Abstract
During a diagnostic flexible bronchoscopy an 84 year old patient suffered a sudden reduction in conscious level following a transbronchial lung biopsy. A subsequent computed tomography brain scan confirmed cerebral air emboli. The patient survived following a period of supportive treatment in the critical care unit.
Transbronchial lung biopsy may cause disruption of vessels walls within the lung parenchyma. Increased airway pressure, caused by the patient exhaling against a bronchoscope wedged within a segmental bronchi, may subsequently force air bubbles through the vessel wall defects. This may explain the occurrence of air emboli. This is a rare report of air embolism complicating transbronchial lung biopsy and all bronchoscopists should aware of this potentially fatal complication.
Keywords: Air embolism, Bronchoscopy, Transbronchial lung biopsy
Introduction
Diagnostic flexible bronchoscopy under conscious sedation is a safe technique with minimal morbidity and mortality. The largest study examining the safety of flexible bronchoscopy (20,986 patients) reported a major complication rate of 1.1% and a mortality rate of 0.02% [1]. Air embolism is not recorded as a potential complication within UK national bronchoscopy guidelines [2], however there have been rare cases of air embolism following transbronchial lung biopsy (TBLB) dating back to 1979 [3–7] (Table 1).
Table 1.
Previous case reports of cerebral air embolism following flexible bronchoscopy and transbronchial lung biopsy.
| Date published | Author | Age of patient | Underlying diagnosis | Procedure | Outcome |
|---|---|---|---|---|---|
| 1979 | Erikson et al. | 48 | Miliary TB | TBLB | Died |
| 1987 | Strange et al. | 89 | Amyloidosis | TBLB | Died |
| 2001 | Shetty et al. | 60 | ILD | TBLB | Died |
| 2004 | Dhillon et al. | 55 | Lung cancer | TBLB | Survived |
| 2010 | Azzola et al. | 60 | Lung cancer | TBLB, TBNA | Died |
| 2010 | Azzola et al. | 68 | Lung cancer | TBLB | Died |
Case report
An 84 year old lady was referred to the rapid access chest clinic for investigation of weight loss and an abnormal chest X-ray (CXR). An apical segment right upper lobe mass with a communicating segmental bronchus was confirmed on thoracic CT (Figure 1). Flexible bronchoscopy was performed under conscious sedation with incremental doses of midazolam (total 2 mg) and alfentanyl (total 250 mcg). As expected, no endobronchial abnormality was detected. TBLB was performed from the apical segment of the right upper lobe, with the bronchoscope positioned in the segmental bronchus. Following the second biopsy, the patient became unresponsive (Glasgow Coma Scale (GCS) = 3) with signs of upper airways obstruction requiring airway management and administration of high flow oxygen. Sedation was reversed with naloxone and flumazenil with no change in neurological status. A CXR confirmed the absence of a pneumothorax and a 12-lead electrocardiogram showed no acute changes. Haemodynamic stability was maintained throughout. The patient was transferred to the critical care unit where intravenous anticonvulsants were required to control multiple seizures. Improvement in GCS occurred over the next 48 h although a residual right hemiparesis (power 3/5) was evident. A CT brain scan, performed two hours following the deterioration, demonstrated small, rounded and black lucencies at the grey–white interface, confirming the diagnosis of cerebral air embolism (Figure 2). The patient was discharged 10 days later to a community rehabilitation unit.
Fig. 1.

Computed tomography thorax (coronal reconstruction) demonstrating a suspected tumour within the right upper lobe and a communicating apical segmental bronchus.
Fig. 2.
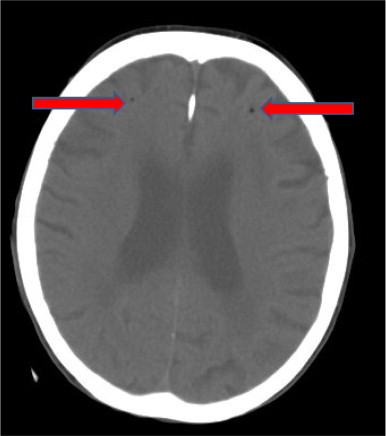
Computed tomography brain demonstrating cerebral air emboli.
Discussion
There are two requirements for air embolism formation [8]: a portal of entry such as a defect in a vessel wall and a pressure gradient which forces the air bubbles through the defect. In the case of TBLB it is postulated that the “portal of entry” is a vessel wall defect created by the biopsy and that the abnormal surrounding lung tissue, caused by the underlying disease process, prevents the normally protective vasoconstriction that serves to occlude these defects [3,4]. The “pressure gradient” may be created by the patient exhaling with the bronchoscope wedged in a bronchus (Zavala method of TBLB [9]) causing the airway pressure to rise distal to the scope [3,4,8]. Wedging of the bronchoscope is described in 4 out of the 6 cases in Table 1. This pressure gradient could also be exacerbated by air trapping in COPD, coughing and performing the biopsies in dependent lung segments (4 out of 6 cases involved biopsies from the basal segments of the right lower lobe).
