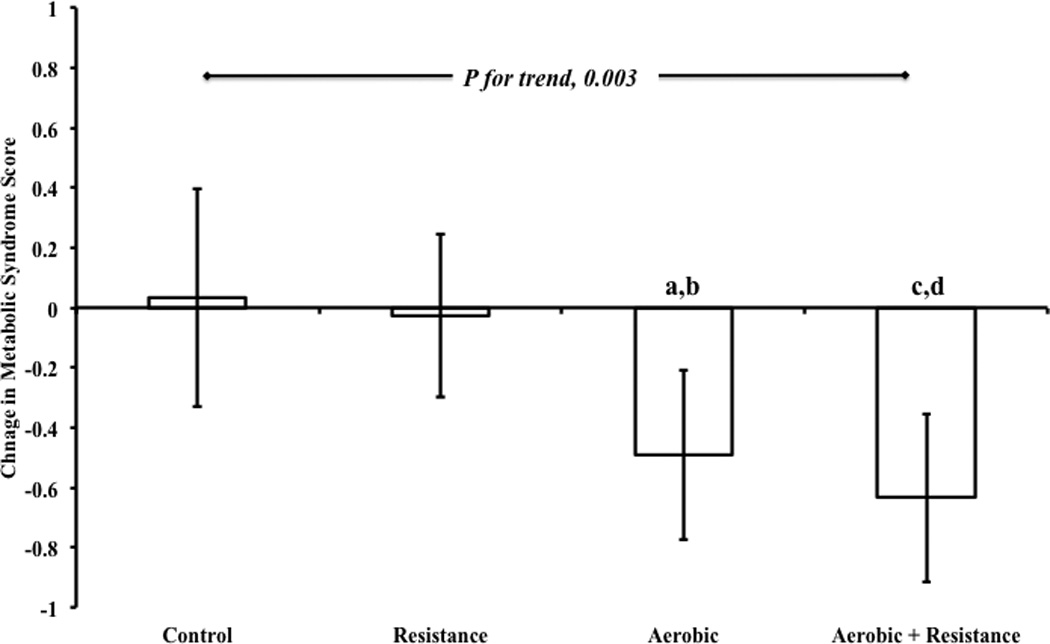
Represents mean change ± 95% CI in NCEP ATP III defined metabolic syndrome scores from baseline to follow-up. Statistical notations represent significance as:
a Aerobic vs. Control, P = 0.028
b Aerobic vs. Resistance P = 0.02
c Aerobic+Resistance vs. Control, P = 0.005
d Aerobic+Resistance vs. Resistance, P = 0.003.
Maximal Cardiorespiratory Capacity
Participants presented at baseline with an absolute VO2peak of 1.92 ± 0.5 L and relative VO2peak of 20.1 ± 4.3 ml/kg/min. This equated to a 5.8 ± 1.2 METs. Time-to-exhaustion during treadmill testing was 641 ± 151 seconds or approximately 10.7 ± 2.5 minutes. This equates to 8.57 ± 1.3 estimated METs. The mean METs measured from VO2peak were 5.75 ± 1.2 and significantly lower than METs estimated from speed and grade at TTE (P<0.05).
After 9 months of exercise training we observed a 5–6% increase in METs measured by gas exchange vs. a 25–30% increase in METs estimated from speed and grade. For measured METs, we observed minor, yet significant increases in the AER and AER+RES training (Fig. 2). However, no between-group differences were otherwise noted. For estimated METs, we also observed significant increases in the AER and AER+RES training groups that were (a) significantly different from measured METs and (b) significantly different from respective measured METs (P<0.05; Fig. 2).
Figure 2.
