Abstract
Background:
Periodontal diseases are ubiquitous, affecting all dentate animals. Regular methods for controlling it have been found to be ineffective, which have paved the way for the use of herbal products as an adjunctive to mechanical therapy as they are free to untoward effects and hence can be used for a long period of time. Ocimum sanctum is a plant which has the greater medicinal value and enormous properties for curing and preventing disease.
Objective:
In the present study we assessed the effectiveness of Ocimum sanctum on dental plaque, gingival inflammation and comparison with gold standard chlorhexidine and normal saline (placebo).
Materials and Methods:
A triple blind randomized control trial was conducted among volunteered medical students. They were randomly allocated into three study groups: (1) Ocimum sanctum mouthwash (n = 36); (2) Chlorhexidine (active control) (n = 36); (3) normal saline (negative control) (n = 36). Assessment was carried out according to plaque score and gingival score. Statistical analysis was carried out later to compare the effect of both mouthwash. ANOVA (Analysis of variance) and post-hoc LSD tests were performed using software package used for statistical analysis (SPSS) version 17. P ≤0.05 was considered as statistically significant.
Results:
Our result showed that Ocimum sanctum mouthrinse is equally effective in reducing plaque and gingivitis as Chlorhexidine. The results demonstrated a significant reduction in gingival bleeding and plaque indices in both groups over a period of 15 and 30 days as compared to control group.
Conclusion:
The results of the present study indicate that Ocimum sanctum mouthrinse may prove to be an effective mouthwash owing to its ability in decreasing periodontal indices by reducing plaque accumulation, gingival inflammation and bleeding. It has no side effect as compared to chlorhexidine.
Keywords: Chlorhexidine, gingival index, Ocimum sanctum, plaque index
INTRODUCTION
Dental diseases are recognized as major public health problems throughout the world. Numerous epidemiological studies have shown that diseases such as tooth decay and diseases of the periodontium are among the most common afflictions of mankind. The medicinal plants are widely used by the medicinal practitioners for curing various diseases in their day to day practice. Modern-day medicines may contain extracts of herbs, or synthetic chemicals based on herbs, but what the natural form offers are less side effects and a cheaper alternative to pharmaceutical drugs. Ocimum sanctum is one such natural substance, which has gone unnoticed in spite of its potential uses in curing a large array of diseases. Common oral diseases such as caries and periodontal diseases are still global problems and are documented as contributing greatly to oral health problems. This is particularly the case in under-privileged populations in both developing and developed countries.[1] Dental plaque has been considered the main etiologic agent in the initiation of gingivitis and its progression to periodontitis.[2] To this day, mechanical methods of dental plaque removal are widely regarded as being a highly effective means of helping to control progression of dental caries and periodontal diseases which rank among the most common diseases in humans.[3] Mouthrinses are generally considered as adjuncts to oral hygiene and widely used in the delivery of active agents to the teeth and gums. Such products could influence plaque accumulation by preventing bacterial attachment and removing bacterial biofilm. Control of the bacterial biofilm on teeth is essential to the maintenance of oral health, and can be achieved by proper oral hygiene, use of fluoride products, and regular check-ups with a dentist.[4] An additional approach is the application of chemical agents with antimicrobial activities on dental surfaces to promote a reduction in biofilm formation. Such agents have been frequently prescribed as adjuvant in the prevention or treatment of oral diseases because they can inhibit bacterial colonization, growth, and metabolism, and consequently interrupt the formation of mature biofilm, changing it at biochemical and ecological levels.[4,5,6] Several compounds have been evaluated for their effectiveness on supragingival plaque and gingivitis including bisbiguanides such as chlorhexidine gluconate,[7] essential oils,[8] phenolic compounds, pyrimidines, quaternary ammonium compounds, oxygenating agents, halogens etc., and among these agents, chlorhexidine is, thus far, the most studied and effective antiseptic for plaque inhibition and prevention of gingivitis when used twice daily as mouth rinse.[9] Many of the currently available mouth rinses such as chlorhexidine mouthwash do have drawbacks, such as alteration in taste sensation, staining of teeth and so on.[10,11] Additionally, data from several studies have shown that its role in caries prevention is inconclusive.[12] In order to overcome such side effects the World Health Organization (WHO) advised researchers to investigate the possible use of natural products such as herb and plant extracts.
