Abstract
The meniscus has several important roles, such as transmission of the load, absorption of the shock in the knee joint, acting as a secondary anteroposterior stabilizer of the knee joint, and contributing to proprioception of the knee joint. Degenerative changes of the knee joint develop in the long-term follow-up even after partial meniscectomy. Thus, there has been growing interest in meniscal repair. In addition, with increased understanding of the important roles of the meniscal root and advancement of diagnostic methods, efforts have been made to ensure preservation of the meniscal roots. In this review article, we will discuss operative techniques and clinical outcomes of arthroscopic repair of the meniscus and the meniscal root and postoperative rehabilitation and complications as well.
Keywords: Knee, Meniscus, Repair
Introduction
The meniscus is responsible for load transmission and shock absorption of the tibiofemoral joint in the human knee1,2). In addition, it acts as a secondary anteroposterior stabilizer of the knee joint, contributing to proprioception of the knee joint, lubrication, and nutrition supply to the articular cartilage3,4,5).
Meniscal tears are the most common knee injuries and seen in patients of all ages due to several causes: degeneration, trauma, and discoid meniscus6). The indications and surgical techniques for excision of torn menisci have been controversial. In addition, increasing degenerative changes have been noted in long-term follow-ups after excision of torn menisci, especially after total meniscectomy7,8). In biomechanical studies, peak contact pressure was shown to increase by up to 235% after total meniscectomy9,10) and by up to 165% even after partial meniscectomy10). In contrast, the contact pressure after meniscal repair decreases almost down to the intact level10,11,12). In terms of clinical outcomes, meniscectomy has been associated with lower clinical outcome scores than meniscal repair13,14,15).
Complete removal of the meniscus is justified only when it is irreparably torn, and the meniscal rim should be preserved if at all possible16,17). The indications for partial meniscectomy are central, intra-substance meniscal lesions, unstable lesions in the white-white zone, irreducible displaced inner edge in bucket-handle tears, the flaps in flap tears, and the flaps in oblique tears16,18,19). Meniscectomy still remains as a common orthopaedic procedure although meniscal repairs are increasingly performed over meniscectomies, especially in young or adolescent patients20,21). The indications for meniscal repair have remained controversial. However, the ideal indication for meniscal repair is an acute 1 to 2 cm longitudinal peripheral tear that can be repaired in conjunction with anterior cruciate ligament (ACL) reconstruction in young patients16,22,23,24). Nevertheless, some authors reported good clinical results after repair of meniscus tears extending into the avascular zone in patients less than 20 years of age25). Other investigators performed meniscal repairs in patients with meniscal tears including those with more than 60 years of age, and they recommended meniscal repair wherever possible regardless of age26,27,28,29,30). The reparability of meniscal tears depends on several factors, such as vascularity, type of tear, chronicity, and size16). A longitudinal tear on red-red zone in an acute setting has a preferable reparability than a radial or a flap tear on white-white zone in a chronic setting16). Meniscal repair can be performed either with an open or arthroscopic technique. Arthroscopic meniscal repair has advantages over open repair in terms of minimal incision, early recovery, and rehabilitation31,32,33). Arthroscopic repair techniques can be divided into 4 categories: inside-out techniques, outside-in techniques, all-inside techniques, and hybrid techniques that combine multiple techniques16). A meniscal tear on mid-third horn or a peripheral capsule area can be repaired with inside-out technique. Repair of a meniscal tear on anterior horn or an attempt to reduction of bucket-handle tear can be performed with outside-in technique. All-inside technique can be used in a meniscal tear on posterior horn16).
In this review article, we will describe the operative methods and clinical outcomes of arthroscopic repair techniques. In addition, we will discuss operative methods and clinical outcomes of meniscal root repair because of the growing interest in the importance of the meniscal root, and rehabilitations and complications after meniscal repair as well.
Inside-Out Repair Technique
1. Operative Method
The inside-out technique can be performed using double-armed needles with an absorbable or non-absorbable suture passing through single-lumen zone-specific repair cannulas. Before meniscal repair, tear debridement and perisynovial tissue abrasion with a meniscal rasp or motorized shaver should be performed to stimulate a proliferative fibroblastic healing response16). First, a 4 to 5 cm skin incision and dissection are made along the posterior border of the collateral ligaments. For medial meniscal repair, the fascia is opened and the hamstrings and medial gastrocnemius are retracted posteriorly. A popliteal retractor can be placed in the interval between the medial head of the gastrocnemius and the posterior capsule of the joint to protect the popliteal vessels and to aid in passing the needles16). For lateral meniscal repair, the knee joint should be brought to 90° of flexion so that the peroneal nerve drops more inferiorly and is protected, and the iliotibial tract is retracted upwards and the biceps tendon downwards. Then, careful dissection should be performed to reflect the lateral gastrocnemius head off the posterior capsule. After this dissection, suturing is performed by passing a long needle with a suture attached through the cannula and then through the meniscus to exit laterally. After the first needle is passed, the cannula is repositioned at the inferior or superior articular surface of the meniscus and then a second needle is passed and retrieved (Fig. 1). After passing the needles, the sutures for the medial meniscus are tied over the joint capsule with the knee in 20° of flexion34), the sutures for the lateral meniscus are tied over the joint capsule with the knee in 90° of flexion16,35).
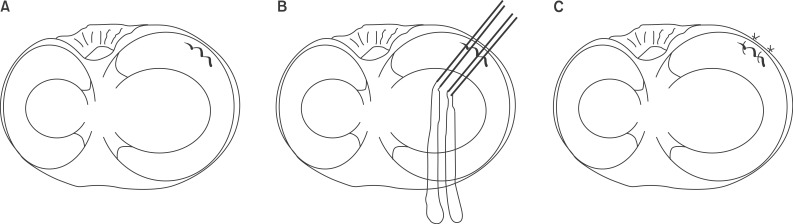
Fig. 1.