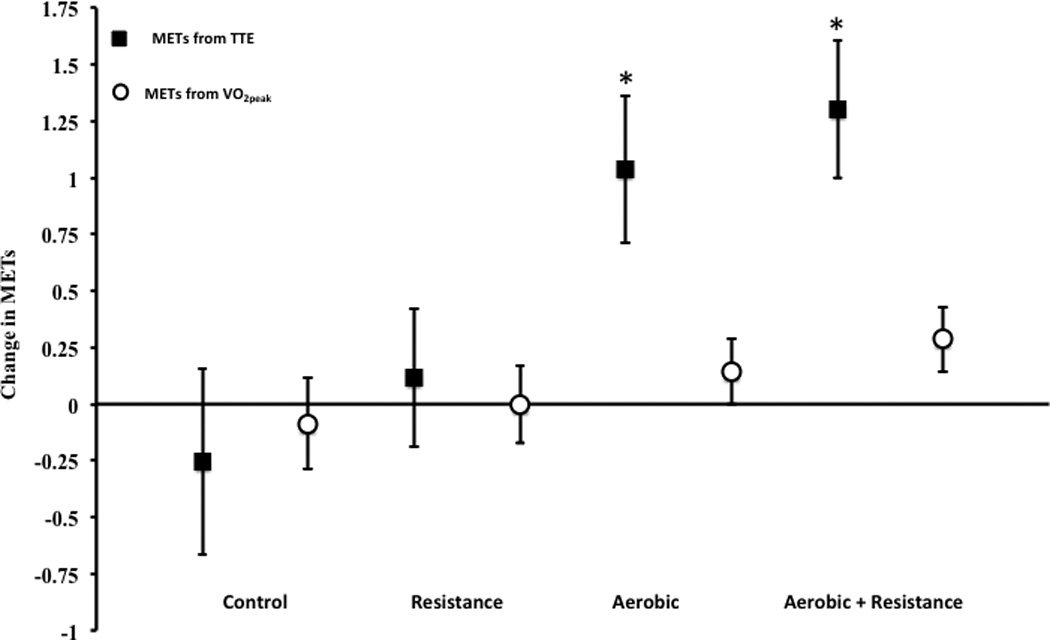
Represents mean change ± 95% CI in METs measured from V02peak and calculated from speed and grade at time-to-exhaustion during maximal treadmill testing. Statistical notations represent significance versus Control; * P < 0.03.
Changes in METs obtained directly from VO2peak were: Control (−0.09, 95% CI, −0.28, 0.11), RES (0.00, 95% CI, −0.14, 0.17), AER (0.14, 95% CI, 0.02, 0.28), AER+RES (0.29, 95% CI, 0.14, 0.42). Changes in METs calculated from speed and grade were: Control (−0.25, 95% CI, −0.66, 0.15), RES (0.12, 95% CI, −0.19, 0.42), AER (1.04, 95% CI, 0.71, 1.36), and AER+RES (1.30, 95% CI, 1.01, 1.61), with the AER and AER+RES being significantly greater than Control and RES (P <0.05).
Time-to-exhaustion following exercise training decreased in the Control group (−28 sec; 95% CI −76, 20) and showed a small increase for the RES (13 sec; 95% CI −23, 49) training group. Neither of these changes was statistically significant. However, a significant increase in TTE was observed for the AER (119 sec; 95% CI 81, 157) and AER+RES (154 sec; 95% CI: 118, 189) with both being significant vs. Control and RES groups (P < 0.05; Fig. 3c).
Figure 3.
