Abstract
Background:
Sexual dysfunction (SD) is a common reported problem in patients with multiple sclerosis (MS).
Aims:
to examine frequency and distribution of SD dimensions and to determine whether SD is related to various clinical and demographic variables in female patients.
Materials and Methods:
A total of 271 MS women (age: 19-50 years) participated in this cross-sectional study. We used a structured demographic and clinical interview and Multiple Sclerosis Intimacy and Sexuality Questionnaire-19 (MSISQ-19). Disability was rated by Expanded Disability Status Score (EDSS).
Results:
63.5% (n = 173) of women had SD included 142 (52.4%) women with primary SD, 102 (37.5%) women with secondary SD and 120 (41%) women with tertiary SD. The most common SD-related complaint was orgasmic problem (41.2%). Women with primary SD were significantly older and had higher EDSS score. No significant relationship was found between primary SD and disease duration. Fatigue (OR = 2.69, 95% CI: 1.352-5.385, P = 0.005), memory and concentration complaints (OR = 1.915, 95% CI: 1.034-3.546, P = 0.039) and some of urinary symptoms such as frequency (OR = 2.108, 95% CI: 1.015-4.375, P = 0.045) were seem to be the significant predictors. Fatigue was also found to be the most powerful predicting factor for tertiary SD (OR = 2.793, 95% CI: 1.358-5.744 P = 0.005).
Conclusion:
SD, a common multifactorial problem among MS women, can arise at any time during the disease and with any level of disability. However, we found relationships between SD and some of clinical variables and symptoms. Understanding these relationships would help us to develop practical approach and treatment for SD.
Keywords: Female sexual dysfunction, MSISQ-19, multiple sclerosis
INTRODUCTION
Multiple sclerosis (MS) is a chronic progressive neurological disease, which is most likely to develop in young adult; at the age that is an important time of life for sexual activity. Sexual dysfunction (SD) is a common reported problem among patients with MS. Unfortunately, it often remains under-diagnosis. SD prevalence ranges from 40 to 80% in MS women.[1] Therefore, SD can affect MS women's quality of life negatively.
Foley and Iverson developed a conceptual model for SD in MS patients. It described SD as having three levels of responsible factors, in terms of primary, secondary, and tertiary.[2] Primary SD is due to neurological changes in central nervous system affecting sexual function directly. Symptoms of this dimension include decreased sexual desire, arousal and orgasmic problems, decreased vaginal lubrication and change in genital sensation. Secondary SD occurs as a result of physical symptoms which indirectly impact on sexual activity. Some examples of these symptoms are fatigue, muscle weakness, spasticity, tremor, cognitive problems, bladder and bowel dysfunction, numbness or sensational change in non-genital areas, and incoordination. Tertiary SD derived from psychological and social aspects of MS that affect sexual feeling negatively, such as negative self-image, lowered self-esteem, fear of being rejected, feeling of dependency, anger, and depression.[3,4]
Female sexuality is a multidimensional subject. There has been less attention paid to frequency and characteristics of sexual complaints among women with MS, in comparison with men.[5] However, in contrast with literature, some studies showed that women with MS experience SD, more common and with higher level than male patients.[6,7,8] Previous studies found variable relationships between SD and age, disease duration, disability, disease course, and other symptoms of the disease.[6,8,9,10,11] Zivadinov et al, indicated that SD in women was significantly correlated with disability, age, primary progressive coarse of disease and symptoms, such as depression, bladder dysfunction, fatigue, and cognitive problems. No relationship was found between disease duration, secondary progressive MS, and bowel dysfunction.[9] In a recently performed study, Celik et al., showed that primary SD was not related to EDSS score and disease duration significantly, but tertiary SD was correlated with EDSS score.[6]
Because of a religious and male-dominant culture in some countries like Iran, women have difficulties expressing their own feelings and sexual experiences; consequently, female SD may not consider as an important issue.[12] There is no study investigated SD in Persian female with MS. According to important role of sexual function on quality of life, and developing new medical and psychological treatment for SD, early diagnosis in MS patient is necessary. Furthermore, understanding characteristics and contributing factors for SD lead to improve treatments and interventions.