Inside-out repair technique. (A) A longitudinal tear is identified. (B) Long needles with sutures attached are passed through appropriate cannulas superior and inferior to the tear site. (C) Vertical sutures are tied over the joint capsule.
2. Clinical Outcomes
There are several studies to report clinical outcomes of meniscal repairs using an inside-out technique. Horibe et al.35) reported that 113 of 120 patients showed clinically successful results at a mean of 8-month follow-up. However, only 73% of the patients had healed completely on a second-look arthroscopy. Steenbrugge et al.30) reported that 85% of patients showed excellent or good results at a mean of 13.2-year follow-up, and no poor results were observed. Logan et al.36) studied 45 elite athletes who underwent meniscal repairs with 83% of them having a concomitant ACL reconstruction. Eighty-one percent of the patients returned to their pre-injury level sports at a mean of 10.4-month follow-up. Seven of 11 failures after meniscal repairs were associated with a new injury. They also concluded that medial meniscal repairs were significantly more likely to fail than lateral meniscal repairs. Vanderhave et al.23) compared 31 cases of inside-out meniscal repairs with concomitant ACL reconstruction in young athletes with 14 cases of meniscal repairs without ACL reconstruction. Forty-three of the 45 patients showed excellent clinical outcomes at a mean of 27-month follow-up. They reported no significantly different clinical results were observed between the medial and lateral meniscus groups. However, patients with ACL reconstruction had significantly longer return-to-activity periods and significantly lower Tegner activity scores than patients without ACL reconstruction. Ra et al.37) reviewed inside-out repair of complete radial tears of the meniscus with a fibrin clot. Eleven of 12 cases showed complete healing on magnetic resonance imaging (MRI) and 6 of 7 patients who underwent a second-look arthroscopic examination showed completely healed meniscus at a mean of 30.3-month follow-up. Haklar et al.38) studied inside-out repair of radial lateral meniscus tear by double horizontal sutures. They reported all patients showed completely healed meniscus on MRI and returned to their former level of activity at a mean of 31-month follow-up and concluded that repairing rather than resecting radial lateral meniscus tears extending into the capsular zone improved activity level. In systematic reviews, 62% of patients showed complete healing, 20% showed incomplete healing, 18% showed failed meniscal repair at a second-look arthroscopy13), and the overall clinical failure rate was 17%39).
Outside-In Repair Technique
1. Operative Method
Warren40) introduced the outside-in meniscal repair technique to decrease the risk of injury to the peroneal nerve during the procedure of lateral meniscal repair. The peroneal nerve could be protected during meniscal repair because the starting point for needle entry is controlled by the surgeon41). The outside-in technique can be used for most of the meniscal tears patterns and locations, especially tears located in the anterior horn. It can also be used to fix a transplanted meniscal allograft to the joint capsule42). The technique can be carried out using an 18-gauge spinal needle or a corresponding suture-passing needle system with a wire-looped retriever. For posteromedial repairs, the knee should be flexed to 10°-20° to allow the sartorial nerve to lie anterior to the repair site. For anteromedial repairs, the knee should be flexed to 40°-50° to allow the sartorial branch of saphenous nerve to lie posterior to the repair site. For lateral meniscal repairs, the knee should be in 90° of flexion to allow the common peroneal nerve to lie posterior to the repair site. A needle is passed from outside to inside through the tear site. Then, an absorbable or nonabsorbable suture is passed through the needle and pulled out of the anterior portal using a grasper. Then a suture-passing needle system is passed from outside to inside on the either inferior or superior articular surface of the meniscus, and a wire-looped retriever is introduced through this system. After this procedure, the first suture is withdrawn back into the joint using a grasper, and delivered through the wire loop (Fig. 2). Then, the suture is pulled out of the suture passer and tied over the joint capsule16). Horizontal mattress suture can be performed with the same method.
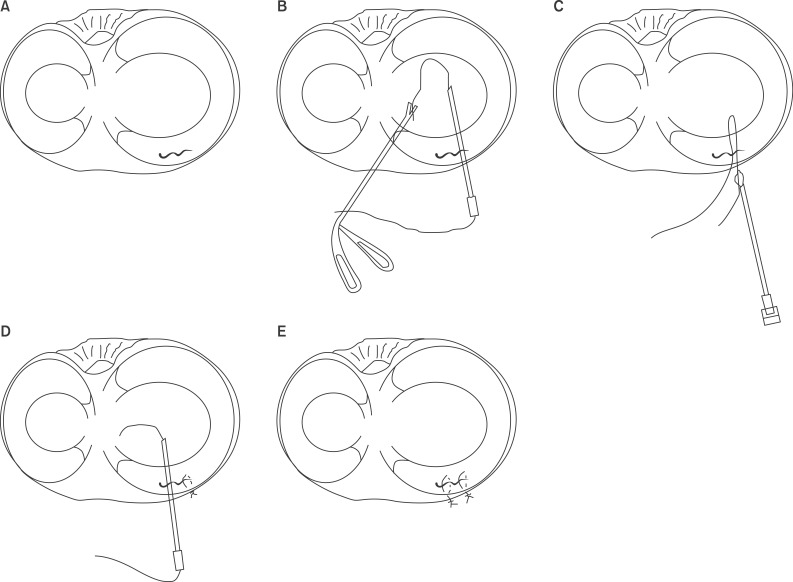
Fig. 2.
Outside-in repair technique. (A) A longitudinal tear is identified. (B) A suture material is passed through an 18-gauge spinal needle superior or inferior to the tear site, and the strand is pulled out of the other portal using a grasper. (C) After introducing a needle system with a wire-looped retriever passed through another surface of the tear site, the strand withdrawn into the joint is pulled out of the working portal. (D) The second suture can be carried out with the same procedure. (E) Vertical sutures are tied over the joint capsule.