Medicinal plants are part and parcel of human society to combat diseases from the dawn of civilization. Ocimum sanctum (Ocimum sanctum) is known as the “Queen of herbs”. It is described as sacred and medicinal plant in ancient literature and is frequently mentioned as one of the main pillars of herbal medicine. Renowned as a general tonic and vitalizer, “The Elixir of Life”, Ocimum sanctum has been traditionally employed in hundreds of different formulations for the treatment of a wide range of disorders, including those of the mouth and throat, lungs, heart, blood, liver, kidney, and the digestive, metabolic, reproductive and nervous systems.
Literature review reveals that no studies have been conducted to assess the antiplaque, and antigingivitis effect of Ocimum sanctum.[13] As studies related to herbal mouth rinses are lacking and as clinicians, we are entangled in poignant situation when patient asks about such herbal mouth rinses, research in this area is necessary to generate the evidence. This study was hence planned with the objective to evaluate clinically the efficacy of Ocimum sanctum in preventing plaque accumulation and gingival inflammation. We also wished to compare it with commercially available mouthwash chlorhexidine and normal saline, which was used as placebo.
This placebo-controlled, triple blind randomized control trial (patients, examiner, statistician were blinded to the allocation of mouthwash in respective groups); three group parallel study was conducted in the department of public health dentistry on volunteered medical students of Teerthanker Mahaveer Medical College and Research Centre. Protocol was approved by the Institutional Review Board (IRB) of Teerthanker Mahaveer University. All subjects signed an IRB approved consent form. Pilot study was done on 5 patients in each group to check the feasibility of the study; results are not included in the present study. The study was carried out according to the guidelines of the Declaration of Helsinki (revised version of 1975 and its amendments of 1983, 1989, and 1996) and I.C.M.R guidelines for biomedical research involving human subjects. In our study we strictly adhered to the guidelines of the Declaration of Helsinki, and I.C.M.R study protocol was approved by an independent committee - the Institutional reviewer board (IRB). Consent was taken from the subjects before the start of the study and all the subjects signed an IRB approved consent form. Ocimum sanctum (test mouthwash) was compared to chlorhexidine (the best current therapy) and placebo.
Materials used for the clinical trial were mouth mirror, explorer, disclosing solution, periodontal probe, tweezers, chlorhexidine solution and self-prepared Ocimum sanctum mouthwash.
Inclusion and exclusion criteria
The students with no history of any dental treatment, antibiotic or anti-inflammatory drug therapy for the past 3 months were included in the study. Students with any history of systemic diseases/conditions, fibrotic gingival enlargement and smoking were excluded from the study. Participants with good general health, a baseline plaque score greater than 1.5 and a baseline decayed, missing and filled teeth (DMFT) index of 3 to 5 were included in the study. DMFT index provide a method for measuring, scoring and analyzing dental conditions in individuals and groups. It describes the status of individuals or groups with respect to the condition being measured. Those volunteers who had used antibiotics or mouthwash for 5 consecutive days or corticosteroids in the past 30 days were excluded from the study. Those subjects who had a history of sensitivity to any mouthwash or used removable prostheses or an orthodontic appliance were excluded from the study. Also, those who had undergone professional measures to remove plaque and calculus in the past 15 days, and did not give consent for clinical trial were excluded.
Preparation of extract
Ocimum sanctum leaves were obtained from courtyards and were washed and dried under controlled conditions. The dried leaves were then powdered finely. Three hundred grams of finely powdered Ocimum sanctum was then macerated with 100% ethanol for a week in a round bottom flask.
The flask was kept in dark to avoid effect of light on the active ingredients. The extract was then filtered through a muslin cloth for coarse residue and finally through Whatman No. 1 filter paper. The filtrate so obtained was reduced at a low temperature < 50°C to obtain a solid residue of Ocimum sanctum extract. From 300 g of Ocimum sanctum powder dissolved in 1 L of ethanol, 18 g of residue (extract) was obtained and thus the yield was 6% w/w. The extract was suspended in polyethylene glycol 400 (20% v/v) and sterile distilled water to give a final concentration of 4% (w/v). As flavoring agent 0.005% spearmint oil was added.
Sample size and randomization
All the undergraduate medical students of Teerthanker Mahaveer Medical College and Research centre were subjected to clinical examination, and a sampling frame (n = 285) was prepared of those who fulfilled the inclusion and exclusion criteria. A sample size of 108 was arrived at by using NMaster Statistical Software. A total of 108 volunteers were randomly allocated into the three study groups through computer-generated random numbers. Random allocation of mouth rinses using the lottery method was done. Individuals were identified by code numbers throughout the study.
The study was designed within the guidelines required by the American Dental Association Council on Scientific Affairs for evaluating the clinical efficacy of chemotherapeutic mouthrinses (American Dental Association Council on Scientific Affairs, 1997). None of the eligible students refused to participate in the study.
