Abstract
Background:
Obstructive sleep apnea syndrome (OSAS) is a common sleep disorder characterized by repeated upper airway obstruction during sleep. While respiratory pauses followed by loud snoring and daytime sleepiness are the main symptoms of OSAS, the patients may complain from sleep disruption, headache, mood disturbance, irritability, and memory impairment. However, the association of sleep apnea with anxiety and depression is not completely understood. Adherence to continuous positive airway pressure (CPAP), the treatment of choice for OSAS, may be influenced by psychological conditions, especially claustrophobia. The aim of this study was to evaluate the association of OSAS with anxiety and depression symptoms. This study also investigated the association of anxiety with body mass index (BMI) and the severity of OSAS.
Materials and Methods:
We conducted a cross-sectional study on 178 adult individuals diagnosed with OSAS at the sleep laboratory between September 2008 and May 2012. The participants were interviewed according to a checklist regarding both their chief complaints and other associated symptoms. The psychological status was assessed according to Beck anxiety inventory (BAI) and Beck depression inventory (BDI) scoring. The severity of breathing disorder was classified as mild, moderate, and severe based on apnea–hypopnea index (AHI) which was ascertained by overnight polysomnography. Daytime sleepiness was assessed by Epworth sleepiness scale (ESS).
Results:
The mean (SD) age of participants was 50.33 years. In terms of sex, 85.5% of the study population were males and14.4% were females. We found no relation between sex and the symptoms of OSAS. Regarding the frequency of anxiety and depression symptoms, 53.9% of the individuals had some degree of anxiety, while 46.1% demonstrated depressive symptoms. In terms of OSAS severity, this study showed that OSAS severity was associated with the frequency of anxiety, chocking, and sleepiness (P : 0.001). According to polysomnographic results, we found that the majority of patients suffering from anxiety and chocking (66.7% and 71.4%, respectively) had severe OSAS, while only 23.1% of patients with sleepiness had severe OSAS.
Conclusion:
Our study showed that the frequency of anxiety in OSAS patients is higher than in the general population regardless of the gender. Furthermore, it is more likely that OSAS patients present with anxiety and depression than the typical symptoms.
Keywords: Anxiety, depression, obstructive sleep apnea syndrome
ABBREVIATIONS
AHI: apnea-hypopnea index
BAI: Beck anxiety inventory
BDI: Beck depression inventory
BMI: body mass index
CPAP: continuous positive airway pressure
EDS: excessive daytime sleepiness
EEG: electroencephalography
ESS: Epworth sleepiness scale
ICSD: International Classification of Sleep Disorders
OSAS: obstructive sleep apnea syndrome
RDI: respiratory disturbance index
INTRODUCTION
Obstructive sleep apnea syndrome (OSAS) is a common sleep-related breathing disorder with a prevalence of 2-4% among adults in the United States.[1] It is characterized by repeated episodes of partial or complete upper airway obstruction during sleep and is accompanied by intermittent hypoxemia, increased respiratory effort, and sleep disturbance. Obesity, age, and male gender are the most important risk factors for this syndrome. The main manifestations of this condition are respiratory pauses during sleep, followed by loud snorts and also excessive daytime sleepiness (EDS).[2] Patients may complain from a sensation of choking, difficulty in falling asleep at night,[3,4,5] morning headaches,[3,6,7] and nightmares.[8] OSAS may cause serious consequences including arterial and pulmonary hypertension,[9] cardiovascular diseases,[10] motor vehicle accidents,[11] impaired cognition, and psychiatric symptoms including depression, irritability, and anxiety.[12,13] While each of these conditions may significantly impair the quality of life,[14] many of the patients remain unrecognized with huge medical and economic burden on both themselves and the society.[3,15] The delay in diagnosis of OSAS has been partially attributed to the nature of this syndrome, as snoring and nocturnal respiratory pauses may not attract appropriate attention of sufferers. Hence, a better understanding of this condition, its complications, and the presenting symptoms is of great value.
