Abstract
Background:
Some health problems are more prevalent in shift workers than day workers. Musculoskeletal disorders are considered as one of the most common health-related problems that can cause disability among health care workers. The aim of this study was to assess the associations between shift working and the prevalence of musculoskeletal symptoms (MSs) among nursing personnel.
Materials and Methods:
This study was conducted among 454 health care workers including nurses and nurses’ aides in a general hospital in Iran. A Nordic musculoskeletal questionnaire was used to evaluate the prevalence of MSs. Logistic regression analysis with adjusting for confounding factors was performed to evaluate the associations between shift working and the prevalence of MSs.
Results:
Lower back, knees, and upper back symptoms with the prevalence of 57.4%, 48.4%, and 47%, respectively, were the most common MSs. The prevalence of MSs in eight regions of the body (lower back, neck, knees, upper back, shoulder, wrist, buttock, and ankle) was higher among shift workers than day workers. The differences were statistically significant only in the lower back and ankle regions (P < 0.05). Odds Ratio for lower back symptoms in shift workers was 1.94 compared to day workers (P = 0.003).
Conclusion:
Findings of this study suggested that shift working could be associated with increased prevalence of lower back disorders among nursing personnel. This study emphasizes on the importance of proper work planning and regulating working hours for nursing personnel.
Keywords: Health personnel, Iran, musculoskeletal pain, nurses, nurses’ aides, work
INTRODUCTION
Nurses comprise 40% of all hospital staff averagely.[1] Nursing personnel work at rotating and night shifts usually. There are about 1 million nurses working in Japan and 75% of them have night shifts in their work schedule.[2] Intensive activity of nurses in different morning, afternoon, and night shifts and irregular sleep–wake patterns can decrease their work efficiency.[3] Nurses working at night shifts are encountered with higher rates of work-related accidents, errors, and burnouts, compared to nurses working in morning shifts.[4] Physical and mental health level of rotating shift work nurses is less than favorable compared to fixed shift work nurses.[5] The relationship between shift work and health problems such as psychological, gastrointestinal problems, and cardiovascular events, car accidents, and adverse pregnancy outcomes has been shown previously. Moreover, shift work nurses have poor behavioral health including smoking, more drug consumption, alcohol abuse, and low physical activity.[6]
On the other hand, musculoskeletal disorders (MSDs) are considered as the second leading cause of short-term sickness absence (less than 2 weeks).[7] In the US and Canada, 3.1% and 4.2% of gross national domestic product is spent for indirect costs of MSDs, respectively.[8] In the US, billions of dollars are spent annually on diagnostic and therapeutic procedures related to these disorders.[9] Results of a study revealed that 21.6% of sick leave taken by nurses was due to low back pain.[10] Also, in the same study, back injuries were considered as one of the leading causes of pain, discomfort, disability, and sickness absence among nurses.[10] Studies indicated that MSDs is prevalent in nurses. Barzideh et al., in a cross-sectional study on 385 randomly selected Iranian nurses, investigated job stress dimensions and their relationship to MSDs. In their study, past 12-month incidence of lower back symptoms was reported as 61.8%.[11] Choobineh et al., in their study conducted among operating room nurses of Shiraz city hospitals in Iran, reported that lower back, ankles/feet, and knee disorders were the most common MSDs.[12]
Although some studies were conducted about the effects of shift working on MSDs, the findings are controversial.[6] The aim of our study was to investigate the associations between shift working and the prevalence of musculoskeletal symptoms (MSs) among nursing personnel.
MATERIALS AND METHODS
Study population and design
This was a cross-sectional study of nursing personnel of a general hospital in Tehran, Iran in 2011. All nursing personnel of the hospital, including nurses and nurses’ aides who had at least 1 year of work experience in the present position, were invited to participate in this study. Six hundred and fifty participants who satisfied the criteria and signed the informed consent were enrolled in the study. Subjects with history of MSDs caused by trauma or rheumatologic disorders and those with incomplete required data were excluded from the study. The questionnaires were anonymous and personal information was kept secure in all stages of the study. This study was approved by the Ethics Committee of Tehran University of Medical Sciences.