Group 1 (n = 36) was given 4% Ocimum sanctum mouthwash and instructed to use 10 mL twice a day for 30 days.
Group 2 (n = 36) was given 0.12% Chlorhexidine and instructed to use 10 mL twice a day for 30 days.
Group 3 (n = 36) was the placebo control group and saline water was given as the mouthwash.
All the three solutions were made of same color with the help of department of pharmacy and kept in coded containers and decoded later. Students were instructed to rinse their mouth with 10 mL of mouthwash twice daily once post breakfast and other post lunch for 30 days for 60 s and not to rinse with water thereafter. Data were collected three times in 30 days for assessing plaque and gingivitis. Clinical measurements for plaque and gingivitis were taken at baseline (prior to the study), at 15 days and at the end of the study (4 weeks) and were recorded on chart. Study subjects, the investigators, assistants, data analyzer involved in the trial were masked with respect to the treatment allocated. During the thirty days of the trial, the subjects continued to exercise their regular non-supervised, self-performed plaque control measures. No oral prophylaxis was done before the start of the study.
A single examiner, who was trained and calibrated to record the plaque and gingival scores, recorded the findings at all three intervals. The examiner was blinded to the allocation of mouthwash in the intervention arms. Since the plaque and gingival indices are reversible, intra-examiner reliability was assessed within an interval of 60 min. Using kappa statistics, intra-examiner reliability was 0.80 for the gingival index and 0.84 for the plaque index.
All parameters including gender, smoking status, level of education, monthly family income, number of teeth present, plaque index, gingival index and gingival bleeding index were not significantly different between the groups at baseline (all P > 0.1).
Plaque and gingivitis analysis
Scoring of supragingival plaque was done by Turesky modification of the Quigley–Hein plaque index.[14] Scoring of gingival inflammation (gingivitis) were done by Gingival Index of Loe and Silness.[15]
Statistical analysis
