ABSTRACT
BACKGROUND
Primary care providers (PCPs) vary in skills to effectively treat depression. Key features of evidence-based collaborative care models (CCMs) include the availability of depression care managers (DCMs) and mental health specialists (MHSs) in primary care. Little is known, however, about the relationships between PCP characteristics, CCM features, and PCP depression care.
OBJECTIVE
To assess relationships between various CCM features, PCP characteristics, and PCP depression management.
DESIGN
Cross-sectional analysis of a provider survey.
PARTICIPANTS
180 PCPs in eight VA sites nationwide.
MAIN MEASURES
Independent variables included scales measuring comfort and difficulty with depression care; collaboration with a MHS; self-reported depression caseload; availability of a collocated MHS, and co-management with a DCM or MHS. Covariates included provider type and gender. For outcomes, we assessed PCP self-reported performance of key depression management behaviors in primary care in the past 6 months.
KEY RESULTS
Response rate was 52 % overall, with 47 % attending physicians, 34 % residents, and 19 % nurse practitioners and physician assistants. Half (52 %) reported greater than eight veterans with depression in their panels and a MHS collocated in primary care (50 %). Seven of the eight clinics had a DCM. In multivariable analysis, significant predictors for PCP depression management included comfort, difficulty, co-management with MHSs and numbers of veterans with depression in their panels.
CONCLUSIONS
PCPs who felt greater ease and comfort in managing depression, co-managed with MHSs, and reported higher depression caseloads, were more likely to report performing depression management behaviors. Neither a collocated MHS, collaborating with a MHS, nor co-managing with a DCM independently predicted PCP depression management. Because the success of collaborative care for depression depends on the ability and willingness of PCPs to engage in managing depression themselves, along with other providers, more research is necessary to understand how to engage PCPs in depression management.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-014-2807-z) contains supplementary material, which is available to authorized users.
KEY WORDS: primary care, mental health, depression, care management
INTRODUCTION
Depression is prevalent in the primary care (PC) setting,1–3 but undertreated4–6. Primary care providers (PCPs) vary in their skills to effectively diagnose and treat depression,4,7–10 a deficit attributed in prior research to lack of comfort with depression management, competing demands and time constraints, and lack of training in depression management.8,11–14 Collaborative care models (CCMs) can facilitate PCP depression management;15–22 these models, however, depend upon active PCP engagement. This study, based on a survey of PCPs in eight geographically dispersed Veterans Affairs (VA) PC practices,23 assesses PCP attitudes and experiences as predictors of self-reported performance of depression management behaviors.
The CCM delivers mental health treatment for depression using a team approach, consistent with core elements of patient-centered medical homes (PCMH). In CCM, depression care managers (DCMs) work with PCPs to assess and follow depression symptoms using structured assessment tools. Supervised by a mental health specialist (MHS), the care managers follow a “stepped care approach” to counsel and support patients with uncomplicated depression within PC, while assisting with the referral of complex patients.24 In comparison to usual care, collaborative care improves depression and quality of life among many PC populations,25,26 reduces hospitalizations and emergency room visits,27 and reduces costs.28 Collaborative care can also prevent adverse depression consequences.29 Variations in collaborative care effectiveness as implemented by different PC practices and healthcare organizations, however, suggest barriers to effective widespread implementation.30–33 One such barrier may be lack of effective PCP engagement in collaborative care.
While PCPs often believe that DCMs enhance depression care12,31, clinicians may vary in levels of willingness or ability to work effectively within the CCM. For example, in one randomized trial, patients referred by the trial to collaborative care who were patients of early CCM adopter clinicians had greater adherence to CCM protocols and achieved better depression outcomes than patients managed by clinicians who adopted CCM late, if at all.30 Early adopter clinicians were those who had voluntarily engaged in CCM prior to the start of the trial. While research has focused on CCM process and outcomes, little is known about PCP characteristics that may contribute to observed variations in collaborative care effectiveness.
As the framework for the analyses here, we adapted the Theory of Planned Behavior,34,35 a well-established theory that links attitudes, perceived control (self-efficacy), and past experience to performance of the behaviors. Based on this theory, we investigated PCP performance of key guideline-recommended depression management behaviors36,37 as a function of PCP attitudes, experience, and access to CCM features. We hypothesized that comfort and difficulty with depression management, experience with depression management, and the CCM features of co-management with a DCM and co-management with a MHS would predict PCP performance of depression management in PC.
METHODS
Overview
This cross-sectional study, approved by Institutional Review Boards for all eight participating sites, uses data from The VA Survey of Depression Care Practices in Primary Care.38,39 We conducted the study in the context of the Regional Expansion of Translating Initiatives for Depression into Effective Solutions (ReTIDES) study. ReTIDES used an encouragement design to test the Evidence-Based Quality Improvement (EBQI) method for spreading a VA-adapted collaborative care program for depression management.23,38,40 The spread process occurred between January 2005 and January 2006. The survey was available both online and in paper-and-pencil formats from October 2006 to July 2008.
Participating Sites
The survey component of ReTIDES was designed to inform CCM spread based on learning about PCP attitudes and behavior in the context of sites with variable levels of CCM implementation. Study sites included five target EBQI encouragement sites and three additional sites of similar size and complexity, all with prior evidence of interest in or implementation of depression collaborative care. Two of the additional sites had hired their own DCMs prior to ReTIDES, and one had volunteered previously for adopting collaborative care. The five experimental sites used a multi-level research/clinical partnership quality improvement approach, engaging site-level stakeholder representatives to develop and implement the VA-adapted collaborative care program.38
Sampling
We identified 397 PCPs from databases provided by each participating site. We sampled all 346 eligible PCPs identified. We administered the survey by e-mail and by paper-and-pencil upon request. We also attended site PC meetings to hand out additional survey copies and encourage participation. Resident physicians not enrolled in an internal medicine residency, providers who had moved away from the site, or without clinical duties, or invalid contact information, or on maternity leave were ineligible for the study. To incentivize voluntary survey participation, a smart phone was raffled off to a randomly selected respondent.