2. Clinical Outcomes
Majewski et al.43) reported that 64 of 88 patients achieved a mean Tegner activity score of 6 points and a mean Lysholm score of 94 points at a mean of 10-year follow-up. However, failure rates were 23.9% because of re-tear of the repaired meniscus. Venkatachalam et al.44) reported that 78.6% of patients showed clinically successful outcomes at a mean of 21-month follow-up. Mariani et al.31) studied 22 meniscal repairs with concomitant ACL reconstruction for a mean of 28 months. The authors reported that 77.3% of the patients showed good clinical results. However, complete healing on MRI was observed in 45.5% of the patients, thus MRI findings were not associated with the clinical symptoms. Morgan et al.45) reported that 65% of patients showed complete healing, 19% showed asymptomatic incomplete healing, and 16% showed failed meniscal repair at a second-look arthroscopy. All failures were associated with ACL deficiencies. van Trommel et al.46) reported that 45% healed completely, 32% healed partially, and 24% failed on MRI or at second-look arthroscopy at a mean of 15-month follow-up. In a systematic review, the overall reoperation rate after outside-in meniscal repair was 25%13).
All-Inside Repair Technique
1. Operative Method
The all-inside repair technique can be used for repairing posterior horn tears. All-inside repairs have been traditionally carried out using suture hooks47). Since the introduction of self-adjusting suture devices representing the next generation of all-inside meniscal repair devices, the surgeon can use these devices for meniscal repair (Fig. 3). Currently, various suture-based fixators are available, and most of the fixators are based on a reverse-barbed fishhook design that maintains apposition and reduction of the torn fragments34). The principle is the same as that of the inside-out repair technique. The advantages of all-inside repair with suture devices include ease of use, avoidance of an accessory incision, shorter operating time, and less risk to neurovascular structures48). The disadvantages are meniscal or chondral damage from manipulation of the devices, implant migration, foreign body reactions, and higher cost16,49). The same methods used with all-inside repair devices can be applied to inside-ourt techniques. It is important to ensure enough meniscal tissue on both sides of the torn fragment to obtain sufficient tissue purchase34). Care must be taken while introducing the fixator to aim needle away from neurovascular structures and to set the needle depth penetration at 14 or 16 mm using a depth penetration limiter16,50).
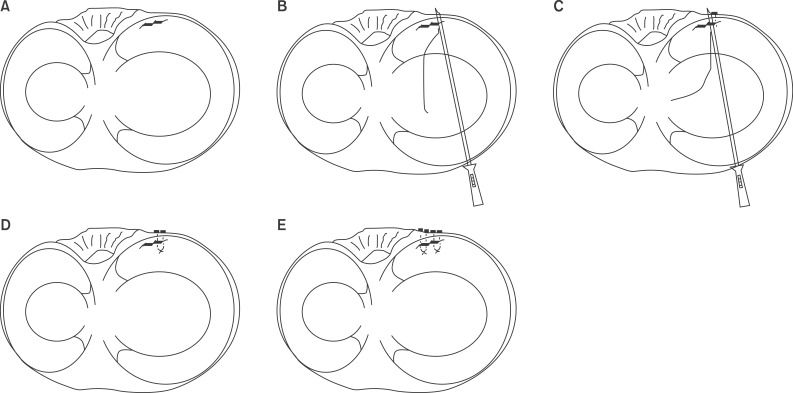
Fig. 3.
All-inside repair technique. (A) A longitudinal tear on the posterior horn is identified. (B) A suture device with self-locking knot system is passed through the tear site. (C) After fixing the first bar on the joint capsule, the suture device is passed to fix a second bar. (D) The knot can slide and be cut with a knot cutter. (E) Two horizontal sutures are performed with another suture device.
2. Clinical Outcomes
Ahn et al.47) studied 39 all-inside repair using a suture hook in ACL-deficient knees for a mean of 19 months. They reported 82.1% complete healing and 15.4% asymptomatic incomplete healing at second-look arthroscopy. Haas et al.50) reported that 86% of patients who underwent meniscal repairs by FasT-Fix device (Smith & Nephew, Andover, MA, USA) showed excellent or good clinical results at a mean of 24.3-month follow-up. Kotsovolos et al.51) studied 61 meniscal repairs using FasT-Fix device with 62% of them undergoing concomitant ACL reconstruction over 18 months. They reported that the success rate was 90.2% and simultaneous ACL reconstruction did not affect the clinical outcomes. Kocabey et al.52) reviewed 52 meniscal repairs using T-Fix (Smith & Nephew) with 62% of concomitant ACL reconstruction. They reported that 96% of patients showed excellent clinical results at a mean of 10.3-month follow-up. Asik et al.53) also studied 47 meniscal repairs using T-Fix for a mean of 26 months. They reported that 89.4% of patients showed excellent or good clinical results, and 83% of patients who underwent second-look arthroscopy showed healing. Quinby et al.54) reviewed 54 meniscal repairs using RapidLoc (DePuy Mitek Inc., Raynham, MA, USA) with concomitant ACL reconstruction. They reported that 90.7% of patients showed clinically successful results. However, Hantes et al.55) reported only 65% of patients showed clinically successful results at a mean of 22-month follow-up. Spindler et al.56) reviewed 85 meniscal repairs using Meniscus Arrow (Bionx, Blue Bell, PA, USA) with concomitant ACL reconstruction, and reported a 89% success rate over a 3-year follow-up period. Lee and Diduch57) reviewed 32 meniscal repairs using Meniscus Arrow with concomitant ACL reconstruction. They reported that there was a clinical success rate of 90.6% at a mean follow-up of 2.3 years which deteriorated to 71.4% at 6.6 years of follow-up. In a systematic review, the overall clinical failure rate was 19%39).
Meniscal Repairs in Medial Meniscal Root Tears
Meniscal root tears are radial tears or avulsions that occur at the insertion of the meniscus. Patients with meniscal root tears can complain of only minimal mechanical symptoms or discomfort with full flexion, and some patients may feel just a 'pop' in the knee joint at the moment of avulsion26,58). If torn fragments get caught in the knee joint during flexion, then patient can feel locking or pain in the knee. There is a growing concern over meniscal root tears because of the appreciation of the important physiological role played by the meniscal root as well as the advancement in various diagnostic tools59,60). According to biomechanical studies, meniscal root tears cause significant increases in tibiofemoral contact pressure which can be similar to that in the totally meniscectomied knee60,61). In addition, meniscal root tears can cause meniscal extrusion, chondral injury, and progressive osteoarthritis62,63).