Data collection
Required data were collected through a questionnaire comprising some sections including demographic and occupational characteristics added to the Nordic musculoskeletal questionnaire. Nordic questionnaire is applied as a standard tool in epidemiological studies to evaluate the prevalence of MSDs.[13] Subjects answered the question “Have MSs in any part of the body disrupted your daily activities (like occupational and entertainment activities or working at home) during the past 12 months?” (MSs include pain, tingling sensation, numbness, and stiffness, or limitation in movement that causes disruption in daily activities). Mentioned body parts also were shown on the body map. Subjects answered this question about their work schedule: “What was your work schedule often during the past year (day work or shift work)?” Working at any time other than normal daylight hours was considered as shift work.[14] Fixed morning or afternoon shifts were considered as day work schedule. Rotating and fixed nighttime work was considered as shift work schedule. The morning shift started at 07:00 h and continued till 14:00 h, the evening shift started at 14:00 h and continued till 20:00 h, and the night shift started from 20:00 h which went on till 07:00 h. All rotating shift workers worked continuously (including weekends) 2 days in the morning shift, 2 days in the evening shift, and 2 days in the night shift, with days of rest after the night shift.
Five questions were used to identify the physical demands. The questions were regarding “moving/lifting very heavy loads,” “long periods of body awkward positions,” “lifting or lowering patient/objects to/from the floor,” “working while bent or twisted at waist,” and “standing in one place/static position (more than 30 min).” Each item was scored using a 4-point scale (“never” to “always”). Responses were dichotomized [one and two (to zero) vs. three and four (to one)]. Zero was considered as low and one considered as high physical demand in each item.
Other data collected were age, gender, height and weight [for calculating the body mass index (BMI)], smoking habits, past medical history, educational level, work experience, etc.
Statistical analysis
Mean, standard deviation (SD), and range of quantitative variables were calculated. Chi-square test and t-test were used to compare the variables. Logistic regression analysis adjusting for confounding factors was used to investigate the associations between study variables and the prevalence of MSDs more precisely. For regression analysis, quantitative variables were dichotomized based on the median. Smoking habits were classified into two categories: smoker and nonsmoker. Exercise was classified into three categories: regular, irregular, and no exercise. P values less than 0.05 were considered statistically significant. The results of statistical analysis were reported as Odds Ratio (OR) with 95% confidence intervals (95% CI). All the mentioned calculations were performed using SPSS 13 software.
RESULTS
Of the 650 questionnaires given to nursing personnel, 524 were returned (the response rate was 80.6%). Based on the exclusion criteria, 70 questionnaires were excluded and finally 454 questionnaires (69.8%) were analyzed.
Seventy-six percent of the study nursing personnel were women and 24% were men. The mean age of the studied sample was 32.2 ± 6.1 (range = 20–55) years and the mean work experience of them was 8.5 ± 3.8 (range = 1–30) years. The mean BMI was 24.2 ± 4 (range = 15.1–42.8) kg/m2. One hundred sixty-two (35.7%) nursing personnel were day workers and 292 (64.3%) were shift workers. Among the shift workers, 36 (8%) were fixed night workers and 256 (56.3%) were rotating shift workers. Table 1 shows the demographic and occupational characteristics of the studied groups (day workers and shift workers). There were no statistically significant differences in the demographic and occupational characteristics between groups (P > 0.05), except in their education level (P < 0.05).
Table 1.