According to International Classification of Sleep Disorders (ICSD-II) published by the American Academy of Sleep Medicine (AASM), OSAS is diagnosed with either a respiratory disturbance index (RDI) ≥15 irrespective of the presence of symptoms, or an RDI >5 accompanied by any of the following features: 1) sleep attacks, EDS, fatigue, or insomnia; 2) awakening with a chocking feeling; 3) loud snoring and/or breathing pauses reported by bed partner. RDI is ascertained by mean number of apneas + hypopneas + respiratory effort-related arousals per hour of sleep.[16] The standard laboratory technique for the diagnosis of sleep apnea is overnight polysomnography.[17] The treatment of choice for OSAS is continuous positive airway pressure (CPAP); however, the adherence to this device may be affected by psychiatric status, especially claustrophobia.[18]
Among the adverse consequences, an association between mood disturbances and anxiety disorder with OSAS has been shown in a large body of epidemiological studies.[19,20,21,22] Nonetheless, there are studies that show contrary results to such a correlation.[15,23] Moreover, overlapping symptoms like passivity and lack of initiation, loss of facial expression, and slowed psychomotor function, which may be noticed in both OSAS (as a result of diurnal drowsiness) and depression, may make it difficult to distinguish between these conditions.[13,23] Hence, further investigations in this area, particularly large-scale studies, are necessary to understand this relationship and the nature of these conditions. The purpose of this study is to determine the prevalence of depression and anxiety in patients diagnosed with OSAS. Also, this study investigated the association of depression and anxiety with body mass index (BMI), Epworth sleepiness scale (ESS), and the severity of OSAS in these patients.
MATERIALS AND METHODS
We conducted this cross-sectional study at the sleep laboratory of Ibn-e-Sina Hospital, Mashhad, Iran, from September 2008 to May 2012. We did polysomnography on the patients referred to this center during this period of time and 191 patients were diagnosed with OSAS. Incomplete and unreliable cases were removed from the study; hence, the data were gathered from 178 patients who were diagnosed with OSAS according to ICSD-II.[16] Prior to data collection, informed consent was obtained from each participant. The information regarding age, gender, weight, height, and medical history of the patients was gathered and analyzed, and unnecessary data were omitted. Detailed history of the presenting symptoms including snoring, daytime sleepiness, nocturnal chocking, nightmares, and headaches was taken by a neurologist. We also asked the patients to determine their chief complaint that made them seek for medical help. To assess the psychiatric status, the participants were asked to fill the Beck depression inventory (BDI-II) and the Beck anxiety inventory (BAI). The BDI-II (revised in 1996) is a self-report questionnaire consisting of 21 multiple-choice questions regarding depression symptoms.[24] BAI is also a self-report questionnaire consisting of 21 multiple-choice questions to evaluate the severity of anxiety symptoms. BDI, BAI, and their applicability have been validated in Iranian population.[25] According to Mental Health Research Centre, Tehran Psychiatric Institute, the Beck scores categorized the severity of anxiety and depression into four groups in following manner. BDI categories are normal (0-9), mild (10-15), moderate (16-23), and severe (24-63). Regarding the BAI, the categories are normal (0-7), mild (8-15), moderate (16-25), and severe (26-63).[26] Daytime sleepiness was assessed by employing the ESS, which constitutes eight questions regarding dozing in different passive situations. According to ESS, the chance of falling asleep in each situation is scored from 0 to 3. The sum of the responses provides a global ranking ranging from 0 to 24. The severity of daytime sleepiness is categorized into four groups: normal (0-8), mild (9-12), moderate (13-16), and severe (>16).[27] Insomnia was considered as difficulty to fall asleep or maintaining the sleep persistency.[28] To evaluate obesity, we determined the BMI, which is calculated as body weight in kilograms divided by the square of the height in meters.[29]
Then the participants underwent overnight polysomnography. Based on the Manual of AASM criteria, sleep apneas were ascertained as ≥10 seconds of air flow pauses.[16] A 50% decrement in the amplitude of baseline airflow followed by ≥3% of oxygen desaturation/or electroencephalography (EEG) recorded arousal was considered as hypopnea.[16] The severity of OSAS was determined by apnea-hypopnea index (AHI; mean number of apnea + hypopnea per hour of sleep). In this study, AHI was classified as mild (5-15), moderate (16-30), and severe (>30).[16]
Statistical analysis
The collected data were analyzed employing SPSS software (version 16). The correlations between variables were investigated using χ2 test, replaced by Fisher's exact test in the case of expected cell ≤5. The significance level was set at P ≤ 0.05.
