ABSTRACT
BACKGROUND
Medical care delivered in hospital-based medicine units requires interprofessional collaborative care (IPCC) to improve quality. However, models such as bedside interprofessional rounds, or encounters that include the team of physician and nurse providers discussing medical care at the patient’s bedside, are not well studied.
OBJECTIVE
To examine the incidence of and time spent in bedside interprofessional rounds on internal medicine teaching services in one academic medical center.
DESIGN AND PARTICIPANTS
Observational descriptive study of internal medicine faculty serving as inpatient medicine attending physicians. Participants completed a daily electronic survey following team rounding sessions to assess rounding characteristics (November 2012–June 2013); variables such as resident level-of-training, attending physician years’ of experience, house staff call day and clinic schedule were obtained from administrative data. Descriptive, Kruskal-Wallis, and multivariable logistic regression statistics were used to evaluate the study objectives.
MAIN MEASURES
Primary outcomes were: (1) incidence of bedside interprofessional rounds, (2) time spent with patients during bedside interprofessional rounding encounters, and, (3) factors associated with increased occurrence of and time spent with patients during bedside interprofessional rounds. Covariates included resident level-of-training, attending physician years’ of experience, census size, and call day.
KEY RESULTS
Of 549 rounding sessions, 412 surveys were collected (75 % response) from 25 attending physicians. Bedside interprofessional rounds occurred with 64 % of patients (median 8.0 min/encounter), differing by unit (intermediate care 81 %, general medicine 63 %, non-medicine 57 %, p < 0.001). Factors independently associated with increased occurrence of bedside interprofessional rounds were senior resident (OR 2.67, CI 1.75–4.06, PGY-3/PGY-4 vs. PGY-2), weekdays (OR 1.74, CI 1.13–2.69), team census size ≤ 11 (OR 2.36, CI 1.37–4.06), and attending physicians with ≤ 4 years’ experience (OR 2.15, CI 1.31–3.55). Factors independently associated with increased time spent during encounters were attending physicians with ≤ 4 years (OR 2.38, CI 1.44–3.95), 5–15 years of experience (OR 1.82, CI 1.10–3.02), and weekdays (OR 1.71, CI 1.10–2.65).
CONCLUSIONS
These findings highlight factors associated with increasing or decreasing occurrence and time spent in bedside interprofessional collaborative care delivery. Systematic changes to census size caps, resident scheduling, and attending physician education and staffing may be required to increase the occurrence of interprofessional collaborative care.
KEY WORDS: interprofessional care, hospital-based care, graduate medical education, bedside rounds
INTRODUCTION
Interprofessional collaborative care (IPCC) is the process during which different professionals work together to improve healthcare quality.1,2 Team-based care delivery with providers of different professions functioning as one unit enhances communication, coordination, and patient-centered shared-decision making, potentially improving process measures and patient-level outcomes.3–6 Despite recommendations to increase awareness and accelerate redesign of delivery models to be team-based and patient centered, the practical application of IPCC in medicine units has not been well studied.7
In hospital-based medicine units, a patient’s care involves mutual relationships, collaboration, and decision-making between physicians, nurses, and patients, highlighting the need for IPCC methods to improve quality.8 However, literature reveals two areas for concern in achieving these goals. First, patients are infrequently included in physician “rounds.” The majority of physician “rounds,” where healthcare providers deliver point-of-care evaluation, diagnosis, and shared-decision making with patients about their hospitalization, occur mostly in hallways and conference rooms, rather than at the bedside.9–11 Yet, patients experiencing bedside rounds report higher levels of satisfaction with their care, and physicians performing bedside rounds believe this activity improves education, team building, and patient care outcomes.10,12,13 The low incidence of bedside rounds is attributable to several factors, including time limitations, systems issues such as patient availability and scheduling conflicts, and attending-specific and learner-specific barriers.14–16 Second, nurse–physician collaboration during “rounds” occurs infrequently; one study reported that < 10 % of time spent coordinating a patient’s care involved nurses.17 Although prior work has focused on physician teams, to our knowledge no work has assessed bedside interprofessional rounds on academic teaching services.13,18,19 Amidst pressures to increase patient satisfaction and patient-care outcomes, local leaders must determine if current care delivery models are optimally designed to provide patient-centered IPCC, or if identifying modifiable systems factors and subsequent improvement are required.
In this study, we sought to advance our understanding of the current state of one model of IPCC, bedside interprofessional rounds (BIR), defined as encounters that include the team of providers—at least two physicians plus a nurse or other care provider—discussing the case at the bedside with the patient. We examine: (1) the incidence of BIR, (2) time spent with patients during BIR encounters in different clinical units, and (3) factors associated with increased occurrence of and time spent with patients during BIR. We hypothesized more experienced attending and resident physicians, smaller team census sizes, and medicine unit (rather than non-medicine unit) patients would be associated with higher incidence of BIR and time spent in BIR encounters.
