Abstract
A 44 year old male former smoker from Ecuador presented with productive cough for 3 weeks, positive tuberculin skin test, 40 lbs weight loss and right lower lobe collapse. He denied wheezing or hemoptysis. He was treated with antibiotics and ruled out for tuberculosis with negative sputum smear. Bronchoscopy showed an endobronchial lesion at the distal end of bronchus intermedius as cause of the collapse. Endobronchial biopsy of the lesion revealed an endobronchial leiomyoma, a rare cause of endobronchial tumor. The patient underwent bilobectomy as definite therapy for the leiomyoma due to its large size and possible extra-luminal extension, which made it not amenable to bronchoscopic resection or bronchoplasty. Differential diagnoses of endobronchial lesions are discussed along with clinical, radiographic, pathologic characteristics and various treatment modalities for endobronchial leiomyomas.
Keywords: Leiomyoma, Endobronchial tumor
Introduction
Leiomyomas of the respiratory tract can present anywhere along the tracheo-bronchial tree or within the lung parenchyma. If definitive diagnosis can be made with biopsy, then lung-preserving techniques such as endobronchial removal or bronchoplasty can be used.
Case report
A 44 year-old male former heavy smoker was referred to our hospital for an abnormal chest radiograph and cough. He reported productive cough, fevers and night sweats for three weeks. On review of systems he had an unintentional weight loss of 40 lbs over the previous four months. He never had a tuberculin skin test (TST) and denied tuberculosis contacts or wheezing. He was originally from Ecuador and had a history of right lower lobe pneumonia in the previous two years. A TST placed on admission was positive (20 mm). Decreased breath sounds on auscultation and dullness on percussion were appreciated at the right base. Blood tests revealed only mild leukocytosis (13,300 cells/uL) without bandemia. His basic metabolic panel and liver function panel results were unremarkable.
The patient's posteroanterior and lateral chest radiographs are shown in Fig. 1A–B. Chest CT images (axial and coronal views) are shown in Fig. 2A–B. Pulmonary function tests were normal. Flexible bronchoscopy showed a smooth round white polypoid lesion with wide base at the distal end of bronchus intermedius almost completely occluding the lumen (Fig. 3). White thick mucoid substance could be seen exuding from the right middle lobe bronchus. Our patient underwent bilobectomy and a biopsy of the polypoid lesion is shown in Fig. 4A–B. The diagnosis of an endobronchial leiomyoma causing complete obstruction of bronchus intermedius was made.
Fig. 1.
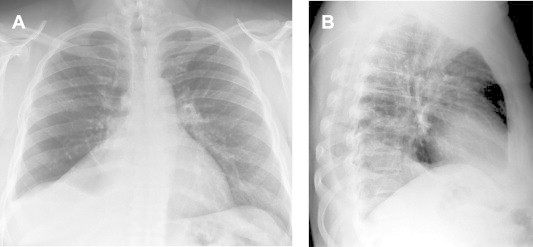
Chest radiograph shows right lower lobe (RLL) collapse, similar to that of 2 years ago A. Posteroanterior view. B. Lateral view.
Fig. 2.
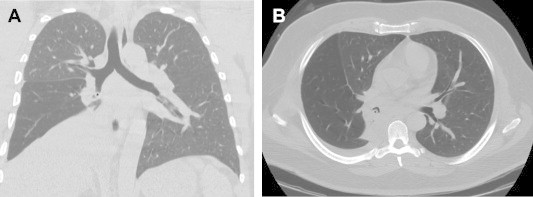
Chest CT scan reveals an endobronchial lesion (asterisk) in the bronchus intermedius with complete atelectasis of right lower lobe and a small pleural effusion. A, Axial window. B, Coronal lung window.
Fig. 3.

Bronchoscopic imaging showing a white, smooth ovoid lesion with nearly complete obstruction of the bronchus intermedius.
Fig. 4.
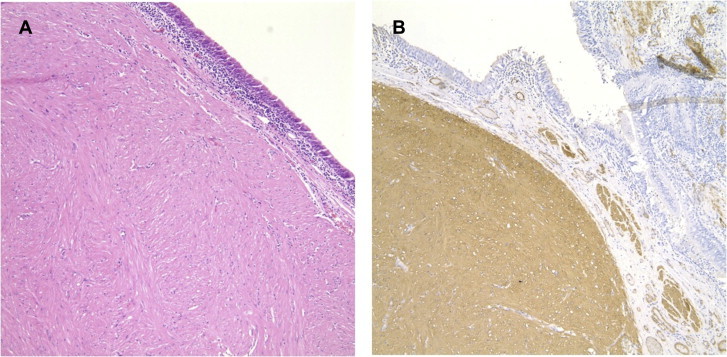
A Bundles of hypertrophied smooth muscle cells in disorganization (hematoxylin-eosin, original magnification ×200). B. Immuno-histochemistry for human alpha-smooth muscle actin monoclonal antibody (original magnification ×100) showing diffuse uptake of the tumor and the adjacent bronchial smooth muscle bundles in the submucosa.