Site-Level Data Collection
We used data from the 2007 VA Clinical Practice Organization Survey Primary Care Directors Module39 to describe site characteristics related to depression care (i.e., depression-specific training, templates). Facility size was based on patient utilization data for FY 2007 from the VA National Patient Care Database41; practice location in urban/rural settings was from the Area Resource File42; and academic affiliation was from the VA Office of Academic Affiliation website.43 These site-level demographics were used for descriptive purposes only and were not included in the regression analyses.
Survey Development
We developed the survey based on literature review, previous provider surveys,44,45 and an expert panel process.46 Literature review identified the elements of coordination46–49 as critical for effective collaboration. The expert panel included regional and national leaders from the VA and Kaiser Permanente healthcare systems, and formed the basis for a subsequent meta-analysis.50 From these sources, we identified the dimensions of comfort, difficulty, and experience with depression care behaviors, as potential key provider-level factors for implementing depression collaborative care. The expert panel also identified access to shared records, joint responsibility for outcomes, leadership support, written agreements between PC and specialty to delineate responsibilities, and adoption of a “stepped care” model as site-level factors; these are not included in the study here.
Measures
Survey and scale items are delineated in Appendix Table 1 (available online). For the conceptual model’s dependent variable of PCP depression care behavior, we assessed PCP performance of depression management behaviors in PC using a six-item scale with a six-point Likert response scale for each item. PCPs indicated the proportion of their patients with suspected or diagnosed depression during the previous 6 months for whom they carried out the behaviors: PC-based assessment, management, DSM-IV diagnosis, patient education/self management support, treatment with antidepressants, or treatment modification in non-responding patients.
We assessed components of the Theory of Planned Behavior to predict PCP depression management. We assessed PCP attitudes toward depression care behaviors using a five-item scale for PCP comfort with depression care behaviors. We assessed the provider’s perceived control of depression care using a six-item scale for PCP difficulty with depression care. We assessed the provider’s experience with collaboration for depression care using experience co-managing with a DCM, experience co-managing with a MHS, availability of a collocated MHS, and a four-item scale for collaboration with MHS. We also assessed CCM features, including experience co-managing depression with a DCM and experience co-managing depression with a MHS; these were based on the proportion of patients with depression that the PCP reported co-managing with a DCM or MHS, rated on a five-point ordinal scale ranging from “none” to “most/almost all/all.” Availability of a collocated MHS was dichotomized as yes/no. We assessed experience with depression management using number of patients with depression in the panel and length of time worked at the VA. Number of patients with depression, or depression caseload, was rated on a four-point ordinal scale ranging from “0” to “> 8.” Length of time worked in professional capacity at the VA was assessed using a four-point ordinal scale ranging from “6 months or less” to “5 years or more.”
For covariates, we used self-reported gender (dichotomized as male/female), provider type, and number of clinics per week worked. Provider type was specified as resident physicians, attending physicians, or nurse practitioner (NP)/physician assistant (PA). Number of clinics per week worked was rated on a linear scale ranging from one to ten half-day sessions.
To develop survey scales, we included respondents who completed half or more of the scale items. We used Principal Components Analyses51 and exploratory factor analysis to refine our hypothesized scales for comfort, difficulty, and experience, and confirmatory factor analysis to confirm collaboration with MHS. Cronbach’s α, indicating scale reliability, was > 0.7 for each scale.52 Scale characteristics are further described in Appendix Table 2 (available online).
Model Development
We performed bivariate linear regression analyses with PCP performance of depression care management behaviors as the dependent variable, the predictors PCP comfort, difficulty, availability of a collocated MHS, collaboration with MHS, length of time worked at the VA, number of patients with depression in panel, and the covariates among the sample respondents (n = 180). Then we used variables that had bivariate associations of p < 0.2, along with the covariates (provider type, gender), to fit a mixed model regression analysis with sites treated as random effects. This model accounted for the intraclass coefficient (0.25) of providers within the VA sites. The variable length of time worked at the VA had multicollinearity with provider type (r = 0.7) and was omitted from the final model. We weighted the final model for provider type (i.e., attending physicians, resident physicians, NP/PAs) to account for non-response. For our final model, we included only cases with valid responses for all predictor variables. We found that data was missing completely at random, obviating the need for imputation of missing data.53
Additionally, we conducted parallel exploratory analyses to predict PCP experience co-managing patients with depression with DCMs. We performed bivariate analyses and then a mixed model regression analysis weighted for nonresponse, as above. All data analyses were conducted using STATA 11.0/IC.
RESULTS
Site Characteristics
Seven of the eight sites were located in urban settings, each serving 30,000–66,000 patients. One of the sites was rural, serving 6,558 patients. Six of the sites were academically affiliated. Two sites had developed computerized templates for depression screening and treatment. Seven had provided PC training in depression treatment or guidelines. None of the sites offered incentives (e.g., financial, protected time, perks) or performance profiling and feedback to promote adherence to clinical practice guidelines for depression treatment.
