Abstract
Background:
Although evidences emphasize on the importance of aftercare programs to achieve continuity of care, different studies have revealed controversial results about the outcome. The objective of this study was to investigate the effect of aftercare program on outcome measures of patients with severe mental disorders.
Materials and Methods:
Of a total 123 eligible patients with severe mental disorders, 61 patients were randomly assigned to the intervention group and 62 patients to the control group. The interventions included follow-up phone calls, home visits, and psychoeducation for families. Assessments were performed on hospital admission, discharge and the following 3rd, 6th and 12th month. Young Mania Rating Scale (YMRS), Hamilton Depression Rating Scale (HDRS), Positive and Negative Syndrome Scale (PANSS), Global Assessment of Functioning (GAF), Clinical Global Impression (CGI), and the World Health Organization Quality of Life Questionnaire (WHO-QOL) were used. Data were analyzed through Chi square, t-test, Mann-Whitney-U, and Repeated Measures Analysis of Co-Variance.
Results:
Mean of the HDRS scores revealed significant difference between the two groups when HDRS scores on the admission day were controlled (P = 0.028). The level of functioning was significantly different between the two groups based on the sequential assessments of GAF (P = 0.040). One year after the onset of trial, the number of psychiatric readmissions were significantly different between the two groups (P = 0.036).
Conclusion:
Readmission rates could be reduced by aftercare services, through the first year, after discharge of patients with severe mental disorders. On the other hand, higher levels of functioning would be expected after one year.
Keywords: Aftercare services, global assessment functioning, mental disorders, quality of life, readmission
INTRODUCTION
Mental disorders are associated with a considerable burden of disease directly because of relative high estimates of prevalence, mortality, disabilities, and costs.[1,2,3] These disorders may also be the risk factors for many other health problems, e.g., somatic diseases, substance misuse, drug side effects, and suicide.[4] They may also contribute to social problems such as poverty, marginalization, and social disadvantage. Finally, they directly or indirectly are held up progress toward achievement of many of the Millennium Development Goals.[5,6]
Considering this serious burden, accurate and effective management has been believed as an essential component of any mental health programs. Hospitalization, pharmacotherapy, and psychotherapy for patients with severe psychiatric disorders have been effective interventions, worldwide. However, most of the patients experience prolonged hospitalizations and repeated readmissions that impose grave burden not just on patients’ quality of life but on fragile financial resources of mental health programs.[7,8]
After beginning of deinstitutionalization reform, clear change happened in the strategy of mental health services. Key to this philosophy is the concept that the needs of patients with severe mental disorders best served when mental healthservices are centered on the individual patient, sensitive to the family, and founded on the community resources.[7,8,9] One of the essentials of deinstitutionalization reform is the principle of “continuity of care”.[10] A basic assumption of the continuum of care is that patients, who passed a period of hospitalization due to severe psychiatric disorders, should be able to move easily between different outpatient settings to prevent relapse and subsequent readmission.[11] However, gaps in continuity of care for patients with severe mental disorders may occur similar to those of other chronic medical conditions.[12] Poor insight, non-adherence to treatment, and weak financial support are additional causes for interruption in continuity of care in patients with mental disorders.[13,14,15,16,17]
Body of evidence attests to the importance of aftercare programs for patients’ continuity of care. Regarding aftercare, different services have been designed to discuss possible solutions, such as intermediate settings (“step-down” services), residential treatment centers, or home-based facilities.[18] Of the home-based services, case management,[19] follow-up phone calls,[20,21,22] or home visits are the most common.[23,24,25,26]
In developed countries, aftercare programs have been based on Community Mental Health Centers (CMHCs) and their social workers. However, in middle and low-income countries, establishment of classic CMHCs may hardly be attainable. For example, employment of social workers in delivery of mental healthcare has faced enormous challenges. Therefore, instead of social workers, engagement of supportive families in the programs would be one of the feasible approaches for integration and effectiveness of existing aftercare services.[27,28,29] However, it is not known, whether participation of family members in aftercare services prevents readmission, and predicts better post-discharge adherence.