METHOD
Study Setting
The study was conducted at a 378-bed university-based acute care hospital in central Pennsylvania. The 64 Internal Medicine beds are located in two units, a general medicine unit and an intermediate care unit. The general medicine unit has 44 beds, and is staffed by 60 nurses, with a nurse-to-patient ratio of 1:4. The intermediate care unit, providing care for patients requiring closer monitoring (e.g. continuous intravenous medications, respiratory therapy) has 20 beds, and is staffed by 41 nurses, with a nurse-to-patient ratio of 1:3. Additional medicine patients are admitted to non-medicine, or “overflow,” units throughout the hospital.
This academic medicine residency program consists of 69 Internal Medicine residents and 14 Internal Medicine-Pediatrics residents. Four teams provide care for all medicine service patients—three academic teaching teams and one non-teaching team; this study focuses on teaching teams only. Teaching teams consist of one junior (PGY2) or senior (PGY3-4) resident, two interns (PGY1), ≤ 2 medical students, and one attending physician. Team rounds typically begin between 8:30–9:00 am.
All house staff physicians receive one day off per week. At the time of data collection, categorical house staff typically had one weekly afternoon clinic session, while on-service attending physicians typically do not have clinic sessions. Attending physicians are all providers in the Division of General Internal Medicine (DGIM) and rotate every 2 weeks—one attending physician provides service for 12 straight days, followed by a weekend covered by a rotating pool of inpatient/outpatient DGIM physicians.
Data Collection
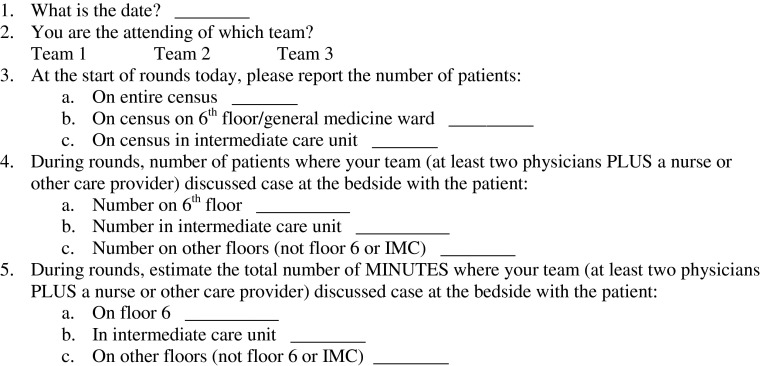
To address the current state of BIR, we created and administered an electronic survey to DGIM attending physicians during inpatient rotations. The survey was designed to identify the incidence, duration of, and factors associated with BIR. From November 2012 to June 2013, daily emails with the data-collection survey link were sent to the three teaching attending physicians at the end of rounds. Non-responders were sent a reminder email after 24–72 h. We described this near-time data collection method in prior work as an effective strategy to reduce recall bias associated with remote-time surveys.10,20 Concurrent but independent from this work, the medicine unit nurse managers performed an audit (observation and staff nursing self report) 5 days per month, recording the total unit census, number of patients receiving BIR, and the total proportion of patients receiving BIR. The study was approved by the Institutional Review Board.
The primary objectives were to determine the frequency of BIR and time spent during BIR encounters; for this study, we defined BIR as: “Encounters including the team of providers—at least two physicians plus a nurse or other care provider—discussing the case at the bedside with the patient.”13,16,21 The data sources were the survey of attending physicians and residency program administrative data. The survey (Appendix 1) was adapted from our prior studies pertaining to call shifts and bedside rounds.10,20 Other survey items included the date, number of patients on team census by unit, number of patients receiving BIR, and total minutes spent participating in BIR by unit. Prior to data collection, the survey was pilot tested and reviewed with five DGIM faculty members who serve as inpatient attending physicians. Several questions were reworded to more accurately describe the intended purpose and desired response. The survey was managed through www.surveymonkey.com.
The two main outcome variables were: (1) frequency of BIR, and, (2) time spent per patient during BIR encounters. Additional variables hypothesized to affect the conduct of rounds were identified through residency program records, including call vs. non-call day, intern or resident scheduled for clinic, resident’s level of training—PGY2 (“junior”) or PGY3-4 (“senior”), attending physician’s years in practice, and the attending physician on-service schedule. Additionally, we created the variable “new to service,” indicating the attending physician’s first day on service.