Demographic and occupational characteristics of nursing personnel in the study groups
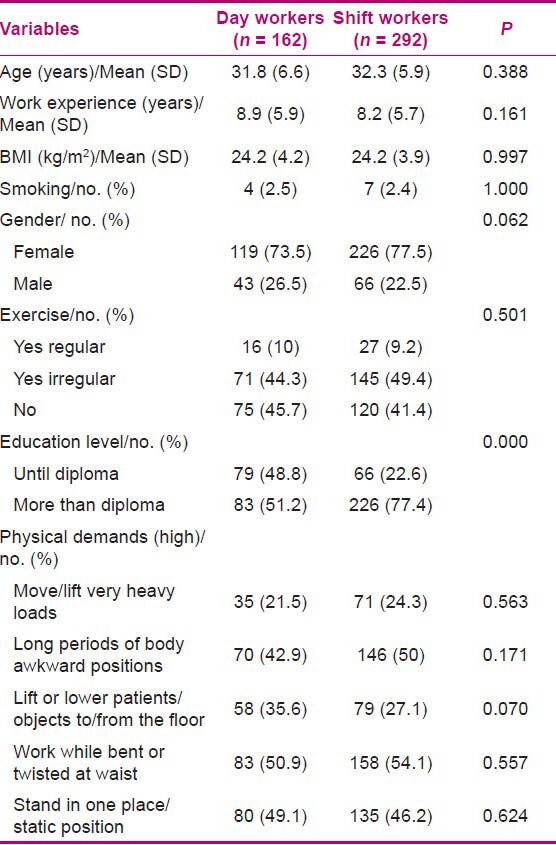
Table 2 shows the prevalence of MSs in the studied sample. Lower back, knees, and upper back symptoms with the prevalence of 57.4%, 48.4%, and 47%, respectively, were the most common MSs. Although the prevalence of MSs in shift workers was higher than in day workers in the lower back, knees, upper back, neck, shoulder, wrist, ankle, and buttock regions, only in the lower back and ankle regions, the differences were statistically significant (P < 0.05). Prevalence of low back symptoms was 48.5% in day workers and 62.3% in shift workers (P = 0.006), and prevalence of ankle symptoms was 26.4% in day workers and 36.0% in shift workers (P = 0.038).
Table 2.
Prevalence of MSs in different body regions of the nursing personnel during the past 12 months
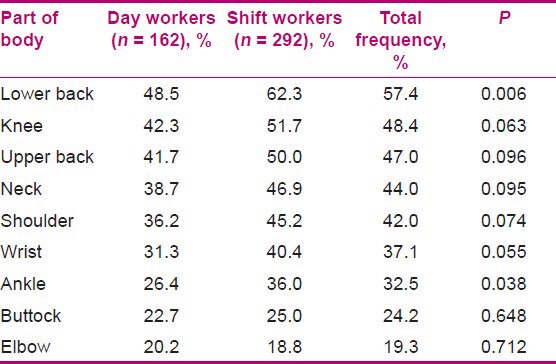
Table 3 shows the results of logistic regression analysis with adjusting for confounding factors. There were significant associations between the prevalence of low back symptoms and shift working (P < 0.05). OR for low back symptoms in shift workers was 1.94 compared to day workers (P = 0.003).
Table 3.