Although aftercare services have been scaled up to developing countries, most of the countries have no mechanisms to monitor progress.[30] In Iran, as a developing country, scattered studies revealed controversial results about impact of aftercare services on outcome of management of severe mental disorders.[26,31,32,33] Objective of this study was to investigate whether the defined aftercare program and psycho-education for family members were associated with change in re-hospitalization rate, quality of life, level of functioning, and severity of psychopathology.
MATERIALS AND METHODS
This study was a quasi-experimental, prospective randomized controlled trial registered in the Iranian Registry of Clinical Trials and approved by the Deputy of Research of Isfahan University of Medical Sciences and Ethics Committee.
Participants
Participants were patients with severe mental disorders, who were admitted to Nour hospital, affiliated to Isfahan University of Medical Sciences, Isfahan, Iran, from April 2009 to August 2011. The inclusion criteria were:
diagnoses of acute episodes of Bipolar I Disorder (mania or mixed), schizophrenia, or schizoaffective disorder based on the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV),[34]
history of at least one previous hospitalization,
age between 18 and 65 years,
permanent address in Isfahan,
living with his or her family.
The exclusion criteria were:
neurological disorders,
substance dependency,
severe general medical diseases, and
cognitive impairment, severe enough to preclude informed consent.
Sampling
Of a total 1187 patients with severe mental disorders who were admitted to Nour hospital from April 2009 to July 2010, 123 patients met the inclusion criteria. Out of the total, 482 patients did not have history of previous hospitalization and 391 patients were not permanent address in Isfahan. Total of 103 patients did not sign the agreement for research and 88 of them had severe substance related disorder, medical disease, or cognitive disorder. Of 123 eligible patients, 61 patients were randomly assigned to the intervention group and 62 patients to the control group. Patients or their legal guardians were given detailed information about the study, and written consents were obtained.
Interventions
The interventions included weekly follow-up phone calls, monthly home visits, and psycho-education sessions for family members. For ethical respects, these interventions offered to the control group after the end of this study. Both of the groups received routine psychiatric treatments.
In follow-up phone calls, current mental state of the patients was asked; the patient was prompted to adhere more to treatment, and emergency psychiatric intervention was provided if needed.
The home visit team consisted of a trained general practitioner and a clinical psychologist. They assessed patients’ mental and physical state, prescribed the drugs, and arranged professional psychiatric interventions, if needed.
The psycho-education program included six sessions. The heading of these sessions are as the following: First session on introduction of family education and story of families, the second session on explanation of psychiatric disorders and symptoms, the third session on treatment and follow-up, the fourth on grounds of family help, the fifth session on problem solving methods, and the final session on specific issues and crisis intervention.[35]
The team also included a chief psychiatrist, who was the senior executive of the project, and two psychiatrists as consultants. The team received 30 hours of theoretical and practical training before the onset of the study. The whole group gathered for weekly meetings in Nour hospital to review the process, to give feedback, and to solve the problems.
Instruments
The severity of psychopathology in all patients of the two groups was assessed by “Young Mania Rating Scale” (YMRS),[36,37] “Hamilton Depression Rating Scale” (HDRS),[38] and “Positive and Negative Syndrome Scale” (PANSS).[39] Global Assessment of Functioning (GAF),[40] Clinical Global Impression-severity index (CGIS),[41] and the WHO Quality of Life Questionnaire (QOL)[42] were also used. All patients were evaluated at the time of admission, on hospital discharge and in the 3rd, 6th, and 12th months after discharge. The clinical rater who rated the patients and filled the questionnaires was different from the care providers, and blinded to the group allocation of the patients.
Data were analyzed through chi square and Repeated Measures Analysis of Co-Variance (ANCOVA). Age, gender, and scores of psychopathologies, GAF, CGIS, and QOL on admission day were considered as covariates.