Data Analysis
Descriptive statistics were used to report characteristics of teams and rounding sessions. The non-parametric Kruskal-Wallis test was used to compare the frequency and minutes of BIR by unit (general medicine unit, intermediate care unit, “overflow” unit). The first main outcome (frequency of BIR) was calculated as the number of patients meeting BIR criteria divided by the number of patients on the census. The second main outcome (time spent per patient during BIR) was calculated as the minutes spent in BIR divided by the number of patients receiving BIR. Since there was no clinically accepted standard for the occurrence of BIR and to maintain balance between groups and assure adequate sample size, we dichotomized both continuous outcome variables at the median, identifying values above this threshold as “high” and values below as “low.” We treated rounding variables as categorical variables, dividing each into balanced groups to assure adequate sample size. Logistic regression analysis was used to identify unadjusted predictors of both main outcomes. Multivariable logistic regression was used to model variables collectively associated with high vs. low occurrence of and time spent with patients during BIR encounters. Variables were selected for inclusion if they were associated with the outcome variable in bivariate analysis (p < 0.10); a backwards process of selection was used to choose variables in the final model keeping only variables that were significant (p < 0.10). The data were analyzed using SAS 9.3 (Cary, NC) and Stata/IC-8 (College Park, Texas).
RESULTS
Rounding Sessions
During the study, a total of 549 surveys were sent, with 412 surveys completed (75 % response) by 25 different attending physicians. An estimated 95 % of surveys were completed within 72 h of the rounding session. See Table 1 for team characteristics during the study period.
Table 1.
Characteristics of Medicine Rounding Sessions (n = 412)
| Variable | n (%) |
|---|---|
| Resident year-of-training | |
| Junior resident (PGY-2) | 267 (65) |
| Senior resident (PGY-3 or PGY-4) | 145 (35) |
| Attending physician years in practice | |
| 1–4 years | 151 (37) |
| 5–15 years | 151 (37) |
| 16–27 years | 110 (27) |
| Day of the week | |
| Weekday | 295 (72) |
| Weekend | 117 (28) |
| Medicine team call daya | |
| No | 310 (75) |
| Yes | 102 (25) |
| Intern or resident in clinic | |
| No | 314 (76) |
| Yes | 98 (24) |
| Attending physician “new to service”b | |
| No | 354 (86) |
| Yes | 58 (14) |
aCall day = team accepts patients primarily from 2:00 pm to 7:00 pm. Non-call day = one of remaining 3 days when primary admissions are overnight “short” call admissions or morning admissions
b“New to service” = the first day on service for the attending physician, including weekdays and weekends
Occurrence of and Time Spent Per Patient During Bedside Interprofessional Rounds
Overall, the average proportion of patients receiving BIR per rounding session was 63.8 % (Table 2). Bedside interprofessional rounds were more likely to occur with patients in the intermediate care unit (81 %) compared with the general medicine ward (63.2 %) and “overflow” units (56.6 %, p < 0.001); differences between the general medicine unit and “overflow” units were not statistically different (p = 0.07). The nursing audit results demonstrated similar occurrences of BIR in the intermediate care unit (72.3 %) and on general medicine ward (62.7 %). Amongst patients receiving BIR, the median number of minutes spent per encounter was 8.0, differing by unit (intermediate care unit-10, general medicine ward-7.5, and “overflow” unit-8.6, p < 0.001); differences between the general medicine unit and “overflow” units were not statistically different (p = 1.0).
Table 2.
Proportion of Patients Receiving and Time Spent During Interprofessional Rounds by Location During Study Period (n = 412 Sessions)
| Variable–mean (s.d.) | Total | General medicine unit | Intermediate care unit | “Overflow” unitsa | p valueb |
|---|---|---|---|---|---|
| Average team census | 12.5 (1.68) | 6.37 (1.82) | 2.6 (1.46) | 3.5 (1.87) | < 0.001 |
| Patients receiving interprofessional rounds per session | 7.9 (3.04) | 3.97 (1.95) | 2.07 (1.34) | 1.88 (1.44) | < 0.001 |
| Percentage of patients receiving interprofessional rounds - % (s.d.) | 63.8 (24.2) | 63.19 (27.02) | 81.07 (30.93) | 56.61 (34.64) | < 0.001 |
| Variable–median (interquartile range) | |||||
| Minutes spent at bedside per session | 60.0 (60) | 30 (30) | 20 (20) | 15 (20) | < 0.001 |
| Minutes spent at bedside per patient amongst patients receiving bedside rounds | 8.0 (5.11) | 7.5 (5.0) | 10.0 (9.0) | 8.57 (5) | < 0.001 |
| Minutes spent at bedside per patient per total census | 5 (5.16) | 5 (4.17) | 10 (8.33) | 5 (5.50) | < 0.001 |
a“Overflow” units refer to non-medicine specific units throughout the hospital
bKruskal Wallis test using Bonferroni correction
Factors Associated with High Occurrence of and Time Spent Per Patient During Interprofessional Rounds
Factors associated with high occurrence and time spent per patient during BIR are shown in Tables 3 and 4, respectively. After adjusting for other significant variables in the model, factors independently associated with high occurrence of BIR were: senior resident (adjusted OR 2.57, CI 1.66–3.99, PGY-3/PGY-4 vs. PGY-2), attending physicians with ≤ 4 years in practice (adjusted OR 1.78, CI 1.05–3.03), team census ≤11 (OR 2.85, CI 1.60–5.07), and weekday (OR 1.92, CI 1.20–3.07); factors not associated with high occurrence of BIR included unit location, weekday, call day, attending physician “new to service,” and intern or resident in clinic. Factors independently associated with high time spent per patient during BIR were: attending physicians with ≤ 4 years or 5–15 years in practice (adjusted OR 2.51, CI 1.49–4.25, adjusted OR 1.91, CI 1.13–3.21, respectively), weekday (adjusted OR 2.04, CI 1.26–3.30), and no resident clinic (adjusted OR 2.22, CI 1.32–3.72); factors not associated with high time spent per patient during BIR included resident year-of-training, unit location, call day, and attending physician “new to service.”