Association between prevalence of low back symptoms and study variables using logistic regression analysis
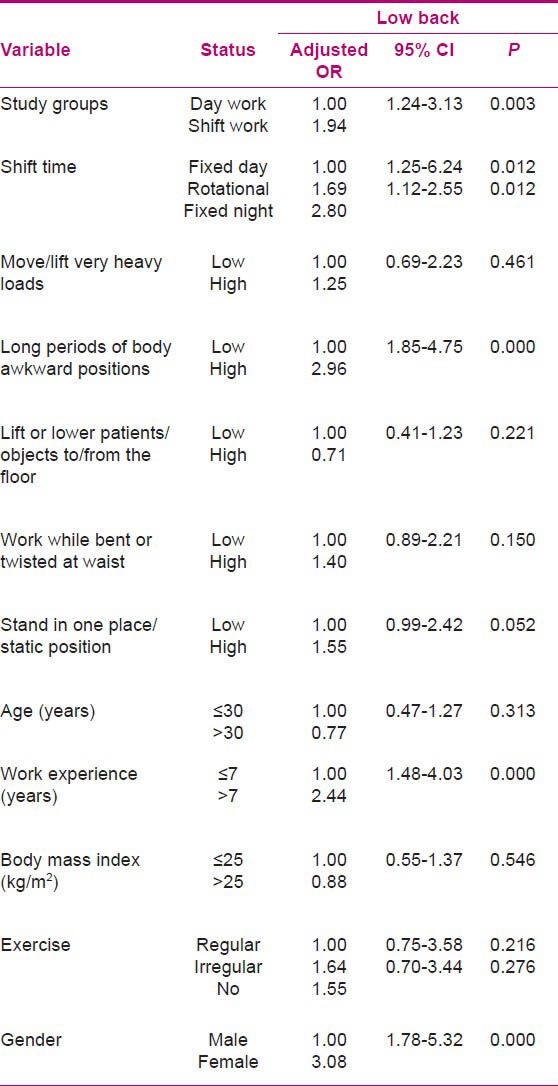
In this study, work experience more than 7 years and female gender were associated with low back symptoms (P < 0.05). Between the items related to physical demands, only “long periods of body awkward positions” was associated with low back symptoms (P = 0.000). There were no significant associations between age, smoking, BMI, and exercise with low back symptoms (P > 0.05).
DISCUSSION
Shift working is one among the risk factors of health-related problems in the work environments. Some studies showed that health problems were more prevalent in shift workers than in day workers.[15] Choobineh et al., in a cross-sectional study on 1203 petrochemical industry workers, found that prevalence of gastrointestinal and musculoskeletal disorders was more in shift workers than in day workers.[15] MSDs are considered as one of the most common health-related problems that can cause disability among health care workers.[16]
In our study, prevalence of low back and ankle symptoms was significantly higher among shift workers compared to fixed day workers. A prospective study by Eriksson et al. on the occupational risk factors of severe low back pain among nurses’ aides showed that low back pain was associated with heavy lifting, moderate work demands, loss of support in workplace, working in nursing homes, and working in night shifts.[17] In a study that was performed among Japanese home care nurses, it was found that after taking a nap for every two night shifts, pain in the arm and leg was reduced significantly.[18]
Angersbach et al. compared the prevalence of different diseases between day workers and shift workers in a retrospective cohort study in an industrial factory. They reported that the prevalence of MSDs following injuries in shift workers was higher than in day workers.[19] Ottoman et al. compared MSDs, autonomic symptoms, appetite disorders, and respiratory infections as the markers of health status among day and shift work polices. In this study, age and shift working were reported as the major risk factors associated with these disorders.[20] In contrast, in our study, the prevalence of MSDs in ages less than 30 years was higher than in ages more than 30 years, but the difference was not statistically significant. It may be because of the heavier tasks of younger nurses.
