Abstract
Objective Review measures of readiness to transition to adult-oriented care for youth with chronic physical health conditions. Methods Identified measures via online searches and reference lists and reviewed methods of development, theoretical underpinnings, characteristics, and psychometrics. Measures were classified according to American Psychological Association Division 54 Evidence-Based Assessment (EBA) Task Force criteria. Strengths and weaknesses of reviewed measures were described. Results 56 measures were identified, of which 10 met inclusion criteria for this review. 6 were disease specific and 4 were generic. Some psychometric properties were reported for each; none reported predictive validity for transition outcomes. According to EBA criteria, the 10 measures met criteria for “promising” assessment. Conclusions Measurement development in transition readiness is still an underdeveloped area. Measures require further testing and new measures are needed. Recommendations include testing measures with larger and diverse samples, ground measures in theory, test psychometrics, and involve multiple stakeholders in measure development.
Keywords: adolescents, assessment, chronic illness, systematic review
Improvements in survival rates for youth with chronic physical health conditions have yielded a growing population of adolescents and young adults (AYA) in need of adult-focused medical care (American Academy of Pediatrics, American Academy of Family Physicians, & American College of Physicians, 2011). Although the transfer to adult-focused care is often medically and developmentally indicated, pediatric providers frequently struggle with the transition process—specifically determining when and how to plan for the transfer of care. The transfer of care is often poorly executed, resulting in inappropriate health care utilization (White, 2002), nonadherence to medical treatments (Annunziato et al., 2007), failure to establish a connection with an adult medical provider (Tuchman, Slap, & Britto, 2008), and continued care in the pediatric setting by default (Blum et al., 1993). Consequences of inadequate or inappropriate care due to poor transition planning include onset of secondary disabilities (Williams, 2009) and increased rates of hospitalization (Gurvitz et al., 2007). On the other hand, a well-planned transition has benefits as indicated by patient-reported satisfaction with care, increase in self-management following transfer, and improved empowerment (Tuchman et al., 2008).
To improve the transition process, a new clinical algorithm was created (American Academy of Pediatrics et al., 2011) and a related “toolkit” (www.gottransition.org) has been disseminated. Both the algorithm and toolkit emphasize the importance of tracking transition readiness. A review of the literature indicates that transition readiness is best defined as indicators that the AYA and their medical support system (family and medical providers) can begin, continue, and finish the transition process through the discrete event of transfer (Betz & Telfair, 2007; Schwartz et al., 2013; Telfair, Alexander, Loosier, Alleman-Velez, & Simmons, 2004). It involves multiple components, is measurable, and is potentially modifiable before transfer (Schwartz, Tuchman, Hobbie, & Ginsberg, 2011). Thus, it is critical to track and promote transition readiness among AYA patients to prepare them to successfully engage in adult medical care. Supports or interventions can be put into place to improve transition readiness, referred to as transition planning (Schwartz et al., 2011).
Despite the clinical algorithm and toolkit intended to enhance the transition process, there is little consensus on the essential components of transition readiness and progress in developing evidence-based assessments for tracking transition readiness has been slow. Extant research has focused on age, skills, and knowledge as components of transition readiness without exploration of broader social-ecological associates such as relationships, socioeconomic factors, and psychosocial factors related to multiple stakeholders in the process (Betz, 2000; Cappelli, MacDonald, & McGrath, 1989). Advancing measurement of transition readiness is essential to better understand intervention targets to enhance the likelihood of engagement in the adult health care system following transfer (Schwartz et al., 2011; 2013). Specifically, evidence-based transition readiness assessments are important for both clinical and research purposes for tracking progress of readiness over time, identifying targets of intervention, assessing outcomes of intervention, and allowing comparisons of transition readiness across cohorts and clinics (Schwartz et al., 2011; 2013).
While many transition readiness measures have been developed, most are new, not widely used, and have not been well tested. Furthermore, while other reviews of transition-related measures have recently been published, they have not included clear recommendations for further measurement testing and development (Stinson et al., 2013; Zhang, Ho, & Kennedy, 2014). Thus, the current article provides a systematic review of published measures of transition readiness for AYA with chronic physical health conditions to provide clinicians and researchers guidance on choosing and developing transition readiness measures for their population of interest. Strengths of this systematic review include strict inclusion criteria of published self-described transition readiness measures with evaluable data; descriptions of all the measures, including theoretical background and psychometrics; guidance on choosing measures; and recommendations for future research in transition readiness measure development. Specifically, the goals of this review are to (1) review existing published measures of transition readiness with psychometric data; (2) classify measures using American Psychological Association Division 54 Evidence-Based Assessment (EBA) Task Force criteria (Cohen et al., 2008) and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher, Liberati, Tetzlaff, & Altman, 2009); (3) evaluate strengths and weaknesses of the measures; and (4) make recommendations for future research and measurement development for transition readiness.
Method
Procedure
Multiple academic databases (PsycInfo, Medline, Health and Psychosocial Instruments, Scopus, Google Scholar) and a general online search engine (Google) were searched to identify transition readiness measures during the following: March 2011 (author KMW), and August 2011, December 2011, April 2012, January 2013, June 2013, and December 2013 (author LDB). Ongoing searches were conducted to assure the most comprehensive and current review before submitting for publication. Combinations of the following terms were used in searches: adolescent, young adult, pediatric, youth, chronic illness, condition; adult care, health care transition, medical transition, transition readiness, transfer; and measure, questionnaire, survey, checklist, assessment, inventory, and tool. Reference lists were checked for additional measures. A search for additional references citing the original source references of the measures in the review, using the cited reference function of Web of Science, was also conducted (author LCD). Some authors of measures that met inclusion criteria were contacted for additional information.
A measure met inclusion criteria if it (1) was self-described as a measure of transition readiness, (2) pertained to chronic physical health condition(s), (3) was administered in English, (4) was published in a peer-reviewed journal, and (5) presented psychometrics. The following were excluded: unpublished measures, lists of general guidelines, open-ended worksheets, measures specifically targeting mental health or developmental disorders, measures that used a single item to assess transition readiness, measures not self-identified as assessing transition readiness, and measures that did not measure a coherent transition readiness construct either based on a proposed theoretical framework or empirical evidence (e.g., studies measuring associates of transition readiness or measures of single item domains were excluded). Also, measures were not included if authors did not explicitly report indices of reliability or validity (e.g., there was no claim of psychometrics reported in the article). Of those papers with reported psychometrics, there may have been other indices of validity (e.g., expert review, expected correlates) that authors did not refer to as validity, but were included here as indicators of validity to provide as much supporting information to readers. Both generic (intended to be generalizable across conditions) and condition-specific measures were included, as both have potential merit when choosing or developing a transition readiness measure. Generic measures can be used with heterogeneous populations. Disease specific measures may be more sensitive to factors specific to a certain population.