Table 3.
Unadjusted and Adjusted Associations Between Rounding Variables and “High” Occurrence of Interprofessional Rounds (n = 412 Rounding Sessions)
| Variable - n (%) | “High” occurrence of interprofessional rounds (n = 206) | Unadjusted OR (95 % CI) | Adjusted OR (95 % CI)a |
|---|---|---|---|
| Team’s resident year-of-training | |||
| Junior resident | 111 | 1 | 1 |
| Senior resident | 95 | 2.67 (1.75–4.06) | 2.57 (1.66–3.99) |
| Attending - yrs since residency: | |||
| ≤4 | 89 | 2.15 (1.31–3.55) | 1.78 (1.05–3.03) |
| 5–15 | 73 | 1.40 (0.85–2.31) | 1.30 (0.77–2.19) |
| ≥16 | 44 | 1 | 1 |
| Team census: | |||
| ≤11 | 67 | 2.36 (1.37–4.06) | 2.85 (1.6–5.07) |
| 12–13 | 91 | 1.24 (0.78–1.98) | 1.29 (0.8–2.12) |
| ≥14 | 48 | 1 | 1 |
| General medicine unit census: | |||
| ≤5 | 70 | 1.59 (0.95–2.65) | |
| 6–7 | 88 | 1.31 (0.81–2.11) | |
| ≥8 | 48 | 1 | |
| Intermediate care unit census: | |||
| ≤2 | 98 | 1 | |
| ≥3 | 108 | 0.73 (0.5–1.08) | |
| “Overflow” unit censusb: | |||
| ≤2 | 64 | 1.34 (0.81–2.21) | |
| 3–4 | 92 | 1.79 (1.11–2.88) | |
| ≥5 | 50 | 1 | |
| Weekday | |||
| No | 47 | 1 | 1 |
| Yes | 159 | 1.74 (1.13–2.69) | 1.92 (1.20–3.07) |
| Call day | |||
| No | 152 | 1 | |
| Yes | 54 | 1.17 (0.75–1.83) | |
| Attending physician “new to service” | |||
| No | 177 | 1 | |
| Yes | 29 | 1.0 (0.57–1.74) | |
| Intern or resident in clinic | |||
| No | 152 | 0.76 (0.48–1.21) | |
| Yes | 54 | 1 | |
“High” occurrence = proportion of bedside interprofessional rounds exceeding the median (> 0.65, or 65 %)
aMultivariable model included control variables that were associated with “high” occurrence of interprofessional rounds in bivariate analysis (p < 0.1)
b“Overflow” units refer to non-medicine specific units throughout the hospital
Table 4.