In a study that was conducted among 1462 workers in the petroleum industry, Parks suggested that shift working accompanied by type of job could be an important predictor of health-related disorders such as headache, MSDs, sleep disorders, and gastrointestinal disturbances.[21] In a review conducted by Caruso and Waters on 23 studies that were related to the association between work schedule and MSDs, with an emphasis on the health care sector, 4 studies with control on physical demands reported no association between shift work and MSDs, while 8 studies found excessive working hours may be associated with increased prevalence of MSDs. Other studies in this review had reported either conflicting results or had been in such a way that their methodologies were not comparable.[6]
In our study, the OR for low back symptoms in fixed night workers compared to fixed day workers was higher than in rotating shift workers compared to fixed day workers. It may be because of continuous lack of night sleep that can cause circadian cycle disturbance. Sveinsdóttir, in a study to investigate the association between the disruption of the circadian cycle caused by shift work and some adverse health effects, reported that nurses working rotating day/evening shifts experienced more severe gastrointestinal and MSs, when compared with nurses working in other shift schedules.[22] They related these findings to the short rest period provided between evening and morning shifts.[22]
In our study, lower back, knees, and upper back symptoms with the prevalence of 57.4%, 48.4%, and 47%, respectively, were the most common MSs. Choobineh et al., in their study conducted in operating room nurses of Shiraz city hospitals in Iran, reported that lower back, ankles/feet, and knee disorders with prevalence of 60.6%, 59%, and 58.1%, respectively, were the most common MSDs.[12] Also, in another study that was conducted by Choobineh et al. among hospital nurses, low back symptoms were the most common MSDs.[23] Dereket al., in a 1-year review of MSDs’ risk factors among 1162 Japanese nurses, found that the prevalence of symptoms in shoulder, low back, neck, and back was 71.9%, 71.3%, 54.71%, and 33.9%, respectively.[24] In a study by Trinkoff et al., the prevalence of low back, neck, and shoulder disorder among 1163 nurses was reported to be 47%, 45.8%, and 35.1%, respectively.[25] In Trinkoff's study, the nurses were considered MSD positive if they had relevant symptoms lasting at least 1 week or occurring at least monthly in the past year, while in our study, the nurses were considered MSD positive if they had symptoms that disturbed their routine functions even once in the past year.
In our study, between the physical items, only “long periods of body awkward positions” was associated with low back symptoms. Vandergrift et al., in a cohort of automobile manufacturing workers, found that awkward back posture and hand force were associated with an increased risk of both prevalence and 1-year incidence of low back pain.[26] Moreover, the results of our study indicated that workers with higher work experiences and female workers were more prone to be affected by low back disorders. In 2006, the research team of the occupational research national agency in America declared after many surveys that the field of relationship between MSDs and long working hours should be given priority in future researches.[27] In a study conducted on nurses by Lipscomb et al., working more than 12 h a day, 40 h per week, and working on holidays were associated with an increase in the prevalence of MSDs in three areas of the body, including neck, shoulder, and low back.[28] Frederickson et al. conducted a 24-year follow-up study to evaluate the risk factors of neck and upper limp disorders among 484 Swedish workers of different fields. They concluded that neck disorder among women was associated with long working hours, high psychological workload, and imbalance in working hours.[29]
In our study, BMI was not associated with back symptoms. Leroux et al., in a study on neck–shoulder symptoms among white-collar workers, found no association between BMI and symptoms.[30] But in another study by Trinkoff et al. on nurses, back and shoulder symptoms were associated with BMI, but such an association was not found in neck symptoms.[31]
In this study, the prevalence of low back symptoms in nurses with no exercise or irregular exercise was more common than in nurses with regular exercise. But the difference was not statistically significant. In the study of Trinkoff et al. on nurses, exercise and back symptoms were associated.[31]
Because of the less number of smokers, we did not find an association between smoking and MSDs.
The cross-sectional study design and the collection of data by self-report were the limitations of our study. The cross-sectional design limits the application of causal inference and self-report may reflect denial, deception, or difficulty in the recall. In order to find the exact relationship between MSs and shift working, prospective studies need to be conducted.
CONCLUSION
The findings of this study suggested that shift working may be associated with increased prevalence of low back symptoms among nursing personnel. This study emphasizes on the importance of proper work planning and regulating the working hours in order to reduce the prevalence of MSDs in nursing personnel and considering such disorders in the occupational checkups. Also, shift workers should be given priority in medical screening programs. However, more prospective studies with stronger control on confounders are needed to confirm this association.
ACKNOWLEDGMENTS
The authors would like to thank the nursing personnel of the hospitals under investigation. This study was conducted with the financial support of the Tehran University of Medical Sciences.
Footnotes
Source of Support: This study was conducted with the financial support of the Tehran University of Medical Sciences
Conflict of Interest: Nil.