Discussion
Clinical discussion
Endobronchial leiomyomas are extremely rare benign tumors; Forkel reported the first case in 1909 [1]. They account for 33–45% of all pulmonary leiomyomas [2,3], and are usually found in young middle age patients (39.1 years in average) without sex predilection [2,4].
Clinical presentation depends on the location of the tumor, its size and changes in the lung distal to the lesion. Bronchial lesions produce symptoms due to partial or complete obstruction of the affected bronchus, which may include wheezing, orthopnea, hemoptysis, recurrent pneumonia and subsequent bronchiectasis [5]. Kwon described cough, dyspnea and fever as major symptoms in pulmonary leiomyomas in the case series he reported [6]. Our patient had all of those symptoms.
Endobronchial lesions comprise a heterogeneous group of pathologic entities (Table 1). Only 10% are benign tumors, papilloma being the most common form [7]. Our patient presented with recurrent pneumonia, significant weight loss and a positive TST, which lead to the presumptive diagnosis of active tuberculosis. However, sputum smear analysis was negative for acid-fast bacilli (AFB). Since endobronchial tuberculosis (EBTB) is sputum positive for AFB only in 16–53.3% [8], and out patient was originally from a high-endemic area, we decided to start empirical treatment for endobronchial tuberculosis. Interestingly, constitutional symptoms including fever, weight loss, anorexia and night sweat are not usually prominent in EBTB [8]. We discontinued antituberculosis therapy two months later; after both endobronchial biopsy and bronchoalveolar lavage cultures for mycobacteria returned negative.
Table 1.
Differential diagnosis of solitary endobronchial lesions.
| Infections |
| Fungal |
| Endobronchial aspergilloma |
| Endobronchial cryptococcosis |
| Endobronchial histoplamosis |
| Endobronchial actinomycosis |
| Endobronchial nocardiosis |
| Endobronchial tuberculosis |
| Hydatid disease |
| Granulomatous disease |
| Sarcoidosis |
| Amyloidosis |
| Fibroepithelial polyp |
| Broncholith |
| Foreign body |
| Tumors |
| Malignant |
| Adenoid cystic carcinoma (cylindroma) |
| Bronchogenic small cell carcinoma |
| Bronchogenic squamous cell carcinoma |
| Mucoepidermoid carcinoma |
| Bronchial carcinoid |
| Adenocarcinoma |
| Kaposi sarcoma |
| Hodgkin and Non Hodgkin lymphoma |
| Chronic lymphocytic leukemia |
| Primary endobronchial plasmocytoma. |
| Endobronchial melanoma. |
| Metastasis |
| Benign (<10%) |
| Papilloma |
| Lipoma |
| Endobronchial hamartoma |
| Endobronchial inflammatory pseudotumor |
| Endobronchial neurogenic tumor |
| Leiomyoma |
| Pleomorphic adenoma |
| Metastatic bronchial endometriosis |
| Others (hemangioma, fibroma, granular cell and glumous tumor) |
The treatment for endobronchial leiomyoma depends on its location in the airway as well as the size and width of the lesion. Most endobronchial leiomyomas reported in the literature have been resected either by lobectomy or pneumonectomy [9]; however less invasive procedures have been reported as safe alternatives including simple bronchoscopic removal with or without laser [6], bronchoplasty, or bronchotomy [10] utilizing sleeve resection of the involved bronchus while sparing the distal lung resection. Parenchymal resection is appropriate if there is a solitary parenchymal nodule or end-stage infection distal to the obstruction [11]. Bronchoscopic intervention is the modality of choice nowadays if the lesion is not wide based [6]. The prognosis of leiomyoma is excellent after complete resection with rare recurrence with only two cases reported [6,12]. Our patient underwent flexible bronchoscopy, during which limited endobronchial biopsies were obtained due to bleeding. He was referred then to thoracic surgery team for resection. A right lung bilobectomy (middle and lower lobes) was carried out via video assisted thoracoscopic surgery (VATS) due to its large size, wide base and suspected extraluminal extension, which would render it not amenable to bronchoscopic resection or bronchoplasty. The patient had an uneventful post-operative course and was followed up in our outpatient clinic. Post surgical pulmonary function tests were within normal limits.