Unadjusted and Adjusted Associations Between Rounding Variables and Increased Time Spent Per Patient During Interprofessional Rounds (n = 412 Rounding Sessions)
| Variable - n (%) | “High” time spent at bedside (n = 203) | Unadjusted OR (95 % CI) | Adjusted OR (95 % CI)a |
|---|---|---|---|
| Team’s resident year-of-training | |||
| Junior resident | 130 | 1 | |
| Senior resident | 73 | 1.07 (0.72–1.62) | |
| Attending physician years since residency graduation: | |||
| ≤4 | 87 | 2.38 (1.44–3.95) | 2.51 (1.49–4.25) |
| 5–15 | 76 | 1.82 (1.10–3.02) | 1.91 (1.13–3.21) |
| ≥16 | 40 | 1 | 1 |
| Team census: | |||
| ≤11 | 48 | 1.16 (0.68–1.98) | 1.07 (0.61–1.88) |
| 12–13 | 106 | 1.67 (1.05–2.67) | 1.64 (1.01–2.66) |
| ≥14 | 49 | 1 | 1 |
| General medicine unit census: | |||
| ≤5 | 63 | 0.88 (0.53–1.47) | |
| 6–7 | 81 | 0.77 (0.48–1.24) | |
| ≥8 | 59 | 1 | |
| Intermediate care unit census: | |||
| ≤2 | 110 | 1.30 (0.88–1.93) | |
| ≥3 | 93 | 1 | |
| “Overflow” unit censusb: | |||
| ≤2 | 66 | 1.05 (0.63–1.73) | |
| 3–4 | 78 | 0.91 (0.57–1.47) | |
| ≥5 | 59 | 1 | |
| Weekday | |||
| No | 46 | 1 | 1 |
| Yes | 157 | 1.71 (1.10–2.65) | 2.04 (1.26–3.30) |
| Call day | |||
| No | 146 | 1 | |
| Yes | 57 | 1.46 (0.93–2.30) | |
| Attending physician “new to service” | |||
| No | 175 | 1 | |
| Yes | 28 | 0.93 (0.53–1.62) | |
| Intern or resident in clinic | |||
| No | 162 | 1.53 (0.97–2.43) | 2.22 (1.32–3.72) |
| Yes | 41 | 1 | 1 |
“High” time spent at bedside = number of minutes greater than median value (> 8.0 min)
aMultivariable model included control variables that were associated with “high” minutes spent per patient during interprofessional rounds in bivariate analysis (p < 0.1)
b“Overflow” units refer to non-medicine specific units throughout the hospital
DISCUSSION
“Rounds” on inpatient units occur in a variety of formats, all with different agendas.22–24 Traditionally, “bedside rounds” have provided a venue for history-taking, physical examination, and diagnostic decision-making amongst teaching attending physicians and trainees.13 From this perspective, the presence and contribution of nurses has been highlighted as ideal for bedside rounds. Although some work has reported interprofessional rounds in intensive care units and Pediatrics, the explicit assessment of concurrent incorporation of bedside interprofessional rounds in medicine units is limited.25 With recent health policy and financial incentives to improve quality, O’Leary et al. described the implementation of “interdisciplinary rounds” involving physicians, nurses, and care coordinators to collaborate on patients’ care plans and improve safety.26 However, these rounds occurred in a conference room rather than the bedside, and the agenda was not primarily for care delivery. Although bedside interprofessional rounds may exist in medicine units in academic centers, their evaluation is not well reported.
In our medicine units during the study period, the percentage of patients receiving bedside interprofessional rounds (BIR) exceeded 60 %, with higher frequencies occurring in the intermediate care unit and lower frequencies in “overflow” units. Factors associated with increased occurrence of BIR were teams with senior residents, less experienced attending physicians, weekdays, and lower team census sizes; factors associated with increased time spent during BIR were less experienced attending physicians, weekdays, and no resident clinic. These findings highlight factors of current-day inpatient models limiting the occurrence of BIR. However, for patients receiving BIR, bedside time was only 8 min, raising questions about the quality of interactions during this limited time. These findings advance our understanding about factors impacting the occurrence of BIR on medicine units and highlight barriers hindering ideal patient-centered care for all admitted patients.
Regardless of unit location, nearly two-thirds of patients received BIR. Due to physician-related factors, systems issues (e.g. electronic medical record, increased patient volumes), and time limitations, physician bedside rounds occur with < 25 % of encounters, with < 10 % of time spent in nurse–physician communication.9,17 Even with our more strict definition of BIR requiring the physical presence of nurses, physicians, and patients, the two-thirds of patients receiving BIR well exceeds the previously reported data on occurrence of physician–patient rounds. With increased awareness of the need to improve quality and patient-centered communication, our hospital has encouraged all hospital-based units to implement and promote BIR during recent years. Several strategies have been initiated to support this goal, including unit-based nurse-physician gatherings, billboard themes, reminder emails, acknowledgment cards to providers for performing BIR, and the installment of touchpad buttons inside patient rooms that illuminate a pink light above the door to alert the nursing staff to the initiation of BIR encounters. We believe all of these efforts have increased levels of BIR on our units.
Patients in our units were more likely to receive BIR on weekdays with teams led by senior residents and less experienced attending physicians; variables not associated were day in call-cycle, intern/resident in clinic, or attending physician “new to the service.” No prior work has investigated factors associated with the frequency of BIR in hospital-based medicine units. Crumlish et al. reported post-call days as the most common days for bedside rounds, with less occurring on non-call days.27 Likewise, our past work demonstrated that “new” patients on post-call days were most likely to receive bedside rounds.21 However, in the context of changes in Accreditation Council for Graduate Medical Education rules, admitting schemes continue to evolve, including the transition from “bolus” to “drip” method (as in our program), to levy daily workload and improve compliance with duty-hour regulations.28,29 We believe the observed stability of BIR throughout the call cycle may reflect the attenuation of the “bolus” cycles of admissions and adjustments that offer protected time during rounds. We hypothesized and found that teams with senior rather than junior residents would be more likely to perform BIR. Senior residents have an additional year of clinical experience, specifically in clinical care issues and team management, which likely increases their proficiency with bedside activities. For similar reasons, we expected more experienced attending physicians to be more likely to perform BIR, a hypothesis not supported by our findings. Possible explanations may be recent graduates seek validation of house staff assessments leading to more bedside encounters, or junior faculty may be more sensitive to leadership-directed initiatives to prioritize BIR. Whatever the reason, this area merits further inquiry and may help direct faculty development efforts.
