Abstract
Purpose
This study evaluated the efficacy of alveolar ridge preservation methods with and without primary wound closure and the relationship between histometric and micro-computed tomographic (CT) data.
Materials and Methods
Porcine hydroxyapatite with polytetrafluoroethylene membrane was implanted into a canine extraction socket. The density of the total mineralized tissue, remaining hydroxyapatite, and new bone was analyzed by histometry and micro-CT. The statistical association between these methods was evaluated.
Results
Histometry and micro-CT showed that the group which underwent alveolar preservation without primary wound closure had significantly higher new bone density than the group with primary wound closure (P<0.05). However, there was no significant association between the data from histometry and micro-CT analysis.
Conclusion
These results suggest that alveolar ridge preservation without primary wound closure enhanced new bone formation more effectively than that with primary wound closure. Further investigation is needed with respect to the comparison of histometry and micro-CT analysis.
Keywords: Bone Substitutes; Polytetrafluoroethylene; X-Ray, Microtomography
Introduction
A socket preservation procedure is a type of augmentation surgery to prevent progressive bone resorption with a bone substitute and a barrier membrane for dental implantation.1 When the barrier membrane is exposed, it can cause infection and decrease bone formation.2 A controversial report, however, showed that barrier membrane exposure did not yield a negative outcome.3 To identify the effect of wound closure on tooth extraction sockets for bone formation, a reliable quantitative measurement is necessary to provide useful information for dental implant installation.
Among various measuring methods, histomorphometric analysis has been highly regarded as the gold standard for its versatility. Researchers can obtain data not only from selected sections in two dimensions (2D), but also from entire samples stereologically in three dimensions (3D). Even though it provides detailed and effective results, there have been ongoing attempts to find alternative methods due to its destructive nature.
One of the latest alternatives is micro-computed tomography (micro-CT), which has recently been introduced to characterize 3D structures in bone tissue and applied to bone research.4 It provides precise measurements within a relatively short period of time without irreversible specimen preparation. In addition, several previous studies showed that micro-CT data were comparable and significantly correlated to histomorphometric data.5,6,7
Nevertheless, whether the selected 2D histologic sections are representative of 3D subjects has not been established. In this respect, we performed both types of analyses in order to examine the results of socket preservation. The primary objective of this study was to compare the change in hard tissue density after applying socket preservation methods with and without primary wound closure. The secondary objective was to evaluate the association between data from histometric and micro-CT analyses.
Materials and Methods
Animal surgery
Four adult male beagle dogs (average age: 2 years, average weight: 13 kg) received dental prophylaxis for sustaining healthy periodontal conditions. Animal experiments were carried out in accordance with the Guidelines of the National Institute of Health (NIH) regarding the care and use of animals for experimental procedures and with the protocols approved by the Institutional Animal Care and Use Committee of Seoul National University. All the surgical procedures were performed under general and local anesthesia induced by intravenous injections of atropine (0.04 mg/kg), intramuscular injection of 2% xylazine hydrochloride (Bayer Korea Ltd., Seoul, Korea), and ketamine hydrochloride (Yuhan, Seoul, Korea). Routine dental infiltration anesthesia with 2% lidocaine hydrochloride/epinephrine 1 : 100,000 (Kwangmyung Pharmaceutical, Seoul, Korea) was used at the surgical site. Mandibular second and fourth premolars were extracted, and the designed treatment was performed with an elevated mucoperiosteal flap.
The experimental design was a balanced block design. Three methods were randomly applied in each extraction socket according to the Latin block experimental design: group A: no treatment; group B: porcine hydroxyapatite graft (Purgo, Seongnam, Korea)+polytetrafluoroethylene (PTFE) membrane (Purgo, Seongnam, Korea) with primary wound closure; and group C: porcine hydroxyapatite graft +PTFE membrane with secondary wound closure. For postsurgical care, 20 mg/kg of cefazolin sodium (Yuhan, Seoul, Korea) was administered with soft diet feeding. Plaque control was performed on a daily basis with topical application of a chlorhexidine gluconate 0.12% solution. After 8 weeks, the animals were euthanized for mandibular block sections.