Response Rate
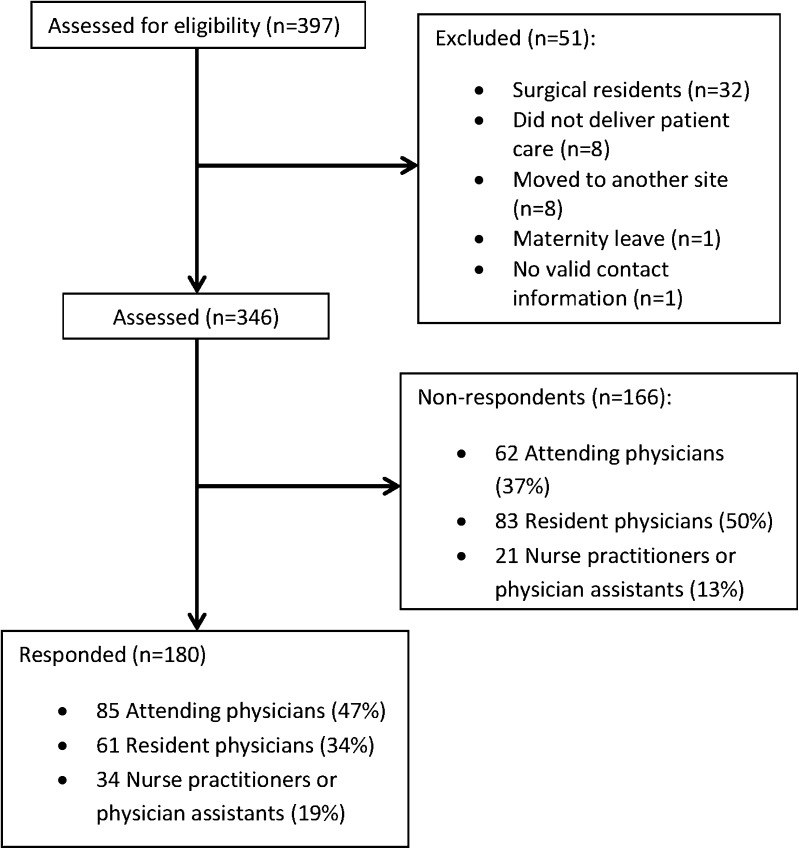
Figure 1 details eligibility and non-response rate. Of the 346 eligible PCPs, 180 responded (response rate =52 %); 85 were attending physicians (47 %), 61 residents (34 %), and 34 NPs/PAs (19 %); 30 % from the study’s three comparison sites. Responders were significantly different from non-responders by provider type, with fewer internal medicine residents and more attending physicians.
Figure 1.
The VA Survey of Depression Care Practices in Primary Care response rate flow diagram.
Of the 180 respondents, 119 (34 %) had sufficient data for the multivariable analysis due to missing items or scales. Because analyses showed that data were missing completely at random, we present provider characteristics on the 119 cases in the final model as representative of the full sample.
Sample Characteristics
The 180 respondents and the 119 with complete survey data are described in Table 1. Proportions of provider characteristics are similar for complete versus incomplete surveys, except for resident physicians. We report here on the 119 with no missing data; results for the 180 are similar. As planned, the majority of respondents had a MHS collocated in the PC clinic (61 %, 72/119), and most had co-managed depressed patients with a DCM (73 %, 87/119) and/or with a MHS (86 %, 102/119).
Table 1.
Primary Care (PC) Provider Respondent Characteristics from The VA Survey of Depression Care Practices in Primary Care
| Provider characteristic | Frequency, based on overall sample of respondents (N = 180) n (%)* |
Frequency, based on sample with complete responses (N = 119) n (%) |
|---|---|---|
| Gender, male | 96 (54 %) | 65 (55 %) |
| PC provider, by training status | ||
| Attending primary care physicians | 85 (47 %) | 68 (57 %) |
| Internal medicine residents† | 61 (34 %) | 26 (22 %) |
| Nurse practitioners, Physician assistants | 34 (19 %) | 25 (21 %) |
| Years practiced at the VA: | ||
| < 5 years | 90 (50 %) | 51 (44 %) |
| 5 or more years | 82 (46 %) | 66 (56 %) |
| Number of clinics per week: | ||
| 0–2 clinics | 80 (44 %) | 53 (47 %) |
| 3–7 clinics | 49 (27 %) | 29 (26 %) |
| 8 or more clinics | 37 (21 %) | 31 (27 %) |
| Number of patients on panel that are depressed: | ||
| None | 7 (4 %) | 5 (4 %) |
| 1–4 patients | 29 (16 %) | 22 (19 %) |
| 5–8 patients | 15 (8 %) | 11 (9 %) |
| > 8 patients | 93 (52 %) | 81 (68 %) |
| Reported having a collocated MHS in the PC clinic | 90 (50 %) | 72 (61 %) |
| Co-managed any depressed patients with a DCM | 112 (62 %) | 87 (73 %) |
| Co-managed any depressed patients with a MHS | 141 (78 %) | 102 (86 %) |
MHS Mental Health Specialist; PC Primary Care; DCM Depression Care Manager
* Percentages may not add up to 100 % due to missing data
† Proportion is significantly different between sample of N = 180 and N = 119 using two-sample proportion test
Description of PCP Attitudes and Behaviors
Among the 119 respondents, 64 (54 %) felt moderately or very comfortable with managing depression. In terms of perceived control over depression treatment, 89 (75 %) PCPs reported some or no difficulty diagnosing depression and 98 (82 %) reported some or no difficulty prescribing antidepressants. However, only 35 (29 %) referred to psychotherapy groups with some or no difficulty.