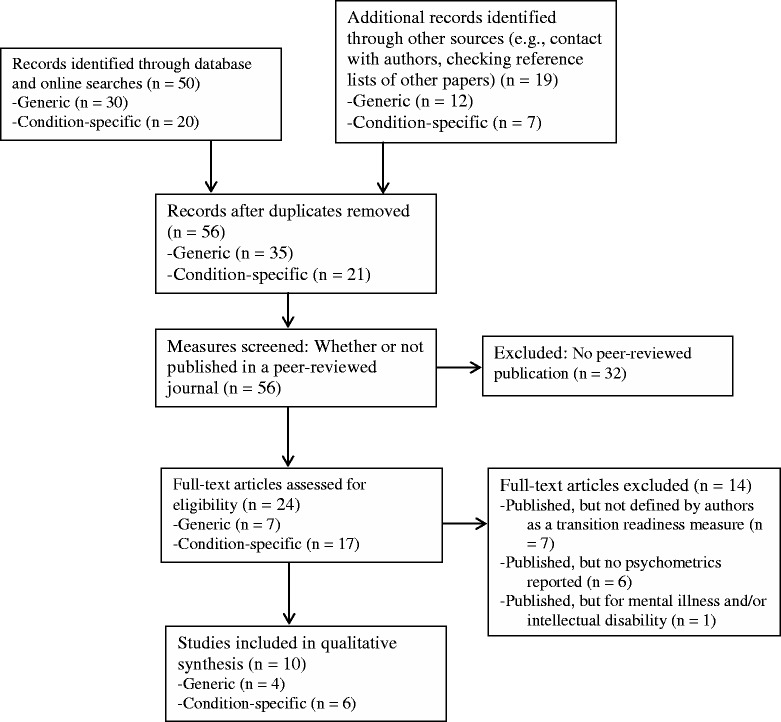
Identified measures that were published in peer-reviewed journals were screened for inclusion/exclusion criteria in team meetings. Resulting measures were categorized as generic or condition-specific, as defined by measure authors, and reviewed for methods of development, theoretical underpinnings, intended respondent, measure format (number of items, response options, scoring, time to complete), content area or subdomains, sample size and characteristics (age, race/ethnicity, health conditions), location of recruitment, response rate, and psychometric data reported by authors. Measures were classified according to EBA criteria as “well-established” (at least two investigators or research groups have published peer-reviewed articles using the measure, measure or manual presented or available on request, good psychometric properties presented in detail), “approaching well-established” (published in at least two articles—regardless of author, sufficient information for evaluation and replication presented, moderate psychometric statistics presented or described in vague terms), or “promising assessment” (published at least once in a peer-reviewed article, sufficient information for evaluation and replication presented, moderate or vague psychometrics presented) (see Cohen et al., 2008 for full details). The review process followed PRISMA guidelines (Moher et al., 2009; Table I). All available data and reported characteristics of the measures were presented.
Review and Description of Measures
Overall, 56 measures were identified—24 published in peer-reviewed journals and 32 identified online or through unpublished abstracts (Figure 1). None of the online measures met inclusion criteria due to lacking published data. Of the published measures, 14 were not included because they were not identified by authors as a measure of transition readiness (n = 7), were not tested for psychometric properties (n = 8), and/or did not pertain to patients with a chronic physical health condition (n = 2). Psychometric data are available for 10 measures that are reviewed here: 4 are generic and 6 are condition-specific. See Figure 1 for a PRISMA flow diagram of measures identified, screened for eligibility, and number included and excluded. Table I (generic) and Table II (condition-specific) summarize data for each measure, listed alphabetically. The tables include references of publications on the measure and all available psychometric data. More detail on generic and condition-specific measures is provided below, including information on stated purpose, measure development, theoretical underpinnings, subscales, scoring, and findings related to correlates. Descriptions of measures are dependent on available published information about measures.
Figure 1.
PRISMA flow chart.
Table I.
Generic Transition Readiness Measures
| Measure | Characteristics | Content areas | Sample | Reliability | Validity |
|---|---|---|---|---|---|
| California Healthy and Ready to Work (HRTW) Transition assessment tool: health care self-care (Betz et al., 2000) | 72 items, patient or parent (proxy) report; coded by provider as yes, no, or with assistance | Knowledge, skills, self-management (14 total domains) | N = 25 from transition clinic (cancer, n = 8; developmental disability, n = 7; other, n = 10), 14–21 yo, 92% minority | IC:8/14 domains Kuder–Richardson α > .60 | Known groups (condition) |
| Self-Management Skills Assessment Guide (SMSAG) (Williams et al., 2010) | 21 items, patient and parent (proxy) report, Likert-type scale | Knowledge, participation in medical decision making and discussions, self-management | Neurological (n = 32 from clinic) and other conditions (n = 17 from transition clinic), 11–19 yo, 14% minority, 65% response rate | IC: patient α = .89, parent α = .93; IRRpatient and parent: r = .56, p < .01 | Known groups (participation transition program), convergent (independence) |
| Transition Readiness Assessment Questionnaire 4.1 (TRAQ) (Sawicki et al., 2011) | 29 items, patient report, Likert-type scale | Skills for self-management; skills for self-advocacya | N = 192 from CF or transition clinic (incl cognitive impairment and mental health condition), 16–26 yo, 36% minority | IC: α = .82–.93 | CVR with youth (n = 15) and experts (n = 12), EFA with two factors, known-groups (age, condition, gender) |
| TRxANSITION Scale (Ferris et al., 2012) | 33 items; interview with patients; rated by clinician as yes, no, somewhat; 8 min | Knowledge, medications, adherence, nutrition, self-management, reproduction, trade/school, insurance, support, new providersa | N = 128 from specialty clinics with various diagnoses, 12–22 yo, 38% minority | IC: item-domain (r = .42–.85), item-total (r = .16–.62), domain-total (r = .34–.74); IRR: κ = .71 | Expert review, convergent validity (age) |
Note. Characteristics include (as indicated in publications) number of items, respondent, response options and format, scoring, amount of time to complete.
IC: internal consistency; IRR: inter-rater reliability. Unless otherwise specified, reported alphas are Cronbach’s alphas. CVR: content validity ratings; EFA: exploratory factor analysis. Known groups validity includes variables found to be related to transition readiness in the expected direction.
aSubscales specified by authors.
Table II.