Micro-CT
Specimens were fixed in 10% buffered formalin for 10 days and scanned with a micro-CT SkyScan machine (Bruker-microCT, Kontich, Belgium). The system consisted of a sealed X-ray tube, 20-100 kV/100 µA, a 2-µm spot size, a precision object manipulator with two translations and one rotation direction, and a 12-bit digitally cooled CCD camera (1024×1024 pixels) with fiber optics. Transmission of X-ray images was carried out with 200 rotation views through 180° rotation (rotation step=0.3), using a 0.5 mm aluminum filter. The tube voltage and current were set at 100 kV and 100 µA, respectively. The exposure time was 316 ms for optimal clearness. All constructed cross sections contained 1024 pixels, with a cross-sectional pixel size of 19.75 µm(Fig. 1). Within 100 consecutive scanned images, the selected region of interest (3mm×3 mm) was located in the central region of the alveolar sockets. The total mineralized tissue volume percentage, graft volume percentage, and new bone volume percentage were calculated using a CT analyzer (Bruker-microCT, Kontich, Belgium).
Fig. 1.
Micro-computed tomograph shows radiographic image for mineral tissue measurement (19.75-µm resolution, 100 kV, 100 µA).
Histologic specimen preparation
For making histologic specimens, the mandibular blocks were dehydrated in 70-100% ethanol, embedded in methacrylate (Technovit 7200 VCL; Kulzer, Wehrheim, Germany), and sectioned in the mesio-distal plane by using a diamond saw (Exakt, Apparatebau, Norderstedt, Germany). From all the block sections, the central four sections were reduced to a final thickness of 30 µm and stained by hematoxylin-eosin (Fig. 2). The specimens were histologically analyzed under an optical microscope (Leica DM 2500, Leica Microsystems, Wetzlar, Germany).
Fig. 2.
Microphotograph shows the histologic specimen for mineral tissue measurement (H&E stain, 12.5×).
Histometric analysis
Digital images were captured and a computer-based image analysis system (Image-Pro Plus; Media Cybernetic, Silver Spring, MD, USA) was used to quantify the findings. Each corresponding area of interest (dimensions: 3 mm×3 mm) was selected in the central region of the alveolar sockets, while the total mineralized area percentage, graft area percentage, and new bone area percentage were histometrically evaluated; a researcher carried out a blinded experiment for this histometric analysis.
Statistical analysis
Quantitative data of micro-CT and histometry were presented in the form of mean±standard deviation for a descriptive purpose. To control the random effects of an individual animal as well as to compare the amount of new bone formation among the three groups, mixed model analyses were performed. The relationship between micro-CT and histometry was also investigated. All analyses were conducted using the free statistical software R (version 3.0.1 R Core Team, 2013, Vienna, Austria).
Results
There was no sign of inflammation during the wound healing period and fully covered epithelium at the surgical site collectively made the samples eligible for evaluation.
Three-dimensional micro-CT analysis showed a significantly lower total mineralized volume percentage in control group A than in the other groups. There was no significant difference in the total mineral volume between group B (graft with primary wound closure) and group C (graft with secondary wound closure). With respect to the new bone volume percentage, group C showed a significantly higher value than groups A and B (Table 1).
Table 1.
Descriptive statistics of 3D micro-computed tomographic data of each group (mean±SD)
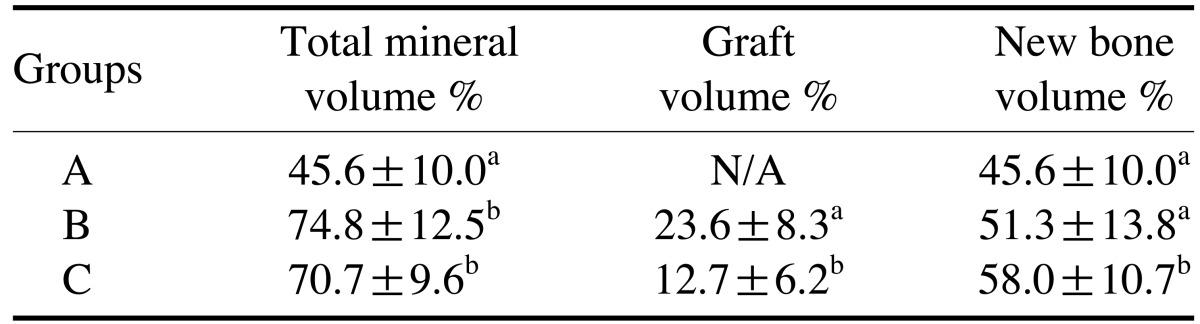
Different superscripts in each column indicate statistical differences and identical superscripts indicate no statistical difference in the designated group. A, control; B, porcine hydroxyapatite with primary wound closure; C, porcine hydroxyapatite with secondary wound closure
However, histometric evaluation revealed that the total mineral area percentage of group C was the largest among the groups. The new bone area in group B was the smallest and was significantly lower than the area in group C (Table 2).