REFERENCES
- 1.Sulivan E, Decker P. New York: Wesley; 1992. Effective management in nursing. [Google Scholar]
- 2.Ohida T, Kamal A, Sone T, Ishii T, Uchiyama M, Minowa M, et al. Night-shift work related problems in young female nurses in Japan. J Occup Health. 2001;43:150–6. [Google Scholar]
- 3.Jebreily M. Survey of the sleep deprivation on quality of nurses’ work and its solution plans. Iran J Med Sci. 2004;3:6–4. [Google Scholar]
- 4.Salemy S. Tehran: Publishing Salmy; 2007. Basic nursing theory and practice; pp. 14–28. [Google Scholar]
- 5.Erin C, Kristin A. Shift working and well-being: Physiological and psychological analysis of shift workers. Am J Undergrad Res. 2003;71:1–5. [Google Scholar]
- 6.Caruso CC, Waters TR. A review of work schedule issues and musculoskeletal disorders with an emphasis on the healthcare sector. Ind Health. 2008;46:523–34. doi: 10.2486/indhealth.46.523. [DOI] [PubMed] [Google Scholar]
- 7.Stansfeld SA, North FM, White I, Marmot MG. Work characteristics and psychiatric disorder in civil servants in London. J Epidemiol Community Health. 1995;49:48–53. doi: 10.1136/jech.49.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health Organ. 2003;81:646–56. [PMC free article] [PubMed] [Google Scholar]
- 9.Gatchel RJ. Musculoskeletal disorders: Primary and secondary interventions. J Electromyogr Kinesiol. 2004;14:161–70. doi: 10.1016/j.jelekin.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 10.Yip Y. A study of work stress, patient handling activities and the risk of low back pain among nurses in Hong Kong. J Adv Nurs. 2001;36:794–804. doi: 10.1046/j.1365-2648.2001.02037.x. [DOI] [PubMed] [Google Scholar]
- 11.Barzideh M, Choobineh AR, Tabatabaee HR. Job stress dimensions and their relationship to musculoskeletal disorders in Iranian nurses. Work. 2013 doi: 10.3233/WOR-121585. [In Press] [DOI] [PubMed] [Google Scholar]
- 12.Choobineh A, Movahed M, Tabatabaie SH, Kumashiro M. Perceived demands and musculoskeletal disorders in operating room nurses of Shiraz city hospitals. Industrial Health. 2010;48:74–84. doi: 10.2486/indhealth.48.74. [DOI] [PubMed] [Google Scholar]
- 13.Palmer K, Smith G, Kellingray S, Cooper C. Repeatability and validity of an upper limb and neck discomfort questionnaire: The utility of the standardized Nordic questionnaire. Occup Med (Lond) 1999;49:171–5. doi: 10.1093/occmed/49.3.171. [DOI] [PubMed] [Google Scholar]
- 14.Rom WN. New York: Lippincott; 2007. Environmental and occupational medicine. [Google Scholar]
- 15.Choobineh A, Soltanzadeh A, Tabatabaee H, Jahangiri M, Khavaji S. Health effects associated with shift work in 12-hour shift schedule among Iranian petrochemical employees. Int J Occup Saf Ergon. 2012;18:419–27. doi: 10.1080/10803548.2012.11076937. [DOI] [PubMed] [Google Scholar]
- 16.Smith DR, Kondo N, Tanaka E, Tanaka H, Hirasawa K, Yamagata Z. Musculoskeletal disorders among hospital nurses in rural Japan. Rural Remote Health. 2003;3:241. [PubMed] [Google Scholar]
- 17.Eriksen W, Bruusgaard D, Knardahl S. Work factors as predictors of intense or disabling low back pain; a prospective study of nurses’ aides. Occup Environ Med. 2004;61:398–404. doi: 10.1136/oem.2003.008482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Takahashi M, Iwakiri K, Sotoyama M, Hirata M, Hisanaga N. Musculoskeletal pain and night-shift naps in nursing home care workers. Occup Med (Lond) 2009;59:197–200. doi: 10.1093/occmed/kqp029. [DOI] [PubMed] [Google Scholar]