While lateral meniscal root tears are commonly associated with acute ACL injuries, medial meniscal root tears often occur secondary to degenerative joint changes58,59,64). Shelbourne and Heinrich65) recommended nonoperative treatment for lateral meniscus tears, such as posterior horn tears and peripheral or posterior third tears that does not extend further than 1 cm in front of the popliteus tendon. Ahn et al.66) reported good clinical outcomes and complete healing at second-look arthroscopy after all-inside meniscal repairs using a suture hook for the lateral meniscus tears combined with ACL injuries. Unstable root tears of the posterior horn of the medial meniscus can be treated either by the aforementioned all-inside repair techniques or by the pull-out repair. The pull-out repair principle is that the meniscus should be repaired to a freshened posterior bony bed. A posteromedial portal or posterior tran-septal portal can be used for additional visualization of the medial meniscal root and its insertion site67). If the introduction of an ACL guide is limited because of the medial femoral condyle (MFC) and soft tissue overlying the posterior cruciate ligament, notchplasty for removal of the synovium and 3 to 5 mm of the articular cartilage from the posterior aspect of the MFC can be performed59). Drilling is carried out from the anterolateral tibia to the base of the root footprint using an ACL guide and then sutures are passed through the meniscus using a suture shuttle device, pulled out through the bone tunnel, and tied anteriorly (Fig. 4)16). Lee et al.26) reported that all patients were able to return to their previous life activities with little or no limitation at a mean of 31.8-month follow-up and all the patients who underwent second-look arthroscopy showed complete healing. Kim et al.28) reviewed 22 meniscal root repairs using a pull out technique for a mean of 25.9 months. They observed significant improvement in functional scores and significant decreases in meniscal extrusions on MRI. However, only 64.7% of the patients who underwent follow-up MRI showed complete healing of the meniscus on MRI. Seo et al.68) reviewed 21 meniscal root repairs with pull out techniques for 13.4 months. They reported that complete healing was not observed in any of the patients who underwent second-look arthroscopy regardless of the improvement in subjective clinical scores.
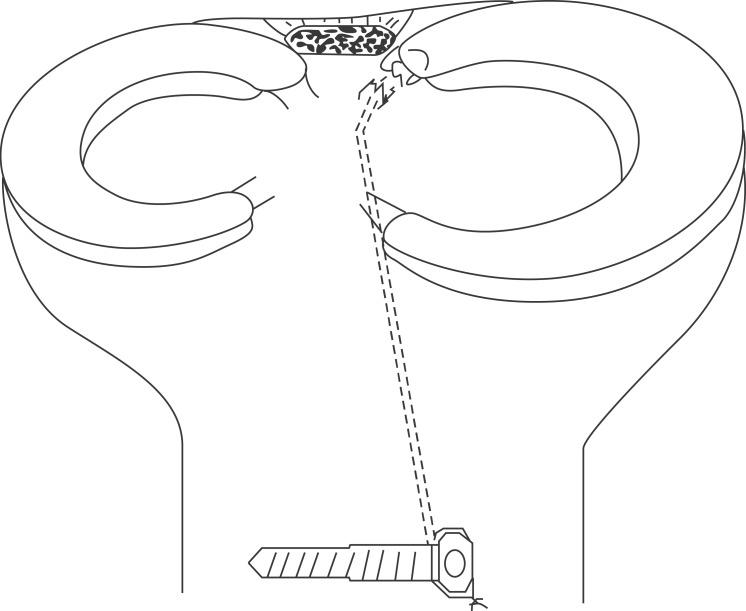
Fig. 4.
Illustration of the pull-out repair of the posterior root of the medial meniscus.
Rehabilitations after Meniscal Repair
There has been no generally accepted consensus regarding rehabilitation protocols after meniscal repairs. While some authors recommend accelerated rehabilitations with early range of motion (ROM) exercises and weight bearing31,69,70,71), other authors recommend restricted rehabilitation. Haklar et al.38) suggested immobilization with non-weight bearing for 6 to 8 postoperative weeks. Squatting beyond 120° and running activities were not allowed for 4 postoperative months. After 4 to 5 months, sporting activities were permitted. Horibe et al.35) recommended immobilization for 1 to 2 postoperative weeks, and full-weight bearing was permitted after 5 to 6 weeks. After 4 to 6 months, vigorous activities were allowed. Most authors agree that patients who have meniscal repairs in complex tear patterns need restricted rehabilitation protocols: patients can return to sports or strenuous work activities when the clinical examination reveals a non-tender joint line, absence of pain and effusion, full ROM, especially full extension, and restored muscle strength34).