RESULTS
According to this study, snoring was the most frequent symptom in patients suffering from OSAS (66.3%), followed by anxiety (53.9%) and then chocking (47.2%) and depression (46.1%) [Table 1]. This study also showed that among the chief complaints, insomnia was the most frequent symptom (20.2%) followed by anxiety and chocking (each one constituting 13.5%) [Figure 1]. Another finding of this study was the association between anxiety and chocking. This study showed that the incidence of chocking in patients suffering from anxiety was almost two times more than those without anxiety symptoms [odds ratio (OR): 2.03, confidence interval (CI): 1.11-3.7, P: 0.020].
Table 1.
The frequency of the main symptoms of OSAS in males, females, and total population
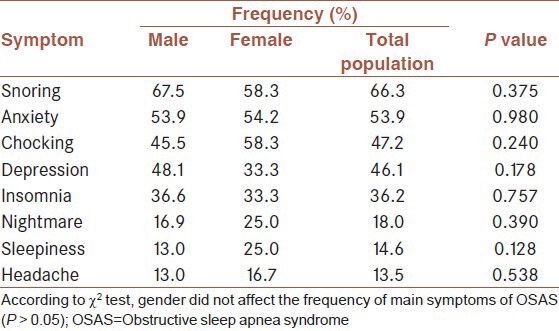
Figure 1.
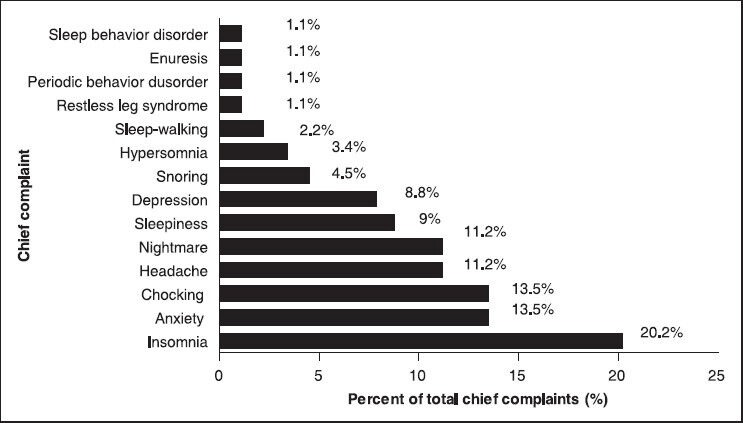
The incidences of the common chief complaints in patients with OSAS
Our study also compared the incidences of main OSAS symptoms in males and females [Table 1]. It showed that the incidence of anxiety was not associated with gender, which might be due to the abnormal distribution of males and females in the target population (males: 85.52%, females: 13.48%). In other words, we could not provide evidence showing a correlation between gender and any of the main symptoms of OSAS in these patients.
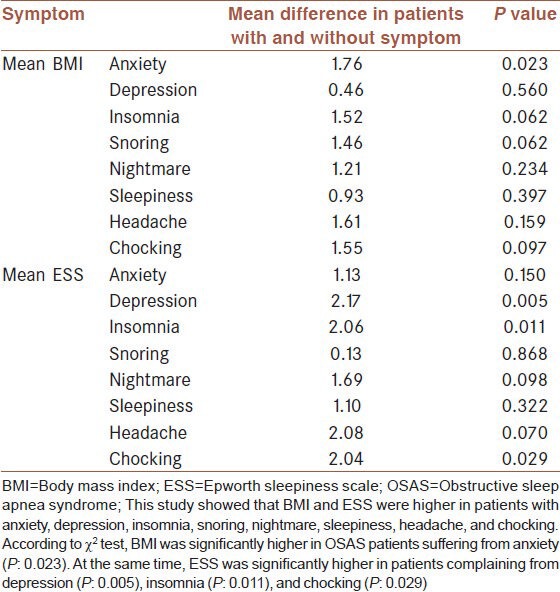
We also investigated the association of BMI and ESS with the frequency of OSAS main symptoms. The mean BMI and ESS were higher in OSAS patients with anxiety, depression, insomnia, snoring, nightmare, sleepiness, headache, and chocking [Table 2].