Air embolism can be asymptomatic, cause mild transient symptoms or life-threatening illness. Cardiac air emboli can lead to bradycardia, tachyarrhythmia, hypotension and cardiac arrest. Cerebral air emboli can lead to reduction in conscious level, focal neurological deficits and seizures.
The diagnosis of air emboli is based on classical symptoms that occur after a potential precipitating event. Demonstration of intra-vascular bubbles can be difficult and should not be relied upon. In cerebral air emboli, air bubbles <1.3 cm in diameter will not be detected on CT and in 1 cm slice CT brain scans it is easy to miss bubbles [10]. The management of air embolism consists of the trendelenberg position, supportive measures, avoidance of positive pressure ventilation (this may increase the pressure gradient thereby increasing the volume of embolised air) and hyperbaric oxygen. Hyperbaric oxygen reduces air bubble volume and diameter. This increases the surface to volume ratio allowing quicker absorption of nitrogen from within the bubble leading to more rapid restoration of distal blood flow. The air bubbles may exist in the circulation for up to 40 h and hyperbaric oxygen could be considered at any point within this time frame [11].
Air embolism is a very rare and often fatal complication of TBLB. All bronchoscopists should be aware of this potential complication and consider it part of the differential diagnosis in any patient with acute deterioration during or immediately after transbronchial biopsy.
References
- 1.Facciolongo N., Patelli M., Gasparini S. Incidence of complications in bronchoscopy: multi-centre prospective study of 20,986 bronchoscopies. Monaldi Arch Chest Dis. 2009;71:8–14. doi: 10.4081/monaldi.2009.370. [DOI] [PubMed] [Google Scholar]
- 2.Du Rand I.A., Blaikley J., Booton R. BTS guideline for diagnostic flexible bronchoscopy in adults. Thorax. 2013;68:i1–i44. doi: 10.1136/thoraxjnl-2013-203618. [DOI] [PubMed] [Google Scholar]
- 3.Eickson A.D., Irwin R.S., Teplitz C., Corrao W.M., Tarpey J.T. Cerebral air embolism complicating transbronchoscopic lung biopsy. Ann Intern Med. 1979;90:937–938. doi: 10.7326/0003-4819-90-6-937. [DOI] [PubMed] [Google Scholar]
- 4.Strange C., Heffner J.E., Collins B.S., Brown F.M., Sahn S.A. Pulmonary haemorrhage and air embolism complicating transbronchial biopsy in pulmonary amyloidosis. Chest. 1987;92:367–369. doi: 10.1378/chest.92.2.367. [DOI] [PubMed] [Google Scholar]
- 5.Shetty P.G., Fatterpekar G.M., Manohar S. Fatal cerebral air embolism as a complication of transbronchoscopic lung biopsy: a case report. Australas Radiol. 2001;45:215–217. doi: 10.1046/j.1440-1673.2001.00905.x. [DOI] [PubMed] [Google Scholar]
- 6.Dhillon S.S., Agrawal A., Gorin A.B. Cerebral arterial air embolism after transbronchial lung biopsy. J Bronchol. 2004;11:125–127. [Google Scholar]
- 7.Azzola A., Von Garnier C., Chhajed P.N., Schrip U., Tamm M. Fatal cerebral air embolism following uneventful flexible bronchoscopy. Respiration. 2010;80:569–572. doi: 10.1159/000321849. [DOI] [PubMed] [Google Scholar]
- 8.Wherrett C.G., Mehran R.J., Beaulieu M.A. Cerebral arterial gas embolism following diagnostic bronchoscopy: delayed treatment with hyperbaric oxygen. Can J Anesth. 2002;49:96–99. doi: 10.1007/BF03020427. [DOI] [PubMed] [Google Scholar]
- 9.Zavala D.C. Pulmonary hemorrhage in fibreoptic transbronchial biopsy. Chest. 1976;70:584–588. doi: 10.1378/chest.70.5.584. [DOI] [PubMed] [Google Scholar]
- 10.Dexter F., Hindman B.J. Recommendations for hyper baric oxygen therapy of cerebral air embolism based on a mathematical model of bubble absorption. Anesth Analg. 1997;84:1203–1207. doi: 10.1097/00000539-199706000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Laydon A.J. Hyperbaric oxygen treatment for cerebral air embolism – where are the data? (Editorial) Mayo Clin Proc. 1991;66:641–646. doi: 10.1016/s0025-6196(12)60525-4. [DOI] [PubMed] [Google Scholar]