Table 2.
Descriptive statistics of 2D histomorphometric data of each group (mean±SD)
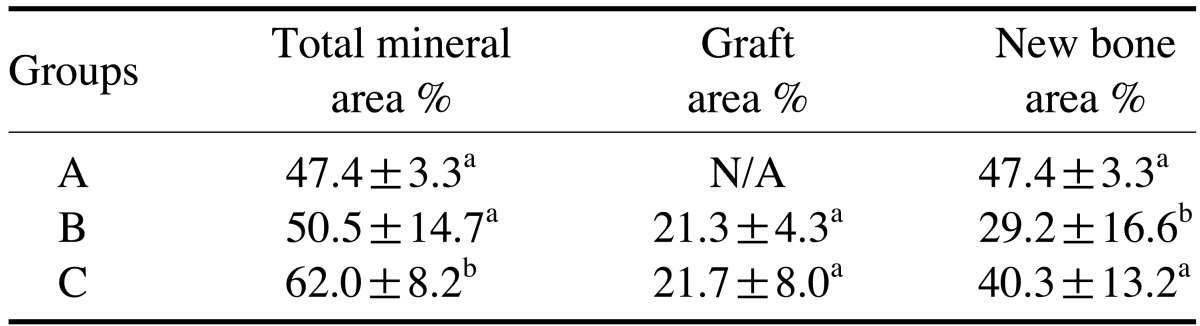
Different superscripts in each column indicate statistical differences and identical superscripts indicate no statistical difference in the designated group. A, control; B, porcine hydroxyapatite with primary wound closure; C, porcine hydroxyapatite with secondary wound closure
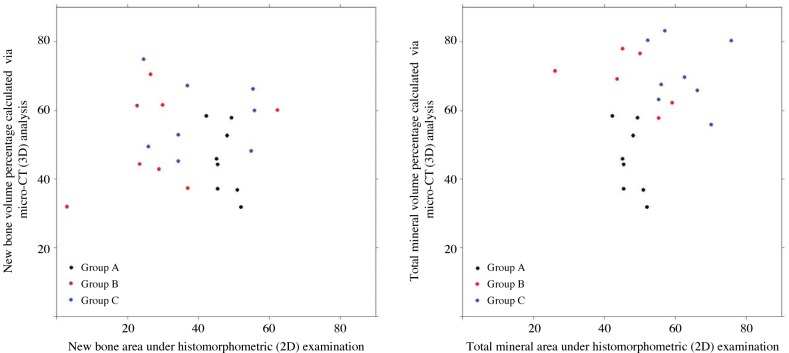
Figure 3 shows the relationship between the data from 2D histometry and 3D micro-CT. There was no significant association between the 2D and the 3D measurements in the amount of new bone formation (P=0.938) or total mineral content (P=0.200).
Fig. 3.
A graph shows the relationship between the two-dimensional histometry and three-dimensional micro-CT data. There is no significant association between the 2D and 3D measurements in the amount of new bone formation (left, P=0.938) or total mineral content (right, P=0.200). Group A, control; group B, porcine hydroxyapatite with primary wound closure; and group C, porcine hydroxyapatite with secondary wound closure.
Discussion
In this study, we performed two different alveolar ridge preservation procedures by using porcine hydroxyapatite with and without primary wound closure and quantitatively evaluated the hard tissue percentage through simple 2D histometry and 3D micro-CT. Micro-CT analysis for the percentage of total mineral volume, which included porcine hydroxyapatite and new bone, showed that the control group had a significantly lower value than the other two experimental groups using porcine hydroxyapatite with primary and secondary wound closure. The graft volume percentage of the two experimental groups was significantly different, which was contrary to the previous report presenting no significant difference in the remaining graft amount between the group with primary membrane closure and that with secondary membrane closure.8 A possible reason for this discrepancy could be the different type of graft materials, barrier membranes, and evaluation methods.