Previous studies investigated SD based on primary-secondary-tertiary model were limited and done with a small sample size.[6,13] Accordingly, we decided to examine the role of different aspects of MS disease on patients’ sexual function, exclusively in women, with a larger sample size and by considering the above mentioned model. The aims of present study were to examine frequency, distribution and interrelation of the three SD dimensions, and to determine whether there are relationships between various clinical and demographic variables and different levels of SD in women with MS.
MATERIALS AND METHODS
We conducted this cross-sectional study from August 2012 to March 2013 in the Ayatollah Kashani Hospital in Isfahan after Isfahan University of Medical Sciences Ethic committee institutionally approved our research. Under-studied population was MS women who were admitted to MS clinic in Ayatollah Kashani Hospital. Inclusion criteria were: definite MS, being married and age between 18-50 years old. Women with an exacerbation during the last 6 months, postmenopauseal or sexually inactive women and women who had other concomitant disease or use medications like beta-blockers and anti-depressants which could affect sexual activity were not included in the study. We selected 275 women non-randomly and consecutively according to inclusion and non-inclusion criteria. Written informed consent was obtained from each of them.
We excluded four patients who did not complete the interview. Therefore, our final sample comprised 271 women. The mean age of participants was 35.1 ± 8.1 years old. The mean duration of disease was 72.2 ± 48.9 months among the patients. They had mean EDSS score of 2.4 ± 1.3. Our sample included 233 patients with relapsing-remitting MS (RRMS), seven patients with primary-progressive MS (PPMS), and 32 patients with secondary-progressive MS (SPMS).
A female physician interviewed each woman with a structured demographic and clinical questionnaire about age, relationship status, child number, educational level and occupation, medical and sexual histories, such as quality of relationships, sexual function, and the presence of any physical symptom or psychological disorder. Moreover, we assessed sexuality of each woman by Multiple Sclerosis Intimacy and Sexuality Questionnaire-19 (MSISQ-19). It is a valid, reliable self-reported questionnaire which contains 19 items. This questionnaire rates how various MS symptoms have impaired sexual activity, sexual satisfaction, and relationship intimacy of patient during the last 6 months. From these 19 items, there are five items regarding primary, nine items for secondary, and five items for tertiary SD. Each item rates from score 1 to score5, indicating how often this item has interfered with sexual activity during previous 6 months; (1 = never, 2 = almost never, 3 = sometimes, 4 = almost always, 5 = always). Score 4 or 5 for each item is considered as SD.[4]
All women underwent a full neurological examination. Neurological impairment and disability were rated by Expanded Disability Status Score (EDSS) assessing pyramidal, cerebellar, brainstem, sensory, bowel and bladder, visual and mental functions.[14]
All data were recorded in the computer and were analyzed by SPSS version 20. Data analysis was performed by using Chi-square, indipende -T, logistic regression and ANOVA test. Pearson correlation was also used to clarify relationships between quantifiable variables. A P-value < 0.05 was considered statistically significant.
RESULTS
According to MSISQ-19 score, SD was diagnosed in 173 (63.5%) of women, who had participated in this study. We divided women into two groups according to the presence of SD. Statistical analysis demonstrated that women with SD were significantly older (36.1 ± 8.0 vs. 33.2 ± 7.9, respectively; P = 0.004), had longer disease duration (78.4 ± 53.5 vs. 60.4 ± 36.8, respectively; P = 0.026) and had higher EDSS score (2.8 ± 1.4 vs. 1.8 ± 0.9, respectively; P = 0.000) than women without SD. Housewives had SD meaningfully more than employed women (P = 0.018). The incidence of SD showed no significant relation with level of education (P = 0.15).
To characterize three levels of influence, patients were reported particularly, presence of primary, secondary and tertiary SD by using MSISQ-19 subscales. One hundred and forty-two women (52.4 %) reported primary SD in several areas, included difficulty reaching orgasm (41.2%), less intense orgasm (34.9%), lack of sexual interest (33.8%), decreased genital sensation (17.6%) and decreased lubrication (25.7%). A total of 87.1% of women with primary SD experienced more than one symptom.