Complications after Meniscal Repair
Many complications associated with meniscal repair are documented in the literatures72). Iatrogenic chondral, meniscal, or neurovascular injuries can occur during the procedure. According to a systematic review, chondral damage due to rigid meniscal implants occurred in 23% of the patients who underwent second-look arthroscopy after meniscal repair; however, this reported prevalence could have been overestimated because most second-look arthroscopies were performed in symptomatic patients39). Neurapraxia of the saphenous or peroneal nerve developed in 3 of the 191 patients (2%) with all-inside implants51,73,74) and 16 of the 142 patients (11%) with inside-out repair30,55,56,73,75). Theses nerve symptoms also resolved spontaneously without severe complications. Meniscal repairs can fail because of improperly placed or tensioned sutures or devices. Postoperative pain can remain persistent because of soft tissue irritation, foreign body reaction or inflammation, and postoperative arthrofibrosis. Overall, local irritative symptoms by all-inside implants were found in 14% of patients, which resolved spontaneously over time (within 12 months) in most cases without leaving behind major sequela51,74,76). On the other hand, all-inside suture materials had to be removed because of persistent irritative symptoms in some cases55,76,77,78). Two mid- to long-term follow-up studies using a meniscus arrow for meniscal repair reported unsatisfactory outcomes because of high failure rates of healing and persistent irritation by the arrow57,77). In other studies, one superficial infection after 20 inside-out repairs required antibiotic treatment30) and 2 deep infections after 34 inside-out repairs that occurred in one with an isolated meniscal tear and the other with concomitant ACL reconstruction were treated with arthroscopic synovectomy and resection of the meniscus73). Majewski et al.43) reported 2 infections in 50 patients after meniscal repair using an outside-in technique, but they did not indicate if the infection was superficial or deep. Spindler et al.56) observed 2 cyclops lesions in 85 patients who underwent all-inside meniscal repair using a meniscus arrow, arthroscopic debridement was the treatment of choice. Kotsovolos et al.51) reported that 4 patients who underwent all-inside meniscal repair using FasT-Fix system with concomitant ACL reconstruction had difficulty in gaining full flexion of the knee joint after operation, one of which required an arthroscopic arthrolysis.
Conclusions
Meniscal repair should be aggressively considered in young patients to enhance functional recovery and durability of the knee joint, if the meniscus is reparable. It should be considered as an option even in patients aged 60 years or older, if the meniscus is reparable. It is important for the surgeon to be equipped with familiarity with the operative indications and techniques and full knowledge of the anatomy and prescribe appropriate rehabilitation to produce good outcomes and avoid complications.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Walker PS, Erkman MJ. The role of the menisci in force transmission across the knee. Clin Orthop Relat Res. 1975;(109):184–192. doi: 10.1097/00003086-197506000-00027. [DOI] [PubMed] [Google Scholar]
- 2.Voloshin AS, Wosk J. Shock absorption of meniscectomized and painful knees: a comparative in vivo study. J Biomed Eng. 1983;5:157–161. doi: 10.1016/0141-5425(83)90036-5. [DOI] [PubMed] [Google Scholar]
- 3.Muller W. Menisci and knee stability. Orthopade. 1994;23:93–97. [PubMed] [Google Scholar]
- 4.Renstrom P, Johnson RJ. Anatomy and biomechanics of the menisci. Clin Sports Med. 1990;9:523–538. [PubMed] [Google Scholar]
- 5.Zimny ML, Albright DJ, Dabezies E. Mechanoreceptors in the human medial meniscus. Acta Anat (Basel) 1988;133:35–40. doi: 10.1159/000146611. [DOI] [PubMed] [Google Scholar]
- 6.Bellisari G, Samora W, Klingele K. Meniscus tears in children. Sports Med Arthrosc. 2011;19:50–55. doi: 10.1097/JSA.0b013e318204d01a. [DOI] [PubMed] [Google Scholar]
- 7.Johnson RJ, Kettelkamp DB, Clark W, Leaverton P. Factors effecting late results after meniscectomy. J Bone Joint Surg Am. 1974;56:719–729. [PubMed] [Google Scholar]
- 8.Wroble RR, Henderson RC, Campion ER, el-Khoury GY, Albright JP. Meniscectomy in children and adolescents: a long-term follow-up study. Clin Orthop Relat Res. 1992;(279):180–189. [PubMed] [Google Scholar]
- 9.Fukubayashi T, Kurosawa H. The contact area and pressure distribution pattern of the knee. A study of normal and osteoarthrotic knee joints. Acta Orthop Scand. 1980;51:871–879. doi: 10.3109/17453678008990887. [DOI] [PubMed] [Google Scholar]
- 10.Baratz ME, Fu FH, Mengato R. Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee: a preliminary report. Am J Sports Med. 1986;14:270–275. doi: 10.1177/036354658601400405. [DOI] [PubMed] [Google Scholar]
- 11.Ode GE, Van Thiel GS, McArthur SA, Dishkin-Paset J, Leurgans SE, Shewman EF, Wang VM, Cole BJ. Effects of serial sectioning and repair of radial tears in the lateral meniscus. Am J Sports Med. 2012;40:1863–1870. doi: 10.1177/0363546512453291. [DOI] [PubMed] [Google Scholar]
