ABSTRACT
Recent mass shootings in the U.S. have reignited the important public health debate concerning measures to decrease the epidemic of gun violence. Editorialists and gun lobbyists have criticized the recent focus on gun violence, arguing that gun-related homicide rates have been stable in the last decade. While true, data from the U.S. Centers for Disease Control and Prevention also demonstrate that although gun-related homicide rates were stable between 2002 and 2011, rates of violent gunshot injuries increased. These seemingly paradoxical trends may reflect the declining lethality of gunshot injuries brought about by surgical advances in the care of the patient with penetrating trauma. Focusing on gun-related homicide rates as a summary statistic of gun violence, rather than total violent gunshot injuries, can therefore misrepresent the rising epidemic of gun violence in the U.S.
Recent mass shootings in the United States have reignited the important public health debate concerning measures to decrease the epidemic of gun violence in this country.1 The United States is an outlier among industrialized nations. According to the United Nations Office on Drugs and Crime,2 the rate of gun-related homicides in the United States (3.3 gun-related homicides per 100,000 population in 2009) exceeds rates in each member nation of the Organisation for Economic Cooperation and Development (OECD—the group of 34 nations including Australia, Canada, Germany, Italy, Japan, Mexico, Switzerland, and the United Kingdom, against which economic and health indicators in the U.S. are frequently compared) by more than tenfold, with the sole exception of Mexico (7.9 gun-related homicides per 100,000 population in 2009). Moreover, with just 5 % of the world’s population, the United States houses 40 % of the world’s guns.3
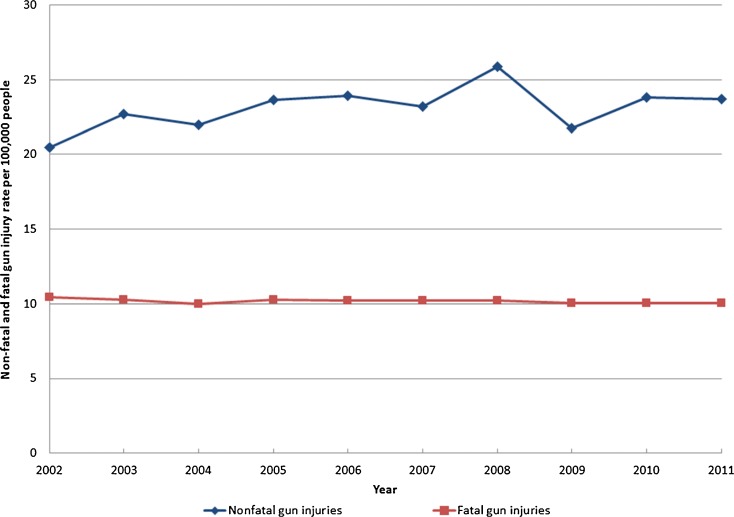
Yet despite clear evidence of high levels of gun violence in the United States, editorialists and gun lobbyists have criticized the recent focus on gun violence, arguing that gun-related homicide statistics demonstrate that gun violence is not rising. In evidence of this claim, they cite data on stable gun-related mortality rates more generally, and gun-related homicide rates in particular.4 And indeed, many of those statements regarding gun-related deaths are remarkably true. Data from the Centers for Disease Control and Prevention (CDC) Web-based Injury Statistics and Reporting System (WISQARS) confirm that gun-related deaths in the United States were stable during the 10-year period between 2002 and 2011, with approximately 10.3 per 100,000 Americans dying annually from a gun-related injury (Fig. 1). In 2002, an estimated 30,242 of 284 million Americans died from a gun-related injury (10.4 per 100,000) compared to an estimated 32,163 out of 311 million Americans in 2011 (10.3 per 100,000). Gun-related homicide rates have been similarly stable at approximately 4 per 100,000 (Fig. 1).
Figure 1.
Rates of non-fatal and fatal gun injuries in the United States, 2002–2011.