Table 2.
The association of main OSAS symptoms with BMI and ESS
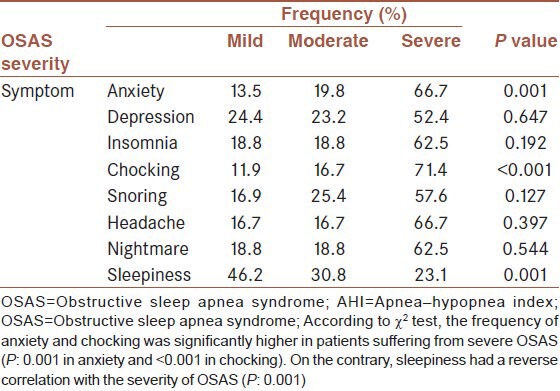
The association between the OSAS severity and its symptoms was also investigated. In terms of severity, OSAS was categorized into mild, moderate, and severe groups This study showed that anxiety (P: 0.001) and chocking (P < 0.001) were significantly more frequent among patients with severe OSAS; on the other hand, sleepiness was observed more in mild OSAS (P: 0.001). We did not find any evidence indicating an association between the severity of OSAS and incidence of depression, insomnia, snoring, headache, and nightmare [Table 3].
Table 3.
The association of the main symptoms of OSAS and its severity (assessed by AHI)
DISCUSSION
This is the first cross-sectional study in the Middle East area that examined the presenting features of OSAS in terms of chief complaints and other presenting complaints. According to this study, snoring was the most frequent symptom in our patients (66.3%), which is compatible with most of the previous studies.[9,15,22] However, it constituted only 4.5% of the chief complaints among our patients. At the same time, insomnia was the most prevalent chief complaint, while it was at the fifth position among the symptoms of OSAS. Hence, it can be concluded that insomnia, compared with snoring, more efficiently forces OSAS patients in Iran to ask for medical help. Anxiety was at the second position among both OSAS symptoms and chief complaints, followed by chocking. While the prevalence of depression, as a feature of OSAS, was almost similar to that of chocking, depression had a greater share as a chief complaint. Our study also showed that in spite of low prevalence of headaches and nightmares as symptoms of OSAS, they had a significant share as the chief complaints of OSAS patients. This study also showed that sleepiness was not a frequent symptom (14.6%), which is in contrast to most descriptive studies.[9,13,20,30] These findings show that snoring and sleepiness (two of the main features of OSAS[12]) were not the significant complaints making the patients ask for medical attention. This fact may be attributed to several factors, in particular, the lack of public information regarding the importance of sleep apnea and its presenting picture in the studied population. As a result, it can be predicted that most OSA patients in Iran mainly complain of symptoms other than snoring and sleepiness such as insomnia, anxiety, depression, and headaches.
In addition, our study showed higher frequency of anxiety and depressive symptoms among OSAS patients compared to the general Iranian population, which was calculated in previous studies applying BDI-II and BAI.[31,32] Regarding the relationship between sex and OSAS symptoms, anxiety was estimated in 53.89% of male and 54.2% of female OSAS patients in our study. As the distribution of sex ratio was not equal (86.5% men vs. 13.5% women), we calculated the OR for sex (male/female), which was 1.011 for OSAS patients with anxiety (P: 0.02). Accordingly, we showed the same incidence of anxiety in male and female patients who suffered from sleep apnea. This finding is in contrast to the results of previous epidemiologic studies in which the prevalence of atypical symptoms like anxiety and depression was reported to be more among female patients.[33,34,35] This difference may arise from factors such as methodology and race-related difference in OSAS symptoms.[2,12] Regarding the incidence of depression in our study, 48% of male and 33% of female OSAS patients had depressive symptoms. The OR of depressive female/male in OSAS patients was 0.54 with CI of 0.22-1.34; however, from the statistics point of view, the evidence was not significant (P: 0.178). In other words, although we showed higher frequency of depressive symptoms in OSAS, which is compatible with large studies,[33,35] we failed to demonstrate any association between sex and depression in OSAS sufferers. Furthermore, we investigated the relationship between the severity of sleep apnea (determined by AHI levels) and OSAS symptoms. We found evidence that the prevalence of anxiety increased as the severity of OSAS was intensified (P: 0.01). This finding is consistent with some other epidemiologic studies.[19,20,36] On the other hand, while a correlation between the severity of sleep apnea and depression, snoring, headaches, insomnia, and nightmare has been demonstrated in some previous studies,[20,21] we failed to show such a correlation. Again, race differences or methodology may be considered in this area.