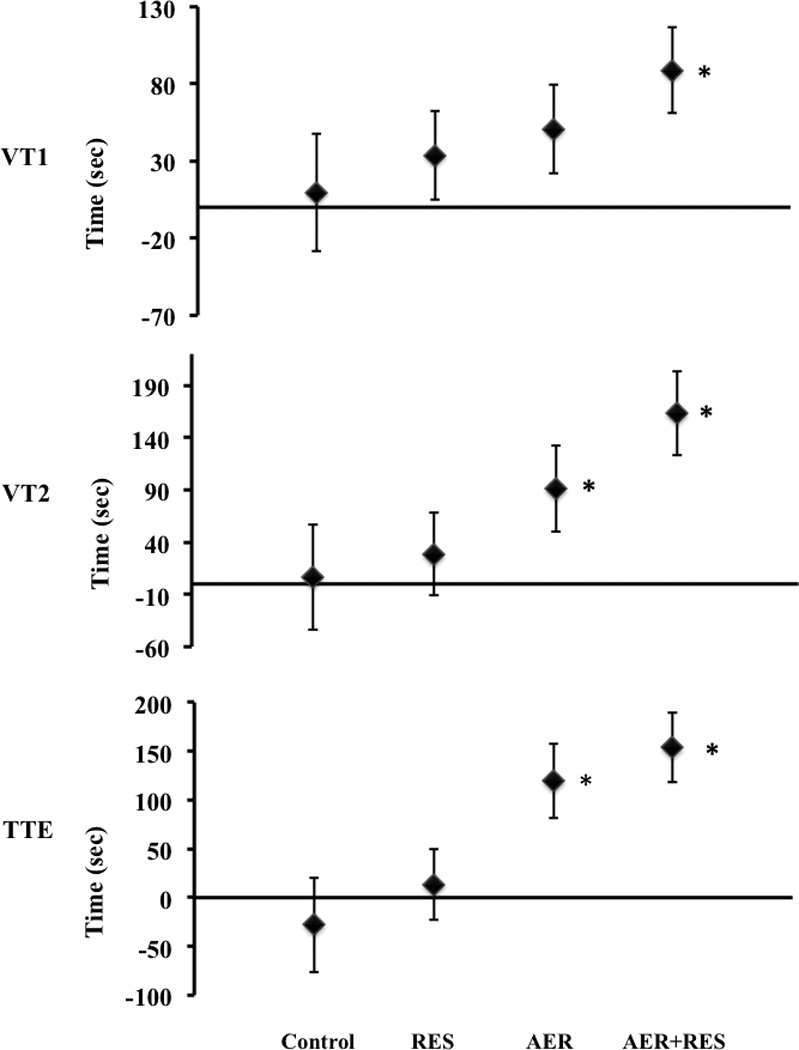
Data represent mean ± 95% CI changes VT1 (top panel), VT2 (middle panel) and time-to-exhaustion (TTE, bottom panel). Statistical notations represent significance versus Control; * P < 0.03.
Sub-maximal Cardiorespiratory Indices and Exercise Efficiency
Similar observations to TTE were noted for the time-to-onset of VT1 (Fig. 3b) and VT2 (Fig. 3c). However, while VT1 improved in all treatment groups, VT2 improved only in the AER and AER+RES training groups compared to baseline. Specifically, VT1 (Fig. 3b) did not improve in the Control group (9.0 sec; 95% CI: −29, 47), but significantly increased in all treatment groups: RES (51 sec; 95% CI: 5, 63); AER (34 sec; 95% CI: 22, 80); AER+RES, (89 sec; 95% CI: 61, 117). For VT2 (Fig. 3c), no significant improvements were noted for the Control, (6 sec; 95% CI: −44, 56) or RES (28 sec; 95% CI: −11, 68) groups, but were significant for the AER (91 sec; 95% CI: 50, 133) and AER+RES (163 sec; 95% CI: 123, 203) groups (Fig. 3b). The net effect of these changes was a significant shift in the slope of the relationship from baseline to follow-up for VT1, VT2 and TTE whereas no significant improvements were observed for the Control group. Lastly, our analysis showed significant associations for changes between metabolic syndrome, TTE (r = −0.33; 95% CI: −0.49, −0.15), VO2peak(r = −0.24; 95%: −0.36, −0.05), and waist circumference (r = −0.14; 95% CI: −0.11, −0.40). No other significant associations were noted for other indices of body anthropometry.