Radiological discussion
The diagnosis of leiomyoma can not be made by imaging alone since there are no pathognomonic features. Atelectasis is the most frequent finding in chest radiographs for endobronchial leiomyomas [11], but other findings such as normal imaging, solitary round mass, pneumonic infiltration, unilateral emphysema or hyperlucency due to air trapping distal to the obstructed bronchus can be found [2]. Most benign endobronchial tumors produce non-specific masses in the wall of the airways, except for lipoma and cartilaginous tumors, which may show fat and calcium respectively. Hamartomas can also have both features [10]. Four cases of leiomyomas with calcification have been reported [5,10]; feature that was not present in this case.
Computed tomography is an excellent tool of investigating bronchial lesions and for delineating leiomyomas in the bronchial tree. Its sensitivity to detect obstructive lesions in the respiratory tract varies from 60 to 100% [13]. Leiomyomas have an attenuation of 25–46 Hounsfield units on unenhanced CT and 46–85 Hounsfield units on contrast enhanced CT [3]. Tracheal leiomyomatosis (TL) appears similar to other benign tumors on CT; including lipomas and neurogenic tumors. When confined to the endotracheal or endobronchial lumen, TL is described as a homogeneous, smooth or lobulated mass with diffuse enhancement and a well delineated margin [14–16], however “iceberg tumors” (small endo-luminal component and large extra-luminal component) have been reported in 15% of cases, which suggests differential diagnoses of carcinoid and mucoepidermoid carcinomas [3].
Fiberoptic bronchoscopy is the best modality to examine the endo-luminal and mucosal lesions of the respiratory tract. Unfortunately, this mode provides limited information regarding the extent of the extra-luminal involvement of the disease and airway patency distal to the bronchial stenosis [17]. Virtual bronchoscopy and 3-D reconstruction of high resolution CT are both novel, non-invasive complementary modalities to identify endo-luminal lesions in the respiratory tract [13], with the advantage of allowing visualization from multiple angles, thus providing significant implications for surgical resection [10].
Pathologic discussion
In the lung, leiomyomas arise from the smooth muscle of the bronchial wall and grow as solitary polypoid tumors with broad bases involving the bronchi or alveolar wall [5,18]. Endobronchial biopsy of this patient showed a segment of benign appearing irregular smooth muscle in the submucosa. Due to the limited tissue sampling it could not be determined whether the smooth muscle represented a leiomyoma or hypertrophied muscularis propria. The lobar resection specimen, however, revealed a well-defined smooth muscle nodule extending from the bronchial wall into the bronchial lumen with nearly complete obstruction. The tumor was composed of bundles of hypertrophied, disorganized smooth muscle cells with minimal vascular or fibrous component – the latter two components are usually predominant in the pulmonary parenchymal leiomyomas [5]. Immuno-histochemistry was diffusely strongly positive for smooth muscle actin (SMA) and desmin, which helped differentiate it from other spindle tumors [19] such as fibromas, neurofibromas, and Schwannoma; and confirmed the diagnosis of leiomyoma (Fig. 4B). There was no evidence of mitotic activity, necrosis or atypia (Fig. 4A), but if present, leiomyosarcoma should be suspected [19], which also carries an excellent prognosis after complete resection.
Conclusion
In conclusion, bronchial leiomyoma is an unusual cause of bronchial obstruction. Diagnosis can be challenging and fiberoptic bronchoscopy is helpful. The treatment is surgical resection with an excellent prognosis.
Disclaimer and conflict of interest disclosure
This paper has not been submitted elsewhere, is not under review, or published previously.
This work in original and all authors meet the criteria for authorship, including acceptance of responsibility for the scientific content of the manuscript. No conflict of interest is declared; informed consent and permission to use all information was obtained from the patient.
All the authors have read and approved the manuscript being submitted to this journal.
Acknowledgments
We would like to thank Dr Stephan Kamholz, for carefully reviewing the above manuscript and for his most useful suggestions.