Condition-Specific Transition Readiness Measures
| Measure | Characteristics | Content areasa | Sample | Reliability | Validity |
|---|---|---|---|---|---|
| Cystic fibrosis | |||||
| Cystic Fibrosis Health Care Transition Readiness Scale (CFHCTS) (Dudman et al., 2011) | 57 items, patient report, Likert-type scale; scored by clinician | Knowledge, skills, self-management | Not tested | Not tested | CVR (n = 4 experts) |
| Readiness Questionnaire (RQ) (Cappelli et al., 1989) | 24 items, patient report; 1 item of parent/provider report; scored by clinician; varied format | Behavior, knowledgea | n = 9 patients from CF clinic and n = 27 patients at CF camp | IRR of single summary question completed by caregivers on overall readiness: r = .65 | Discriminate analyses |
| Kidney transplant | |||||
| Readiness for Transition Questionnaire (RTQ) (Gilleland et al., 2012) | 22 items, patient and parent report (parent reports on patient and parent behaviors), likert-type scale; | Overall transition readiness, Adolescent responsibility, Parent involvementa | n = 32 parents and n = 48 patients from kidney transplant transition clinic, 15–21 yo, 42% minority, 89% response rate | IC: patient α = .79–.94, parent α = .85–.89; IRR parent and patient: r = .50–.68, p < .01 | Convergent: theoretically and empirically driven regression models to predict transition readiness with hypothesized correlates |
| HIV | |||||
| Transition Readiness Questionnaire (TRQ) (Wiener, Zobel, Battles, & Ryder, 2007) | 21 items, patient or parent report, interview with clinician ratings | Self-management, Skills, Knowledge, Support, Resources | n = 39 caregivers and n = 12 patients ≥ 18 in HIV transition program, 9–25 yo, 55% minority, 68% response rate | Not reported | Responsivity to intervention, Convergent validity (anxiety, number of years at NIH, lower confidence in community provider) |
| Liver transplant | |||||
| Transition Readiness Survey: Adolescent/ Young Adult (TRS: A/YA) (Fredericks et al., 2010) | Patient: 38 written items and 4 provider administered questions; parent: 36 items (proxy of adolescent skills and parent knowledge); some items must be scored by clinician; varied format | Self-management, Demonstrated Skills, Psychosocial adjustment, Regimen Knowledgea | n = 58 parents and n = 71 transplant recipients, 11–20 yo, 37% minority; 98% response of eligible patients | IC: patient α = .68–.85, total α = .85; parent: α = .19–.79, total = .75; IRR parent and patient: r = −.26–.58 | PCA, Known groups (age, clinic attendance) |
| Sickle cell disease | |||||
| Sickle Cell Transfer Questionnaire (SCTQ) (Telfair et al., 1994, 2004) | 67 items, patient or parent (proxy) report, varied format of yes/no and open ended | Demography, Concerns about transition, Emotions about move to an adult program, Reasons for a transition program, Adolescent’s perceptions about content of transitiona | n = 60 21–30 yo, n = 36 13–19 yo, 95% minority; n = 25 caregivers; 65% return rate | Not reported | Delphi review; Known groups (age, severity, education, location of care) |
Note. Characteristics include (as indicated in publications) number of items, respondent, response options and format, scoring, amount of time to complete. IC: internal consistency; IRR: inter-rater reliability; CVR: content validity ratings; PCA: principal component factor analysis; CF: cystic fibrosis. Reported alphas are Cronbach’s alphas. Known groups validity includes variables found to be related to transition readiness in the expected direction.
aSubscales specified by authors.
Generic Measures
Seven generic measures were published in peer-reviewed journals, and psychometric data were provided on four. All four reported data on internal consistency [Healthy and Ready to Work (HRTW), Self-Management Skills Assessment Guide (SMSAG), Transition Readiness Assessment Questionnaire (TRAQ), TRxANSITION Scale (TRxANSITION)]. The TRAQ conducted factor analysis to identify subscales. Content validity for three of the four measures (HRTW, TRAQ, and TRxANSITION) were supported by feedback of experts, patients, parents, and/or providers. Only the TRAQ and TRAxNSITION measures reported data on construct validity. All four measures met EBA criteria for classification as a “promising assessment.”
California HRTW Transition Assessment Tool
The HRTW Tool is a comprehensive measure of overall transition readiness, broadly defined, that includes a subset of items on health care self-care for measuring transition to adult care (Betz, 1998, 2000; Betz, Redcay, & Tan, 2003). These items assess patients’ knowledge and skills for disease self-management with 14 domains assessed (e.g., knowledge of condition, communication, transportation use). Relevant knowledge and skills were determined through a literature review. Item development of the broader measure was based on developmental (Erickson, 1963; Piaget & Inhelder, 1969) and self-care (Orem, 1995) theoretical frameworks. The percent of each coded response (yes, no, with assistance, NA) is calculated to understand the patient’s disease knowledge and skills. Internal consistency was low for many domains, presumably because of restricted range of responses and low sample size (Betz et al., 2003). Youth with cancer had more self-care health care skills than youth with developmental disability (Betz et al., 2003). This measure has been adapted and shortened (15 items) for use in chronic rheumatic disease (Lawson et al., 2011).
The Self-Management Skills Assessment Guide
The SMSAG (Williams et al., 2010) was developed to assess health care self-management said to be a proxy for transition readiness among youth based on literature review and extant measures. Items of existing transition readiness assessments were selected to assess a wide range of self-management skills and were adapted to be relevant for all chronic health conditions and to fit on a consistent response scale. Responses are averaged to create a Medical Self-Management total score. There were no group differences by age, gender, minority status, or parent education. The sample recruited from the transition clinic had higher scores than those from the neurology clinic. Parent-rated independence was related to parent and youth scores.
Transition Readiness Assessment Questionnaire 4.1
The TRAQ (Sawicki et al., 2011) was developed to measure mastery of disease self-management skills. It was derived from a pool of items from nine existing nonvalidated clinical tools and informed by content validity ratings and feedback from experts and AYA patients. TRAQ response options are based on the Stages of Change Model (Prochaska & DeClemente, 1986). Two domains were identified through principal component exploratory factor analysis (Skills for Self-Management and Skills for Self-Advocacy) and domain scores are computed by averaging items. The scales have high internal consistency. Older age and absence of cognitive or mental health impairment related to higher scores on both domains. Female patients scored higher on self-advocacy. There were no differences by race/ethnicity. This measure has undergone more testing than most transition readiness measures and evidences good validity and reliability, but its focus is limited to skills. Authors have also developed a shorter 20-item version (Wood, Sawicki, Reiss, & Livingood, 2012), which is currently under review for publication (Sawicki, personal communication).
The UNC TRxANSITION Scale
The TRxANSITION (Ferris et al., 2012) measures 10 domains of transition readiness: Type of Illness, Rx = medications, Adherence, Nutrition, Self-management, Informed reproduction, Trade/school, Insurance, Ongoing support, and New health providers. Development of items was rooted in theoretical models of learning and self-determination (Committee on Developments in the Science of Learning, 2000; Ryan & Deci, 2000), and informed by existing literature, and qualitative data collection with experts and patients. A total score of transition readiness and domain scores are computed based on clinician ratings of patient responses. Transition readiness was related to age.
