Abstract
A 64-year-old male patient was admitted with respiratory failure, although chest X-rays revealed only mild bronchiolitis. Streptococcus pneumoniae, which usually presents as massive lobular pneumonia, was isolated from sputum, however, pan-pathogen screening using a next-generation sequencer also detected human metapneumovirus genome fragments.
Keywords: Human metapneumovirus, Streptococcus pneumoniae, Next-generation sequencer, Real-time PCR, Co-infection
Introduction
It has been reported that Human metapneumovirus (hMPV) was associated with various upper and lower respiratory tract syndromes, including common colds, bronchitis, pneumonia, and asthma exacerbation, with more severe diseases reported for young children, elderly subjects, and immunocompromised patients [1–3].
In adults, large outbreaks of hMPV infection in long-term care facilities (LTCF) have been reported, the magnitude and severity of which were similar to those of outbreaks typically associated with influenza or RS virus infection [4,5]. Boivin et al. reported that 9 (9.4%) of 96 patients in the LTCF died due to respiratory infection, including 3 patients who had confirmed hMPV infection [4].
In this report, we found a severe respiratory failure case due to co-infection hMPV and Streptococcus pneumoniae in adult patient, and this case was diagnosed by not only routine microbiological methods and but also genetic analysis, including next-generation sequencer.
Case report
A 64-year-old male patient who had been followed up for mild dilated cardiomyopathy became dyspneic and was admitted to our hospital in March 2013. He had been febrile (37.5 °C) for 1 week and had been coughing and short of breath for 2 days although he was a nonsmoker.
His physiological parameters upon admission were as follows: blood pressure 94/52 mmHg, respiratory rate 24 breaths/min and PaO2 62 mmHg, despite the immediate administration of supplemental oxygen (10 L/min).
Laboratory studies revealed no leukocytosis (white blood cells, 3500/mL), but its differentiation was as follows: Neu 87.5%, Lym 7.6%, Mono 3.8%, Eo: 0.6%, and Baso 0.4%, respectively, and inflammation was indicated by C-reactive protein 26.79 mg/dL (<0.8 mg/dL). In addition, aspartate transaminase 291 U/L and alanine transaminase 381 U/L; mild renal dysfunction was indicated by creatinine 1.18 mg/dL and blood urea nitrogen59 mg/dL. A normal brain natriuretic peptide (BNP) level of 315.4 mg/mL and barely detectable troponin I (0.09 ng/mL) suggested that heart failure had not worsened and that the patient did not have myocardial infarction.
We isolated S. pneumoniae, which usually causes lobular pneumonia and/or bronchopneumonia, from the patient's sputum samples. Gram staining of the sputum also showed typical lancet-shaped Gram-positive diplococcic. We did not isolated S. pneumoniae from the blood samples, but the rapid antigen test of urine for S. pneumoniae (Binax Now, Binax, Portland, USA) was also positive. The serotype of the isolated S. pneumoniae was 23F deteremined by Quellung reaction, and the MICs in parentheses indicated that the organism was susceptible to ampicillin (2 μg/mL), ceftriaxon (1 μg/mL), levofloxacin (0.5 μg/mL) and meropenem (0.5 μg/mL) determined by using an automated identification system (MicroScan WalkAway; Siemens, Munich, Germany).
However, in addition to no leukocytosis, chest radiography and computed tomography did not reveal a massive infiltration shadow, but rather showed only very mild bronchiolitis, although the patient required ventilator control after admission (Fig. 1). Therefore, we again considered panbronchiolitis due to atypical pathogens, including mycoplasma, viruses and Chlamydia. However, antibodies against Mycoplasma pneumoniae, Chlamydophila pneumoniae and Chlamydophila psittaci were negative, and paired sera did not change. Immunochromatography with Esplain Influenza A&B (Fujirebio Diagnostics Inc., Tokyo, Japan) and Quicknavi-RSV (Otsuka Pharmaceutical Co. Ltd., Tokyo, Japan) confirmed that he was negative for the influenza virus and RSV antigen, respectively.
Fig. 1.

Chest radiography (A) and computed tomography (B) images upon admission. Absence of consolidation and small multiple lobular shadows in upper and middle fields of right lung suggests bronchiolitis.
Shotgun sequencing of nucleic acids extracted from sputum samples using the MiSeq next-generation DNA sequencer (Illumina, San Diego, CA, USA) as described [6], which was performed routinely for difficult to diagnosis cases in our department, detected a 151-base sequence with 99% similarity to a moiety of the human metapneumovirus (hMPV) genome (Fig. 2). Furthermore, hMPV genes were detected in sputum by regular nested-PCR, and the sequence of this amplicon was reconfirmed as that of hMPV after the extraction of the PCR product. We also confirmed the findings by real-time PCR (Taqman, Light cycler 480, Roche, Basel, Switzerland), which detected 1.9 × 104 copies/mL of the hMPV gene. Diluted antibody for hMPV in his serum was significantly increased to ×10,240, but the rapid antigen detection test (Check hMPV: Meiji Seika Pharma, Tokyo, Japan) was negative.