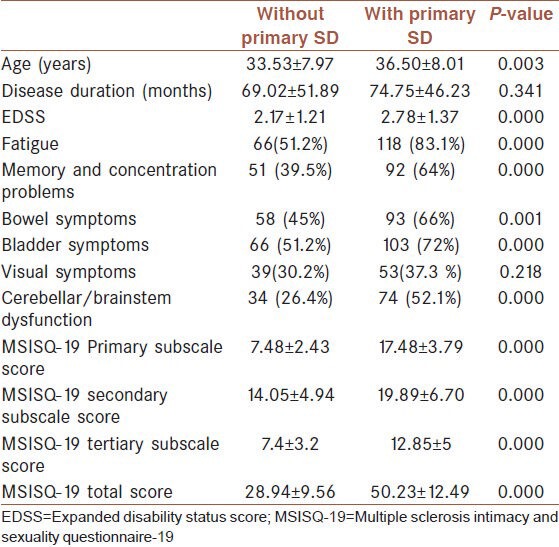
Table 1 shows the difference between women with and without primary SD in relation to clinical variables and some of physical symptoms. Women with primary SD were reported to had significantly higher EDSS score (P-value = 0.000, independent T-test). Nevertheless, 71 women with primary SD (50%) had EDSS ≤2.0. They reported primary SD with the same symptoms as women with higher level of disability. Although decreased sensation of genital (9.6%) and decreased lubrication (10.5%) were reported less common in female with lower EDSS score. Unlike most of clinical variables, disease duration was not significantly different between women with and without primary SD.
Table 1.
Comparison of female patients with and without SD
One hundred and two (37.5%) MS female patients experienced secondary SD. Common problems of this dimension in increasing order, included weakness and mobility difficulty (15.4%), cognitive deterioration (12.2%), urinary symptoms (12%), spasticity (11%), pain-burning (11%), and tremor (9.2%). One hundred and twenty women (41%) had tertiary SD. Feeling less feminine (27%), worries about satisfying their partners (19.9%), lack of confidence (19.5%), fear of rejection (14.3%), and feeling less attractive (11.4%) were reported, respectively.
Notable significant relations were observed between some symptoms of secondary SD and primary SD [Table 1]. Women with primary SD exhibited fatigue (P = 0.000), bowel-bladder symptoms (P = 0.000), memory and concentration problems (P = 0.000), brainstem and cerebellar symptoms (P = 0.000) more frequent. Among lower urinary tract symptoms, frequency (P = 0.000) and incontinency (P = 0.006) were found to have stronger relationship with primary SD. Women with primary SD had higher secondary SD and tertiary SD MSISQ-19 subscale score statistically (P = 0.000).
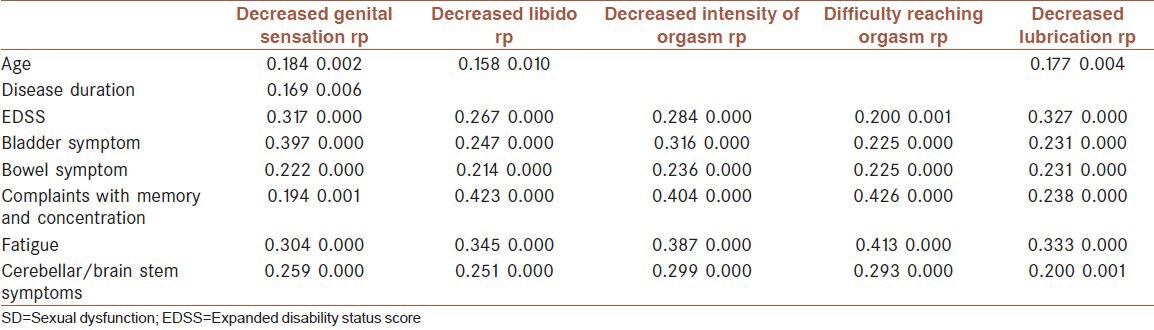
We conducted correlation analysis between different items of primary SD score in MSISQ-19 and other features and symptoms of patients [Table 2]. As you see a positive correlation was found between decreased genital area sensation, orgasmic capacity disorders, and urinary symptoms. MSISQ-19 subscale item regarding memory and concentration was also more correlated with decreased libido and difficulty reaching orgasm.