DISCUSSION
The primary findings from our current study show that AER and AER+RES training reduce metabolic syndrome scores and, subsequently, the prevalence of individuals with concurrent T2D and metabolic syndrome. What is notable is that AER+RES performed in accordance with contemporary exercise guidelines is an effective strategy for reducing metabolic syndrome scores in individuals with T2D and should be considered as a viable treatment as preservation of muscle function becomes increasingly important with age (29). When examined as individual metabolic syndrome component features, we also found that waist circumference was significantly reduced in all exercise groups, while systolic blood pressure was significantly reduced only in the AER group. No other significant component feature reductions were noted for metabolic syndrome. These findings are clinically important to individuals who present with T2D, low cardiorespiratory fitness, and metabolic syndrome simultaneously.
Previous research shows a greater CVD and all-cause mortality risk for individuals who have coexisting metabolic syndrome and T2D (17, 27). In 2006, Guzder et al. (2006) demonstrated that age, sex, smoking status, total cholesterol, antiplatelet therapy, antihypertensive therapy, and lipid lowering therapy-adjusted survival curves in patients with conjoint metabolic syndrome and T2D exhibited a hazard ratio (HR) for incident CVD of 2.05 compared to individuals with T2D alone. Under the assumption that the presence of T2D qualified all participants with a minimum of one metabolic syndrome feature, compounding risk was also observed for the accretion of two (HR, 1.93 ± 0.39), three (HR 2.71 ± 0.18), four (HR, 4.23 ± 0.56), or and all five (HR, 4.76 ± 0.042) metabolic syndrome component features. Najarian et al. (2006) have also shown in data in the Framingham Study that the relative risk of stroke in individuals with T2D and metabolic syndrome is approximately 32%–55% higher compared with those individuals presenting with T2D or metabolic syndrome alone (27). Previous reports from our group in men show similar findings (12). In a prospective report from the Aerobics Center Longitudinal Study, we found that CVD deaths were higher in individuals with T2D alone (5.5/1,000 man years; HR: 2.9; 95% CI: 2.1, 4.0) and in combination with metabolic syndrome 6.5/1,000 man years; HR: 3.4; 95% CI: 2.8, 4.2) vs. men without T2D or metabolic syndrome (1.9/1,000 man years) or metabolic syndrome only (3.3/1,000 man years; HR: 1.8; 95% CI: 1.5, 2.0, (12).
Epidemiology trials also demonstrate that AER and RES are inversely and independently associated with metabolic syndrome (9, 14, 18). While clinical exercise intervention trials also support the efficacy of AER or RES training for reducing metabolic syndrome, less is known about combining AER+RES training, especially for those presenting with T2D and metabolic syndrome. A difficulty in interpreting the current literature with regard to the RES training aspect of metabolic syndrome is a relative paucity of trials examining RES training on metabolic syndrome versus examining the role of RES on the individual component features of metabolic syndrome. This difficulty is exemplified in a recent systematic and meta-analysis by Strasser et al. (2010), who examined 13 trials involving RES and metabolic syndrome. While the authors provided an excellent review of RES training on the component features of metabolic syndrome, they did not account for metabolic syndrome as a composite score. Fewer reports still have examined the effect of AER+RES training in metabolic syndrome.
Similar in nature to HART-D, Sigal et al. reported in the DARE trial significant reductions in HBA1c coinciding with AER, RES and AER+RES training (30). Despite the reporting of metabolic syndrome composite features, no further analysis was undertaken to examine metabolic syndrome itself. To date, only the study of Bateman et al. (20011) has examined the effects of AER+RES on metabolic syndrome in participants from the STRRIDE study (6). Though STRRIDE did not examine individuals with T2D, they demonstrated similar effects to our current report in a convenience sample of 84 out of 196 individuals presenting with all five NCEP ATP III defined metabolic syndrome components. Specifically, participants in AER and AER+RES training decreased metabolic syndrome, while those undertaking RES and Control conditions showed no significant reductions in metabolic syndrome. Overall, the findings of HART-D and STRRIDE demonstrate that AER and AER+RES training are equally effective for reducing metabolic syndrome in T2D and non-diabetic individuals, respectively.