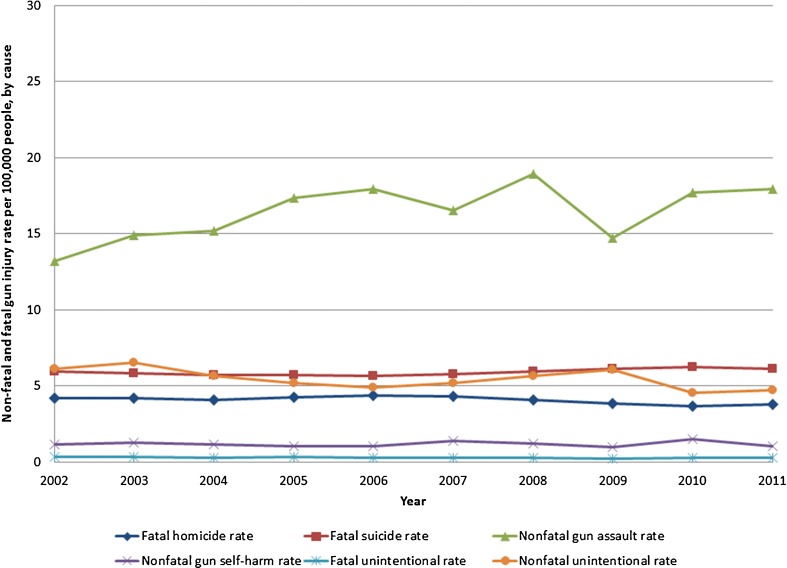
While critics of stronger gun control policies are correct to note that overall gun-related deaths and gun-related homicides have remained constant over the last 10 years, they fail to recognize a simple but important fact: non-fatal gunshot injuries, in particular non-fatal violent gun injuries, have been rising (Figs. 1 and 2). In 2002, for instance, there were 58,841 non-fatal gunshot injuries in the United States (20.5 per 100,000 Americans) compared to 73,883 in 2011 (23.7 per 100,000) (Fig. 1). Nearly all of the increase in non-fatal gunshot injuries in this 10-year period was attributable to increases in violent gun injuries (i.e., assaults), rather than unintentional gunshot injuries or injuries arising from attempted self-harm (Fig. 2). During this same period, death rates from gun-related homicide, suicide, and unintentional injury were stable (Fig. 2). These figures highlight the important point that focusing on gun-related deaths rather than total gunshot injuries (fatal plus non-fatal) can obscure our understanding of changing gun violence in this country, particularly since gun-related homicide rates have been stable, while non-fatal, violent gun injury rates have grown. Gun violence has therefore not been stable. It has been increasing.
Figure 2.
Rates of non-fatal and fatal gun injuries in the United States, by cause of injury, 2002–2011.
How is it possible that non-fatal gunshot injuries rose from 2002 to 2011 while fatal gunshot injuries remained stable? The answer is improvements in the management of life-threatening penetrating trauma arising from gunshot injury. Victims of gunshot injury today experience more rapid and advanced emergency medical care and trauma management than victims even a decade ago, making gun injuries less lethal today than ever before. In fact, many of the recent advances in the management of civilian gunshot injury have been learned from military experiences in the battlefields of Iraq and Afghanistan, where improvements in field hemostasis,5 endovascular repair of vascular injury, and neuro-critical care have occurred.6,7 For example, aggressive intracranial pressure monitoring and frequent neurosurgical intervention among victims of battlefield blast and penetrating injury has been demonstrated to improve mortality, a practice which has translated to civilian care.8 Similarly, early and even pre-emptive correction of coagulopathy (e.g., through use of recombinant factor VIIa) in battlefield victims has been demonstrated to result in fewer transfusions with no increase in thrombosis, providing valuable information for civilians suffering gunshot injury. 9,10 More generally, many of the improvements in the quality of civilian traumatic care have followed advances made in major military conflicts. World War I, for example, marked the beginning of motorized ambulance evacuation of the wounded, a practice later translated to the civilian world.11 The Korean War heralded the beginning of radio communication in the field and helicopter evacuation, and the war in Vietnam provided evidence for the use of field deployed medics, the basis for modern civilian paramedics.12
As a general principle, the annual rate of death from gunshot injury in a population is the multiple of total gunshot injuries (fatal plus non-fatal) times the lethality of gunshot injuries. For any given number of gunshot injuries in a population, the rate of death from gunshot injuries will depend on the lethality of those injuries. The lethality of gunshot injuries will, in turn, depend on the cause of gunshot injury (e.g. attempted suicide vs. violent assault), as well as the state of medical care to manage those injuries. For example, as self-inflicted gunshot wounds are associated with the highest mortality, rising rates of attempted suicide will increase the population-level mortality associated with guns. Similarly, improvements in medical care that lead to greater survival after gunshot injury will lower population-level mortality associated with gunshot injury.