The data were analyzed using SPSS version 17. ANOVA followed by post-hoc least significant difference (LSD) were used for analysis. P value of 0.05 was taken to be significant.
RESULTS
Attrition of the sample
There was no attrition of sample in all the three groups as all the study groups completed the study.
Plaque and gingivitis score
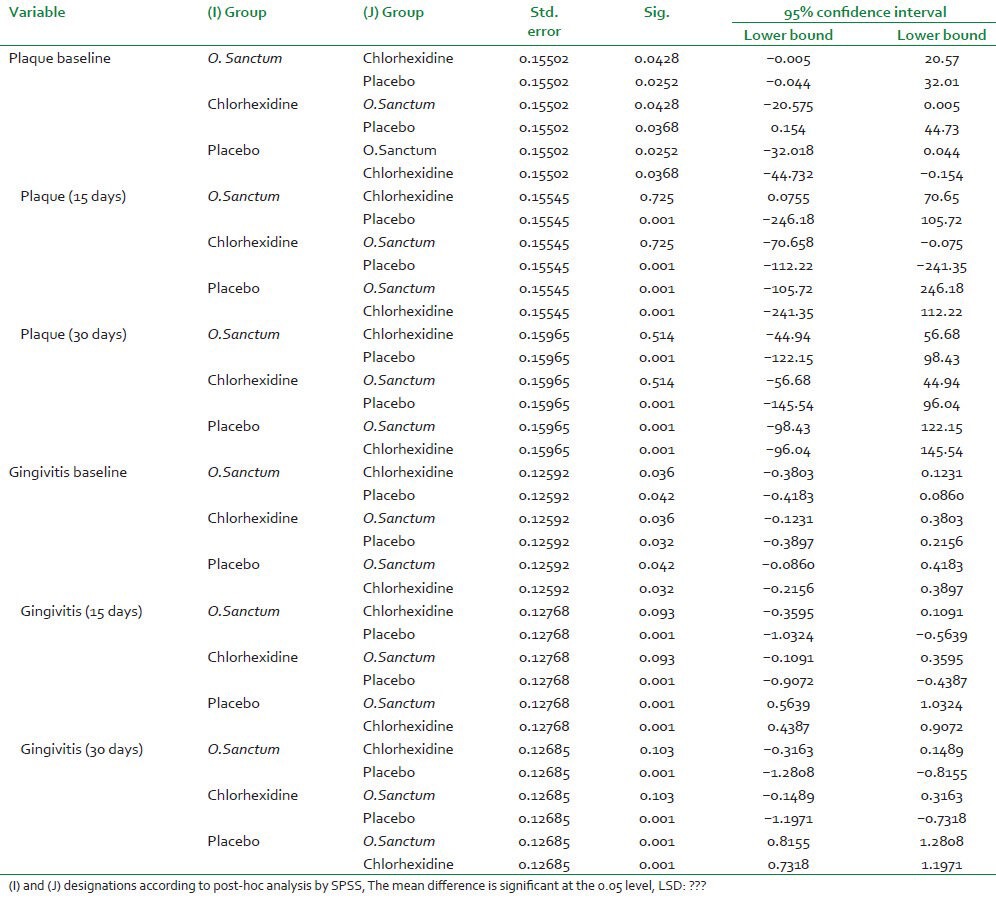
Table 1 represents descriptive baseline statistics. No statistical difference was observed for baseline variables [Table 1]. The mean plaque and gingival scores for the Group I, II, III are depicted in Table 2. ANOVA was used to analyze the reduction in plaque and gingivitis in the three groups. ANOVA [Tables 3 and 4] was carried out to assess the intra-group and inter-group variations for plaque and gingivitis, respectively. There was difference in the baseline value in plaque and gingivitis as no subject was given oral prophylaxis before the start of study. There was a significant decrease in the plaque and gingivitis in both the Ocimum sanctum and chlorhexidine groups at 15 days and 30 days (P < 0.05) [Table 3]. There was progressive decrease in the plaque and gingivitis score at 5% level of significance in Ocimum sanctum and chlorhexidine groups. Chlorhexidine group showed maximum decease as compared to Ocimum sanctum group but difference was not statistically significant. Multiple comparisons were obtained by post-hoc LSD. The difference in the decrease in plaque (P = 0.725 at 15 days and P = 0.514 at 30 days) and gingivitis (P = 0.093 for 15 days and P = 0.103 for 30 days) between Ocimum sanctum and chlorhexidine groups was not statistically significant. However, the difference between Ocimum sanctum and the placebo group and chlorhexidine and the placebo group was significant (P < 0.05). Data show that there was no significant difference between Ocimum sanctum based mouth rinse and chlorhexidine for any clinical parameters throughout the study.
Table 1.
Baseline background of the students using different mouthwash
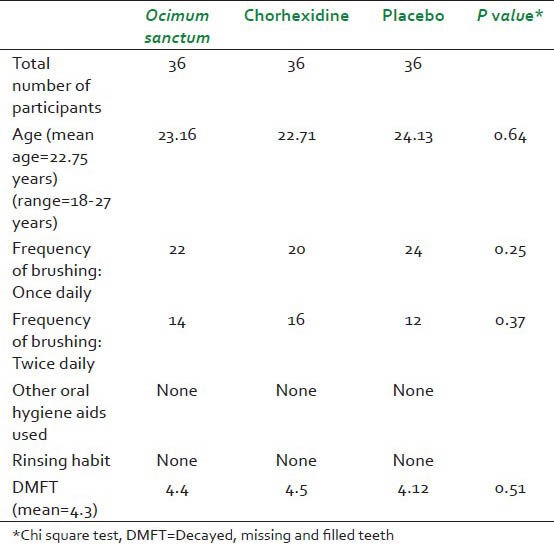
Table 2.
Plaque and gingivitis score at baseline, after 15 days and after 30 days
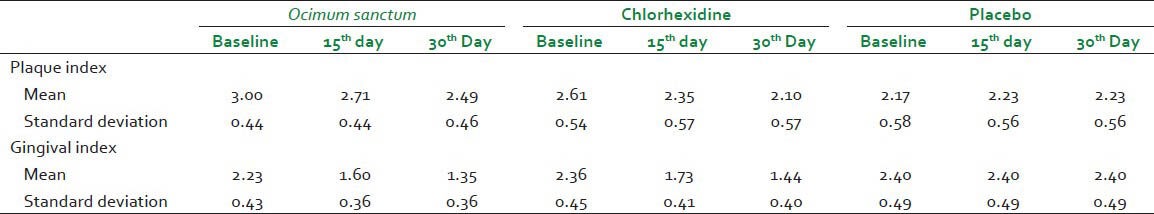
Table 3.