RESULTS
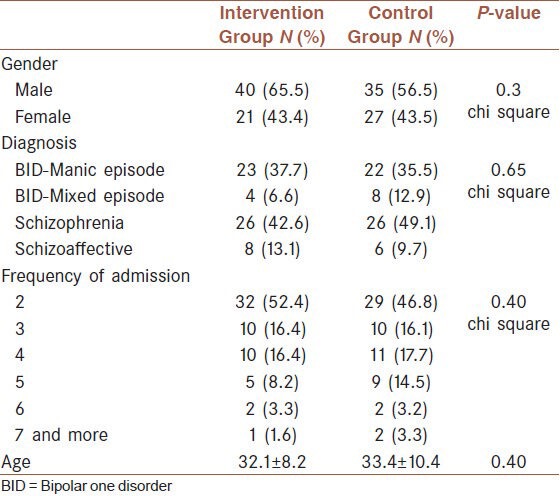
Table 1 presents the basic information of patients. Four patients in the intervention group and nine patients in control group withdrew consents at time of discharge. Three patients in intervention group and seven patients in control group did not find for evaluation at the third month after discharge. One patient died because of suicide in intervention group. At the end of the study, one more patient died in the intervention group due to suicide and two more patients were not accessible in control group.
Table 1.
Baseline characteristics of patients
There was not any significant difference between the two groups in terms of sequential assessments of CGIS scores on hospital discharge, and in the 3rd, the 6th, and the 12th month following it (P = 0.437). There was no significant differences between the CGIS scores of the two groups when age, gender and the CGIS score on admission day were controlled (P > 0.05) [Table 2]. Figure 1 presents the changes in the mean CGIS scores of each group during the course of the study.
Table 2.
Sequential measures of patients
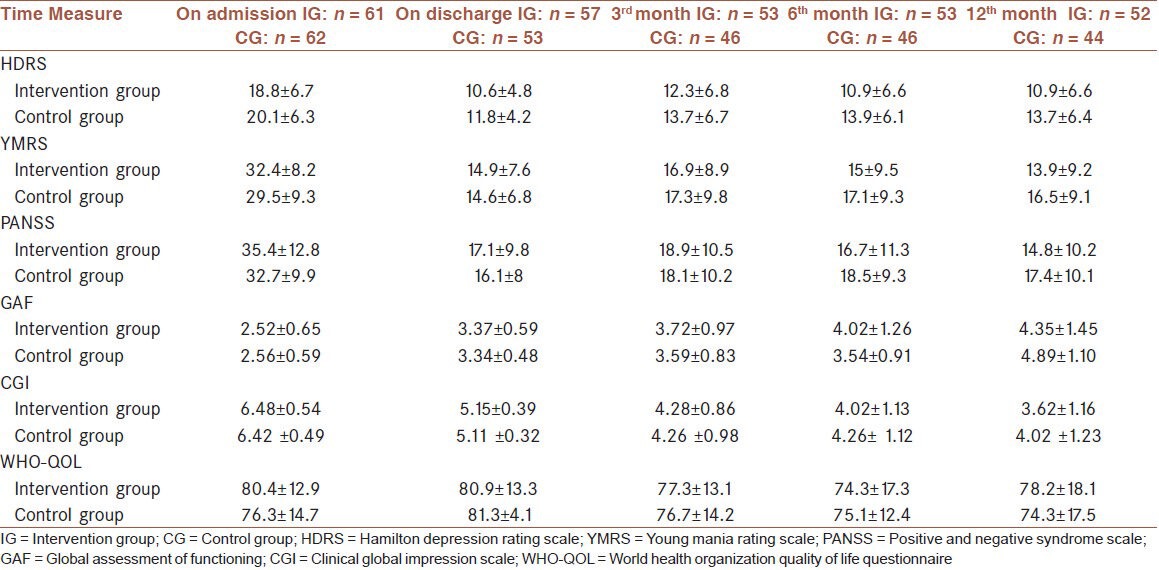
Figure 1.