A higher frequency of BIR occurred with lower census sizes, suggesting team workload is a driver of BIR. This finding is consistent with our prior qualitative work that suggests bedside rounds are limited by several factors, including team census size, geographic dispersion of patients, and time limitations.14,16 These findings raise questions regarding the ideal census size for teaching teams in academic medical centers. Seeking to balance both quality of care and education, team functioning is variable and depends on numerous factors beyond census size, many of which are patient-related. For certain patients, BIR may not be relevant or required. However, given that patients have overwhelmingly reported their preference for bedside rounds and patient satisfaction is increasingly tied to reimbursement, these data may help to address the question of whether many or all patients on the team census could receive bedside rounds in our delivery system.10,12,30 In a prior study, when bedside teachers were asked about how they responded to barriers to conducting physician–patient rounds, they described utilizing a triage process resulting in an average of ∼70 % of patients receiving bedside rounds (similar to our findings).21 In similar settings, these data suggest an achievable frequency of patient-centered bedside rounds to be < 75 %, thereby excluding a significant proportion of patients from patient-centered IPCC. However, decreasing team census sizes to accommodate patient-centered care may compromise patient exposures and trainees’ educational opportunities, or may be financial untenable.31,32 The census size cap at which patient care, education, and financial feasibility are optimally balanced may well vary between hospital systems and requires further investigation.
For each patient receiving BIR, on average, he/she only received 8 min of the team’s presence on rounds. Ultimately, although our model has increased the likelihood of nurses and physicians interacting with patients, the quality of those interactions were not assessed and is of key importance.33,34 Although rounding sessions are not the only times whereby team members engage with patients, this is the prime period when inter-relational coordination between providers occurs.35 Given this relative paucity of patient-centered time, the ability to engage patients in a truly collaborative and authentic manner may be limited. However, in our institution, as well as others recently studied, rounding sessions are impacted by trainee and nursing schedules, care coordination meetings, and educational conferences, all of which limit the available time to perform BIR to less than 3 h.17 With our average team census size of 13, the necessity to complete certain care delivery tasks outside of patients’ rooms, and address care issues for the remaining patients who did not receive bedside rounds (3.5 in our study), increasing team bedside time may not be possible without addressing other modifiable systems or process factors, or, more dramatically, the care delivery models of inpatient medicine units. The unanswered question is whether 8 min per patient is sufficient time for adequate shared-decision making, authentic interprofessional collaborative care, and desired outcomes.1,8,36,37 In the context of the Affordable Care Act and the reimbursement models of team-based care and increased focus on patient-centered care, IPCC and patient-centered care models will become more valued and likely will drive significant change in care delivery.3,38 Without new models or reimbursement modifications, rounds in hospital-based units are inherently associated with the systems designs of present-day models.
There are several limitations to our study. First, although the survey was pilot tested for content, the construct validity of the instrument was not rigorously assessed. However, the similar results obtained by the concurrent nursing audit support the validity of our approach. Second, our institution has embraced a positive and supportive culture regarding BIR, and given these results are from one institution, this work may not be fully generalizable to other hospitals. Next, due to lack of data availability, we were unable to include residents’ days off, a key variable of interest, in our analysis. Lastly, surveys were not anonymous, raising the possibility of both social desirability bias and the Hawthorne effect, whereby participants may have modified their behavior because of their knowledge that they were being examined. Participants were reminded about the quality improvement assessment of the work, which should have decreased inaccuracies in reporting.
Optimal interprofessional collaborative care models are required to achieve desired patient satisfaction and patient-care outcomes. In this study, the frequency of bedside interprofessional rounds exceeded 60 %, with patients receiving an average of 8 min of team presence at the bedside when BIR occurred. Weekdays, smaller census size, senior residents, and less experienced attending physicians, were found to be independent predictors of increased occurrence of BIR. To our knowledge, these results are the first to demonstrate associations between system-related and participant-related factors and bedside interprofessional rounds. As hospitals and residency programs promote interprofessional collaborative care models, attention will need to be given to systems-based barriers to BIR in order to foster an environment that is both suitable and comfortable for interprofessional collaborative care to occur.
Acknowledgements
The authors would like to thank the medicine nursing staff and physicians for their dedication to patient centered care. We would also like to thank the Internal Medicine attending physicians for their willingness to participate in this study.
Conflicts of Interest
The authors declare that they do not have a conflict of interest.
Appendix 1: Survey of Inpatient Attending Physicians
Contributor Information
Jed D. Gonzalo, Phone: +1-717-5318161, FAX: +1-717-5317726, Email: jgonzalo@hmc.psu.edu.