Table 2.
Correlation analyses between clinical variables and primary SD symptoms
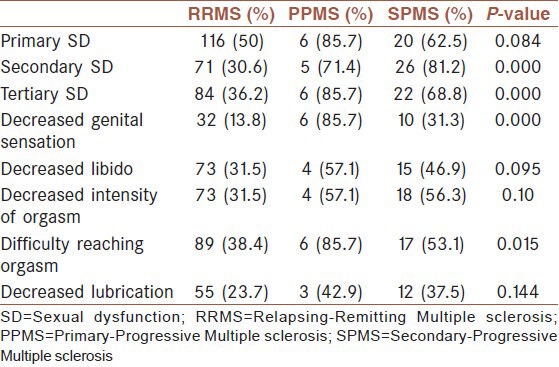
Primary SD was diagnosed in 50% of women with RRMS, 87.6% of PPMS women, and 62.5% of SPMS women. Secondary and tertiary SD was significantly more reported in women with any progressive form of disease. Primary SD was more common in women with SPMS and PPMS, but that failed to reach significance. Although SPMS and PPMS women were reported some primary SD-related items of MSISQ-19 significantly more frequent [Table 3]. The ANOVA test also indicated a significance difference between the disease courses for decreased genital sensation (P = 0.000) and decreased intensity of orgasm (P = 0.044).
Table 3.
Disease courses differences in presence of SD
We conducted Binary logistic regression for each SD dimension to determine independent variables for primary SD among the MS females. Fatigue (OR = 2.69, 95% CI: 1.352-5.385, P = 0.005), memory and concentration complaints (OR = 1.915, 95% CI: 1.034-3.546, P = 0.039) and some of urinary symptoms such as frequency (OR = 2.108, 95% CI: 1.015-4.375, P = 0.045) were seem to be the significant predictors. Fatigue was also found to be the most powerful predicting factor for tertiary SD (OR = 2.793, 95% CI: 1.358-5.744, P = 0.005). Moreover, EDSS score (OR = 1.86, 95% CI: 1.212-2.868, P = 0.005), dysuria (OR = 3.668, 95% CI: 1.131-11.9, P = 0.03), memory and concentration complaints (OR = 2.638, 95% CI: 1.225-5.68, P = 0.013), fatigue (OR = 3.27, 95% CI: 1.274-8.396, P = 0.014) and cerebellar problems (OR = 2.318, 95% CI: 1.09-4.929, P = 0.029) were found as contributory factors for secondary SD.
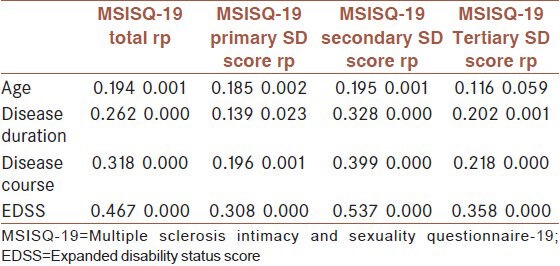
We also performed correlation analysis between the MSISQ-19 total and subscale scores and some clinical features [Table 4]. A significant correlation was found between secondary SD and both disease duration and disease courses. We also observed a strong association between EDSS score and each of the SD dimensions.
Table 4.
Correlation analyses between MSISQ-19 scores and clinical features
DISCUSSION AND CONCLUSION
Our study was designed to investigate frequency and distribution of SD dimensions, and to identify contributory factors for SD in women with MS. The high frequency of SD in present study appears that, SD is a common problem among female MS patients consistent with the previous knowledge.
Primary SD was reported as the most common SD dimension. It was consistent with a previously performed study by demirkiran et al.[13] The result of our study reveals that despite the burden of MS-related physical and psychological influence, MS seems to have a detrimental impact on female sexuality, directly. Nevertheless, relatively high percentage of secondary and tertiary SD in present study emphasizes the multi-causal and multidimensional nature of SD in women as it was shown in previous studies.[15,16] Therefore, in assessment and treatment of SD the important role of secondary and tertiary SD should be considered, especially in women with higher level of disability.