The biological effects of exercise training on metabolic syndrome are related to changes in a number of physiologic and cardiovascular adaptations to exercise training and have been thoroughly reviewed elsewhere and are not elaborated on here (16). However, an underlying question we posed when undertaking our current analysis was to examine potential differences between clinical trials that rely on laboratory measure of VO2peak and epidemiologic trials that typically use TTE and corresponding estimated MET values. One of the features we observed in some of our trials, inclusive of HART-D, was a disparity between the relative increase in measured VO2peak and TTE (10, 11). In our current analysis, we observed a significant difference between MET values measured from VO2peak or measured METs (5–6%) and TTE or estimated METs (25–30%), with the latter showing a stronger relationship with metabolic syndrome. It is easy to rationalize this apparent inequality in terms of the mathematical variance associated with estimating METs from an equation based on speed and grade versus the actual measurement of VO2peak. This disparity, however, makes it difficult to reconcile epidemiology and clinical trials as data from epidemiology trials suggest a 13% and 15% reduction in all-cause and CVD risk mortality, respectively, for each METs attained during exercise testing (20). Rather than assuming that the difference between the two measures was simply a matter of the mathematical variance introduced with prediction equations, we hypothesized that some of this disparity could be explained by improvements in exercise efficiency.
Our findings showing significant, yet higher correlations for estimated METs compared with VO2peak or measured METs are intriguing. Though both measurements detail “maximal cardiorespiratory capacity,” per se and may covary to some degree, they also reflect differences in the physiologic response to graded exercise testing. While VO2peak reflects changes in measured cardiorespiratory capacity, which, in and of itself is a reflection of maximal cardiac output and muscle oxygen utilization, TTE may reflect an improvement in sub-maximal exercise efficiency. Unfortunately, little data exists examining this relationship. Numerous methods have been proposed to measure exercise efficiency in athletic and clinical populations including mechanical efficiency, gross efficiency, delta efficiency, oxygen uptake efficiency slope, and others (5, 13, 22, 23, 26). While all of these methods have their strengths and weaknesses, each measure is largely dependent on a single point of observation or on the slope of the changing relationship between the oxygen uptake of sequential stages, and hence, the workload involved in exercise testing.
We have examined the slope of the relationship between VT1, VT2 and maximal exercise, finding that the slope of this relationship improved in the AER and AER + RES groups and that these changes were more strongly related to TTE than measured VO2peak. From these data, we conclude that exercise training improves the underlying physiology associated with exercise testing and that these improvements equate to an improvement in TTE, and subsequently, partially explain the difference between estimated METs vs. those obtained from laboratory derived VO2peak.
A primary strength of HART-D is that it was a highly controlled clinical exercise intervention lasting 9-months. Our study is limited in its generalizability to those with T2D. Still, findings from STRRIDE suggest that the findings are similar in those without T2D. It might also be argued that given the medical management (i.e., prescriptive medications) surrounding our cohort could have introduced uncontrollable statistical variance into our reported outcomes. It may also be argued that the RES stimulus was not sufficient to affect changes in metabolic syndrome components similar to AER regardless of the fact that the study was 9-months in length. Future studies using RES training should therefore consider the training intensity and volume components of RES. From a clinical perspective, we have accounted for changes in medication within our statistical analysis by using baseline and follow-up medication use. This, in turn, strengthens our findings, as they are standard measures of clinical care and patient healthcare management. One of the strongest features of our study is that it was designed to emulate current public guideline statements for exercise. Taken in combination our results show that AER or AER+RES training plays an important role in the management of individuals with T2D who also present with sufficient qualifying components to also have metabolic syndrome.
Acknowledgements
This study was supported by a grant from the National Institutes of Health (DK0-68298) and the results of the present study do not constitute endorsement by ACSM.
We wish to thank all HART-D participants and Pennington Biomedical Research Center staff members who contributed to the main HART-D outcome.