In terms of depression management behaviors, about one-third of PCPs (41/119, 34 %) reported proceeding with PC-based care rather than MHS-based care for most or all of their patients who screened positive for depression in the past 6 months. One-quarter (30/119, 25 %) reported assuming primary responsibility for managing most or all of their veterans with depression. Slightly more (46/119, 39 %) reported prescribing antidepressants themselves. Over half (65/119, 55 %) reported not referring to psychotherapy.
Predicting PCP Depression Management Behaviors (Table 2)
Table 2.
Predictors of Primary Care Provider (PCP) Performance of Depression Management in Primary Care: Results of Bivariate Linear Regression and Mixed Model Regression Analysis*
| Link to conceptual model | Independent variables | Results of bivariate linear regression (n = 180) | Results of mixed model regression analysis† (n = 119) | ||
|---|---|---|---|---|---|
| Regression coefficient (CI) | p value | Regression coefficient (CI) | p value | ||
| Attitude towards depression care behaviors | PCP comfort with depression management | 0.59 (0.45–0.73) | < 0.001 | 0.23 (0.12–0.33) | < 0.001 |
| Perceived control of depression care | PCP difficulty with depression management | 0.63 (0.52–0.73) | < 0.001 | 0.46 (0.39–0.52) | < 0.001 |
| Experience with collaboration for depression care | Experience with co-managing depression with MHS | 3.29 (0.74–5.83) | 0.01 | 2.12 (0.43–3.80) | 0.01 |
| Presence of collocated MHS | 9.47 (1.84–17.11) | 0.02 | −1.01(−10.22–8.20) | 0.83 | |
| Collaboration with a MHS | 0.11 (0.02–0.20) | 0.01 | −0.03 (−0.13–0.06) | 0.46 | |
| Experience with co-managing depression with DCM | 3.10 (0.35–5.86) | 0.03 | 1.22 (−0.57–3.02) | 0.18 | |
| Experience with depression management | Number of patients with depression in panel | 8.16 (4.30–12.02) | < 0.001 | 5.87 (2.64–9.09) | < 0.001 |
| Length of time at VA > 5 years | 12.5 (5.6–19.5) | < 0.001 | -- ‡ | -- ‡ | |
| Covariates | Gender, male | −5.45 (−12.59–1.70) | 0.13 | 2.55 (−1.56–6.66) | 0.22 |
| Training status: Resident | −11.0 (−19.0–3.0) | 0.008 | 4.92 (−2.19–12.03) | 0.18 | |
| Training status: NP/PA | 0.38 (−9.01–9.78) | 0.94 | 5.70 (−1.52–12.92) | 0.12 | |
| Number of clinics per week | 0.35 (−4.13–4.83) | 0.88 | -- ‡ | -- ‡ | |
* Data from The VA Survey of Depression Care Practices in Primary Care
† Model uses sites as random effect and weighted for non-response
‡ Variable was not included in the multivariable model
MHS Mental Health Specialist; PCP Primary Care Provider; DCM Depression Care Manager; NP Nurse Practitioner; PA Physician Assistant
In bivariate regression analyses, PCP attitudes towards depression care behaviors (comfort with depression management), perceived control (difficulty with depression management), experience with collaboration (presence of collocated MHS, co-managing depressed patients with MHS, co-managing depressed patients with DCM, collaboration with MHS), and experience with depression care (length of time at VA, number of patients with depression in panel), were significantly associated with PCP depression management behaviors in the expected directions. Among covariates, residents were significantly less likely to carry out depression behaviors than attending physicians; NP/PA behaviors were similar to those of attending physicians. Neither gender nor number of clinics per week significantly predicted behaviors.
In a multivariable analysis adjusted for provider gender and type and weighted for non-response, significant predictors for PCP depression management behaviors included PCP comfort (p = 0.003), difficulty (p < 0.001), co-management with MHS (p = 0.01), and number of patients with depression in panel (p = 0.001).
Predicting PCP Co-Management with DCMs (Table 3)
Table 3.
Predictors of Primary Care Provider (PCP) Co-Management with Depression Care Manager (DCM): Results of Bivariate Linear Regression and Multi-Level Multivariable Model*
| Link to conceptual model | Independent variables | Results of bivariate linear regression (n = 180) | Results of mixed model regression analysis† (n = 123) | ||
|---|---|---|---|---|---|
| Regression coefficient (CI) | p value | Regression coefficient (CI) | p value | ||
| Attitude towards depression care behaviors | Comfort with co-managing depression with DCM | 0.35 (0.14–0.57) | 0.001 | 0.34 (0.14–0.53) | 0.001 |
| PCP comfort with depression management | 0.003 (−0.007–0.013) | 0.58 | — ‡ | — ‡ | |
| Perceived control of depression care | PCP difficulty with depression management | 0.007 (−0.002–0.015) | 0.12 | 0.005 (−0.008–0.017) | 0.43 |
| Experience with collaboration for depression care | Presence of collocated MHS | 0.43 (−0.02–0.88) | 0.06 | −0.23 (−0.58–0.11) | 0.19 |
| Collaboration with a MHS | 0.004 (−0.001–0.009) | 0.13 | 0.001 (−0.004–0.006) | 0.61 | |
| Experience with depression management | Number of patients with depression in panel | 0.05 (−0.18–0.28) | 0.67 | — ‡ | — ‡ |
| Length of time at VA > 5 years | −0.05 (−0.47–0.37) | 0.81 | — ‡ | — ‡ | |
| Covariates | Gender, male | −0.16 (−0.59–0.26) | 0.48 | 0.13 (−0.43–0.69) | 0.65 |
| Training status: Resident | −0.07 (−0.56–0.43) | 0.80 | 0.79 (−0.30–1.89) | 0.16 | |
| Training status: NP/PA | 0.21 (−0.35–0.78) | 0.45 | −0.29 (−0.68–0.09) | 0.14 | |
| Number of clinics per week | 0.30 (0.05–0.55) | 0.02 | 0.51 (0.02–1.00) | 0.04 | |
* Data from The VA Survey of Depression Care Practices in Primary Care
† Model uses sites as random effect and weighted for non-response
‡ Variable was not included in the multivariable model
MHS Mental Health Specialist; PCP Primary Care Provider; DCM Depression Care Manager; NP Nurse Practitioner; PA Physician Assistant
In exploratory bivariate analyses, comfort with co-managing depression with DCM, presence of collocated MHS, and number of clinics worked per week were significantly associated with co-management with DCM. In a multivariable analysis adjusted for provider gender and type and weighted for non-response, comfort with co-managing depression with DCM (p = 0.001) and number of clinics worked per week (p = 0.04) were significant predictors of co-managing with DCMs.