References
- 1.Freireich K., Bloomberg A., Langs E.W. Primary bronchogenic leiomyoma. Dis Chest. 1951 Mar;19(3):354–358. doi: 10.1378/chest.19.3.354. [DOI] [PubMed] [Google Scholar]
- 2.Sharifi N., Massoum S.H., Shahri M.K., Rezaei A., Ashari A.A., Attar A.S. Endobronchial leiomyoma; report of a case successfully treated by bronchoscopic resection. J Res Med Sci. 2010 Nov;15(6):364–370. [PMC free article] [PubMed] [Google Scholar]
- 3.Kim Y.K., Kim H., Lee K.S., Han J., Yi C.A., Kim J. Airway leiomyoma: imaging findings and histopathologic comparisons in 13 patients. AJR Am J Roentgenol. 2007;189(2):393–399. doi: 10.2214/AJR.07.2079. [DOI] [PubMed] [Google Scholar]
- 4.Shahian D.M., McEnany M.T. Complete endobronchial excision of leiomyoma of the bronchus. J Thorac Cardiovasc Surg. 1979;77:87–91. [PubMed] [Google Scholar]
- 5.White S.H., Ibrahim N.B., Forrester-Wood C.P., Jeyasingham K. Leiomyomas of the lower respiratory tract. Thorax. 1985 Apr;40(4):306–311. doi: 10.1136/thx.40.4.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kwon Y.S., Kim H., Koh W.J., Suh G.Y., Chung M.P., Kwon O.J. Clinical characteristics and efficacy of bronchoscopic intervention for tracheobronchial leiomyoma. Respirology. 2008 Nov;13(6):908–912. doi: 10.1111/j.1440-1843.2008.01366.x. [DOI] [PubMed] [Google Scholar]
- 7.Kwong J.S., Müller N.L., Miller R.R. Diseases of the trachea and main-stem bronchi: correlation of CT with pathologic findings. Radiographics. 1992 Jul;12(4):645–657. doi: 10.1148/radiographics.12.4.1636031. [DOI] [PubMed] [Google Scholar]
- 8.Kashyap S., Mohapatra P.R., Saini V. Endobronchial tuberculosis. Indian J Chest Dis Allied Sci. 2003 Oct–Dec;45(4):247–256. [PubMed] [Google Scholar]
- 9.Yamada H., Katoh O., Yamaguchi T., Natsuaki M., Itoh T. Intrabronchial leiomyoma treated by localized resection via bronchotomy and bronchoplasty. Chest. 1987 Feb;91(2):283–285. doi: 10.1378/chest.91.2.283. [DOI] [PubMed] [Google Scholar]
- 10.Ko S.M., Han S.B., Lee S.K., Woo S.K., Kim M.J., Keum D.Y. Calcified endobronchial leiomyoma. Br J Radiol. 2007 May;80(953):e91–e93. doi: 10.1259/bjr/25631438. [DOI] [PubMed] [Google Scholar]
- 11.Ayabe H., Tsuji H., Tagawa Y., Tomita M., Tsuda N., Chen J. Endobronchial leiomyoma: report of a case treated by bronchoplasty and a review of the literature. Surg Today. 1995;25(12):1057–1060. doi: 10.1007/BF00311694. [DOI] [PubMed] [Google Scholar]
- 12.Harris P.F., Maness G.M., Ward P.H. Leiomyoma of the larynx and trachea: case reports. South Med J. 1967;60:1223–1227. doi: 10.1097/00007611-196711000-00018. [DOI] [PubMed] [Google Scholar]
- 13.Finkelstein S.E., Schrump D.S., Nguyen D.M., Hewitt S.M., Kunst T.F., Summers R.M. Comparative evaluation of super high-resolution CT scan and virtual bronchoscopy for the detection of tracheobronchial malignancies. Chest. 2003 Nov;124(5):1834–1840. doi: 10.1378/chest.124.5.1834. [DOI] [PubMed] [Google Scholar]
- 14.McCarthy M.J., Rosado-de-Christenson M.L. Tumors of the trachea. J Thorac Imaging. 1995;10:180–198. doi: 10.1097/00005382-199522000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Rodriguez E., Pombo F., Aguilera C., Capdevila A. Recurring tracheal leiomyoma presenting as a calcified mediastinal mass. Eur J Radiol. 1996;22:82–84. doi: 10.1016/0720-048x(95)00718-6. [DOI] [PubMed] [Google Scholar]
- 16.Douzinas M., Sheppard M.N., Lennox S.C. Leiomyoma of the trachea – an unusual tumour. Thorac Cardiovasc Surg. 1989;37:285–287. doi: 10.1055/s-2007-1020334. [DOI] [PubMed] [Google Scholar]
- 17.Aquino S.L., Vining D.J. Virtual bronchoscopy. Clin Chest Med. 1999;20:725–730. doi: 10.1016/s0272-5231(05)70251-3. [DOI] [PubMed] [Google Scholar]
- 18.Metta H., Corti M., Redini L., Dure R., Campitelli A.M., Narbaitz M. Endobronchial leiomyoma: an unusual non-defining neoplasm in a patient with AIDS. Rev Inst Med Trop Sao Paulo. 2009 Jan-Feb;51(1):53–55. doi: 10.1590/s0036-46652009000100010. [DOI] [PubMed] [Google Scholar]
- 19.Wilson R.W., Kirejczyk W. Pathological and radiological correlation of endobronchial neoplasms. Part I. Benign tumors. Ann Diagn Pathol. 1997;1:31–46. doi: 10.1016/s1092-9134(97)80007-x. [DOI] [PubMed] [Google Scholar]