Daniel R. Wolpaw, Email: dwolpaw@hmc.psu.edu.
Erik Lehman, Email: elehman@phs.psu.edu.
Cynthia H. Chuang, Email: cchuang@hmc.psu.edu.
REFERENCES
- 1.Zwarenstein M, Goldman J, Reeves S. Interprofessional collaboration: effects of practice-based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009;3 doi: 10.1002/14651858.CD000072.pub2. [DOI] [PubMed] [Google Scholar]
- 2.Davies C. Getting health professionals to work together. BMJ. 2000;320(7241):1021–1022. doi: 10.1136/bmj.320.7241.1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Butcher L. Teamswork! Hospitals & health networks/AHA. Mar 2012;86(3):24–27, 21. [PubMed]
- 4.Schmitt MH, Gilbert JH, Brandt BF, Weinstein RS. The coming of age for interprofessional education and practice. Am J Med. 2013;126(4):284–288. doi: 10.1016/j.amjmed.2012.10.015. [DOI] [PubMed] [Google Scholar]
- 5.Kohn LT, Corrigan J, Donaldson MS. To err is human: building a safer health system. Washington, D.C.: National Academy Press; 2000. [PubMed] [Google Scholar]
- 6.Curley C, McEachern JE, Speroff T. A firm trial of interdisciplinary rounds on the inpatient medical wards: an intervention designed using continuous quality improvement. Med Care. 1998;36(8 Suppl):AS4–AS12. doi: 10.1097/00005650-199808001-00002. [DOI] [PubMed] [Google Scholar]
- 7.Foundation. JMJ. Transforming Patient Care: Aligning Interprofessional Education and Clinical Practice Redesign.; January 17–20, 2013., 2013; Atlanta, GA.
- 8.Reeves S, Lewin S. Interprofessional collaboration in the hospital: strategies and meanings. J Health Serv Res Pol. 2004;9(4):218–225. doi: 10.1258/1355819042250140. [DOI] [PubMed] [Google Scholar]
- 9.Gonzalo JD, Masters PA, Simons RJ, Chuang CH. Attending rounds and bedside case presentations: medical student and medicine resident experiences and attitudes. Teach Learn Med. 2009;21(2):105–110. doi: 10.1080/10401330902791156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gonzalo JD, Chuang CH, Huang G, Smith C. The return of bedside rounds: an educational intervention. J Gen Intern Med. 2010;25(8):792–798. doi: 10.1007/s11606-010-1344-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gonzalo J. The return of bedside rounds. Journal of General Internal Medicine. Nov 9 2010. [DOI] [PMC free article] [PubMed]
- 12.Lehmann LS, Brancati FL, Chen MC, Roter D, Dobs AS. The effect of bedside case presentations on patients’ perceptions of their medical care. N Engl J Med. 1997;336(16):1150–1155. doi: 10.1056/NEJM199704173361606. [DOI] [PubMed] [Google Scholar]
- 13.Gonzalo JD, Heist BS, Duffy BL, et al. The value of bedside rounds: a multicenter qualitative study. Teach Learn Med. 2013;25(4):326–333. doi: 10.1080/10401334.2013.830514. [DOI] [PubMed] [Google Scholar]
- 14.Nair BR, Coughlan JL, Hensley MJ. Impediments to bed-side teaching. Med Educ. 1998;32(2):159–162. doi: 10.1046/j.1365-2923.1998.00185.x. [DOI] [PubMed] [Google Scholar]
- 15.Ramani S, Orlander JD, Strunin L, Barber TW. Whither bedside teaching? A focus-group study of clinical teachers. Acad Med. 2003;78(4):384–390. doi: 10.1097/00001888-200304000-00014. [DOI] [PubMed] [Google Scholar]
- 16.Gonzalo JD, Heist BS, Duffy BL, et al. Identifying and overcoming the barriers to bedside rounds: a multicenter qualitative study. Acad Med. 2014;89(2):326–334. doi: 10.1097/ACM.0000000000000100. [DOI] [PubMed] [Google Scholar]
- 17.Stickrath C, Noble M, Prochazka A, et al. Attending rounds in the current era: what is and is not happening. JAMA. 2013;173(12):1084–1089. doi: 10.1001/jamainternmed.2013.6041. [DOI] [PubMed] [Google Scholar]
- 18.Horwitz RI, Kassirer JP, Holmboe ES, et al. Internal medicine residency redesign: proposal of the Internal Medicine Working Group. Am J Med. 2011;124(9):806–812. doi: 10.1016/j.amjmed.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 19.Stickrath C, Aagaard E, Anderson M. MiPLAN: a learner-centered model for bedside teaching in today’s academic medical centers. Acad Med. 2013;88(3):322–327. doi: 10.1097/ACM.0b013e318280d8f7. [DOI] [PubMed] [Google Scholar]