DISCUSSION
Our quantitative findings confirm a largely qualitative body of research11–14 showing that PCP attitudes and behaviors can act as barriers or facilitators for successful collaborative care. Our study suggests that variations among PCP characteristics may partly be responsible for observed variations in achievement of collaborative care goals. PCPs who were more comfortable with depression management, had less difficulty with managing depression, had more experience co-managing patients with depression with MHS, and had more patients with depression on their panel were more likely to perform depression behaviors in the PC setting.
In agreement with previous qualitative work,11–14 this study highlights PCP discomfort with depression management as a key barrier. We found that only about half of PCPs were comfortable with carrying out necessary depression management activities, and even fewer reported actually performing the needed behaviors. Overall, only one in five PCPs reported assuming primary responsibility for managing most or all of their patients with depression at these eight study VA sites involved in depression care improvement.
While most PCPs treated depressed patients with antidepressants, we found that PCPs often did not refer patients with depression to psychotherapy. Psychotherapy is considered equally efficacious to antidepressants for uncomplicated depression,54,55 and most PC patients prefer psychotherapy over antidepressant medications.56–58 Further research may help us understand the barriers in PC-initiated referral for psychotherapy in the VA and in similar settings.
Access to a collocated MHS and collaboration with MHS for patients with depression did not independently predict PCP depression management behaviors. Although collocated MHSs generally improve PCP satisfaction and comfort, previous studies also have not found outcome impacts of MHS collocation alone.59,60
Co-management with a DCM also did not independently predict PCP depression management behaviors. However, the observed relationships between comfort with the DCM, having more half days in clinic (and thus presumably more exposure to the DCM), and co-management with DCM may signal the importance of developing strong relationships between PCPs and DCMs. Prior research indicates that availability of a DCM alone does not assure engagement with PCPs.61 Although clinicians value DCMs and believe that DCMs improve depression care, the success of the CCM depends upon a strong PCP relationship with, and confidence in, the DCM.61 Future research may be needed to identify modifications in the DCM role that promote more active and universal PCP engagement.
A strength of this study is the development and use of scales to conceptualize PCP comfort, difficulty, experience with depression management, collaboration with MHS, and performance of depression management behaviors. Studies investigating provider-level barriers to depression management have been largely qualitative. Although our scales could not be validated against pre-existing surveys, our systematic survey development approach was based on prior surveys, expert panel consensus, and theory. The observed high reliability of our scales increases the validity and reliability of our results.
The study has limitations. First, this study is observational, cannot address causation, and is not designed to compare the benefits of any particular CCM element or approach. Second, our response rate was moderate, although comparable to published provider surveys.62 While nonrespondents were more likely to be resident physicians, we weighted our final analyses to account for response differences based on provider type. Third, our sample size was further reduced for multivariable regression by item-level missing variables. However, analysis showed missing data completely at random with a few missing items per respondent, making imputation of missing items unlikely to change results and therefore inadvisable. Fourth, unmeasured structural, organizational, and patient-level barriers may have shaped results.63 Fifth, we had no measure in the survey for the subjective norms component of the Theory of Planned Behavior. We suspect norms may not be a major predictor, given providers’ lack of response to feedback on depression outcomes in multiple trials.64–67
The positive effects of collaborative care on patients with depression in PC are well documented. The model is also consistent with innovative team-based PC approaches, such as the PCMH. However, the success of CCMs depends on PCP engagement in managing depression appropriately, including development of supportive co-management partnerships with DCMs or MHSs. New studies of PC depression improvement should focus on the potential barriers to PCP performance of depression management behaviors in PC. These include lack of PCP comfort with depression management, organizational impediments to some needed behaviors including referral to psychotherapy, and difficulties in establishing active partnerships between some PCPs and their collocated DCMs or MHSs for co-managing care for shared patients.
Electronic supplementary material
(PDF 30 kb)
(PDF 21 kb)
Acknowledgements
Contributors include Michelle Seelig, MD, MSHS, Jeff Spina, MD in survey development, and Martin Lee, PhD, and Michael Mitchell, PhD, for statistical consultation. We would like to thank Jack Needleman, PhD, for reviewing earlier drafts of this manuscript.
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs, or the US government, or other affiliated institutions.