Dr. Church receives honoraria for lectures from scientific, educational, and lay groups. Dr. Church has a book entitled “Move Yourself: The Cooper Clinic Medical Director’s Guide to All the Healing Benefits of Exercise.” Dr. Church has received research funding from the American Heart Association and the National Institutes of Health as well as unrestricted research funding from Coca-Cola. Dr. Church has overseen study sites for large pharmaceutical trials funded by Sanofi Aventis, Orexigen, Arena and Amylin. Dr. Church is a member of the Jenny Craig Medical Advisory Board and has served as a consultant to Technogym, Trestle Tree, Vivus, Lockton-Dunning and Neuliven Health. In addition, he serves as the Senior Medical Advisor for Catapult Health
Footnotes
Disclosures
No other disclosures are otherwise noted.
REFERENCES
- 1.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC., Jr Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; International Association for the Study of Obesity. Circulation. 2009 Oct 20;120(16):1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 2.Albright A, Franz M, Hornsby G, Kriska A, Marrero D, Ullrich I, Verity LS. American College of Sports Medicine position stand. Exercise and type 2 diabetes. Med Sci Sports Exerc. 2000;32(7):1345–1360. doi: 10.1097/00005768-200007000-00024. [DOI] [PubMed] [Google Scholar]
- 3.American College of Sports Medicine Guidelines for Exercise Testing and Prescription. 4th ed. Lea & Febiger; 1991. pp. 285–300. [Google Scholar]
- 4.American College of Sports Medicine Position Stand. The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Medicine and science in sports and exercise. 1998 Jun;30(6):975–991. doi: 10.1097/00005768-199806000-00032. [DOI] [PubMed] [Google Scholar]
- 5.Baba R, Nagashima M, Goto M, Nagano Y, Yokota M, Tauchi N, Nishibata K. Oxygen uptake efficiency slope: a new index of cardiorespiratory functional reserve derived from the relation between oxygen uptake and minute ventilation during incremental exercise. Journal of the American College of Cardiology. 1996 Nov 15;28(6):1567–1572. doi: 10.1016/s0735-1097(96)00412-3. [DOI] [PubMed] [Google Scholar]
- 6.Bateman LA, Slentz CA, Willis LH, Shields AT, Piner LW, Bales CW, Houmard JA, Kraus WE. Comparison of aerobic versus resistance exercise training effects on metabolic syndrome (from the Studies of a Targeted Risk Reduction Intervention Through Defined Exercise - STRRIDE-AT/RT) The American journal of cardiology. 2011 Sep 15;108(6):838–844. doi: 10.1016/j.amjcard.2011.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bauman A, Bull F, Chey T, Craig CL, Ainsworth BE, Sallis JF, Bowles HR, Hagstromer M, Sjostrom M, Pratt M. The International Prevalence Study on Physical Activity: results from 20 countries. The international journal of behavioral nutrition and physical activity. 2009;6:21. doi: 10.1186/1479-5868-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beaver WL, Wasserman K, Whipp BJ. A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol. 1986 Jun;60(6):2020–2027. doi: 10.1152/jappl.1986.60.6.2020. [DOI] [PubMed] [Google Scholar]
- 9.Brage S, Wedderkopp N, Ekelund U, Franks PW, Wareham NJ, Andersen LB, Froberg K. Features of the metabolic syndrome are associated with objectively measured physical activity and fitness in Danish children: the European Youth Heart Study (EYHS) Diabetes care. 2004 Sep;27(9):2141–2148. doi: 10.2337/diacare.27.9.2141. [DOI] [PubMed] [Google Scholar]