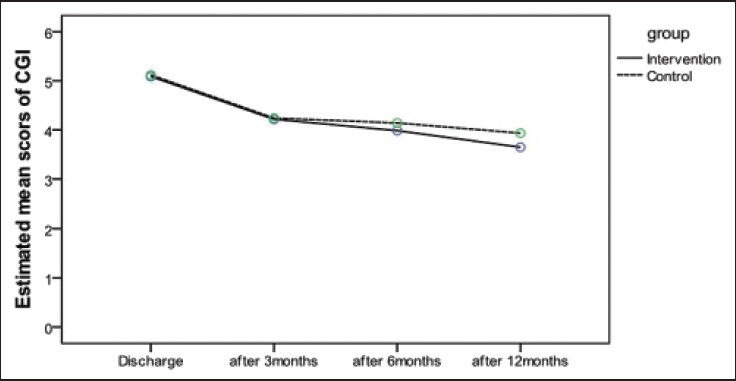
Changes in the mean CGIS scores of each group during the course of the study
Data analysis also indicated that the severity of depressive symptoms was not significantly different between the groups based on the sequential assessments of HDRS (P = 0.856). There was no significant differences between the HDRS scores of the two groups when age and gender were controlled (P > 0.05). However, HDRS scores revealed significant difference between the two groups when HDRS score on the admission day were controlled (P = 0.028) [Table 2]. Figure 2 represents the changes in the mean HDRS scores of each group during the course of the study.
Figure 2.
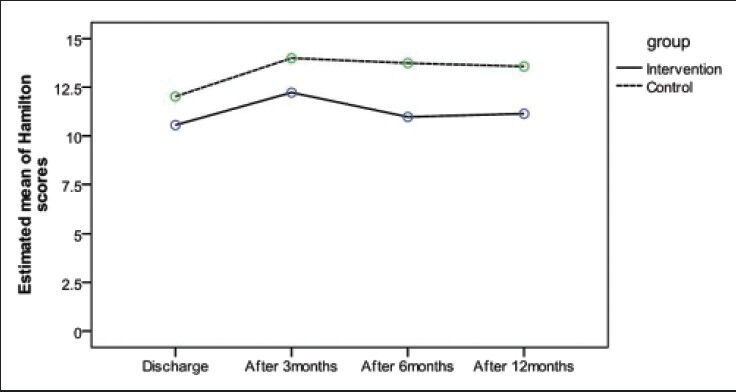
Changes in the mean HDRS scores of intervention and control groups during the course of the study
The severity of psychotic symptoms, which were evaluated through sequential rating of PANSS on discharge time, and in the 3rd, the 6th, and the 12th month following discharge, was not significantly different between the control and the intervention groups (P = 0.097). The difference was still insignificant after controlling variables of age, gender and admission day PANSS score (P > 0.05) [Table 2]. Figure 3 shows the changes of mean PANSS score during the course of the study.
Figure 3.
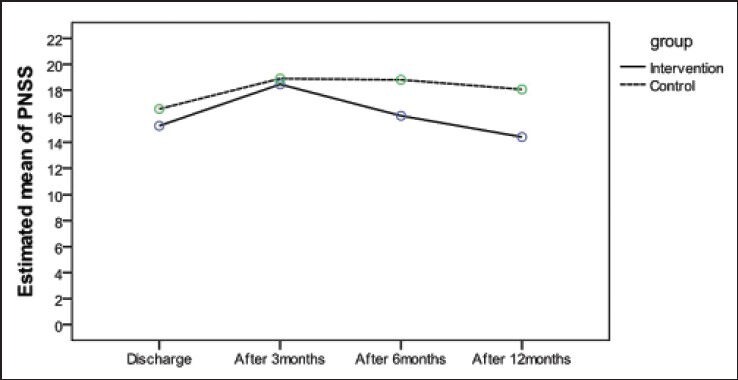
Changes of mean PANSS score in intervention and control groups during the course of the study
Moreover, the severity of manic symptoms, rated based on YMRS through sequential assessments, was not significantly different between the two groups (P = 0.065). The difference was still insignificant after controlling variables of age, gender and admission day YMRS score (P > 0.05) [Table 2]. Figure 4 indicates the changes in the mean YMRS score during the course of the study.