Condition-Specific Measures
Twenty-one condition-specific measures [cystic fibrosis (n = 4), liver transplant (n = 3), sickle cell disease (n = 2), HIV/AIDS (n = 3), spina bifida (n = 1), kidney transplant (n = 1), childhood cancer survivor (n = 2), metabolic conditions (n = 1), chronic rheumatic disease (n = 1), and mental health/intellectual disability (n = 3)] were evaluated, of which 15 were published and 6 met inclusion criteria. The condition-specific measures reviewed here were developed to assess disease-specific factors that can affect transition readiness. Three of the six measures reported reliability data with Cronbach’s alpha values for internal consistency [Readiness Questionnaire (RQ), Readiness for Transition Questionnaire (RTQ), Transition Readiness Survey (TRS)]. The TRS was the only condition-specific measure to conduct a factor analysis (Fredericks et al., 2010). Three measures received feedback from experts via Delphi reviews [Sickle Cell Transfer Questionnaire (SCTQ)] or content validity ratings [Cystic Fibrosis Health Care Transition Readiness Scale (CFHCTRS), RQ]. Two reported data on convergent and construct validity via correlations with theoretically related constructs [RTQ, Transition Readiness Questionnaire (TRQ)]. All six measures met EBA criteria for “promising assessment.”
Cystic Fibrosis Health Care Transition Readiness Scale
The CFHCTRS (Dudman, Rapley, & Wilson, 2011) assesses adolescents’ health knowledge and self-management skills. Item development was informed by self-efficacy theory (Bandura, 2006) and the trans-theoretical model (Zimmerman, Olsen, & Bosworth, 2000), interviews with patients (n = 2) and parents (n = 4), and extant literature. The items are worded as “I can …” to elicit ratings of self-efficacy, with some items requiring reverse scoring to reflect higher scores for patients with greater self-efficacy. Experts provided content validity ratings on items, resulting in omission of nine items lacking content validity. Subsequent data collection and factor analysis is planned (Dudman et al., 2011).
Readiness Questionnaire
The RQ (Cappelli et al., 1989) assesses the knowledge and readiness of adolescents with cystic fibrosis to transfer to adult care. Interviews with pediatric and adult caregivers and pediatric and adult patients with cystic fibrosis informed item development. The questions assess disease-specific and generic transition knowledge and skills. An extensive scoring protocol is described in the manuscript to determine the total score and two subscales (Knowledge and Behavior). A single item to rate overall transition readiness is scored by a caregiver. Discriminate analysis based on the two groups of able to and not able to cope with transition showed that the behavioral subscore correctly classified 80.5% of subjects compared with 69.4% by knowledge, 77.7% by total score, and 44% by age.
Readiness for Transition Questionnaire
The RTQ (Gilleland, Amaral, Mee, & Blount, 2012) is designed to measure transition readiness, health management behavior, and family involvement in health care. The RTQ was originally developed for kidney transplant recipients via a review of literature on transition, existing transition measures, adolescent medicine policy, and position papers, and was later adapted for pediatric cancer survivors (Gilleland et al., 2013). The measure comprises three subscales: Overall Transition Readiness, Adolescent Responsibility, and Parental Involvement. Scores are yielded for Overall Transition Readiness (2 items) and individual subscales. Higher adolescent responsibility and knowledge were related to higher transition readiness.
Transition Readiness Questionnaire
This questionnaire was developed to assess transition readiness and inform targets of intervention for patients with HIV in advance of forced transfer of care when the pediatric clinic at the National Institutes of Health (NIH) closed (Wiener, Zobel, Battles, & Ryder, 2007). Many were being transferred to an adult provider in the community. The measure, informed by a literature review on barriers to transition, yields a Global Readiness score that comprises items about other provider, insurance/financial concerns, transportation to appointments, pharmacy, disease knowledge, having a social worker or other assistance. The measure was administered by phone to parents (of patients <18 years old) and patients (≥18 years old) before and after (M = 6.8 months) targeted intervention to enhance transition readiness. Transition readiness scores were significantly higher at T2 compared with T1. Transition readiness at T1 was negatively related to anxiety and less years spent in the NIH clinic, but was not related to disease severity. Lack of confidence in the new provider was negatively related to transition readiness at both time points. The scoring of the measure is conducted by the clinician.
Transition Readiness Survey: Adolescent/Young Adult and Parent
The Transition Readiness Survey: Adolescent/Young Adult and Parent (TRS: A/YA) (Fredericks et al., 2010) was designed to screen transition readiness skills in pediatric liver transplant recipients in a clinical setting and was based on literature reviews and clinical observations. The measure is composed of four subscales identified through factor analysis: Demonstrated Skills, Self-Management, Psychosocial Adjustment, and Perceived Regimen Knowledge. Parents provide their perception of their child’s skills and their own regimen knowledge (TRS: P). Higher scores indicate greater skills, knowledge, and adjustment. Fredericks and colleagues (2010) describe the scoring protocol for both versions, which includes percentage correct. Age was associated with most transition readiness indices and parent knowledge was associated with better clinic attendance. However, there were no associations between transition readiness and health outcomes or adherence with the exception of higher self-management scores being related to lower medication adherence. Internal consistency of total scores and subscales was good with the exception of parent reported regimen knowledge. The first author reports that this measure is currently being revised to reduce the number of overall items (Fredericks, personal communication).
Sickle Cell Transfer Questionnaire
The SCTQ (Telfair et al., 2004; Telfair, Myers, & Drezner, 1994) was developed for AYA with sickle cell disease via interviews, extant measure review, and Delphi reviews. Item scoring varies by subscale and is available from the authors (Telfair, personal communication). The SCTQ is unique in that it identifies specific concerns about transition, including difficulty terminating relationships with medical providers, concerns about adult medical providers, emotions surrounding transition, and anxiety about being responsible for their own care. Transition readiness was related to older age, less severe sickle cell disease genotype, and college education (Telfair et al., 1994). This measure has been adapted for use in cystic fibrosis (Westwood, Henley, & Willcox, 1999). The Concerns and Emotions section has been used for pre/post engagement assessment in a pilot transition program for adolescents with sickle cell disease (Smith, Lewis, Whitworth, Gold, & Thornburg, 2011). The intervention had some effect on concerns and emotions, but within subjects changes were not examined for significance.
Discussion
The large number of unpublished tools and increasing number of published transition readiness measures, a special issue in this Journal (“Health care Transition,” 2011, volume 36, number 2) dedicated to transition, and other recent reviews of measures related to transition (Stinson et al., 2013; Zhang et al., 2014) are indicative of increasing recognition of the need to study and measure readiness to transition to adult care for youth with chronic health conditions. Ten measures met criteria for this review and also met EBA criteria for “promising assessment.” The promising measures serve as a valuable starting point from which to refine current and inform future measures of transition readiness.