- 12.Muriuki MG, Tuason DA, Tucker BG, Harner CD. Changes in tibiofemoral contact mechanics following radial split and vertical tears of the medial meniscus an in vitro investigation of the efficacy of arthroscopic repair. J Bone Joint Surg Am. 2011;93:1089–1095. doi: 10.2106/JBJS.I.01241. [DOI] [PubMed] [Google Scholar]
- 13.Paxton ES, Stock MV, Brophy RH. Meniscal repair versus partial meniscectomy: a systematic review comparing reoperation rates and clinical outcomes. Arthroscopy. 2011;27:1275–1288. doi: 10.1016/j.arthro.2011.03.088. [DOI] [PubMed] [Google Scholar]
- 14.Salata MJ, Gibbs AE, Sekiya JK. A systematic review of clinical outcomes in patients undergoing meniscectomy. Am J Sports Med. 2010;38:1907–1916. doi: 10.1177/0363546510370196. [DOI] [PubMed] [Google Scholar]
- 15.Stein T, Mehling AP, Welsch F, von Eisenhart-Rothe R, Jager A. Long-term outcome after arthroscopic meniscal repair versus arthroscopic partial meniscectomy for traumatic meniscal tears. Am J Sports Med. 2010;38:1542–1548. doi: 10.1177/0363546510364052. [DOI] [PubMed] [Google Scholar]
- 16.Canale ST, Beaty JH. Campbell's operative orthopaedics. 12th ed. St Louis, MO: Mosby; 2012. pp. 2075–2078.pp. 2014 [Google Scholar]
- 17.Chatain F, Robinson AH, Adeleine P, Chambat P, Neyret P. The natural history of the knee following arthroscopic medial meniscectomy. Knee Surg Sports Traumatol Arthrosc. 2001;9:15–18. doi: 10.1007/s001670000146. [DOI] [PubMed] [Google Scholar]
- 18.Day B, Mackenzie WG, Shim SS, Leung G. The vascular and nerve supply of the human meniscus. Arthroscopy. 1985;1:58–62. doi: 10.1016/s0749-8063(85)80080-3. [DOI] [PubMed] [Google Scholar]
- 19.Biedert RM. Treatment of intrasubstance meniscal lesions: a randomized prospective study of four different methods. Knee Surg Sports Traumatol Arthrosc. 2000;8:104–108. doi: 10.1007/s001670050195. [DOI] [PubMed] [Google Scholar]
- 20.Montgomery SR, Zhang A, Ngo SS, Wang JC, Hame SL. Cross-sectional analysis of trends in meniscectomy and meniscus repair. Orthopedics. 2013;36:e1007–e1013. doi: 10.3928/01477447-20130724-15. [DOI] [PubMed] [Google Scholar]
- 21.Abrams GD, Frank RM, Gupta AK, Harris JD, McCormick FM, Cole BJ. Trends in meniscus repair and meniscectomy in the United States, 2005-2011. Am J Sports Med. 2013;41:2333–2339. doi: 10.1177/0363546513495641. [DOI] [PubMed] [Google Scholar]
- 22.Pujol N, Beaufils P. Healing results of meniscal tears left in situ during anterior cruciate ligament reconstruction: a review of clinical studies. Knee Surg Sports Traumatol Arthrosc. 2009;17:396–401. doi: 10.1007/s00167-008-0711-y. [DOI] [PubMed] [Google Scholar]
- 23.Vanderhave KL, Moravek JE, Sekiya JK, Wojtys EM. Meniscus tears in the young athlete: results of arthroscopic repair. J Pediatr Orthop. 2011;31:496–500. doi: 10.1097/BPO.0b013e31821ffb8d. [DOI] [PubMed] [Google Scholar]
- 24.Tenuta JJ, Arciero RA. Arthroscopic evaluation of meniscal repairs: factors that effect healing. Am J Sports Med. 1994;22:797–802. doi: 10.1177/036354659402200611. [DOI] [PubMed] [Google Scholar]
- 25.Noyes FR, Barber-Westin SD. Arthroscopic repair of meniscal tears extending into the avascular zone in patients younger than twenty years of age. Am J Sports Med. 2002;30:589–600. doi: 10.1177/03635465020300042001. [DOI] [PubMed] [Google Scholar]
- 26.Lee JH, Lim YJ, Kim KB, Kim KH, Song JH. Arthroscopic pullout suture repair of posterior root tear of the medial meniscus: radiographic and clinical results with a 2-year follow-up. Arthroscopy. 2009;25:951–958. doi: 10.1016/j.arthro.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 27.Noyes FR, Barber-Westin SD. Arthroscopic repair of meniscus tears extending into the avascular zone with or without anterior cruciate ligament reconstruction in patients 40 years of age and older. Arthroscopy. 2000;16:822–829. doi: 10.1053/jars.2000.19434. [DOI] [PubMed] [Google Scholar]
- 28.Kim JH, Chung JH, Lee DH, Lee YS, Kim JR, Ryu KJ. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: a prospective comparison study. Arthroscopy. 2011;27:1644–1653. doi: 10.1016/j.arthro.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 29.Barrett GR, Field MH, Treacy SH, Ruff CG. Clinical results of meniscus repair in patients 40 years and older. Arthroscopy. 1998;14:824–829. doi: 10.1016/s0749-8063(98)70018-0. [DOI] [PubMed] [Google Scholar]
- 30.Steenbrugge F, Verdonk R, Hurel C, Verstraete K. Arthroscopic meniscus repair: inside-out technique vs. Biofix meniscus arrow. Knee Surg Sports Traumatol Arthrosc. 2004;12:43–49. doi: 10.1007/s00167-003-0446-8. [DOI] [PubMed] [Google Scholar]
- 31.Mariani PP, Santori N, Adriani E, Mastantuono M. Accelerated rehabilitation after arthroscopic meniscal repair: a clinical and magnetic resonance imaging evaluation. Arthroscopy. 1996;12:680–686. doi: 10.1016/s0749-8063(96)90170-x. [DOI] [PubMed] [Google Scholar]
- 32.Vander Schilden JL. Improvements in rehabilitation of the postmeniscectomized or meniscal-repaired patient. Clin Orthop Relat Res. 1990;(252):73–79. [PubMed] [Google Scholar]