Funders
The ReTIDES project “Expanding and Testing VA Collaborative Care Models for Depression” was supported by VA HSR&D (Project #MNT 03-215, PIs Lisa Rubenstein, MD MSHS, and Edmund Chaney, PhD) and VA Mental Health Quality Enhancement Research Initiative. Funding support for preparation of this paper was provided by VA Office of Academic Affiliations, through the Health Services Research Fellowship Training Program (TMP 65-020). Dr. Yano’s time was funded by the VA HSR&D Service through a Senior Research Career Scientist Award (Project # RCS 05-195).
Conflicts of Interest
The authors declare that they do not have a conflict of interest.
REFERENCES
- 1.Kessler R, Chiu W, Demler O, Walters E. Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R) Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singleton N, Bumpstead R, O’Brien M, Lee A, Meltzer H. Office of National Statistics: Psychiatric Morbidity Among Adults Living in Private Households, 2000. London: Her Majesty’s Stationery Office; 2001. [DOI] [PubMed] [Google Scholar]
- 3.Yano E, Chaney E, Campbell D, et al. Yield of practice-based depression screenings in VA primary care settings. J Gen Intern Med. 2012;27(3):331–338. doi: 10.1007/s11606-011-1904-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Young AS, Klap R, Sherbourne CD, Wells KB. The quality of care for depressive and anxiety disorders in the United States. Arch Gen Psychiatry. 2001;58(1):55–61. doi: 10.1001/archpsyc.58.1.55. [DOI] [PubMed] [Google Scholar]
- 5.Wang P, Lane M, Olfson M, Pincus H, Wells K, Kessler R. Twelve-Month Use of Mental health services in the United States. Arch Gen Psychiatry. 2005;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 6.Katz SJ, Kessler RC, Lin E, Wells KB. Medication management of depression in the United States and Ontario. J Gen Intern Med. 1998;13(2):77–85. doi: 10.1046/j.1525-1497.1998.00022.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin EH, Von Korff M, Katon W, et al. The role of the primary care physician in patients’ adherence to antidepressant therapy. Med Care. 1995;33(1):67–74. doi: 10.1097/00005650-199501000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Henke R, McGuire T, Zaslavsky A, Ford D, Meredity L, Arbelaez J. Clinician- and organization-level factors in the adoption of evidence-based care for depression in primary care. Health Care Manag Rev. 2008;33(4):289–299. doi: 10.1097/01.HCM.0000318766.29277.49. [DOI] [PubMed] [Google Scholar]
- 9.Pincus HA, Pechura CM, Elinson L, Pettit AR. Depression in primary care: linking clinical and systems strategies. Gen Hosp Psychiatry. 2001;23(6):311–318. doi: 10.1016/S0163-8343(01)00165-7. [DOI] [PubMed] [Google Scholar]
- 10.Baik SY, Bowers BJ, Oakley LD, Susman JL. The recognition of depression: the primary care clinician’s perspective. Ann Fam Med. 2005;3(1):31–37. doi: 10.1370/afm.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fickel J, Parker L, Yano E, Kirchner J. Primary care-mental health collaboration: an example of assessing usual practice and potential barriers. J Interprofessional Care. 2007;21(2):207–216. doi: 10.1080/13561820601132827. [DOI] [PubMed] [Google Scholar]
- 12.Henke RM, Chou AF, Chanin JC, Zides AB, Scholle SH. Physician attitude toward depression care interventions: implications for implementation of quality improvement initiatives. Implement Sci. 2008;3:40. doi: 10.1186/1748-5908-3-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anthony JS, Baik SY, Bowers BJ, Tidjani B, Jacobson CJ, Susman J. Conditions that influence a primary care clinician’s decision to refer patients for depression care. Rehabil Nurs. 2010;35(3):113–122. doi: 10.1002/j.2048-7940.2010.tb00286.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Benzer JK, Beehler S, Miller C, et al. Grounded theory of barriers and facilitators to mandated implementation of mental health care in the primary care setting. Depress Res Treat. 2012;2012:597157. doi: 10.1155/2012/597157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thielke S, Vannoy S, Unutzer J. Integrating mental health and primary care. Prim Care Clin Off Pract. 2007;34:571–592. doi: 10.1016/j.pop.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 16.Watts B, Shiner B, Pomerantz A, Stender P, Weeks W. Outcomes of a quality improvement project integrating mental health into primary care. Qual Saf Health Care. 2007;16:378–381. doi: 10.1136/qshc.2007.022418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Collins C, Hewson DL, Munger R, Wade T. Evolving Models of Behavioral Health Integration in Primary Care. New York, NY: Milbank Memorial Fund; 2010. [Google Scholar]
- 18.Pomerantz A, Shiner B, Watts B, et al. The white river model of colocated collaborative care. Fam Syst Health. 2010;28(2):114–129. doi: 10.1037/a0020261. [DOI] [PubMed] [Google Scholar]
- 19.Butler M, Kane RL, McAlpine D, et al. Integration of Mental Health/Substance Abuse and Primary Care No. 173. Rockville, MD: Agency for Healthcare Research and Quality; 2008. [Google Scholar]
- 20.Katon W, Von Korff M, Lin E, et al. Collaborative management to achieve treatment guidelines: impact on depression in primmary care. JAMA. 1995;273:1026–1031. doi: 10.1001/jama.1995.03520370068039. [DOI] [PubMed] [Google Scholar]