Stereological histometric analysis has been regarded as the gold standard technique for quantitative evaluation of particular cells and tissues, generating highly accurate measurement data of bone tissue.9 Although this method provides valuable information, it not only requires a considerable amount of time and cost for analysis,10 but also has limitations for practical usage in bone research due to irreversible sample preparation.11 Therefore, several researchers have adopted simple 2D histometry in biomaterial-treated bone defects to evaluate a particular tissue amount.8,12,13
On the other hand, micro-CT provides multiple-angled attenuated radiographic projection data to acquire 3D information and ensures specimen preservation with a relatively short period of time for analysis as opposed to histometry. However, micro-CT is not suitable to sufficiently assess cells of bone tissue such as osteoid, osteoblasts, and osteoclasts. Despite these differences, previous studies revealed that micro-CT was still comparable to stereologic histomorphometry for determining bone tissue quantity.14,15,16
Instead of using stereologic histomorphometry, simple 2D histometry has been frequently adopted in biomaterial studies.8,12,13 Although the authors of these reports mentioned that they carefully selected histologic specimens, these 2D data often generate excessively high variation and uncertainty that hinder accurate estimation of the samples' real properties. Therefore, the validity of simple 2D histometry has not yet been reported.
According to our results from the histometric and micro-CT analyses, more new bone formation was observed in the preserved socket with secondary wound closure than in that with primary wound closure. However, histometric analysis generally showed different results from those of micro-CT, in contrast to our expectation. The total mineral area percentage was statistically different between the control and group C (porcine hydroxyapatite with secondary wound closure). There was no statistical difference in the graft area percentage between group B (porcine hydroxyapatite with primary wound closure) and group C (porcine hydroxyapatite with secondary wound closure), while in the case of graft volume percentage, micro-CT data showed a significant difference between both groups. New bone formation area percentage of the control group was prominent as compared to that of group B (porcine hydroxyapatite with primary wound closure). This finding might be in parallel with the previous report which stated that placement of the biomaterial in the fresh extraction socket retards healing.13
Many researchers have claimed that bovine hydroxyapatite is not resorbable, but rather remains as it is when applied.17,18 This might be due to the differences in materials and lead to inconsistent bone regeneration.19 Packing density could be a critical factor for degradation, as it was suggested that appropriate resorption took a longer time when bovine hydroxyapatite was packed tightly.20 Porcine hydroxyapatite, which was not densely packed in our study, presented a lower volume percentage than the results from the aforementioned study. The chances of the degradation of porcine hydroxyapatite and/or the spill-out of the graft material might increase in the case of secondary wound closure, which needs further investigation.
Controversy still exists over the biological effects of resorbable barrier membrane exposure. Several researchers have demonstrated that exposed resorbable barrier membranes increase inflammation and decrease bone regeneration.21,22,23 When resorbable membranes are not secured, membrane movement and resorption result in a disruption of the clot surface, adversely affecting bone regeneration. However, other reports have stated that primary flap closure with a resorbable membrane is not necessary to achieve bone augmentation, if there is minimal inflammation and rapid epithelial migration over the exposed membrane.24 In this study, we utilized a non-resorbable barrier membrane, which is usually removed in case of infection, since there was no sign of inflammation during the wound healing process. Interestingly, our study revealed that group C (porcine hydroxyapatite with secondary wound closure) showed the highest new bone formation. In this respect, we suppose that porcine hydroxyapatite would be osteoconductive and the non-resorbable barrier membrane would effectively protect the extraction socket irrespective of wound closure.
Based on the scatter plots (Fig. 3), we could not find any significant association between the two analytical methods. Although the corresponding histologic section cut was selected on the basis of the micro-CT image, a simple 2D histometric analysis showed greater variation when compared to the micro-CT evaluation. Moreover, the destructive character of histologic specimen preparation prevented additional assessments. It has been reported that a high correlation exists between stereologic histometry and micro-CT.7 In this study, we used 5-µm-thick histologic specimens for 2D histometry and the corresponding micro-CT cuts with a 14-µm nominal resolution. However, our study showed no significant relationship between simple 2D histometry and micro-CT in all measurements: the total mineral density, graft density, and new bone density. This might be due to the histologic specimen thickness and nominal resolution of micro-CT of 30 µm and 19.75 µm, respectively, which were different from the values in previous research.