According to the literature, the frequency of sexual problems is variable from study to study. Between 21- 60% of women with MS reported, decreased or lack of sexual desire.[6,10,13,17,18,19,20] Orgasmic dysfunction and decreased vaginal lubrication have been documented in 37- 51% of women.[10,17,18,20,21] In the current study, the most common sexual problems were orgasmic dysfunction (including decreased intension and difficulty reaching orgasm) and decreased sexual desire.
Association between SD and degree of disability has been reported by some of the past studies.[8,9,17,20] In our study, we found a significant relation between primary SD and EDSS score. On the other hand, frequency of primary SD is notable in less disable women. These findings indicate that in spite of the strong relationship between SD and EDSS score, SD can present even without a severe physical or neurological impairment. Significant correlations between secondary and tertiary SD and disease duration were shown in the present study. But such a relation was not observed between primary SD and disease duration. It is consistent with some previous reports.[8,9]
Longitudinal studies revealed that the frequency of SD and deterioration of sexual activity in patient with MS increase over time.[22,23] A follow-up study by Stenager et al., demonstrated the level of SD increased over a 5-year period.[22] The result of our study shows that SD can occur at any time after diagnosis of MS. Tzortzis et al, evaluated primary SD in 63 newly diagnosed MS women with no major neurological impairment or risk factor. Primary SD was reported more frequently in MS patients in comparison with control group (34.9%).[24] Accordingly, assessment for SD should be done in all MS women with any level of disability and at any time during the disease course.
The relationship between tertiary SD and EDSS suggests that women with more severe disability experience significantly lower level of sexual confidence. Women with primary SD significantly exhibited secondary SD more and also had higher MSISQ-19 secondary subscale score. It is in concordance with the strong correlation between primary SD and some symptoms of secondary SD, such as fatigue, memory and concentration problems, urinary dysfunction, and celleberal complaints. The strongest relationship was observed between fatigue and primary SD in women with MS. Our findings are similar to others’ reported in past researches.[8,9,13,18] The correlation between fatigue and tertiary SD may be explained by the important role of depression as a contributory factor. All these findings suggest fatigue as an important risk factor for SD in MS female patients. Hence, any practical treatment for SD in women with MS should contain strategies to manage fatigue.
Depression, anxiety, and other psychosocial factors (symptoms of tertiary SD) found to be associated with sexuality among MS patients in most of the previous studies.[9,13,19] Barak et al., demonstrated that depression was correlated with SD and anorgasmia specifically.[19] In the current study, high frequency of women with tertiary SD and strong relationship between primary and tertiary SD emphasized the effective role of psychosocial factors on sexual function of MS women in different levels.
High percentage of MS women experience urinary symptoms.[25] This problem could have a negative impact on patients’ quality of life like SD.[15] The result of our study reveals that SD was more likely to occur in female patient with bladder problems. An association between sphincteric dysfunction and SD was documented in some studies.[8,9,23,26,27] We also observed that bladder symptoms were mostly correlated with decreased genital sensation and decreased orgasmic capacity in women. Such of these selective relations between bladder dysfunction and symptoms of primary SD was reported previously.[13,28] Zorzen et al., reported that bladder dysfunction was correlated with deterioration of sexual activity over time. They suggested that the correlation is due to sharing the same autonomic segment.[23]
Demirikan et al., investigated types and frequency of sexual problems in 51 patients including 68.6% RRMS, 17.6% SPMS, and 13.7% PPMS. They found that patients with progressive forms of MS had more primary SD symptoms. They suggested the presence of a relationship between SD and progressive nature of disease.[13] The result of current study shows no significant difference in the presence of primary SD regarding disease courses. However, secondary SD and tertiary SD are more common in women with progressive types of disease significantly. So, higher frequency of SD in women with PRMS and SPMS may be due to the higher level of disability and psychological affects that accompany these courses.
There were some limitations in our study. For better understanding the role of each contributing factor, which was investigated in current study, it would be better to evaluate them separately, by neutralizing the confounding effects of other variables and risk factors. Sexuality is a two-sided issue and MS also impacts upon other members of patient's family. Therefore, investigation of sexuality and role of social variables in patients’ partners were suggested for future research.