This general principle implies that gun-related deaths in a population may be stable over time (as in Figs. 1 and 2) even while the total rate of gunshot injuries is rising. For example, Fig. 2 demonstrates that from 2002 to 2011, the non-fatal gun assault rate increased considerably (from nearly 13 to 18 per 100,000), while the gun-related homicide rate remained constant at approximately four gun homicides per 100,000. The declining lethality of violent gunshot injuries between 2002 and 2011 therefore offset increases in the overall rate of violent gun injuries.
Figures 1 and 2 also illustrate why regulatory policies to reduce the proliferation of semi-automatic weapons and more catastrophic ammunition are critical. Increasing use of semi-automatic weapons and more catastrophic ammunition increases the lethality of violent gun injuries—i.e., a given violent gunshot injury is more likely to be lethal when semi-automatic weapons are used—thereby increasing the mortality rate from guns for any given total level of violent gunshot injuries. Without curbing the growth of semi-automatic weapons, gun homicide rates may therefore rise even if other public policies are actually successful in reducing the total rate of violent gunshot injuries.
Although we have emphasized recent trends in fatal and non-fatal gunshot injuries, the links between total gunshot injuries, gun-related deaths, and advances in gunshot care are even more relevant when considering changes in gun-related deaths and non-fatal gunshot injuries over several decades. For instance, in an analysis that assumed that the distinction between homicide and aggravated assault is merely the outcome befalling the victim, Harris and colleagues13 studied trends in lethality of gunshot injury from 1964 to 1999, defining lethality as the ratio of gun homicides to the sum of gun-related homicides and aggravated assaults. From such a conceptual framework, these authors showed a sustained decline in the lethality of gunshot injury from 1964 to 1999, estimating that gun deaths would have been twice as high in 1999 (29,300 vs. 15,500) if medical management of gunshot injury had not improved since 1964. In order to show that the trend in decreasing gun lethality was largely due to medical advances, and not safer guns, the authors demonstrated similar declines in mortality for other weaponry, including knives and objects.
Advances in medical care that have led to a decline in the lethality of gunshot injuries have important implications for the medical and non-medical costs associated with gunshot injuries as well. Not surprisingly, medical costs associated with gunshot injuries have been estimated to be large and are growing. For example, in 1994, medical costs per gunshot injury in the United States were estimated at approximately $17,000, resulting in $2.3 billion in lifetime medical costs.14 Similar analyses using data from Pennsylvania estimated that inpatient hospital charges for gunshot injuries nearly doubled from $15,182 per injury in 1996–1998 to $30,814 during 2001–2003.15 While large, medical costs associated with gunshot injuries likely substantially underestimate the total costs of these injuries due to losses in job productivity, long-term disability, and psychological illness. For example, limited data suggests that inclusion of these non-medical costs raises the costs of gunshot injuries for those surviving to nearly $100 billion annually.16 While detailed data on more recent trends in the medical and non-medical costs of gunshot injuries are lacking (and needed), the declining lethality of gunshot injuries not only suggests that greater numbers of survivors may be alive to incur both the medical and non-medical costs of gunshot injuries, but that greater morbidity associated with survival from gunshot injuries may contribute to both rising medical and non-medical costs as well.