- 19.Angersbach D, Knauth P, Loskant H, Karvonen MJ, Undeutsch K, Rutenfranz J. A retrospective cohort study comparing complaints and diseases in day and shift workers. Int Arch Occup Environ Health. 1980;45:127–40. doi: 10.1007/BF01274132. [DOI] [PubMed] [Google Scholar]
- 20.Ottmann W, Karvonen MJ, Schmidt KH, Knauth P, Rutenfranz J. Subjective health status of day and shift-working policemen. Ergonomics. 1989;32:847–54. doi: 10.1080/00140138908966847. [DOI] [PubMed] [Google Scholar]
- 21.Parkes KR. Shiftwork, Job type, and the work environment as joint predictors of health-related outcomes. J Occup Health Psychol. 1999;4:256–68. doi: 10.1037//1076-8998.4.3.256. [DOI] [PubMed] [Google Scholar]
- 22.Sveinsdottir H. Self-assessed quality of sleep, occupational health, working environment, illness experience and job satisfaction of female nurses working different combination of shifts. Scand J Caring Sci. 2006;20:229–37. doi: 10.1111/j.1471-6712.2006.00402.x. [DOI] [PubMed] [Google Scholar]
- 23.Choobineh A, Rajaeefard A, Neghab M. Association between perceived demands and musculoskeletal disorders among hospital nurses of Shiraz University of Medical Sciences: A questionnaire survey. Int J Occup Saf Ergon. 2006;12:409–16. doi: 10.1080/10803548.2006.11076699. [DOI] [PubMed] [Google Scholar]
- 24.Smith DR, Mihashi M, Adachi Y, Koga H, Ishitake T. A detailed analysis of musculoskeletal disorder risk factors among Japanese nurses. J Safety Res. 2006;37:195–200. doi: 10.1016/j.jsr.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 25.Trinkoff AM, Lipscomb JA, Geiger-Brown J, Brady B. Musculoskeletal problems of the neck, shoulder, and back and functional consequences in nurses. Am J Ind Med. 2002;41:170–8. doi: 10.1002/ajim.10048. [DOI] [PubMed] [Google Scholar]
- 26.Vandergrift JL, Gold JE, Hanlon A, Punnett L. Physical and psychosocial ergonomic risk factors for low back pain in automobile manufacturing workers. Occup Environ Med. 2012;69:29–34. doi: 10.1136/oem.2010.061770. [DOI] [PubMed] [Google Scholar]
- 27.Caruso CC, Bushnell T, Eggerth D, Heitmann A, Kojola B, Newman K, et al. Long working hours, safety, and health: Toward a National Research Agenda. Am J Ind Med. 2006;49:930–42. doi: 10.1002/ajim.20373. [DOI] [PubMed] [Google Scholar]
- 28.Lipscomb JA, Trinkoff AM, Geiger-Brown J, Brady B. Work-schedule characteristics and reported musculoskeletal disorders of registered nurses. Scand J Work Environ Health. 2002;28:394–401. doi: 10.5271/sjweh.691. [DOI] [PubMed] [Google Scholar]
- 29.Fredriksson K, Alfredsson L, Koster M, Thorbjornsson CB, Toomingas A, Torgen M, et al. Risk factors for neck and upper limb disorders: Results from 24 years of follow up. Occup Environ Med. 1999;56:59–66. doi: 10.1136/oem.56.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Leroux I, Brisson C, Montreuil S. Job strain and neck-shoulder symptoms: A prevalence study of women and men white collar workers. Occup Med (Lond) 2006;56:102–9. doi: 10.1093/occmed/kqj005. [DOI] [PubMed] [Google Scholar]
- 31.Trinkoff AM, Lipscomb JA, Geiger-Brown J, Storr CL, Brady BA. Perceived physical demands and reported musculoskeletal problems in registered nurses. Am J Prev Med. 2003;24:270–5. doi: 10.1016/s0749-3797(02)00639-6. [DOI] [PubMed] [Google Scholar]