Although histologic specimens may provide valuable information for cell/tissue interactions, 2D histometry is not applicable to a real 3D situation and could cause a biased interpretation depending on the area selection. Therefore, studies that presented only simple 2D histometric data for the evaluation of bone biopsies are likely to require careful interpretation. Further confirmation is needed in terms of how the simple 2D histometry could generate a reliable quantification of mineralized tissue representing the whole specimens in future studies.
Within the limits of this study, there was a significantly larger amount of new bone formation after socket preservation with secondary wound closure than that after socket preservation with primary wound closure; this was supported by the results from both micro-CT and histometric analyses. However, the micro-CT analysis was not associated with the histometric evaluation in the hard tissue density calculation.
Acknowledgments
We are much indebted to Dr. Shin-Jae Lee for his comprehensive cooperation in the statistical evaluation of the data.
Footnotes
This study was supported by a grant of Seoul National University (860-20120007).
References
- 1.Cardaropoli D, Cardaropoli G. Preservation of the postextraction alveolar ridge: a clinical and histologic study. Int J Periodontics Restorative Dent. 2008;28:469–477. [PubMed] [Google Scholar]
- 2.Hämmerle CH, Jung RE. Bone augmentation by means of barrier membranes. Periodontol 2000. 2003;33:36–53. doi: 10.1046/j.0906-6713.2003.03304.x. [DOI] [PubMed] [Google Scholar]
- 3.Kim DM, Nevins M, Camelo M, Schupbach P, Kim SW, Camelo JM, et al. The feasibility of demineralized bone matrix and cancellous bone chips in conjunction with an extracellular matrix membrane for alveolar ridge preservation: a case series. Int J Periodontics Restorative Dent. 2011;31:39–47. [PubMed] [Google Scholar]
- 4.Kim JE, Shin JM, Oh SO, Yi WJ, Heo MS, Lee SS, et al. The three-dimensional microstructure of trabecular bone: analysis of site-specific variation in the human jaw bone. Imaging Sci Dent. 2013;43:227–233. doi: 10.5624/isd.2013.43.4.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chappard D, Retailleau-Gaborit N, Legrand E, Basle MF, Audran M. Comparison insight bone measurements by histomorphometry and microCT. J Bone Miner Res. 2005;20:1177–1184. doi: 10.1359/JBMR.050205. [DOI] [PubMed] [Google Scholar]
- 6.Fajardo RJ, Ryan TM, Kappelman J. Assessing the accuracy of high-resolution X-ray computed tomography of primate trabecular bone by comparisons with histological sections. Am J Phys Anthropol. 2002;118:1–10. doi: 10.1002/ajpa.10086. [DOI] [PubMed] [Google Scholar]
- 7.Müller R, Van Campenhout H, Van Damme B, Van Der Perre G, Dequeker J, Hildebrand T, et al. Morphometric analysis of human bone biopsies: a quantitative structural comparison of histological sections and micro-computed tomography. Bone. 1998;23:59–66. doi: 10.1016/s8756-3282(98)00068-4. [DOI] [PubMed] [Google Scholar]
- 8.Kim DM, De Angelis N, Camelo M, Nevins ML, Schupbach P, Nevins M. Ridge preservation with and without primary wound closure: a case series. Int J Periodontics Restorative Dent. 2013;33:71–78. doi: 10.11607/prd.1463. [DOI] [PubMed] [Google Scholar]
- 9.Dalle Carbonare L, Valenti MT, Bertoldo F, Zanatta M, Zenari S, Realdi G, et al. Bone microarchitecture evaluated by histomorphometry. Micron. 2005;36:609–616. doi: 10.1016/j.micron.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 10.Gielkens PF, Schortinghuis J, de Jong JR, Huysmans MC, Leeuwen MB, Raghoebar GM, et al. A comparison of micro-CT, microradiography and histomorphometry in bone research. Arch Oral Biol. 2008;53:558–566. doi: 10.1016/j.archoralbio.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 11.González-Garcia R, Monje F. Is micro-computed tomography reliable to determine the microstructure of the maxillary alveolar bone? Clin Oral Implants Res. 2013;24:730–737. doi: 10.1111/j.1600-0501.2012.02478.x. [DOI] [PubMed] [Google Scholar]