Finally, we studied the association of BMI and ESS with the severity of sleep apnea and the presenting symptoms. Similar to multiple previous studies,[2,15,21,37,38] our study demonstrated that high levels of AHI (indicating the severity of OSAS) correlated with high BMI. In other words, severe OSAS is more frequent in people with high BMI. Moreover, we examined the relationship of ESS and BMI with the symptoms of OSAS. In terms of ESS, this study showed that ESS was around 1.52 (CI: 0.13-3.18) higher in OSAS individuals with depression symptoms; however, the evidence was very weak (P: 0.071) and this correlation may be attributed to overlapping symptoms like fatigue and tendency to dozing. On the other hand, we did not find an association between ESS and anxiety. In terms of BMI, we did not find any significant link between BMI and depression symptoms but found evidence showing that the mean BMI in OSAS patients with anxiety was 1.76 (CI: 0.24-3.28) higher than in OSAS patients without this symptom (P: 0.023). In summary, our study indicated that high BMI not only was associated with the severity of OSAS but also increased the frequency of anxiety.
Although we achieved interesting results, there were limitations in our study. We did not determine anxiety disorders and depression as a disorder. Symptoms regarding anxiety and depression, which were evaluated by BAI and BDI-II, could be assessed in other means. As a result, different data may be achieved according to methodology. The size of studied population may also be a limitation. In addition, cultural conflicts may influence the results. For example, data regarding sexual function (particularly among women in a traditional society), job performance, and impulsivity may be false. Considering these facts, further investigation is still a necessity in this area.
CONCLUSION
We conclude that the likelihood of presenting anxiety was higher in OSAS patients than in the general population. We also showed that anxiety was more frequent in OSAS patients with high BMI and severe OSAS. In addition, this study, which was conducted in a Middle East region, demonstrated the high possibility of presenting OSAS with atypical features such as anxiety, headaches, and insomnia. Therefore, it is advisable for a variety of medical specialists including psychiatrists to keep in mind the probable diagnosis of OSAS in such conditions, particularly in societies with low public information regarding this serious syndrome.
ACKNOWLEDGMENT
The authors appreciate the cooperation of Psychiatry and Behavior Research Center at Mashhad University of Medical Sciences.
Footnotes
Source of Support: Psychiatry and Behavioral Sciences Research Center, Mashhad University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Yaggi HK, Cancato J, Karen WN. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353:2034–41. doi: 10.1056/NEJMoa043104. [DOI] [PubMed] [Google Scholar]
- 2.McnNicholas WT, Bonsignore MR the Management Committee of EU COST ACTION B26. Sleep apnea as independent risk factor for cardiovascular disease: Current evidence, basic mechanisms and research priorities. Eur Respir J. 2007;29:156–78. doi: 10.1183/09031936.00027406. [DOI] [PubMed] [Google Scholar]
- 3.Fishman AP, Elias JA, Grripi MA, Senior RM, Pack AI. 4th ed. USA: McGraw-Hill; 2008. Fishman's pulmonary diseases and disorders. [Google Scholar]
- 4.Nguên XL, Rakotonanahary D, Chaskalovic J, Fleury B. Insomnia related to sleep apnea: Effect of long-term auto-adjusting positive airway pressure treatment. Eur Respir J. 2012 doi: 10.1183/09031936.00080011. [In Press] [DOI] [PubMed] [Google Scholar]