- 21.Unutzer J, Katon W, Callahan C, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288(22):2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 22.Wagner E, Austin B, Davis C, Hindmarsh M, Schafer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Aff. 2001;20(6):64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- 23.Smith JL, Williams JW, Jr, Owen RR, Rubenstein LV, Chaney E. Developing a national dissemination plan for collaborative care for depression: QUERI Series. Implement Sci. 2008;3:59. doi: 10.1186/1748-5908-3-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Katon W, Von Korff M, Lin E, et al. Stepped collaborative care for primary care patients with persistent symptoms of depression: a randomized trial. Arch Gen Psychiatry. 1999;56(12):1109–1115. doi: 10.1001/archpsyc.56.12.1109. [DOI] [PubMed] [Google Scholar]
- 25.Gilbody S, Bower P, Fletcher J, Richards D, Sutton AJ. Collaborative care for depression. Arch Intern Med. 2006;166:2314–2321. doi: 10.1001/archinte.166.21.2314. [DOI] [PubMed] [Google Scholar]
- 26.Bower P, Gilbody S, Richards D, Fletcher J, Sutton A. Collaborative care for depression in primary care. Br J Psychiatry. 2006;189:484–493. doi: 10.1192/bjp.bp.106.023655. [DOI] [PubMed] [Google Scholar]
- 27.Unutzer J, Katon WJ, Fan MY, et al. Long-term cost effects of collaborative care for late-life depression. Am J Manag Care. 2008;14(2):95–100. [PMC free article] [PubMed] [Google Scholar]
- 28.Jacob V, Chattopadhyay SK, Sipe TA, Thota AB, Byard GJ, Chapman DP. Economics of collaborative care for management of depressive disorders: a community guide systematic review. Am J Prev Med. 2012;42(5):539–549. doi: 10.1016/j.amepre.2012.01.011. [DOI] [PubMed] [Google Scholar]
- 29.Yoon J, Rose DE, Canelo I, et al. Medical home features of VHA primary care clinics and avoidable hospitalizations. J Gen Intern Med. 2013;28(9):1188–1194. doi: 10.1007/s11606-013-2405-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chaney EF, Rubenstein LV, Liu CF, et al. Implementing collaborative care for depression treatment in primary care: a cluster randomized evaluation of a quality improvement practice redesign. Implement Sci. 2011;6:121. doi: 10.1186/1748-5908-6-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nutting P, Gallagher K, Riley K, et al. Care management for depression in primary care practice: findings from the RESPECT-depression trial. Ann Fam Med. 2008;6:30–37. doi: 10.1370/afm.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nutting PA, Gallagher KM, Riley K, White S, Dietrich AJ, Dickinson WP. Implementing a depression improvement intervention in five health care organizations: experience from the RESPECT-Depression trial. Adm Policy Ment Health. 2007;34(2):127–137. doi: 10.1007/s10488-006-0090-y. [DOI] [PubMed] [Google Scholar]
- 33.Solberg LI, Fischer LR, Wei F, et al. A CQI intervention to change the care of depression: a controlled study. Eff Clin Pract. 2001;4(6):239–249. [PubMed] [Google Scholar]
- 34.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211. doi: 10.1016/0749-5978(91)90020-T. [DOI] [Google Scholar]
- 35.Rimer BK, Glanz K. Theory at a Glance: A Guide for Health Promotion Practice (2nd ed). National Cancer Institute. US Dept of Health and Human Services. National Institutes of Health; 2005.
- 36.Depression Guideline Panel. Depression in Primary Care: detection and Diagnosis (Volume 1: Detection and Diagnosis). Rockville, (MD): Agency for Health Care Policy and Research (AHCPR); 1993.
- 37.Depression Guideline Panel. Depression in Primary Care (Volume 2: Treatment of Major Depression). Rockville, (MD): Agency for Health Care Policy and Research (AHCPR); 1993.
- 38.Rubenstein L, Chaney E, Ober S, et al. Using evidence-based quality improvement methods for translating depression collaborative care research into practice. Fam Syst Health. 2010;28:91–113. doi: 10.1037/a0020302. [DOI] [PubMed] [Google Scholar]
- 39.Yano E, Fleming B, Canelo, et al. National Survey Results for the Primary Care Director Module of the VHA Clinical Practice Organizational Survey. Sepulveda, CA: VA HSR&D Center for the Study of Healthcare Provider Behavior; 2008. [Google Scholar]
- 40.Collaborative care for depression in the primary care setting: a primer on VA’s Translating Initiatives for Depression into Effective Solutions (TIDES) Project. In: VA Health Services Research and Development Service, Office of Research and Development, Dept of Veterans Affairs, ed. Washington, DC 2008.
- 41.Veterans Health Administration. Corporate Data Warehouse.
- 42.Area Resource File (ARF). Rockville, MD: US Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions; 2008.
- 43.Department of Veterans Affairs. Office of Academic Affiliations. http://www.va.gov/oaa/. Accessed Jan 29, 2014.
- 44.Williams JW, Jr, Rost K, Dietrich AJ, Ciotti MC, Zyzanski SJ, Cornell J. Primary care physicians’ approach to depressive disorders. Effects of physician specialty and practice structure. Arch Fam Med. 1999;8(1):58–67. doi: 10.1001/archfami.8.1.58. [DOI] [PubMed] [Google Scholar]
- 45.Meredith LS, Jackson-Triche M, Duan N, Rubenstein LV, Camp P, Wells KB. Quality improvement for depression enhances long-term treatment knowledge for primary care clinicians. J Gen Intern Med. 2000;15(12):868–877. doi: 10.1046/j.1525-1497.2000.91149.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Seelig MD, Yano EM, Asch SM, Lin E, Gelberg L, Rubenstein LV. From marriage of convenience to partnership: what will it take for mental health and primary care providers to collaborate for depression care? Technical Monograph #06HFP0001. VA HSR&D Center of Excellence for the Study of Health Care Provider Behavior; 2006.