- 33.Fazalare JJ, McCormick KR, Babins DB. Meniscal repair of the knee. Orthopedics. 2009;32:199. doi: 10.3928/01477447-20090301-09. [DOI] [PubMed] [Google Scholar]
- 34.Sgaglione NA, Steadman JR, Shaffer B, Miller MD, Fu FH. Current concepts in meniscus surgery: resection to replacement. Arthroscopy. 2003;19(Suppl 1):161–188. doi: 10.1016/j.arthro.2003.10.032. [DOI] [PubMed] [Google Scholar]
- 35.Horibe S, Shino K, Nakata K, Maeda A, Nakamura N, Matsumoto N. Second-look arthroscopy after meniscal repair: review of 132 menisci repaired by an arthroscopic inside-out technique. J Bone Joint Surg Br. 1995;77:245–249. [PubMed] [Google Scholar]
- 36.Logan M, Watts M, Owen J, Myers P. Meniscal repair in the elite athlete: results of 45 repairs with a minimum 5-year follow-up. Am J Sports Med. 2009;37:1131–1134. doi: 10.1177/0363546508330138. [DOI] [PubMed] [Google Scholar]
- 37.Ra HJ, Ha JK, Jang SH, Lee DW, Kim JG. Arthroscopic inside-out repair of complete radial tears of the meniscus with a fibrin clot. Knee Surg Sports Traumatol Arthrosc. 2013;21:2126–2130. doi: 10.1007/s00167-012-2191-3. [DOI] [PubMed] [Google Scholar]
- 38.Haklar U, Kocaoglu B, Nalbantoglu U, Tuzuner T, Guven O. Arthroscopic repair of radial lateral meniscus tear by double horizontal sutures with inside-outside technique. Knee. 2008;15:355–359. doi: 10.1016/j.knee.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 39.Grant JA, Wilde J, Miller BS, Bedi A. Comparison of inside-out and all-inside techniques for the repair of isolated meniscal tears: a systematic review. Am J Sports Med. 2012;40:459–468. doi: 10.1177/0363546511411701. [DOI] [PubMed] [Google Scholar]
- 40.Warren RF. Arthroscopic meniscus repair. Arthroscopy. 1985;1:170–172. doi: 10.1016/s0749-8063(85)80005-0. [DOI] [PubMed] [Google Scholar]
- 41.Morgan CD, Casscells SW. Arthroscopic meniscus repair: a safe approach to the posterior horns. Arthroscopy. 1986;2:3–12. doi: 10.1016/s0749-8063(86)80003-2. [DOI] [PubMed] [Google Scholar]
- 42.Rodeo SA. Arthroscopic meniscal repair with use of the outside-in technique. Instr Course Lect. 2000;49:195–206. [PubMed] [Google Scholar]
- 43.Majewski M, Stoll R, Widmer H, Muller W, Friederich NF. Midterm and long-term results after arthroscopic suture repair of isolated, longitudinal, vertical meniscal tears in stable knees. Am J Sports Med. 2006;34:1072–1076. doi: 10.1177/0363546505284236. [DOI] [PubMed] [Google Scholar]
- 44.Venkatachalam S, Godsiff SP, Harding ML. Review of the clinical results of arthroscopic meniscal repair. Knee. 2001;8:129–133. doi: 10.1016/s0968-0160(01)00061-8. [DOI] [PubMed] [Google Scholar]
- 45.Morgan CD, Wojtys EM, Casscells CD, Casscells SW. Arthroscopic meniscal repair evaluated by second-look arthroscopy. Am J Sports Med. 1991;19:632–637. doi: 10.1177/036354659101900614. [DOI] [PubMed] [Google Scholar]
- 46.van Trommel MF, Simonian PT, Potter HG, Wickiewicz TL. Different regional healing rates with the outside-in technique for meniscal repair. Am J Sports Med. 1998;26:446–452. doi: 10.1177/03635465980260031901. [DOI] [PubMed] [Google Scholar]
- 47.Ahn JH, Wang JH, Yoo JC. Arthroscopic all-inside suture repair of medial meniscus lesion in anterior cruciate ligament: deficient knees: results of second-look arthroscopies in 39 cases. Arthroscopy. 2004;20:936–945. doi: 10.1016/j.arthro.2004.06.038. [DOI] [PubMed] [Google Scholar]
- 48.Lozano J, Ma CB, Cannon WD. All-inside meniscus repair: a systematic review. Clin Orthop Relat Res. 2007;455:134–141. doi: 10.1097/BLO.0b013e31802ff806. [DOI] [PubMed] [Google Scholar]
- 49.Barber FA, McGarry JE. Meniscal repair techniques. Sports Med Arthrosc. 2007;15:199–207. doi: 10.1097/JSA.0b013e3181595bed. [DOI] [PubMed] [Google Scholar]
- 50.Haas AL, Schepsis AA, Hornstein J, Edgar CM. Meniscal repair using the FasT-Fix all-inside meniscal repair device. Arthroscopy. 2005;21:167–175. doi: 10.1016/j.arthro.2004.10.012. [DOI] [PubMed] [Google Scholar]
- 51.Kotsovolos ES, Hantes ME, Mastrokalos DS, Lorbach O, Paessler HH. Results of all-inside meniscal repair with the FasT-Fix meniscal repair system. Arthroscopy. 2006;22:3–9. doi: 10.1016/j.arthro.2005.10.017. [DOI] [PubMed] [Google Scholar]
- 52.Kocabey Y, Nyland J, Isbell WM, Caborn DN. Patient outcomes following T-Fix meniscal repair and a modifiable, progressive rehabilitation program, a retrospective study. Arch Orthop Trauma Surg. 2004;124:592–596. doi: 10.1007/s00402-004-0649-6. [DOI] [PubMed] [Google Scholar]
- 53.Asik M, Sen C, Erginsu M. Arthroscopic meniscal repair using T-fix. Knee Surg Sports Traumatol Arthrosc. 2002;10:284–288. doi: 10.1007/s00167-002-0296-9. [DOI] [PubMed] [Google Scholar]
- 54.Quinby JS, Golish SR, Hart JA, Diduch DR. All-inside meniscal repair using a new flexible, tensionable device. Am J Sports Med. 2006;34:1281–1286. doi: 10.1177/0363546505286143. [DOI] [PubMed] [Google Scholar]
- 55.Hantes ME, Zachos VC, Varitimidis SE, Dailiana ZH, Karachalios T, Malizos KN. Arthroscopic meniscal repair: a comparative study between three different surgical techniques. Knee Surg Sports Traumatol Arthrosc. 2006;14:1232–1237. doi: 10.1007/s00167-006-0094-x. [DOI] [PubMed] [Google Scholar]