- 5.Arroll B, Fernando A, Goodyear-Smith F, Samaranayake C, Warman G. Prevalence of causes of insomnia in primary care: A cross-sectional study. Br J Gen Pract. 2012;62:e99–103. doi: 10.3399/bjgp12X625157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kristiansen HA, Kvǽrner KJ, Akre H, Øvrland B, Sandvik L, Russell MB. Sleep apnea headache in general population. Cephalalgia. 2012;32:451–8. doi: 10.1177/0333102411431900. [DOI] [PubMed] [Google Scholar]
- 7.Ho ML, Brass SD. Obstructive sleep apnea. Neurol Int. 2011;3:e15. doi: 10.4081/ni.2011.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baharmmam AS, Al-Shimemeri SA, Salama RI, Sharif MM. Clinical and polysomnographic charactristics and response to continous positive airway pressure therapy in obstructive sleep apnea patients. Sleep Med. 2012;14:149–54. doi: 10.1016/j.sleep.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 9.Duran J, Esnaola S, Rubio R. Obstructive sleep apnea-hypopnea and related clinical features in a population based sample of subjects aged 30 to 70 years. Am J Respir Crit Care Med. 2001;163:685–9. doi: 10.1164/ajrccm.163.3.2005065. [DOI] [PubMed] [Google Scholar]
- 10.Lurie A. Cardiovascular disorders associated with obstructive sleep apnea. Adv Cardiol. 2011;46:197–266. doi: 10.1159/000325110. [DOI] [PubMed] [Google Scholar]
- 11.Findley L, Univerzagt M, Suratt P. Automobile accidents involving patients with obstructive sleep apnea. Am Rev Respir Dis. 1988;138:337–40. doi: 10.1164/ajrccm/138.2.337. [DOI] [PubMed] [Google Scholar]
- 12.Kielb SA, Ankoli-Israel S, Rebok GW, Spira AP. Cognition in obstructive sleep apnea-hypopnea syndrome (OSAS): Current clinical knowledge and the impact of treatment. Neuromolecular Med. 2012;14:180–93. doi: 10.1007/s12017-012-8182-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Galecki P, Florkowski A, Zboralski K, Pietras T, Szemraj J, Talarowska M. Psychiatric and psychological complications in obstructive sleep apnea syndrome. Pneumonol Alergol Pol. 2011;79:26–31. [PubMed] [Google Scholar]
- 14.Partinen M, Guilleminault C. Daytime sleepiness and vascular morbidity at seven-year follow-up in obstructive sleep apnea patients. Chest. 1990;97:27–32. doi: 10.1378/chest.97.1.27. [DOI] [PubMed] [Google Scholar]
- 15.Wiegand L, Zwillich CW. Obstructive sleep apnea. Dis Mon. 1994;40:197–252. doi: 10.1016/0011-5029(94)90013-2. [DOI] [PubMed] [Google Scholar]
- 16.2nd ed. New York: Westchester, III; 2005. American Academy of Sleep Medicine; International classification of sleep disorders: Diagnostic and coding manual. [Google Scholar]
- 17.USA: Wiley; 2005. Sleep. A comprehensive HANDBOOK. Teofilo L. Lee-Chiong; p. 336. [Google Scholar]
- 18.Chasens ER, Pack AI, Maislin G, Dinges DF, Weaver TE. Claustrophobia and adherence to CPAP treatment. West J Nurs Res. 2005;27:307–21. doi: 10.1177/0193945904273283. [DOI] [PubMed] [Google Scholar]
- 19.Velasco-Rey MC, Sánchez-Muñoz M, Gutiérrez-López MI, Trujillo-Borrego A, Sánchez-Bonome L. Psychotic depression induced by Obstructive Sleep Apnoea Syndrome (OSAS): A case reported. Actas Esp Psiquiatr. 2012;40:43–5. [PubMed] [Google Scholar]
- 20.Akashiba T, Kavahara S, Akahoshi T, Omori C, Saito O, Majima T, et al. Relationship between quality of life and mood or depression in patients with severe obstructive sleep apnea syndrome. Chest. 2002;122:861–5. doi: 10.1378/chest.122.3.861. [DOI] [PubMed] [Google Scholar]