ANOVA of the three study groups
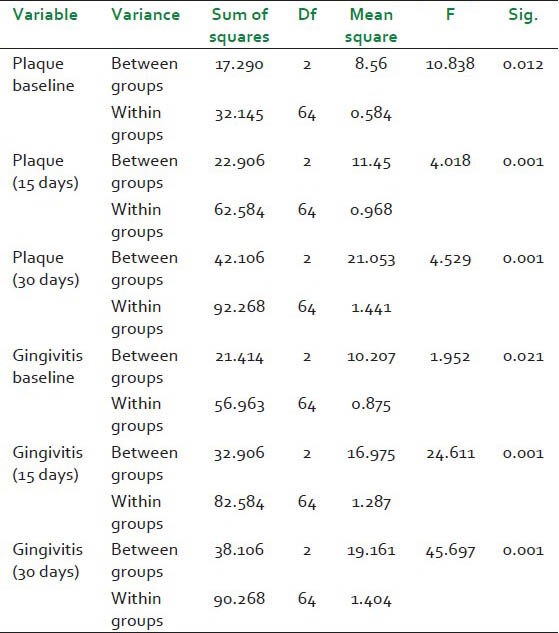
Table 4.
-Post -hoc LSD test for multiple comparison
DISCUSSION
This study was conducted on volunteer students in the Department of Public health Dentistry, Teerthanker Mahaveer Dental College and Research Centre, Moradabad, India over a period of 30 days. The study was carried out according to the guidelines of the Declaration of Helsinki and I.C.M.R for biomedical research involving human subjects.
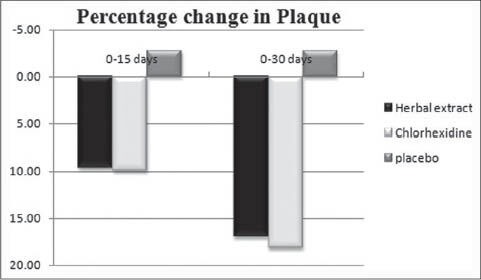
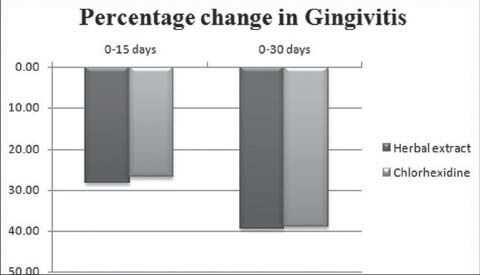
Our data show that a mouthrinse based on the Ocimum sanctum is equally effective in reducing periodontal indices as chlorhexidine. The results demonstrated a significant reduction of gingival and plaque indexes in both groups I and II over a period of four weeks [Graph 1 and 2]. Placebo group showed a slight increase in the plaque index score but was not statistically significant [Graph 3]. There was a significant percentage change in the plaque and gingivitis over a period of four weeks in patients on Ocimum sanctum and chlorhexidine [Graph 3 and 4]. Chlorhexidine has been utilized for several decades and it is still considered one of the most effective anti-plaque agents in dentistry. However, long-term use of chlorhexidine is limited by altering taste and staining of teeth; therefore new formulations with similar or superior efficacy and possibly fewer long-term effects need to be investigated.
Graph 1.
Plaque index
Graph 2.
Gngival index
Graph 3.
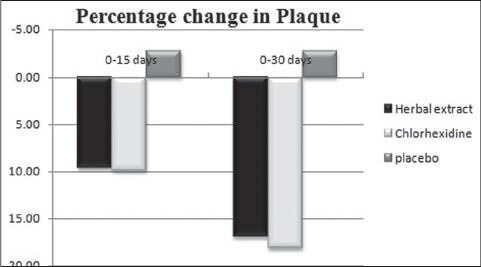
Percentage change in Plaque index over a period of 30 days
Graph 4.