- 20.Gonzalo J, Herzig S, Reynolds E, Yang J. Factors associated with non-compliance during 16-hour long call shifts. J Gen Intern Med. 2012;27(11):1424–1431. doi: 10.1007/s11606-012-2047-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gonzalo JD, Heist BS, Duffy BL, et al. The art of bedside rounds: a multi-center qualitative study of strategies used by experienced bedside teachers. J Gen Intern Med. 2013;28(3):412–420. doi: 10.1007/s11606-012-2259-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kroenke K. Attending rounds: guidelines for teaching on the wards. J Gen Intern Med. 1992;7(1):68–75. doi: 10.1007/BF02599106. [DOI] [PubMed] [Google Scholar]
- 23.LaCombe MA. On bedside teaching. Ann Intern Med. 1997;126(3):217–220. doi: 10.7326/0003-4819-126-3-199702010-00007. [DOI] [PubMed] [Google Scholar]
- 24.Janicik RW, Fletcher KE. Teaching at the bedside: a new model. Med Teach. 2003;25(2):127–130. doi: 10.1080/0142159031000092490. [DOI] [PubMed] [Google Scholar]
- 25.Landry MA, Lafrenaye S, Roy MC, Cyr C. A randomized, controlled trial of bedside versus conference-room case presentation in a pediatric intensive care unit. Pediatrics. 2007;120(2):275–280. doi: 10.1542/peds.2007-0107. [DOI] [PubMed] [Google Scholar]
- 26.O’Leary KJ, Buck R, Fligiel HM, et al. Structured interdisciplinary rounds in a medical teaching unit: improving patient safety. Arch Intern Med. 2011;171(7):678–684. doi: 10.1001/archinternmed.2011.128. [DOI] [PubMed] [Google Scholar]
- 27.Crumlish CM, Yialamas MA, McMahon GT. Quantification of bedside teaching by an academic hospitalist group. J Hosp Med. 2009;4(5):304–307. doi: 10.1002/jhm.540. [DOI] [PubMed] [Google Scholar]
- 28.Arora VM, Georgitis E, Siddique J, et al. Association of workload of on-call medical interns with on-call sleep duration, shift duration, and participation in educational activities. JAMA: J Am Med Assoc. 2008;300(10):1146–1153. doi: 10.1001/jama.300.10.1146. [DOI] [PubMed] [Google Scholar]
- 29.ACGME. ACGME Outcomes Project. 1999. http://www.acgme.org. Accessed February 7, 2014
- 30.Gonzalo J. Bedside rounding strategies used by bedside teachers. The authors’ reply. J Gen Intern Med. 2013;28(9):1131. doi: 10.1007/s11606-013-2462-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McCoy CP, Stenerson MB, Halvorsen AJ, Homme JH, McDonald FS. Association of volume of patient encounters with residents’ in-training examination performance. J Gen Intern Med. 2013;28(8):1035–1041. doi: 10.1007/s11606-013-2398-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McMahon GT, Katz JT, Thorndike ME, Levy BD, Loscalzo J. Evaluation of a redesign initiative in an internal-medicine residency. N Engl J Med. 2010;362(14):1304–1311. doi: 10.1056/NEJMsa0908136. [DOI] [PubMed] [Google Scholar]
- 33.O’Leary KJ, Thompson JA, Landler MP, et al. Patterns of nurse-physician communication and agreement on the plan of care. Qual Saf Health Care. 2010;19(3):195–199. doi: 10.1136/qshc.2008.030221. [DOI] [PubMed] [Google Scholar]
- 34.O’Leary KJ, Ritter CD, Wheeler H, Szekendi MK, Brinton TS, Williams MV. Teamwork on inpatient medical units: assessing attitudes and barriers. Qual Saf Health Care. 2010;19(2):117–121. doi: 10.1136/qshc.2008.028795. [DOI] [PubMed] [Google Scholar]
- 35.Havens DS, Vasey J, Gittell JH, Lin WT. Relational coordination among nurses and other providers: impact on the quality of patient care. J Nurs Manag. 2010;18(8):926–937. doi: 10.1111/j.1365-2834.2010.01138.x. [DOI] [PubMed] [Google Scholar]
- 36.Reeves S, Zwarenstein M, Goldman J, et al. Interprofessional education: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2008;1 doi: 10.1002/14651858.CD002213.pub2. [DOI] [PubMed] [Google Scholar]
- 37.Lefrancois D, Leung S. Bedside rounding strategies used by bedside teachers. J Gen Intern Med. 2013;28(9):1130. doi: 10.1007/s11606-013-2461-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Weinstein RS, Brandt BF, Gilbert JH, Schmitt MH. Bridging the quality chasm: interprofessional teams to the rescue? Am J Med. 2013;126(4):276–277. doi: 10.1016/j.amjmed.2012.10.014. [DOI] [PubMed] [Google Scholar]