The self-reported questionnaire applied in this study would help physicians to find targets for further investigations; and it would provide a convenient way for patients to talk about their sexual problems. Although using additional objective measures could increase the accuracy of our results.
In conclusion, due to variable presentations and multifactorial nature of SD among women with MS, developing a symptomatic therapy for SD based on the symptoms and underlying causes could be more beneficial. We also demonstrated relationships between SD and some aspects of disease. Hence, in order to provide an effective approach and management for SD all the mentioned symptoms and clinical variables should be kept in mind.
ACKNOWLEDGMENT
The research project number is 390508.
Footnotes
Source of Support: Isfahan University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Foley FW, Sander A. Sexuality, multiple sclerosis and women. Mult Scler Manage. 1997;4:1–9. [Google Scholar]
- 2.Foley FW, Iverson J. Sexuality and multiple sclerosis. In: Kalb RC, Scheinberg LC, editors. Multiple sclerosis and family. New York: Demos; 1992. pp. 63–82. [Google Scholar]
- 3.Foley FW, LaRocca NG, Sanders AZ, Zemon V. Rehabilitation of intimacy and sexual dysfunction in couples with multiple sclerosis. Mult Scler. 2001;7:417–21. doi: 10.1177/135245850100700612. [DOI] [PubMed] [Google Scholar]
- 4.Sanders AS, Feloy FW, LaRocca NG, Nicholas G, Zemon V. The Multiple Sclerosis Intimacy and Sexuality Questionnaire-19 (MSISQ-19) Sex Disabil. 2000;18:3–24. [Google Scholar]
- 5.McCabe MP, McKern S, McDonald E, Vowels LM. Changes over time in sexual and relationship functioning of people with Multiple Sclerosis. J Sex Marital Ther. 2003;29:305–21. doi: 10.1080/00926230390195506-2372. [DOI] [PubMed] [Google Scholar]
- 6.Celik DB, Poyraz EÇ, Bingöl A, Idiman E, Ozakbaş S, Kaya D. Sexual dysfunction in multiple sclerosis: Gender differences. J Neurol Sci. 2013;324:17–20. doi: 10.1016/j.jns.2012.08.019. [DOI] [PubMed] [Google Scholar]
- 7.MaCabe MP. Relationship functioning and sexuality among people with multiple sclerosis. J Sex Res. 2002;39:302–9. doi: 10.1080/00224490209552154. [DOI] [PubMed] [Google Scholar]
- 8.Fraser C, Mahoney J, McGurl J. Correlates of sexual dysfunction in men and women with multiple sclerosis. J Neurosci Nurs. 2008;40:312–7. doi: 10.1097/01376517-200810000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Zivadinov R, Zorzon M, Bosco A, Bragadin LM, Moretti R, Bonfigli L, et al. Sexual dysfunction in multiple sclerosis: II. Correlation analysis. Mult Scler. 1999;5:428–31. doi: 10.1177/135245859900500i610. [DOI] [PubMed] [Google Scholar]
- 10.Valleroy ML, Kraft GH. Sexual disturbances arising from multiole sclerosis. Arch Phys Med Rehabil. 1984;65:125–8. [PubMed] [Google Scholar]
- 11.Nortvedt MW, Riise T, Frugard J, Mohn J, Bakke A, Skar AB, et al. Prevalence of bladder, bowel and sexual problems among multiple sclerosis patients two to five years after diagnosis. Mult Scler. 2007;13:106–12. doi: 10.1177/1352458506071210. [DOI] [PubMed] [Google Scholar]
- 12.Safa-Isfahani K. Female-centered world views in Iranian culture: Symbolic representations of sexuality in dramatic games. J Women Cult Soc. 1980;6:33–53. [Google Scholar]