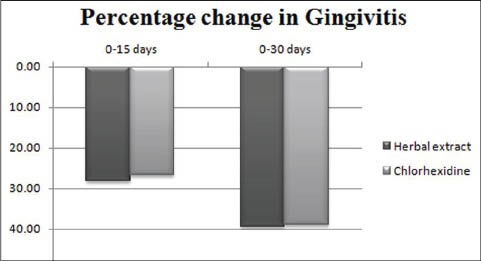
Percentage change in Gingival index over a period of 30 days
One of the candidates is the leaves of the Indian herb Ocimum sanctum. This plant has been used in India and other parts of Asia for thousands of years for medical purposes. In traditional literature, preparations of the leaves of Ocimum sanctum are claimed to be effective in a wide spectrum of inflammatory and infectious diseases. Key historical documents include the Rigveda (“Book of Eternal Knowledge”), thought to have been developed around 5000 BC, the Charaka and Sushruta Samhita medical texts, circa 2700 to 600 BC and Nighantu Adarsha, revised in 800 AD. In such Ayurvedic scriptures, Ocimum sanctum is frequently mentioned as one of the main pillars of herbal medicine. The sacred plant is described as a protector of life, preventing misery and disease from birth through old age and death — and even then aiding the passage to the heavens. Ocimum sanctum is an important symbol in many Hindu religious traditions, which link the plant with Goddess figure. The name ‘Tulsi’ in Sanskrit means ‘the incomparable one’. The presence of a Tulsi plant symbolizes the religious bend of a Hindu family. It is cultivated for religious and medicinal purposes and for its essential oil.[16,17,18]
Ocimum sanctum has been tested against a variety of microorganisms like Candida albicans, Staphyloccus aureus, enteric pathogens, Klebsiella, Escherichia coli and Proteus.[18] It has also demonstrated anti-gonorrheal efficacy against multiresistant strains of Neisseria gonorrhea and clinical isolates of beta lactamase-producing methicillin-resistant Staphylococcus aureus.[18,19]
In the present study, the Ocimum sanctum extract mouthwash avoided plaque formation during the trial, possible explanation for this effect is the antibacterial agents present in Ocimum sanctum i.e. Eugenol (l-hydroxy-2-methoxy-4-allylbenzene) Ursolic acid (2,3,4,5,6,6a, 7,8,8a, 10,11,12,13 14-btetradecahydro-1H-picene-4a-carboxylic acid) and Carvacrol (5-isopropyl-2-methylphenol), Linalool (3,7-dimethylocta-1,6-dien-3-ol), Limatrol, Caryophyllene (4,11,11-trimethyl-8-methylene-bicyclo [7.2.0]undec-4-ene), Methyl carvicol (also called Estragol: 1- allyl-4-methoxybenzene). In addition, the stem and leaves of Ocimum sanctum contain a variety of constituents that may have anti-bacterial activity, including saponins, flavonoids, triterpenoids and tannins that forms high molecular weight complexes with soluble proteins in saliva, increases bacterial lysis on the tooth surface and saliva, and moreover interfere with bacterial adherence mechanisms on tooth surfaces.[16,19]
This study showed a significant anti-gingivitis and anti-inflammatory effect of Ocimum sanctum extract mouthwash, which can be attributed to compounds isolated from Ocimum sanctum extract. Civsilineol, Civsimavatine, Isothymonin, Apigenin, Rosavinic acid and Eugenol were observed for their anti-inflammatory activity or cyclooxygenase inhibitory activity.[20,21] Singh,[22] Singh and Majumdar[23] in their study reported that linoleic acid present in different amount in the fixed oil of different species of O. sanctum L. has the capacity to block both the cyclooxygenase and lipoxygenase pathways of arachidonate metabolism and could be responsible for the anti-inflammatory activity.
Ocimum sanctum has also demonstrated a good efficacy as an anti-caries agent.[24,25] However, a triple blind study on a mouthrinse solution demonstrating the valuable property of Ocimum sanctum in preventing plaque accumulation and gingival inflammation has never been published. The present study fills this gap and supports the earlier data on the efficacy of Ocimum sanctum formulations delivering the natural bioactive components locally in the oral cavity.[26]
In order to eliminate the bias of decreased flow of the saliva overnight, treatment doses were applied after the breakfast and lunch. The participants were allowed to continue with their routine oral hygiene practices. Similar study design was followed in a clinical trial where the subjects continued to exercise their regular non-supervised, self-performed plaque control measures.[3] Carlos Alfredo Franco Neto et al.,[27] stated that there is no difference in the efficacy of chlorhexidine between 0.12 to 0.2% and the former concentration leads to less staining of teeth. Hence, in this study 0.12% concentration was used since the study duration was 4 weeks. Mohammad Hassan Najafi et al.[28] also reported that 0.2% concentration does not seem to be more effective in controlling dental plaque and gingivitis than. 12%. P. Agarwal et al.[24] analyzed the effect of various concentrations of the Ocimum sanctum extract ranging from 0.5 to 10%, and it was observed that a 4% concentration of the extract was optimum as an antibacterial agent against bacterial flora of the oral cavity; thus, in the present study, a concentration of 4% was used. The results of Ocimum sanctum extract mouth rinse on plaque and gingivitis could not be compared with other studies as exploration of the available literature revealed that no studies have been reported in literature which has tried to assess the same effect. However, studies have been conducted which have assessed the effect of Chlorhexidine on plaque and gingivitis and have found a significant reduction.[29] This is the first study to demonstrate the anti-plaque and anti-gingivitis action of Ocimum sanctum. However studies have been reported which suggest that Ocimum sanctum possess other remarkable properties for general and oral health.