- 10.Church TS, Blair SN, Cocreham S, Johannsen N, Johnson W, Kramer K, Mikus CR, Myers V, Nauta M, Rodarte RQ, Sparks L, Thompson A, Earnest CP. Effects of aerobic and resistance training on hemoglobin A1c levels in patients with type 2 diabetes: a randomized controlled trial. JAMA. 2010 Nov 24;304(20):2253–2262. doi: 10.1001/jama.2010.1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Church TS, Earnest CP, Skinner JS, Blair SN. Effects of different doses of physical activity on cardiorespiratory fitness among sedentary, overweight or obese postmenopausal women with elevated blood pressure: a randomized controlled trial. JAMA. 2007 May 16;297(19):2081–2091. doi: 10.1001/jama.297.19.2081. [DOI] [PubMed] [Google Scholar]
- 12.Church TS, Thompson AM, Katzmarzyk PT, Sui X, Johannsen N, Earnest CP, Blair SN. Metabolic syndrome and diabetes, alone and in combination, as predictors of cardiovascular disease mortality among men. Diabetes care. 2009 Jul;32(7):1289–1294. doi: 10.2337/dc08-1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.de Koning JJ, Noordhof DA, Lucia A, Foster C. Factors affecting gross efficiency in cycling. Int J Sports Med. 2012 Nov;33(11):880–885. doi: 10.1055/s-0032-1306285. [DOI] [PubMed] [Google Scholar]
- 14.Earnest CP, Artero EG, Sui X, Lee DC, Church TS, Blair SN. Maximal estimated cardiorespiratory fitness, cardiometabolic risk factors, and metabolic syndrome in the aerobics center longitudinal study. Mayo Clinic proceedings Mayo Clinic. 2013 Mar;88(3):259–270. doi: 10.1016/j.mayocp.2012.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fletcher GF, Ades PA, Kligfield P, Arena R, Balady GJ, Bittner VA, Coke LA, Fleg JL, Forman DE, Gerber TC, Gulati M, Madan K, Rhodes J, Thompson PD, Williams MA American Heart Association Exercise CR, Prevention Committee of the Council on Clinical Cardiology CoNPA, Metabolism CoC, Stroke N, Council on E, Prevention. Exercise standards for testing and training: a scientific statement from the American Heart Association. Circulation. 2013 Aug 20;128(8):873–934. doi: 10.1161/CIR.0b013e31829b5b44. [DOI] [PubMed] [Google Scholar]
- 16.Ford ES, Li C. Physical activity or fitness and the metabolic syndrome. Expert Rev Cardiovasc Ther. 2006 Nov;4(6):897–915. doi: 10.1586/14779072.4.6.897. [DOI] [PubMed] [Google Scholar]
- 17.Guzder RN, Gatling W, Mullee MA, Byrne CD. Impact of metabolic syndrome criteria on cardiovascular disease risk in people with newly diagnosed type 2 diabetes. Diabetologia. 2006 Jan;49(1):49–55. doi: 10.1007/s00125-005-0063-9. [DOI] [PubMed] [Google Scholar]
- 18.Jurca R, Lamonte MJ, Church TS, Earnest CP, Fitzgerald SJ, Barlow CE, Jordan AN, Kampert JB, Blair SN. Associations of muscle strength and fitness with metabolic syndrome in men. Medicine and science in sports and exercise. 2004 Aug;36(8):1301–1307. doi: 10.1249/01.mss.0000135780.88930.a9. [DOI] [PubMed] [Google Scholar]
- 19.King AC, Blair SN, Bild DE, Dishman RK, Dubbert PM, Marcus BH, Oldridge NB, Paffenbarger RS, Jr, Powell KE, Yeager KK. Determinants of physical activity and interventions in adults. Medicine and science in sports and exercise. 1992 Jun;24(6 Suppl):S221–S236. [PubMed] [Google Scholar]
- 20.Kodama S, Saito K, Tanaka S, Maki M, Yachi Y, Asumi M, Sugawara A, Totsuka K, Shimano H, Ohashi Y, Yamada N, Sone H. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. 2009 May 20;301(19):2024–2035. doi: 10.1001/jama.2009.681. [DOI] [PubMed] [Google Scholar]