- 12.Kim YS, Kim SH, Kim KH, Jhin MJ, Kim WK, Lee YK, et al. Rabbit maxillary sinus augmentation model with simultaneous implant placement: differential responses to the graft materials. J Periodontal Implant Sci. 2012;42:204–211. doi: 10.5051/jpis.2012.42.6.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lindhe J, Cecchinato D, Donati M, Tomasi C, Liljenberg B. Ridge preservation with the use of deproteinized bovine bone mineral. Clin Oral Implants Res. doi: 10.1111/clr.12170. (in press) [DOI] [PubMed] [Google Scholar]
- 14.Uchiyama T, Tanizawa T, Muramatsu H, Endo N, Takahashi HE, Hara T. A morphometric comparison of trabecular structure of human ilium between microcomputed tomography and conventional histomorphometry. Calcif Tissue Int. 1997;61:493–498. doi: 10.1007/s002239900373. [DOI] [PubMed] [Google Scholar]
- 15.Müller R, Hahn M, Vogel M, Delling G, Ruegsegger P. Morphometric analysis of noninvasively assessed bone biopsies: comparison of high-resolution computed tomography and histologic sections. Bone. 1996;18:215–220. doi: 10.1016/8756-3282(95)00489-0. [DOI] [PubMed] [Google Scholar]
- 16.Engelke K, Graeff W, Meiss L, Hahn M, Delling G. High spatial resolution imaging of bone mineral using computed microtomography. Comparison with microradiography and undecalcified histologic sections. Invest Radiol. 1993;28:341–349. doi: 10.1097/00004424-199304000-00016. [DOI] [PubMed] [Google Scholar]
- 17.Artzi Z, Tal H, Dayan D. Porous bovine bone mineral in healing of human extraction sockets. Part 1: histomorphometric evaluations at 9 months. J Periodontol. 2000;71:1015–1023. doi: 10.1902/jop.2000.71.6.1015. [DOI] [PubMed] [Google Scholar]
- 18.Skoglund A, Hising P, Young C. A clinical and histologic examination in humans of the osseous response to implanted natural bone mineral. Int J Oral Maxillofac Implants. 1997;12:194–199. [PubMed] [Google Scholar]
- 19.Vance GS, Greenwell H, Miller RL, Hill M, Johnston H, Scheetz JP. Comparison of an allograft in an experimental putty carrier and a bovine-derived xenograft used in ridge preservation: a clinical and histologic study in humans. Int J Oral Maxillofac Implants. 2004;19:491–497. [PubMed] [Google Scholar]
- 20.Fugazzotto PA. GBR using bovine bone matrix and resorbable and nonresorbable membranes. Part 1: histologic results. Int J Periodontics Restorative Dent. 2003;23:361–369. [PubMed] [Google Scholar]
- 21.Hürzeler MB, Quiñones CR, Schüpbach P. Guided bone regeneration around dental implants in the atrophic alveolar ridge using a bioresorbable barrier. An experimental study in the monkey. Clin Oral Implants Res. 1997;8:323–331. doi: 10.1034/j.1600-0501.1997.080411.x. [DOI] [PubMed] [Google Scholar]
- 22.von Arx T, Cochran DL, Schenk RK, Buser D. Evaluation of a prototype trilayer membrane (PTLM) for lateral ridge augmentation: an experimental study in the canine mandible. Int J Oral Maxillofac Surg. 2002;31:190–199. doi: 10.1054/ijom.2001.0205. [DOI] [PubMed] [Google Scholar]
- 23.Oh TJ, Meraw SJ, Lee EJ, Giannobile WV, Wang HL. Comparative analysis of collagen membranes for the treatment of implant dehiscence defects. Clin Oral Implants Res. 2003;14:80–90. doi: 10.1034/j.1600-0501.2003.140111.x. [DOI] [PubMed] [Google Scholar]
- 24.Zubillaga G, Von Hagen S, Simon BI, Deasy MJ. Changes in alveolar bone height and width following post-extraction ridge augmentation using a fixed bioabsorbable membrane and demineralized freeze-dried bone osteoinductive graft. J Periodontol. 2003;74:965–975. doi: 10.1902/jop.2003.74.7.965. [DOI] [PubMed] [Google Scholar]