CONCLUSION
Ocimum sanctum has stood the test by demonstrating similar effect on plaque and gingivitis when compared with the benchmark control Chlorhexidine and is having no side effects of the latter. In the placebo group where saline water was administered, the slight increase in plaque was found. Ocimum sanctum mouthwash is much more cost effective than chlorhexidine and is easily available. Being an Ayurvedic product, it has no known side effects[25] compared to chlorhexidine and hence is safe for use over a long period of time. This is an encouraging result which clearly favors promotion of Ocimum sanctum as a mouth rinse among rural communities especially belonging to low socioeconomic strata as Ocimum sanctum is easily accessible and is cheap and safe alternative to chlorhexidine. However as this is the first attempt to assess the effect of Ocimum sanctum on plaque and gingivitis, clinical trial of longer duration with a larger sample size should play a vital role in commercialization of Ocimum sanctum mouthwash.
ACKNOWLEDGEMENT
The first author (DG) is grateful to his mentor Dr. D. J Bhaskar and Dr. Mary Suvarna for their constant support and guidance throughout the study. Authors also thank all the participants for their cooperation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Hugoson A, Norderyd O. Has the prevalence of periodontitis changed during the last 30 years? J Clin Periodontol. 2008;35:338–45. doi: 10.1111/j.1600-051X.2008.01279.x. [DOI] [PubMed] [Google Scholar]
- 2.Löe H, Theilade E, Jensen SB. Experimental gingivitis in man. J Periodontol. 1965;36:177–87. doi: 10.1902/jop.1965.36.3.177. [DOI] [PubMed] [Google Scholar]
- 3.Axelsson P, Lindhe J. Effect of controlled oral hygiene procedures on caries and periodontal disease in adults. Results after 6 years. J Clin Periodontol. 1981;8:239–48. doi: 10.1111/j.1600-051x.1981.tb02035.x. [DOI] [PubMed] [Google Scholar]
- 4.Selwitz RH, Ismail AI, Pitts NB. Dental caries. Lancet. 2007;369:51–9. doi: 10.1016/S0140-6736(07)60031-2. [DOI] [PubMed] [Google Scholar]
- 5.Paraskevas S. Randomized controlled clinical trials on agents used for chemical plaque control. Int J Dent Hyg. 2005;3:162–78. doi: 10.1111/j.1601-5037.2005.00145.x. [DOI] [PubMed] [Google Scholar]
- 6.Zhan L, Featherstone JD, Gansky SA, Hoover CI, Fujino T, Berkowitz RJ, et al. Antibacterial treatment needed for severe early childhood caries. J Public Health Dent. 2006;66:174–9. doi: 10.1111/j.1752-7325.2006.tb02576.x. [DOI] [PubMed] [Google Scholar]
- 7.Van Strydonck DA, Slot DE, Van der Velden U, Van der Weijden F. Effect of a chlorhexidine mouthrinse on plaque, gingival inflammation and staining in gingivitis patients: A systematic review. J Clin Periodontol. 2012;39:1042–55. doi: 10.1111/j.1600-051X.2012.01883.x. [DOI] [PubMed] [Google Scholar]
- 8.Botelho MA, Bezerra-Filho JG, Correa LL, Heukelbach J. Effect of a novel essential oil mouthrinse without alcohol on gingivitis: A double-blinded randomized controlled trial. J Appl Oral Sci. 2007;15:175–80. doi: 10.1590/S1678-77572007000300005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ribeiro LG, Hashizume LN, Maltz M. The effect of different formulations of chlorhexidine in reducing level of mutan streptococci in the oral cavity. J Dent. 2007;35:359–70. doi: 10.1016/j.jdent.2007.01.007. [DOI] [PubMed] [Google Scholar]
- 10.Twetman S. Antimicrobials in future caries control. Caries Res. 2004;38:223–9. doi: 10.1159/000077758. [DOI] [PubMed] [Google Scholar]
- 11.Gupta D, Bhaskar DJ, Gupta RK, Karim B, Gupta V, Punia H, et al. Effect of Terminalia chebula Extract and Chlorhexidine on Salivary pH and Periodontal Health: 2 Weeks Randomized Control Trial. Phytother Res. 2013 doi: 10.1002/ptr.5075. [In press] [DOI] [PubMed] [Google Scholar]