The difficult truth is that despite important advances in the management of gunshot injury even over the last decade, gun-related homicides in the United States have failed to decline, while at the same time, violent gunshot injuries continue to rise. Compared to other developed nations, the U.S. has the highest rate of gun ownership and the highest gun-related homicide rate. While rates of gun ownership alone do not explain why the U.S. has dramatically higher gun-related homicide rates than other developed nations—e.g., Switzerland has approximately half the rate of gun ownership as the U.S. (ranking second among OECD nations), but has one-seventh the gun homicide rate—a number of studies demonstrate positive correlations between gun ownership rates and gun-related deaths, both across nations and across states of the U.S. For example, across 26 high-income nations, greater gun availability has been associated with higher rates of gun-related homicide.17 Similarly, across states of the U.S., greater rates of household gun ownership have been associated with higher rates of gun-related homicide.18 The scientific evidence on the association between gun ownership rates and gun-related homicide is mixed and hotly debated, however.
Although a number of factors aside from gun ownership rates also likely explain greater gun-related homicides in the U.S. compared to other developed nations—e.g. differences in socioeconomic conditions, education, and income inequality—there is also evidence to suggest that gun regulatory policies themselves may have an impact on rates of violent gun injury. In the U.S. alone, states with greater numbers of gun regulatory laws are associated with lower rates of both homicides and suicides due to guns.19 Outside of the U.S., countries like Australia and Japan have received widespread attention for their strict gun ownership policies and low rates of gun-related deaths. For example, in Japan, gun ownership is restricted to a limited set of guns, only after special access is granted based on formal instruction, written, mental, and drug tests, and background checks. Similarly, Australian gun control policy has been touted as highly effective in reducing gun-related homicide rates, based on the prohibition of semi-automatic and automatic guns, massive buyback of guns, and increased licensing rules, including a need for licensees to demonstrate a “need” for a particular weapon, as well as a requirement to complete a gun safety course. Whether low gun-related homicide rates in these countries are attributable to stricter gun control policies is an area of open scientific debate.20,21
In summary, gun violence in the United States appears to be a growing, rather than stable, problem. Critics of stronger gun control legislation who focus on the stable rate of gun-related homicides in the United States are, in effect, ignoring an escalating trend in gun violence evidenced by increasing rates of non-fatal violent gun injury. Shootings, irrespective of the reason and outcome, provide a clearer measure of the impact of guns on public health.
Acknowledgements
Dr. Jena had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Support was provided by the Office of the Director, National Institutes of Health (1DP5OD017897-01, Dr. Jena).
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Contributor Information
Anupam B. Jena, Phone: +1-617-4328322, Email: jena@hcp.med.harvard.edu
Eric C. Sun, Phone: +1-301-3251458, FAX: +1-310-4517007, Email: esun1@stanford.edu
Vinay Prasad, Phone: +1-219-2290170, Email: vinayak.prasad@nih.gov
REFERENCES
- 1.Kellermann AL, Rivara FP. Silencing the science on gun research. JAMA. 2013;309:549–50. doi: 10.1001/jama.2012.208207. [DOI] [PubMed] [Google Scholar]
- 2.UNODC Homicide Statistics. 2013. (Accessed November 6, 2013, at www.unodc.org).