Fig. 2.
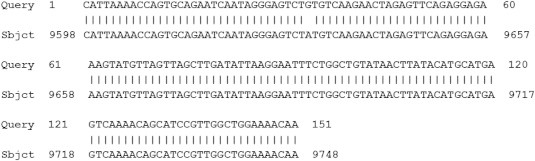
Genetic analysis of hMPV in sputum. Alignment of complete HMPV genome sequence by nucleotide sequence using BLASTN. Reading obtained with MiSeq sequencer (query) was compared with that of HMPV strain Sabana (Subject: NCBI accession number, HM197719.1).
We diagnosed severe respiratory failure due to panbronchiolitis caused by hMPV and S. pneumoniae co-infection. Administration of minocycline (2 × 100 mg/day) and meropenem (3 × 1 g/day) were started because we suspected not only S. pneumonaie infection, but also other pathogens including mycoplasma initially. Minocycline was suspended at Day 3, but meropenem was continued for 10 days. These antibacterial therapy and careful respiratory management led to complete recovery.
Discussion
Interactions between viral and bacterial disease are usually interpreted as viral infections predisposing individuals to severe bacterial infections [7,8]. Various mechanisms have been proposed, including virus-induced damage to respiratory cells causing a predisposition to opportunistic bacterial infection or the up-regulation of bacterial adhesion molecules by viral infection [9].
The present study found that exposure to hMPV might modulate S. pneumoniae infection. Verkaik et al. screened 57 children aged up to 2 years for colonization with four common respiratory bacterial species associated with seroconversion to hMPV [10]. Whereas a relationship was between exposure to Haemophilus influenzae, Moraxella catarrhalis or Staphylococcus aureus and hMPV seroconversion was not identified, S. pneumoniae exposure was significantly associated with increased seroconversion to hMPV. This increase might have been due to increased susceptibility to hMPV infection, increased viral replication or virus spread or enhanced immune responses [10]. The authors concluded from the serological data that either hMPV infection leads to more frequent S. pneumoniae carriage or exposure to S. pneumoniae increases susceptibility to hMPV infection.
Kukavica-Ibrulj et al. also found that hMPV infection predisposes mice to severe pneumococcal pneumonia [2]. They used an established experimental murine model to validate the hypothesis that hMPV, like influenza virus, increases pneumococcus replication in the lungs and enhances host immunological responses [8]. Secondary bacterial infections often complicate respiratory viral infections, although the mechanisms through which viruses predispose hosts to exacerbated bacterial disease are not completely understood. The most frequently postulated mechanisms include viral destruction of the respiratory epithelium that might increase bacterial adhesion, virus-induced immunosuppression that can lead to bacterial superinfection and an inflammatory response to viral infection that might up-regulate the expression of molecules that bacteria utilize as receptors [2,11].
We found only mild bronchiolitis on chest X-ray and CT images in our patient, although he had symptoms of severe respiratory failure. S. pneumoniae usually induces lobular pneumonia or bronchopneumonia when it became a major pathogen. Therefore, hMPV in our patient dominantly infected and induced severe damage to bronchiolar regions, and this process was accelerated by S. pneumoniae infection. Colonizing S. pneumoniae might increase hMPV infection and replication, and the number of S. pneumoniae also synergistically increased. A significant increase in hMPV antibody during the acute phase also suggested previous hMPV infection followed by S. pneumoniae infection in our patient. The mechanisms of severe respiratory failure due to hMPV infection followed by S. pneumoniae should be further studied.
We detected hMPV sequences from the patient's sputum and confirmed the findings by real-time PCR, which detected 1.9 × 104 copies/mL of the hMPV gene. These results suggested that such genetic analysis is valuable when patients present with infection caused by hMPV. We did not detect hMPV antigen by immunochromatography using Check hMPV, which usually detects 1 × 106 copies/mL of the hMPV gene [12,13]. The discrepancy between the positive genetic findings and the negative antigen assays also indicates the value of genetic analysis. Although high-throughput next-generation sequencing technologies might be difficult to apply to routine clinical diagnosis, they have potential for clinical genomic studies, as they can exceed the data output of the most sophisticated capillary sequencers based on the Sanger method [14]. We suggest that genetic analysis of samples along with cultures should become routine practice [15].
In conclusion, we described severe respiratory failure caused by co-infection with hMPV and S. pneumoniae in a patient whose chest X-ray and CT images showed only mild bronchitis. Genetic analysis, such as next-generation sequencing, revealed hMPV infection. Synergistic effects between hMPV and bacteria should be fully investigated.