A handful of the measures were informed by theory (TRAQ, HRTW, CFHCTRS), representing diverse fields (e.g., developmental psychology, health psychology) and yielding different perspectives on transition, which strengthens our understanding of this complex process. Mixed methods participatory approaches to measure development were also strengths of several measures in this review drawing from patients, providers, and expert input (TRAQ, TRxANSITION, CFHCTRS, RQ, RTQ, SCTQ, TRS). By considering patient and family perspectives in addition to clinical expertise, using a participatory approach increases the likelihood of clinical acceptability of the measure and likelihood that the measure will identify clinically valid targets of intervention (Spring, 2007). Ethnic and racial diversity of original samples was also a strength of several measures (HRTW, RTQ, TRAQ, TRQ).
Validity data varied. At minimum, some studies presented evidence of content validity (TRAQ, TRxANSITION, SCTQ). Most presented promising findings with samples of patients and/or parents supporting known groups validity (HRTW, SMSAG, TRAQ, TRS, SCTQ) or convergent validity (SMSAG, TRxANSITION, RTQ, TRQ). Findings revealed that transition readiness was related to variables such as older age, less severe disease or condition, participation in a transition clinic, lower anxiety, and higher confidence in adult providers. Additionally, The TRAQ and TRS were factor analyzed, yielding strong subscales with the exception of one on the TRS.
Despite promising data on the measures, it is important to consider some limitations and characteristics of the measures. Most were developed for use with specific clinical populations to serve a clinical need (e.g., as a screener or a tool to plan forced transfers of care). As such, most were not intended to launch a program of research on measurement development and validation. In fact, although some measures presented data supporting the validity of the measure, many authors did not present it as such and no measures were tested in more than one study, thus limiting some measures’ ability to reach “approaching well-established assessment” criteria. Also, despite the fact that all met criteria for “promising assessment,” the amount of psychometric data varied greatly. Few measures presented reliability statistics or factor analysis, fewer provided data on content validity, and no measures were tested for predictive validity. Thus, understanding the relationship between current measures and patient outcomes after transfer of care is lacking. Reliability of some generic measures was also limited by using samples of patients with various health conditions and presenting psychometrics for the entire sample, though reliability and validity may have differed across groups (e.g., HRTW Transition Assessment Tool, TRAQ). The samples were also limited to convenience samples, many of which were noted to be attending a transition clinic (e.g., Self-management Skills Assessment, TRAQ, RTQ, TRQ). Thus, the samples seem to be biased toward those already engaged in care and, in many instances, transition focused care. There is a lack of effort to validate transition readiness measures on patients who presumably need the most help transitioning—those who are not seen in clinic.
Additionally, there remains a lack of consistency and cohesion with regards to the construct of transition readiness. Knowledge and skills/self-management were each included in at least 60% of the measures suggesting that these are key components of transition readiness. However, these content areas neglect the broader psychosocial context of transition and theoretically are not sufficient for ensuring optimal outcomes after transfer (Bandura, 2005; Schwartz et al., 2013). Few have subscales exploring emotional and psychological aspects of transition (e.g., TRS, SCTQ) or other potential aspects such as motivation for or goals of transition, or relationships among patients, parents, and/or providers. Some also have the option to create a total score (e.g., SMSAG, TRxANSITION, RQ, TRQ), while most have individual subscales representing different aspects of transition readiness. The role of parents and providers in transition readiness conceptual models and measurement is also unclear as the perspectives of parents and providers are absent in most measures. Some measures allow for the parent to provide proxy report, while a few have parent report items reflecting the parent’s knowledge or skills (e.g., RTQ, TRS).
The current review also has some limitations that must be considered. The measures may have undergone further testing, but such research is yet to be disseminated. Inclusion criteria was also restricted to those measures that were defined by the authors as measuring transition readiness. Because of the lack of cohesion and theory related to transition readiness, this distinction is somewhat arbitrary and may have resulted in the omission of relevant measures that were not defined by authors as transition readiness. We did this to set limits on a potentially exhaustive list of measures that address components theoretically important for transition (e.g., self-care, adherence, disease management, transfer of responsibility, attitudes). However, the substantial overlap between transition readiness measures and other measures and the “arbitrariness” by which some measures are labeled transition readiness indicates the need for better definitions and theoretical frameworks to define transition readiness. Also, we could not always rely on the authors of the measures to clearly define validity data. Given the newness of the field and lack of evidence-based measures, we erred on the side of presenting all supportive data. Additional limitations of the inclusion criteria are the omission of measures that may be used clinically, but are not published, and measures developed in other languages. The review did, however, include two measures from Canada (SMSAG and RQ) and one from Australia (CFHCTRS).
In addition, while all of the measures in the current review were rated promising according to the EBA criteria, there was variation in the level of development and available psychometric data among the measures. For example, the TRAQ has more validity data than other measures, but could not receive a higher rating than “promising” because it has not yet been published and tested in another sample. Similarly, the CFHCTRS met criteria for “promising” because it included content validity ratings despite no psychometric data in a patient sample. Thus, there is a lack of sensitivity of this scale for a field with new measures, many of which are still in development.
This review revealed some important considerations when choosing a transition readiness measure. There is no best one-size-fits-all measure, although the TRAQ and TRxANSITION both are promising generic measures with a variety of supporting data. The TRAQ focuses on disease management skills, which may be limiting for some and fine for others. Its basis in the Stages of Change may lend itself to more readily identify targets of intervention to move toward action and maintenance. The TRxANSITION may have appealed to some, as it covers more content, including other issues related to transition to adulthood. It also assesses patient knowledge relative to medical records—a potential advantage—but also adds administrator burden in that it requires ratings by a clinician or investigator. Both measures are relatively brief. The other generic measures, the HRTW and the Self-Management Assessment, have less psychometric support but are beneficial in that they have both patient and parent forms. The HRTW also covers a wide range of topics, although it is also lengthy at 72 items. It is also important to recognize that the development of disease-specific measures suggests that there are aspects of transition readiness unique to certain conditions that cannot be captured in generic measures. In sum, specific considerations for choosing the right measure include generic or disease specific, content, psychometrics, measure length (range of 21–72 items), self-report or clinician ratings and scoring (e.g., measures requiring subjective rating or comparison of patient report of knowledge with medical records), and availability of parent version to report their perspectives or to serve as a proxy reporter for child.