- 21.Azargra-Calero E, Espinar-Eskalona E, Barrera-Mora J, Liamas-Carreras J. Obstructive sleep apnea syndrome (OSAS). Review of literature. Med Oral Patol Oral Cir Bucal. 2012;17:925–9. doi: 10.4317/medoral.17706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Andrews JG, Oei TP. The roles of depression and anxiety in the understanding and treatment of Obstructive Sleep Apnea Syndrome. Clin Psychol Rev. 2004;24:1031–49. doi: 10.1016/j.cpr.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 23.Asghari A, Mohammadi F, Kamrava SK, Tavakoli S, Farhadi M. Severity of depression and anxiety in obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol. 2012;269:2549–53. doi: 10.1007/s00405-012-1942-6. [DOI] [PubMed] [Google Scholar]
- 24.Ghasemzadeh H, Mojtabai R, Karamghadiri N, Ebrahimkhani N. Psychometric properties of a Persian-language version of the Beck depression inventory – second edition: BDI-II-Persian. Depress Anxiety. 2005;21:185–92. doi: 10.1002/da.20070. [DOI] [PubMed] [Google Scholar]
- 25.Kaviani H, Mousavi AS. Psychometric properties of the Persian version of Beck anxiety inventory. Tehran Univ Med J. 2005;65:136–40. [Google Scholar]
- 26.Iran: Mental Health Research Center, Tehran Psychiatric Institute; [Last accessed on 2010 Dec]. Beck anxiety inventory scoring. Available from: http://mhrn.net/template/farsi/index.aspx . [Google Scholar]
- 27.Iran: Mental Health Research Center, Tehran Psychiatric Institute; [Last accessed on 2010 Dec]. Beck depression inventory scoring. Available from: http://mhrn.net/template/farsi/index.aspx . [Google Scholar]
- 28.Kryger MH, Roth T, Dement WC. 5th ed. USA, Philadelphia, St. Louis: Elsivier; 2011. Principles and practice of sleep medicine. [Google Scholar]
- 29.Overmeen S, Reading P. Singapore: Wiley-Blackwell; 2010. Sleep disorders in neurology, a PRACTICAL APROACH. [Google Scholar]
- 30.Mason RJ, Broaddus VC, Murray JF, Nadel JA. 4th ed. USA: Philadelphia; 2005. Murray and Nadel's textbook of respiratory medicine. [Google Scholar]
- 31.Kaviani H, Abhari AA. Prevalence of anxiety disorders in Tehran city. Iran J Psychiatry Clin Psychol. 2003;3:4–11. [Google Scholar]
- 32.Talaei A, Fayyazi BM, Rezaei AA. J Psych Behav Sci. Vol. 4. Iran: Mazandaran University of Medical Sciences; 2009. Depression and its correlation with self-esteem and social support among Iranian university students; pp. 17–22. [Google Scholar]
- 33.Valipour A. Gender-related differences in the obstructive seep apnea syndrome. Pneumologie. 2012;66:584–8. doi: 10.1055/s-0032-1325664. [DOI] [PubMed] [Google Scholar]
- 34.Sharafkhaneh A, Giray N, Richardson P, Young T, Hirshkowitz M. Association of Psychiatric disorders and sleep apnea in a large cohort. Sleep. 2005;28:1405–11. doi: 10.1093/sleep/28.11.1405. [DOI] [PubMed] [Google Scholar]
- 35.Harris M, Glozier N, Ratnavadivel R, Grunstein RR. Obstructive sleep apnea and depression. Sleep Med Rev. 2009;13:437–44. doi: 10.1016/j.smrv.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 36.Akashiba T, Kavahara S, Akahoshi T, Omori C, Saitto O, Majima T, et al. Relationship between quality of life and mood or depression in patients with severe obstructive sleep apnea syndrome. Chest. 2002;122:861–5. doi: 10.1378/chest.122.3.861. [DOI] [PubMed] [Google Scholar]
- 37.Morimoto S, Takahashi T, Okaishi K, Okuro M, Nakahashi T, Sakamado D, et al. Sleep apnoea syndrome as a risk for mortality in elderly inpatients. J Inter Med Res. 2012;40:601–11. doi: 10.1177/147323001204000222. [DOI] [PubMed] [Google Scholar]
- 38.Amra B, Golshan M, Fietze I, Penzel T, Welte T. Correlation between chronic obstructive pulmonary disease and obstructive sleep apnea syndrome in a general population in Iran. J Res Med Sci. 2011;16:885–9. [PMC free article] [PubMed] [Google Scholar]