Figure 4.
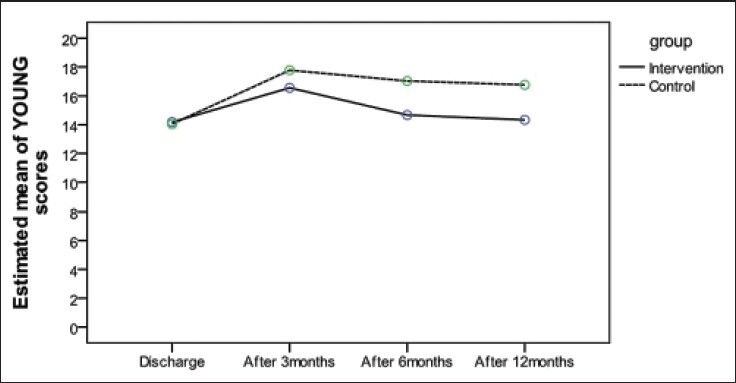
Changes in the mean YMRS score in intervention and control groups during the course of the study
The level of functioning was significantly different between the groups based on the sequential assessments of GAF (P = 0.040). Results can be viewed in Table 2. However, GAF scores were not significantly different between the two groups when age, gender, and GAF scores on the admission day were controlled (P > 0.05) [Table 2]. Figure 5 represents the changes in the mean GAF scores of each group during the course of the study.
Figure 5.
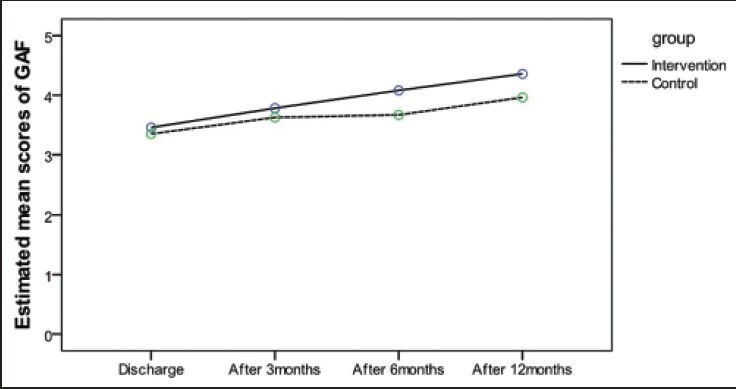
Changes in the mean GAF scores of each group during the course of the study
No significant differences were observed between the two groups, in terms of sequential assessments of QOL on hospital discharge, in the 3rd, the 6th, and the 12th month following discharge from the hospital (P = 0.446). There were no significant differences between the QOL scores of the two groups when age, gender and the QOL score on the admission day were controlled (P > 0.05) [Table 2]. Figure 6 presents the changes in the mean QOL scores of each group during the course of the study.
Figure 6.