- 21.Lee DC, Sui X, Artero EG, Lee IM, Church TS, McAuley PA, Stanford FC, Kohl HW, 3rd, Blair SN. Long-term effects of changes in cardiorespiratory fitness and body mass index on all-cause and cardiovascular disease mortality in men: the Aerobics Center Longitudinal Study. Circulation. 2011 Dec 6;124(23):2483–2490. doi: 10.1161/CIRCULATIONAHA.111.038422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lucia A, Hoyos J, Perez M, Santalla A, Chicharro JL. Inverse relationship between VO2max and economy/efficiency in world-class cyclists. Medicine and science in sports and exercise. 2002 Dec;34(12):2079–2084. doi: 10.1249/01.MSS.0000039306.92778.DF. [DOI] [PubMed] [Google Scholar]
- 23.Lucia A, San Juan AF, Montilla M, CaNete S, Santalla A, Earnest C, Perez M. In professional road cyclists, low pedaling cadences are less efficient. Medicine and science in sports and exercise. 2004 Jun;36(6):1048–1054. doi: 10.1249/01.mss.0000128249.10305.8a. [DOI] [PubMed] [Google Scholar]
- 24.Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, Troiano RP. Amount of time spent in sedentary behaviors in the United States, 2003–2004. American journal of epidemiology. 2008 Apr 1;167(7):875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Meyer T, Lucia A, Earnest CP, Kindermann W. A conceptual framework for performance diagnosis and training prescription from submaximal gas exchange parameters--theory and application. Int J Sports Med. 2005;26(Suppl 1):S38–S48. doi: 10.1055/s-2004-830514. [DOI] [PubMed] [Google Scholar]
- 26.Moseley L, Jeukendrup AE. The reliability of cycling efficiency. Medicine and science in sports and exercise. 2001 Apr;33(4):621–627. doi: 10.1097/00005768-200104000-00017. [DOI] [PubMed] [Google Scholar]
- 27.Najarian RM, Sullivan LM, Kannel WB, Wilson PW, D'Agostino RB, Wolf PA. Metabolic syndrome compared with type 2 diabetes mellitus as a risk factor for stroke: the Framingham Offspring Study. Archives of internal medicine. 2006 Jan 9;166(1):106–111. doi: 10.1001/archinte.166.1.106. [DOI] [PubMed] [Google Scholar]
- 28.Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organization technical report series. 2000;894:i–xii. 1–253. [PubMed] [Google Scholar]
- 29.Porter MM, Vandervoort AA, Lexell J. Aging of human muscle: structure, function and adaptability. Scandinavian journal of medicine & science in sports. 1995 Jun;5(3):129–142. doi: 10.1111/j.1600-0838.1995.tb00026.x. [DOI] [PubMed] [Google Scholar]
- 30.Sigal RJ, Kenny GP, Boule NG, Wells GA, Prud'homme D, Fortier M, Reid RD, Tulloch H, Coyle D, Phillips P, Jennings A, Jaffey J. Effects of aerobic training, resistance training, or both on glycemic control in type 2 diabetes: a randomized trial. Annals of internal medicine. 2007 Sep 18;147(6):357–369. doi: 10.7326/0003-4819-147-6-200709180-00005. [DOI] [PubMed] [Google Scholar]
- 31.Sparks LM, Johannsen NM, Church TS, Earnest CP, Moonen-Kornips E, Moro C, Hesselink MK, Smith SR, Schrauwen P. Nine months of combined training improves ex vivo skeletal muscle metabolism in individuals with type 2 diabetes. The Journal of clinical endocrinology and metabolism. 2013 Apr;98(4):1694–1702. doi: 10.1210/jc.2012-3874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sun XG, Hansen JE, Garatachea N, Storer TW, Wasserman K. Ventilatory efficiency during exercise in healthy subjects. American journal of respiratory and critical care medicine. 2002 Dec 1;166(11):1443–1448. doi: 10.1164/rccm.2202033. [DOI] [PubMed] [Google Scholar]