Despite 10 available transition readiness measures, results from this review highlight the need for further testing of existing measures and development of new measures to establish evidence-based and empirically tested tools. Relative to other areas of assessment in pediatric psychology (Holmbeck et al., 2008; Palermo et al., 2008), AYA transition is still in the early stages of development. We are unaware of any new measures being developed with the exception of the Transition Readiness Inventory (TRI) for AYA survivors of childhood cancer (Schwartz et al., 2014). The development of the TRI is following NIH PROMIS (Patient Reported Outcomes Measurement Information System) guidelines. PROMIS methods (e.g., literature review, item binning and winnowing, item development, stakeholder input, item testing, mixed methods data collection) are a gold standard set by NIH for developing patient-reported outcomes and apply to the development of transition readiness measures (Forrest et al., 2012). We encourage the inclusion of PROMIS methods for future measurement development and also offer the following specific recommendations and considerations related to further validation of existing measures and new measure development in this burgeoning field:
Test for psychometric properties with appropriate sample sizes. Although some measures report more psychometrics than others, further assessment of reliability and validity is imperative. Sample sizes should be optimal for testing internal consistency of individual subscales, factor analysis, and multivariate models. Assessing predictive validity using longitudinal designs (Colver et al., 2013) is also critical, as it is unknown if transition readiness measures predict optimal outcomes. Markers of disease status (e.g., CD4 cell count in patients with HIV, hemoglobin A1c in patient with diabetes) indicating stable disease, health care utilization, including engagement in adult health care and acute care, patient and caregiver satisfaction with the transition process and transfer of care, and patient emotional well-being and quality of life are all potential outcomes (Colver et al., 2013; Holmes-Walker, Llewellyn, & Farrell, 2007; Reid et al., 2004). For guidelines on assessing psychometrics, refer to Holmbeck and Devine (2010).
Test measures with diverse and nonconvenience samples. It is important that researchers include diverse samples when further testing existing measures and creating new ones to enhance the generalizability and validity of measures. For generic measures, this ideally includes heterogenous samples with regards to conditions and examining reliability and validity within diagnostic groups and across groups. For all measures, a balance of race/ethnicity, income, gender, condition severity, age (ideally starting in early to mid adolescence), and engagement in care (recruiting those less engaged in care and not solely relying on convenience samples in clinic) is ideal. It is especially important to understand whether transition readiness measures are differentially relevant to patient populations from different cultural backgrounds.
Ground measures in theory. It is important that new measures, or ones that identify and adapt items from other measures, are grounded in theory. This is important for both supporting the validity of new measures and informing the constructs assessed. Although many clinical models of transition rely on age as an indicator for timing of transfer, and current measures focus heavily on knowledge and skills, the actual components related to transition readiness could be exhaustive when considering issues such as medical, interpersonal, and motivational factors. A theoretical model can provide a framework for the measure and the components to be assessed. For example, social ecological models such as the recently validated SMART (Social-ecological Model of AYA Readiness to Transition; Schwartz et al., 2013) may offer an overarching framework given the many demographic, environmental, and social complexities surrounding transition (Hamdani, Jetha, & Norman, 2011; Schwartz et al., 2011; Telfair & DeBaun, 2012).
Involve multiple stakeholder perspectives in measure development and assessment. Research and consensus statements emphasize the importance of collaboration between medical teams, parents, and patients for successful transition (American Academy of Pediatrics et al., 2011; Rosen, Blum, Britto, Sawyer, & Siegel, 2003; Van Staa, Jedeloo, van Meeteren, & Latour, 2011). Using various perspectives and expertise in the development phase increases the measure’s likelihood of acceptability and its clinical utility for guiding intervention (Spring, 2007). In addition, assessing transition readiness from multiple perspectives can promote collaboration between patients, parents, and providers, and comparison across stakeholders to reveal discrepancies in pertinent variables such as knowledge and goals. Such discrepancies may be important intervention targets.
Examine strengths and weaknesses of generic versus condition-specific measures. The clinical utility of generic versus condition-specific measures needs further assessment. Although there is value to having measures that transcend diagnoses, factors related to successful transition may vary by diagnosis (American Academy of Pediatrics et al., 2011). Generic measures may be more useful for clinical practice in primary care or a heterogenous disease population. Generic measures can address many cross-cutting concerns about AYA transition (e.g., emotional maturity, concerns about the adult health care system), but they may miss elements of disease management and knowledge of specific conditions. Generic measures may be strengthened through the addition of disease-specific modules. Furthermore, the adaptability of current disease-specific measures to other diseases should be tested (Gilleland et al., 2013).
Assess the ability to inform targets of intervention and respond to interventions. Transition readiness measures should inform viable targets of intervention to increase transition readiness over time and prepare for transfer (Schwartz et al., 2011). As part of this research, identifying and testing indicators of successful transition are critical to advancing this field and informing intervention development. Thus, assessment of transition readiness should lead to interventions that result in higher transition readiness scores over time. The ability of transition readiness measures to demonstrate responsiveness to intervention needs further attention, as well (Wiener et al., 2007).
This review is a testament to the growing interest in studying and measuring transition readiness. Rigorous methods should be used to further test current and develop new measures to facilitate transition planning of AYA from pediatric to adult-focused care. Such measures are called for by medical colleagues (American Academy of Pediatrics et al., 2011) and are needed to track progress of transition readiness and inform targets of intervention that can ultimately facilitate a successful transfer of care (Schwartz et al., 2011). Pediatric psychologists are well positioned and trained to contribute to this growing body of measures.
Funding
This work was supported by an R21 grant (CA141332), “Transition Readiness of AYA Survivors of Childhood Cancer,” awarded to Lisa Schwartz, PhD from the National Cancer Institute at the National Institutes of Health.