- 3.Wintemute GJ. Tragedy’s legacy. N Engl J Med. 2013;368:397–9. doi: 10.1056/NEJMp1215491. [DOI] [PubMed] [Google Scholar]
- 4.Years of potential life lost from unintentional injuries among persons aged 0–19 years - United States, 2000–2009. MMWR Morb Mortal Wkly Rep 2012;61:830–3. [PubMed]
- 5.Eastridge BJ, Jenkins D, Flaherty S, Schiller H, Holcomb JB. Trauma system development in a theater of war: Experiences from Operation Iraqi Freedom and Operation Enduring Freedom. J Traumatol. 2006;61:1366–72. doi: 10.1097/01.ta.0000245894.78941.90. [DOI] [PubMed] [Google Scholar]
- 6.Nguyen T, Kalish J, Woodson J. Management of civilian and military vascular trauma: lessons learned. Semin Vasc Surg. 2010;23:235–42. doi: 10.1053/j.semvascsurg.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 7.Thorson CM, Dubose JJ, Rhee P, et al. Military trauma training at civilian centers: a decade of advancements. J Traumatol Acute Care Surg. 2012;73:S483–9. doi: 10.1097/TA.0b013e31827546fb. [DOI] [PubMed] [Google Scholar]
- 8.DuBose JJ, Barmparas G, Inaba K, et al. Isolated severe traumatic brain injuries sustained during combat operations: demographics, mortality outcomes, and lessons to be learned from contrasts to civilian counterparts. J Traumatol. 2011;70:11–6. doi: 10.1097/TA.0b013e318207c563. [DOI] [PubMed] [Google Scholar]
- 9.Holcomb JB, Jenkins D, Rhee P, et al. Damage control resuscitation: directly addressing the early coagulopathy of trauma. J Traumatol. 2007;62:307–10. doi: 10.1097/TA.0b013e3180324124. [DOI] [PubMed] [Google Scholar]
- 10.Perkins JG, Schreiber MA, Wade CE, Holcomb JB. Early versus late recombinant factor VIIa in combat trauma patients requiring massive transfusion. J Traumatol. 2007;62:1095–9. doi: 10.1097/TA.0b013e31804798a4. [DOI] [PubMed] [Google Scholar]
- 11.Tracy EJ. Combining Military and Civilian Trauma Systems: The Best of Both Worlds. Adv Emerg Nurs J. 2005;27:170–5. [Google Scholar]
- 12.Hoff WS, Schwab CW. Trauma system development in North America. Clinical orthopaedics and related research 2004;422:17–22. [DOI] [PubMed]
- 13.Harris AR, Thomas SH, Fisher GA, Hirsch DJ. Murder and Medicine: The Lethality of Criminal Assault 1960–1999. Homicide Stud. 2002;6:128–66. doi: 10.1177/108876790200600203. [DOI] [Google Scholar]
- 14.Cook PJ, Lawrence BA, Ludwig J, Miller TR. The medical costs of gunshot injuries in the United States. JAMA. 1999;282:447–54. doi: 10.1001/jama.282.5.447. [DOI] [PubMed] [Google Scholar]
- 15.Pennsylvania Health Care Cost Containment Council. Firearm-related injuries in Pennsylvania; 2005.
- 16.Cook PJ, Ludwig J. Gun Violence: The Real Costs. New York: Oxford University Press; 2000. [Google Scholar]
- 17.Hemenway D, Miller M. Firearm availability and homicide rates across 26 high-income countries. J Traumatol. 2000;49:985–8. doi: 10.1097/00005373-200012000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Miller M, Hemenway D, Azrael D. State-level homicide victimization rates in the US in relation to survey measures of household firearm ownership, 2001–2003. Soc Sci Med. 2007;64:656–64. doi: 10.1016/j.socscimed.2006.09.024. [DOI] [PubMed] [Google Scholar]
- 19.Fleegler EW, Lee LK, Monuteaux MC, Hemenway D, Mannix R. Firearm legislation and firearm-related fatalities in the United States. JAMA Int Med. 2013;173:732–40. doi: 10.1001/jamainternmed.2013.1286. [DOI] [PubMed] [Google Scholar]
- 20.Chapman S, Alpers P, Agho K, Jones M. Australia’s 1996 gun law reforms: faster falls in firearm deaths, firearm suicides, and a decade without mass shootings. Inj Prev. 2006;12:365–72. doi: 10.1136/ip.2006.013714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hemenway D. How to find nothing. J Public Health Policy. 2009;30:260–8. doi: 10.1057/jphp.2009.26. [DOI] [PubMed] [Google Scholar]