References
- 1.Boivin G., Abed Y., Pelletier G., Ruel L., Moisan D., Côté S. Virological features and clinical manifestations associated with human metapneumovirus: a new paramyxovirus responsible for acute respiratory-tract infections in all age groups. J Infect Dis. 2002;186:1330–1340. doi: 10.1086/344319. [DOI] [PubMed] [Google Scholar]
- 2.Kukavica-Ibrulj I., Hamelin M.E., Prince G.A., Gagnon C., Bergeron Y., Bergeron M.G. Infection with human metapneumovirus predisposes mice to severe pneumococcal pneumonia. J Virol. 2009;83:1341–1349. doi: 10.1128/JVI.01123-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Deyde V.M., Xu X., Bright R.A., Shaw M., Smith C.B., Zhang Y. Surveillance of resistance to adamantanes among influenza A(H3N2) and A(H1N1) viruses isolated worldwide. Infect Dis. 2007;196:630–632. doi: 10.1086/518936. [DOI] [PubMed] [Google Scholar]
- 4.Boivin G., De Serres G., Hamelin M.E., Côté S., Argouin M., Tremblay G. An outbreak of severe respiratory tract infection due to human metapneumovirus in a long-term care facility. 2007;44:1152–1158. doi: 10.1086/513204. [DOI] [PubMed] [Google Scholar]
- 5.Honda H., Iwahashi J., Kashiwagi T., Imamura Y., Hamada N., Anraku T. Outbreak of human metapneumovirus infection in elderly inpatients in Japan. J Am Geriatr Soc. 2006;54:177–180. doi: 10.1111/j.1532-5415.2005.00575_10.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nakamura S., Nakaya T., Iida T. Metagenomic analysis of bacterial infections by means of high-throughput DNA sequencing. Exp Biol Med. 2011;236:968–971. doi: 10.1258/ebm.2011.010378. [DOI] [PubMed] [Google Scholar]
- 7.Stensballe L.G., Hjuler T., Andersen A., Kaltoft M., Ravn H., Aaby P. Hospitalization for respiratory syncytial virus infection and invasive pneumococcal disease in Danish children aged <2 years: a population-based cohort study. Clin Infect Dis. 2008;46:1165–1171. doi: 10.1086/529438. [DOI] [PubMed] [Google Scholar]
- 8.Seki M., Yanagihara K., Higashiyama Y., Fukuda Y., Kaneko Y., Ohno H. Immunokinetics in severe pneumonia due to influenza virus and bacteria coinfection in mice. Eur Respir J. 2004;24:143–149. doi: 10.1183/09031936.04.00126103. [DOI] [PubMed] [Google Scholar]
- 9.Ishizuka S., Yamaya M., Suzuki T., Takahashi H., Ida S., Sasaki T. Effects of rhinovirus infection on the adherence of Streptococcus pneumoniae to cultured human airway epithelial cells. J Infect Dis. 2003;188:1928–1939. doi: 10.1086/379833. [DOI] [PubMed] [Google Scholar]
- 10.Verkaik N.J., Nguyen D.T., de Vogel C.P., Moll H.A., Verbrugh H.A., Jaddoe V.W. Streptococcus pneumoniae exposure is associated with human metapneumovirus seroconversion and increased susceptibility to in vitro HMPV infection. Clin Microbiol Infect. 2011;17:1840–1844. doi: 10.1111/j.1469-0691.2011.03480.x. [DOI] [PubMed] [Google Scholar]
- 11.Peltola V.T., McCullers J.A. Respiratory viruses predisposing to bacterial infections: role of neuraminidase. Pediatr Infect Dis J. 2004;23:S87–S97. doi: 10.1097/01.inf.0000108197.81270.35. [DOI] [PubMed] [Google Scholar]
- 12.Matsuzaki Y., Takashita E., Okamoto M., Mizuta K., Itagaki T., Katsushima F. Evaluation of a new rapid antigen test using immunochromatography for detection of human metapneumovirus in comparison with real-time PCR assay. J Clin Microbiol. 2009;47:2981–2984. doi: 10.1128/JCM.00321-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hamada N., Hara K., Matsuo Y., Imamura Y., Kashiwagi T., Nakazono Y. Performance of a rapid human metapneumovirus antigen test during an outbreak in a long-term care facility. Epidemiol Infect. 2013;23:1–4. doi: 10.1017/S0950268813001246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pareek C.S., Smoczynski R., Tretyn A. Sequencing technologies and genome sequencing. J Appl Genet. 2011;52:413–435. doi: 10.1007/s13353-011-0057-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Seki M., Gotoh K., Nakamura S., Akeda Y., Yoshii T., Miyaguchi S. Fatal sepsis caused by an unusual Klebsiella species that was misidentified by an automated identification system. J Med Microbiol. 2013;62:801–803. doi: 10.1099/jmm.0.051334-0. [DOI] [PubMed] [Google Scholar]