- 56.Spindler KP, McCarty EC, Warren TA, Devin C, Connor JT. Prospective comparison of arthroscopic medial meniscal repair technique: inside-out suture versus entirely arthroscopic arrows. Am J Sports Med. 2003;31:929–934. doi: 10.1177/03635465030310063101. [DOI] [PubMed] [Google Scholar]
- 57.Lee GP, Diduch DR. Deteriorating outcomes after meniscal repair using the Meniscus Arrow in knees undergoing concurrent anterior cruciate ligament reconstruction: increased failure rate with long-term follow-up. Am J Sports Med. 2005;33:1138–1141. doi: 10.1177/0363546505275348. [DOI] [PubMed] [Google Scholar]
- 58.Koenig JH, Ranawat AS, Umans HR, Difelice GS. Meniscal root tears: diagnosis and treatment. Arthroscopy. 2009;25:1025–1032. doi: 10.1016/j.arthro.2009.03.015. [DOI] [PubMed] [Google Scholar]
- 59.Vyas D, Harner CD. Meniscus root repair. Sports Med Arthrosc. 2012;20:86–94. doi: 10.1097/JSA.0b013e31825186ca. [DOI] [PubMed] [Google Scholar]
- 60.Kim JG, Lee YS, Bae TS, Ha JK, Lee DH, Kim YJ, Ra HJ. Tibiofemoral contact mechanics following posterior root of medial meniscus tear, repair, meniscectomy, and allograft transplantation. Knee Surg Sports Traumatol Arthrosc. 2013;21:2121–2125. doi: 10.1007/s00167-012-2182-4. [DOI] [PubMed] [Google Scholar]
- 61.Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90:1922–1931. doi: 10.2106/JBJS.G.00748. [DOI] [PubMed] [Google Scholar]
- 62.Bin SI, Kim JM, Shin SJ. Radial tears of the posterior horn of the medial meniscus. Arthroscopy. 2004;20:373–378. doi: 10.1016/j.arthro.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 63.Lerer DB, Umans HR, Hu MX, Jones MH. The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol. 2004;33:569–574. doi: 10.1007/s00256-004-0761-2. [DOI] [PubMed] [Google Scholar]
- 64.Brody JM, Lin HM, Hulstyn MJ, Tung GA. Lateral meniscus root tear and meniscus extrusion with anterior cruciate ligament tear. Radiology. 2006;239:805–810. doi: 10.1148/radiol.2393050559. [DOI] [PubMed] [Google Scholar]
- 65.Shelbourne KD, Heinrich J. The long-term evaluation of lateral meniscus tears left in situ at the time of anterior cruciate ligament reconstruction. Arthroscopy. 2004;20:346–351. doi: 10.1016/j.arthro.2004.01.029. [DOI] [PubMed] [Google Scholar]
- 66.Ahn JH, Lee YS, Chang JY, Chang MJ, Eun SS, Kim SM. Arthroscopic all inside repair of the lateral meniscus root tear. Knee. 2009;16:77–80. doi: 10.1016/j.knee.2008.07.008. [DOI] [PubMed] [Google Scholar]
- 67.Ahn JH, Wang JH, Yoo JC, Noh HK, Park JH. A pull out suture for transection of the posterior horn of the medial meniscus: using a posterior trans-septal portal. Knee Surg Sports Traumatol Arthrosc. 2007;15:1510–1513. doi: 10.1007/s00167-007-0310-3. [DOI] [PubMed] [Google Scholar]
- 68.Seo HS, Lee SC, Jung KA. Second-look arthroscopic findings after repairs of posterior root tears of the medial meniscus. Am J Sports Med. 2011;39:99–107. doi: 10.1177/0363546510382225. [DOI] [PubMed] [Google Scholar]
- 69.Barber FA. Accelerated rehabilitation for meniscus repairs. Arthroscopy. 1994;10:206–210. doi: 10.1016/s0749-8063(05)80095-7. [DOI] [PubMed] [Google Scholar]
- 70.Kozlowski EJ, Barcia AM, Tokish JM. Meniscus repair: the role of accelerated rehabilitation in return to sport. Sports Med Arthrosc. 2012;20:121–126. doi: 10.1097/JSA.0b013e318253d7c6. [DOI] [PubMed] [Google Scholar]
- 71.Shelbourne KD, Patel DV, Adsit WS, Porter DA. Rehabilitation after meniscal repair. Clin Sports Med. 1996;15:595–612. [PubMed] [Google Scholar]
- 72.Gwathmey FW, Jr, Golish SR, Diduch DR. Complications in brief: meniscus repair. Clin Orthop Relat Res. 2012;470:2059–2066. doi: 10.1007/s11999-012-2303-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Albrecht-Olsen P, Kristensen G, Burgaard P, Joergensen U, Toerholm C. The arrow versus horizontal suture in arthroscopic meniscus repair. A prospective randomized study with arthroscopic evaluation. Knee Surg Sports Traumatol Arthrosc. 1999;7:268–273. doi: 10.1007/s001670050162. [DOI] [PubMed] [Google Scholar]
- 74.Koukoulias N, Papastergiou S, Kazakos K, Poulios G, Parisis K. Clinical results of meniscus repair with the meniscus arrow: a 4- to 8-year follow-up study. Knee Surg Sports Traumatol Arthrosc. 2007;15:133–137. doi: 10.1007/s00167-006-0141-7. [DOI] [PubMed] [Google Scholar]
- 75.Cannon WD, Jr, Vittori JM. The incidence of healing in arthroscopic meniscal repairs in anterior cruciate ligament-reconstructed knees versus stable knees. Am J Sports Med. 1992;20:176–181. doi: 10.1177/036354659202000214. [DOI] [PubMed] [Google Scholar]
- 76.Jones HP, Lemos MJ, Wilk RM, Smiley PM, Gutierrez R, Schepsis AA. Two-year follow-up of meniscal repair using a bioabsorbable arrow. Arthroscopy. 2002;18:64–69. doi: 10.1053/jars.2002.25343. [DOI] [PubMed] [Google Scholar]
- 77.Kurzweil PR, Tifford CD, Ignacio EM. Unsatisfactory clinical results of meniscal repair using the meniscus arrow. Arthroscopy. 2005;21:905. doi: 10.1016/j.arthro.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 78.Tsai AM, McAllister DR, Chow S, Young CR, Hame SL. Results of meniscal repair using a bioabsorbable screw. Arthroscopy. 2004;20:586–590. doi: 10.1016/j.arthro.2004.04.064. [DOI] [PubMed] [Google Scholar]