- 13.Demirkiran M, Sarica Y, Uguz S, Yerdelen D, Aslan K. Multiple sclerosis patients with and without sexual dysfunction: Are there any difference? Mult Scler. 2006;12:209–14. doi: 10.1191/135248506ms1253oa. [DOI] [PubMed] [Google Scholar]
- 14.Kurtzke JF. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS) Neurology. 1983;33:1444–52. doi: 10.1212/wnl.33.11.1444. [DOI] [PubMed] [Google Scholar]
- 15.Bronner G, Elran E, Golomb J, Korczyn AD. Female sexuality in multiple sclerosis: The multidimensional nature of the problem and intervention. Acta Neurol Scand. 2010;121:289–301. doi: 10.1111/j.1600-0404.2009.01314.x. [DOI] [PubMed] [Google Scholar]
- 16.Guo ZN, He SY, Zhang HL, Wu J, Yang Y. Multiple sclerosis and sexual dysfunction. Asian J Androl. 2012;14:530–5. doi: 10.1038/aja.2011.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hutler BM, Lundberg PO. Sexual function in women with advanced multiple sclerosis. J Neurol Neurosurg Psychiatry. 1995;59:83–6. doi: 10.1136/jnnp.59.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zorzon M, Zivadinov R, Bosco A, Bragadin LM, Moretti R, Bonfigli L, et al. Sexual dysfunction in multiple sclerosis: A case-control study. I. frequency and comparison of groups. Mult Scler. 1999;5:418–27. doi: 10.1177/135245859900500i609. [DOI] [PubMed] [Google Scholar]
- 19.Barak Y, Achiron A, Elizur A, Gabbay U, Noy S, Sarova-Pinhas I. Sexual dysfunction in relapsing-remitting multiple sclerosis: Magnetic resonance imaging, clinical, and psychological correlates. J Psychiatry Neurosci. 1996;21:255–8. [PMC free article] [PubMed] [Google Scholar]
- 20.Hennessy A, Robertson NP, Swingler R, Compston AS. Urinary, faecal and sexual dysfunction in patient with multiple sclerosis. J Neurol. 1999;246:1027–32. doi: 10.1007/s004150050508. [DOI] [PubMed] [Google Scholar]
- 21.Dachille G, Ludovico GM, Pagliarulo G, Vestita G. Sexual dysfunction in multiple sclerosis. Minerva Urol Nefrol. 2008;60:77–9. [PubMed] [Google Scholar]
- 22.Stenager E, Stenager EN, Jensen K. Sexual function in multiple sclerosis: A 5-year follow-up study. Ital J Neurol Sci. 1996;17:67–9. doi: 10.1007/BF01995711. [DOI] [PubMed] [Google Scholar]
- 23.Zorzon M, Zivadinov R, Monti Bragadin L, Moretti R, De Massi R, Nasuelli D, et al. Sexual dysfunction in multiple sclerosis: A 2-year follow up study. J Neurol Sci. 2001;187:1–5. doi: 10.1016/s0022-510x(01)00493-2. [DOI] [PubMed] [Google Scholar]
- 24.Tzortzis V, Skriapas K, Hadjigeorgious G, Mitsogiannis I, Aggelaksi K, Gravas S, et al. Sexual dysfunction in newly diagnosed multiple sclerosis women. Mult Scler. 2008;14:561–3. doi: 10.1177/13524585080140040901. [DOI] [PubMed] [Google Scholar]
- 25.Litwiller SE, Frohman EM, Zimmern PE. Multiple sclerosis and the urologist. J Urol. 1999;161:743–57. [PubMed] [Google Scholar]
- 26.Mattson D, Petrie M, Srivastava DK, McDermott M. Multiple sclerosis: Sexual dysfunction and its response to medications. Acta Neurol. 1995;52:826–8. doi: 10.1001/archneur.1995.00540330040012. [DOI] [PubMed] [Google Scholar]
- 27.Minderhoud JM, Leemhuis JG, Kremer J, Laban E, Smit PM. Sexual disturbances arising from multiple sclerosis. Acta Neurol Scand. 1984;70:299–306. doi: 10.1111/j.1600-0404.1984.tb00827.x. [DOI] [PubMed] [Google Scholar]
- 28.Lundberg PO. Sexual dysfunction in female patients with multiple sclerosis. Int Rehabil Med. 1981;3:32–4. doi: 10.3109/03790798109167112. [DOI] [PubMed] [Google Scholar]