- 47.Gittell JH, Seidner R, Wimbush J. A relational model of how high-performance work systems work. Organ Sci. 2010;21(2):490–506.
- 48.Gittell JH, Fairfield KM, Bierbaum B, et al. Impact of relational coordination on quality of care, postoperative pain and functioning, and length of stay: a nine-hospital study of surgical patients. Med Care. 2000;38(8):807–819. doi: 10.1097/00005650-200008000-00005. [DOI] [PubMed] [Google Scholar]
- 49.McDonald K, Sundaram V, Bravata D, et al. Care Coordination. Technical Review 9 (Prepared by the Stanford University-UCSF Evidence-based Practice Center under contract 290020017) Rockville, MD: Agency for Healthcare Research and Quality; 2007. [Google Scholar]
- 50.Foy R, Hempel S, Rubenstein L, et al. Meta-analysis: the effect of interactive communication between collaborating primary care physicians and specialists. Ann Intern Med. 2010;152(4):247–258. doi: 10.7326/0003-4819-152-4-201002160-00010. [DOI] [PubMed] [Google Scholar]
- 51.Kline R. Principles and Practice of Structural Equation Modeling. New York: The Guilford Press; 2005. [Google Scholar]
- 52.Groves R, Fowler F, Jr, Couper M, Lepkowski J, Singer E, Tourangeau R. Survey Methodology. 2. Hoboken, NJ: John Wiley & Sons; 2009. [Google Scholar]
- 53.Little RJ, Rubin DB. Statistical Analysis with Missing Data. Hoboken, NJ: Wiley-Interscience; 2002. [Google Scholar]
- 54.Gelenberg AJ. A review of the current guidelines for depression treatment. J Clin Psychiatry. 2010;71(7):e15. doi: 10.4088/JCP.9078tx1c. [DOI] [PubMed] [Google Scholar]
- 55.Gelenberg AJ, Freeman M, Markowitz J, et al. Practice Guideline for the Treatment of Patients with Major Depressive Disorder. 3rd ed. American Psychiatric Association; 2010. http://psychiatryonline.org/pdfaccess.ashx?ResourceID=243261&PDFSource=6. Accessed Feb 20, 2014.
- 56.Dwight-Johnson M, Sherbourne CD, Liao D, Wells KB. Treatment preferences among depressed primary care patients. J Gen Intern Med. 2000;15(8):527–534. doi: 10.1046/j.1525-1497.2000.08035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Prins MA, Verhaak PF, Bensing JM, van der Meer K. Health beliefs and perceived need for mental health care of anxiety and depression–the patients’ perspective explored. Clin Psychol Rev. 2008;28(6):1038–1058. doi: 10.1016/j.cpr.2008.02.009. [DOI] [PubMed] [Google Scholar]
- 58.Gum AM, Arean PA, Hunkeler E, et al. Depression treatment preferences in older primary care patients. Gerontologist. 2006;46(1):14–22. doi: 10.1093/geront/46.1.14. [DOI] [PubMed] [Google Scholar]
- 59.Bower P, Knowles S, Coventry PA, Rowland N. Counselling for mental health and psychosocial problems in primary care. Cochrane Database Syst Rev. 2011; (9):CD001025. doi:10.1002/14651858.CD001025.pub3. [DOI] [PMC free article] [PubMed]
- 60.Harkness EF, Bower PJ. On-site mental health workers delivering psychological therapy and psychosocial interventions to patients in primary care: effects on the professional practice of primary care providers. Cochrane Database Syst Rev. 2009; (1):CD000532. doi:10.1002/14651858.CD000532.pub2. [DOI] [PMC free article] [PubMed]
- 61.Nutting PA, Gallagher K, Riley K, et al. Care management for depression in primary care practice: findings from the RESPECT-Depression trial. Ann Fam Med. 2008;6(1):30–37. doi: 10.1370/afm.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kellerman SE, Herold J. Physician response to surveys. A review of the literature. Am J Prev Med. 2001;20(1):61–67. doi: 10.1016/S0749-3797(00)00258-0. [DOI] [PubMed] [Google Scholar]
- 63.Chaudoir SR, Dugan AG, Barr CH. Measuring factors affecting implementation of health innovations: a systematic review of structural, organizational, provider, patient, and innovation level measures. Implement Sci. 2013;8(1):22. doi: 10.1186/1748-5908-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rollman BL, Hanusa BH, Gilbert T, Lowe HJ, Kapoor WN, Schulberg HC. The electronic medical record. A randomized trial of its impact on primary care physicians’ initial management of major depression [corrected] Arch Intern Med. 2001;161(2):189–197. doi: 10.1001/archinte.161.2.189. [DOI] [PubMed] [Google Scholar]
- 65.Fihn SD, McDonell MB, Diehr P, et al. Effects of sustained audit/feedback on self-reported health status of primary care patients. Am J Med. 2004;116(4):241–248. doi: 10.1016/j.amjmed.2003.10.026. [DOI] [PubMed] [Google Scholar]
- 66.Simon GE, VonKorff M, Rutter C, Wagner E. Randomised trial of monitoring, feedback, and management of care by telephone to improve treatment of depression in primary care. BMJ. 2000;320(7234):550–554. doi: 10.1136/bmj.320.7234.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Callahan CM, Hendrie HC, Dittus RS, Brater DC, Hui SL, Tierney WM. Improving treatment of late life depression in primary care: a randomized clinical trial. J Am Geriatr Soc. 1994;42(8):839–846. doi: 10.1111/j.1532-5415.1994.tb06555.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 30 kb)
(PDF 21 kb)