References
- American Academy of Pediatrics, American Academy of Family Physicians, & American College of Physicians. Clinical Report—Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011;128:182–200. doi: 10.1542/peds.2011-0969. [DOI] [PubMed] [Google Scholar]
- Annunziato R A, Emre S, Shneider B, Barton C, Dugan C A, Shemesh E. Adherence and medical outcomes in pediatric liver transplant recipients who transition to adult services. Pediatric Transplantation. 2007;11:608–614. doi: 10.1111/j.1399-3046.2007.00689.x. [DOI] [PubMed] [Google Scholar]
- Bandura A. Adolescent development from an agentic perspective. In: Pajares F, Urdan T C, editors. Self-efficacy beliefs of adolescents. Vol. 46. Charlotte, NC: Information Age Publishing; 2005. pp. 1–43. [Google Scholar]
- Bandura A. Self efficacy beliefs of adolescents. Greenwich, CT: Information Age Publishing; 2006. [Google Scholar]
- Betz C L. Facilitating the transition of adolescents with chronic conditions from pediatric to adult health care and community settings. Issues Comprehensive Pediatric Nursing. 1998;21:97–115. doi: 10.1080/014608698265528. [DOI] [PubMed] [Google Scholar]
- Betz C L. California Healthy and Ready to Work Transition Health Care Guide: Developmental guidelines for teaching health care self-care skills to children. Issues Comprehensive Pediatric Nursing. 2000;23:203–244. doi: 10.1080/014608600300029867. [DOI] [PubMed] [Google Scholar]
- Betz C L, Redcay G, Tan S. Self-reported health care self-care needs of transition-age youth: A pilot study. Issues in Comprehensive Pediatric Nursing. 2003;26:159–181. doi: 10.1080/01460860390223880. [DOI] [PubMed] [Google Scholar]
- Betz C L, Telfair J. Health care transitions: An introduction. In: Betz C L, Nehring W M, editors. Promoting health care transitions for adolescents with special health care needs and disabilities. Baltimore, MD: Paul H. Brookes Pub; 2007. pp. 3–19. [Google Scholar]
- Blum R, Garell D, Hodgman C, Jorissen T, Okinow N, Orr D, Slap G. Transition from child-centered to adult health-care systems for adolescents with chronic conditions. A position paper of the Society for Adolescent Medicine. Journal of Adolescent Health. 1993;14:570–576. doi: 10.1016/1054-139x(93)90143-d. [DOI] [PubMed] [Google Scholar]
- Cappelli M, MacDonald N E, McGrath P J. Assessment of readiness to transfer to adult care for adolescents with cystic fibrosis. Child Health Care. 1989;18:218–224. doi: 10.1207/s15326888chc1804_4. [DOI] [PubMed] [Google Scholar]
- Cohen L, La Greca A M, Blount R, Kazak A, Holmbeck G N, Lemanek K L. Introduction to special issue: Evidence-based assessment in pediatric psychology. Journal of Pediatric Psychology. 2008;33:911–915. doi: 10.1093/jpepsy/jsj115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colver A F, Merrick H, Deverill, Le Couteur A, Parr J, Pearce M S, Rapley T, Vale L, Watson R, McConachie H, on behalf of the Transition Collaborative Group Study protocol: Longitudinal study of the transition of young people with complex health needs from child to adult health services. Biomedical Central Public Health. 2013;13:1–11. doi: 10.1186/1471-2458-13-675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Committee on Developments in the Science of Learning. How people learn: Brain, mind, experience, and school. Washington, DC: National Academies Press; 2000. [Google Scholar]
- Dudman L, Rapley P, Wilson S. Development of a transition readiness scale for young adults with cystic fibrosis: Face and content validity. Neonatal, Paediatric, and Child Health Nursing. 2011;14:9–13. [Google Scholar]
- Erickson E. Childhood and society. 2nd ed. New York, NY: Norton; 1963. [Google Scholar]
- Ferris M, Harward D, Bickford K, Layton J, Ferris M, Hogan S, Gipson D S, McCoy L P, Hooper S. A clinical tool to measure the components of health-care transition from pediatric care to adult care: The UNC TRxANSITION Scale. Renal Failure. 2012;34:744–753. doi: 10.3109/0886022X.2012.678171. [DOI] [PubMed] [Google Scholar]
- Fredericks E, Dore-Stites D, Well A, Magee J, Freed G, Shieck V, Lopez M. Assessment of transition readiness skills and adherence in pediatric liver transplant recipients. Pediatric Transplantation. 2010;14:944–953. doi: 10.1111/j.1399-3046.2010.01349.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrest C, Bevans K, Tucker C, Riley A, Ravens-Sieberer U, Gardner W, Pajer K. Commentary: The Patient-Reported Outcome Measurement Information System (PROMIS®) for children and youth: application to pediatric psychology. Pediatr Psychol. 2012;37:614–621. doi: 10.1093/jpepsy/jss038. doi:10.1093/jpepsy/jss038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilleland J, Amaral S, Mee L, Blount R. Getting ready to leave: Transition readiness in adolescent kidney transplant recipients. Journal of Pediatric Psychology. 2012;37:85–96. doi: 10.1093/jpepsy/jsr049. [DOI] [PubMed] [Google Scholar]
- Gilleland J, Lee J, Vangile K, Schilling LH, Record B, Wasilewski-Masker K, Mertens AC. Assessment of transition readiness among survivors of childhood cancer. 2013. Paper presented at the The National Conference in Pediatric Psychology, New Orleans, LA. [Google Scholar]
- Gurvitz M, Inkelas M, Lee M, Stout K, Escarce J, Chang R. Changes in hospitalization patterns among patients with congenital heart disease during the transition from adolescence to adulthood. Journal of The American College of Cardiology. 2007;49:875–882. doi: 10.1016/j.jacc.2006.09.051. [DOI] [PubMed] [Google Scholar]
- Hamdani Y, Jetha A, Norman C. Systems thinking perspectives applied to healthcare transition for youth with disabilities: A paradigm shift for practice, policy, and research. Child: Care, Health and Development. 2011;37:806–814. doi: 10.1111/j.1365-2214.2011.01313.x. [DOI] [PubMed] [Google Scholar]
- Holmbeck G N, Devine K A. Psychosocial and family functioning in spina bifida. Developmental Disabilities Research Reviews. 2010;16:40–46. doi: 10.1002/ddrr.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmbeck G N, Thill A W, Bachanas P, Garber J, Miller K B, Abad M, Bruno E F, Carter J S, David-Ferdon C, Jandasek B, Mennuti-Washburn J E, O'Mahar K, Zukerman J. Evidence-based assessment in pediatric psychology: Measures of psychosocial adjustment and psychopathology. Journal of Pediatric Psychology. 2008;33:958–980. doi: 10.1093/jpepsy/jsm059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes-Walker D J, Llewellyn A C, Farrell K. A transition care programme which improves diabetes control and reduces hospital admission rates in young adults with Type 1 diabetes aged 15-25. Diabetic Medicine. 2007;24:764–769. doi: 10.1111/j.1464-5491.2007.02152.x. [DOI] [PubMed] [Google Scholar]
- Lawson E F, Hersh A O, Applebaum M A, Yelin E H, Okumura M J, von Scheven E. Self-management skills in adolescents with chronic rheumatic disesase: A cross-sectional survey. Pediatric Rheumatology. 2011;9:1–7. doi: 10.1186/1546-0096-9-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman D G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- Orem D. Nursing: Concepts of practice. 5th ed. St. Louis, MO: Mosby; 1995. [Google Scholar]