- 12.Autio-Gold J. The role of chlorhexidine in caries prevention. Oper Dent. 2008;33:710–6. doi: 10.2341/08-3. [DOI] [PubMed] [Google Scholar]
- 13.Ahonkhai I, Ba A, Edogun O, Mu U. Antimicrobial activities of the volatile oils of Ocimum bacilicum L. and Ocimum gratissimum L. (Lamiaceae) against some aerobic dental isolates. Pak J Pharm Sci. 2009;22:405–9. [PubMed] [Google Scholar]
- 14.Turesky S, Gilmore ND, Glickman I. Reduced plaque formation by the chloromethyl analogue of Victamine C. J Periodontol. 1970;41:41–3. doi: 10.1902/jop.1970.41.41.41. [DOI] [PubMed] [Google Scholar]
- 15.Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–51. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 16.Pattanayak P, Behera P, Das D, Panda SK. Ocimum sanctum Linn. A reservoir plant for therapeutic applications: An overview. Pharmacogn Rev. 2010;4:95–105. doi: 10.4103/0973-7847.65323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Geeta, Vasudevan DM, Kedlaya R, Deepa S, Ballal M. Activity of Ocimum sanctum (the traditional Indian medicinal plant) against enteric pathogens. Indian J Med Sci. 2001;55:434–8. [PubMed] [Google Scholar]
- 18.Singh PH. 1st ed. India: CRC Press; 2002. Rasayana: Ayurvedic Herbs for Longevity and Rejuvenation; pp. 272–80. [Google Scholar]
- 19.Shokeen P, Bala M, Sing M, Tandon V. In vitro activity of eugenol, an active component from Ocimum sanctum, against multiresistant and susceptible strains of Neisseria gonorrhea. Int J Antimicrob Agents. 2008;32:172–9. doi: 10.1016/j.ijantimicag.2008.03.018. [DOI] [PubMed] [Google Scholar]
- 20.Kelm MA, Nair MG, Strasburg GM, DeWitt DL. Antioxidant and cyclooxygenase inhibitory phenolic compounds from Ocimum sanctum Linn. Phytomedicine. 2000;7:7–13. doi: 10.1016/S0944-7113(00)80015-X. [DOI] [PubMed] [Google Scholar]
- 21.Jaggi RK, Madan R, Singh B. Anticonvulsant potential of holy basil, Ocimum sanctum Linn., and its cultures. Indian J Exp Biol. 2003;41:1329–33. [PubMed] [Google Scholar]
- 22.Singh S. Comparative evaluation of antiinflammatory potential of fixed oil of different species of Ocimum and its possible mechanism of action. Indian J Exp Biol. 1998;36:1028–31. [PubMed] [Google Scholar]
- 23.Singh S, Majumdar DK. Evaluation of anti-inflammatory activity of fatty acid of Ocimum Sanctum fixed oil. Indian J Exp Biol. 1997;35:380–5. [PubMed] [Google Scholar]
- 24.Agarwal P, Nagesh L, Murlikrishnan Evaluation of the antimicrobial activity of various concentrations of Tulsi (Ocimum sanctum) extract against Streptococcus mutans: An in vitro study. Indian J Dent Res. 2010;21:357–9. doi: 10.4103/0970-9290.70800. [DOI] [PubMed] [Google Scholar]
- 25.Prakash P, Gupta N. Therapeutic uses of Ocimum sanctum linn (Ocimum sanctum) with a note on eugenol and its pharmacological actions: A short review. Indian J Physiol Pharmacol. 2005;49:125–31. [PubMed] [Google Scholar]
- 26.Gupta D, Bhaskar DJ, Gupta RK. 1st ed. Gemany: Lap Lambert Academic Publishing; 2013. Contemporary and Alternative Dentistry: Ayurveda in Dentistry. [Google Scholar]
- 27.Franco Neto CA, Parolo CC, Rösing CK, Maltz M. Comparative analysis of the effect of two chlorhexidine mouthrinses on plaque accumulation and gingival bleeding. Braz Oral Res. 2008;22:139–44. doi: 10.1590/s1806-83242008000200008. [DOI] [PubMed] [Google Scholar]
- 28.Najafi MH, Taheri M, Mokhtari MR, Forouzanfar A, Farazi F, Mirzaee M, et al. Comparative study of 0.2% and 0.12% digluconate chlorhexidine mouth rinses on the level of dental staining and gingival indices. Dent Res J (Isfahan) 2012;9:305–8. [PMC free article] [PubMed] [Google Scholar]
- 29.Herrera D. Chlorhexidine mouthwash reduces plaque and gingivitis. Evid Based Dent. 2013;14:17–8. doi: 10.1038/sj.ebd.6400915. [DOI] [PubMed] [Google Scholar]