- Palermo T M, Long A M, Lewandowski A S, Drotar D, Quittner A L, Walker L S. Evidence-based assessment of health-related quality of life and functional impairment in pediatric psychology. Journal of Pediatric Psychology. 2008;33:983–996. doi: 10.1093/jpepsy/jsn038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piaget J, Inhelder B. The psychology of the child. New York, NY: Basic Books; 1969. [Google Scholar]
- Prochaska J, DeClemente C. Toward a comprehensive, transtheoretical model of change: Stages of change and addictive behaviors. In: Miller W, Heather N, editors. Treating addictive behaviors: Processes of change. New York, NY: Plenum Press; 1986. pp. 3–28. [Google Scholar]
- Reid G, Irvine M, McCrindle B, Sananes R, Ritvo P, Siu S, Webb G D. Prevalence and correlates of successful transfer from pediatric to adult health care among a cohort of young adults with complex congenital heart defects. Pediatrics. 2004;113(3 Pt 1):e197–e205. doi: 10.1542/peds.113.3.e197. [DOI] [PubMed] [Google Scholar]
- Rosen D S, Blum R W, Britto M, Sawyer S M, Siegel D M. Transition to adult health care for adolescents and young adults with chronic conditions: Position paper of the Society for Adolescent Medicine. Journal of Adolescent Health. 2003;33:309–311. doi: 10.1016/s1054-139x(03)00208-8. [DOI] [PubMed] [Google Scholar]
- Ryan R, Deci E. Testing a self-determiniation theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist. 2000;55:68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- Sawicki G S, Lukens-Bull K, Yin X, Demars N, Huang I, Livingood W, Reiss J, Wood D. Measuring the transition readiness of youth with special healthcare needs: Validation of the TRAQ—Transition Readiness Assessment Questionnaire. Journal of Pediatric Psychology. 2011;36:160–171. doi: 10.1093/jpepsy/jsp128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz L A, Brumley L D, Tuchman L K, Barakat L P, Hobbie W L, Ginsberg J P, Daniel L C, Kazak A E, Bevans K, Deatrick J A. Stakeholder validation of a model of readiness for transition to adult care. JAMA Pediatric. 2013;67:939–946. doi: 10.1001/jamapediatrics.2013.2223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz L A, Butler E S, Brumley L D, Barakat L P, Deatrick J A, Hobbie W L, Ginsberg JP, Bevans K, Kazak AE, Tuchman LK, Tuchman L K. Using theory and PROMIS methods to develop the Transition Readiness Inventory (TRI) for adolescent and young adult survivors of childhood cancer. 2014. Paper presented at the Society of Pediatric Psychology Annual Conference, Philadelphia, PA. [Google Scholar]
- Schwartz L A, Tuchman L K, Hobbie W, Ginsberg J. A social-ecological model of readiness for transition to adult-oriented care for adolescents and young adults with chronic health conditions. Child: Care, Health and Development. 2011;37:883–895. doi: 10.1111/j.1365-2214.2011.01282.x. [DOI] [PubMed] [Google Scholar]
- Smith G M, Lewis V R, Whitworth E, Gold D T, Thornburg C D. Growing up with sickle cell disease: A pilot study of a transition program for adolescents with sickle cell disease. Clinical and Laboratory Observations. 2011;33:379–382. doi: 10.1097/MPH.0b013e318211bb2e. [DOI] [PubMed] [Google Scholar]
- Spring B. Evidence-based practice in clinical psychology: What it is, why it matters; what you need to know. Journal of Clinical Psychology. 2007;63:611–631. doi: 10.1002/jclp.20373. [DOI] [PubMed] [Google Scholar]
- Stinson J, Kohut S, Spiegel L, White M, Gill N, Colbourne G, Sigurdson S, Duffy K W, Tucker L, Stringer E, Hazel B, Hochman J, Reiss J, Kaufman M. A systematic review of transition readiness and transfer satisfaction measures for adolescents with chronic illness. International Journal of Adolescent Medicine and Health. 2013;6:1–16. doi: 10.1515/ijamh-2013-0512. [DOI] [PubMed] [Google Scholar]
- Telfair J, Alexander L, Loosier P, Alleman-Velez P, Simmons J. Providers' perspectives and beliefs regarding transition to adult care for adolescents with sickle cell disease. Journal of Health Care for the Poor and Underserved. 2004;15:443–461. doi: 10.1353/hpu.2004.0049. [DOI] [PubMed] [Google Scholar]
- Telfair J, DeBaun M. Transition and Sickle cell disease. Pediatrics. 2012;130:926–935. doi: 10.1542/peds.2011-3049. [DOI] [PubMed] [Google Scholar]
- Telfair J, Myers J, Drezner S. Transfer as a component of the transition of adolescents with Sickle cell disease to adult care: Adolescent, adult and parent perspectives. Journal of Adolescent Health. 1994;15:558–565. doi: 10.1016/1054-139x(94)90139-t. [DOI] [PubMed] [Google Scholar]
- Tuchman L, Slap G, Britto M. Transition to adult care: Experiences and expectations of adolescents with a chronic illness. Child: Care, Health and Development. 2008;34:557–563. doi: 10.1111/j.1365-2214.2008.00844.x. [DOI] [PubMed] [Google Scholar]
- Van Staa A, Jedeloo S, van Meeteren J, Latour J M. Crossing the transition chasm: Experiences and recommendations for improving transitional care of young adults, parents, and providers. Child: Care, Health and Development. 2011;37:821–832. doi: 10.1111/j.1365-2214.2011.01261.x. [DOI] [PubMed] [Google Scholar]
- Westwood A T R, Henly L D, Willcox P. Transition from paediatric to adult care for persons with cystic fibrosis: Patient and parent perspectives. Journal of Paediatric Child Health. 1999;35:442–445. doi: 10.1046/j.1440-1754.1999.355394.x. [DOI] [PubMed] [Google Scholar]
- White P H. Access to health care: Health insurance considerations for young adults with special health care needs/disabilities. Pediatrics. 2002;110:1328–1335. [PubMed] [Google Scholar]
- Wiener L S, Zobel M, Battles H, Ryder C. Transition from a pediatric HIV intramural clinical research program to adolescent and adult community-based care services: Assessing transition readiness. Social Work in Health Care. 2007;46:1–19. doi: 10.1300/J010v46n02_01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams R G. Fumbling the handoff: Managing the transition to adult care for adolescents with chronic conditions. Journal of Adolescent Health. 2009;44:307–308. doi: 10.1016/j.jadohealth.2009.01.001. [DOI] [PubMed] [Google Scholar]
- Williams T, Sherman E, Dunseith C, Mah JK, Blackman M, Latter J, Mahamed I, Slick D J, Thornton N. Measurement of medical self-management and transition readiness among Canadian adolescents with special healthcare needs. International Journal of Child and Adolescent Health. 2010;3:527–535. [Google Scholar]
- Wood D, Sawicki GS, Reiss J, Livingood W. Transition readiness assessment questionnaire 5.0. 2012. Unpublished instrument. Retrieved from www.hscj.ufl.edu/jaxhats/ [Google Scholar]
- Zhang L, Ho J, Kennedy S. A systematic review of the psychometric properties of transition readiness assessment tools in adolescents with chronic disease. BMC Pediatrics. 2014;14:4. doi: 10.1186/1471-2431-14-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman G L, Olsen C G, Bosworth M F. A “stages of change” approach to helping patients change behavior. American Family Physician. 2000;61:1409–1416. [PubMed] [Google Scholar]