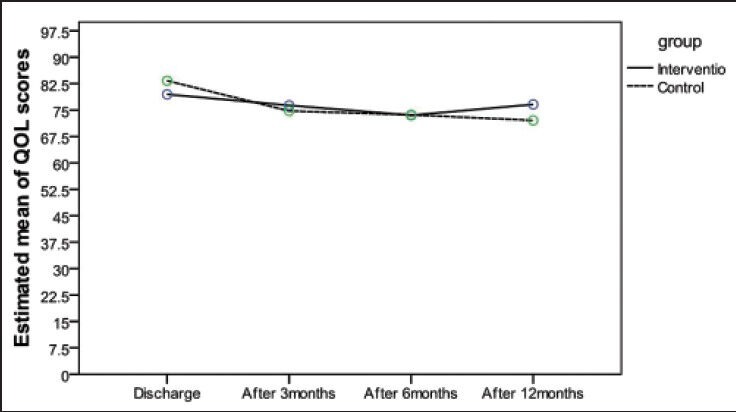
Changes in the mean QOL scores of intervention and control groups during the course of the study
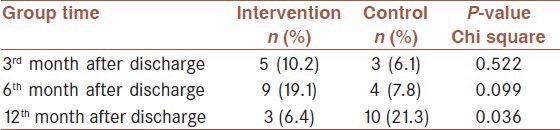
Regarding the frequency of re-hospitalization, no significant differences were observed between the two groups three (P = 0.552) and six months (0.099) following discharge from the hospital. However, one year after the onset of trial, the number of psychiatric re-hospitalizations was significantly lower in the intervention group (P = 0.036) [Table 3].
Table 3.
Rates of re-admission after discharge
Analysis of frequencies of referring to psychiatrist and level of drug compliance did not reveal significant differences between the two groups in the 3rd (P = 0.639), the 6th (P = 0.686), and the 12th months (P = 0.795) following discharge.
DISCUSSION
Our study revealed that psychiatric readmissions could be reduced by aftercare services, through the first year, after discharge in patients with severe mental disorders. These findings are similar to other studies that reported reduction in total days of hospitalization and number of readmissions.[24,43,44] Although, sum of the number of the re-admissions were equal for both groups, 3 patients in the intervention group were repeatedly admitted for 8 times. Whereas in the control group, there were 2 patients with 5 re-admissions. In addition, temporal distributions of re-hospitalizations were not same in the 2 groups. So, different patterns of distributions might have a role in this clinically significant finding. This result was similar to findings of other studies that reported reduction in total days of hospitalization and number of readmissions.[24]
Severity of depressive symptoms was also decreased during the first year after discharge, which were consistent with previous studies.[45]
The results also showed that aftercare services could also be associated with higher levels of functioning after one year. Whereas other studies reported opposite findings or revealed controversies regarding GAF level.[14,46,47]
Regarding symptomatic re-admission and severity of psychopathology, there was no clear effect, which specifically could be attributed to aftercare services, except for depression. There may be two possible explanations for this finding. The first one is simple: Aftercare service is ineffectual. Another interpretation, however, is also possible: As referrals to psychiatrist or receiving the drugs were similar in both groups, the response rates regarding the severity of psychopathology were also similar.
This study was limited in some ways. First, patients were not homogeneous regarding their psychiatric diagnoses. Second, combining follow-up phone calls and home visit might obscure the conclusion that which one is more effective? Third, studies with larger samples and longer follow-up duration are needed for strengthening these results. Finally, we had two cases of suicide in the intervention group, which we were not capable of clarification.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Geneva: [Last accessed on 2012]. World Health Organization. Global Burden of Disease 2004 Update. Available from: http://www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_full.pdf . [Google Scholar]
- 2.Baxter AJ, Charlson FJ, Somerville AJ, Whiteford HA. Mental disorders as risk factors: Assessing the evidence for the Global Burden Of Disease Study. BMC Med. 2011;9:134. doi: 10.1186/1741-7015-9-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Measuring the global burden of disease and risk factors, 1990-2001. In: Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ, editors. Global Burden of Disease and Risk Factors. Washington DC: The World Bank; 2006. pp. 1–13. [Google Scholar]
- 4.Ezzati M, Vander Hoorn S, Lopez AD, Danaei G, Rodgers A, Mathers CD, et al. Comparative quantification of mortality and burden of disease attributable to selected risk factors. In: Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL, editors. Global burden of disease and risk factors. New York: Oxford University Press; 2006. pp. 241–68. [PubMed] [Google Scholar]
- 5.Tunstall-Pedoe H. WHO Global Report. Geneva: World Health Organization; 2005. Preventing Chronic Diseases. A Vital Investment; p. 200. [Google Scholar]
- 6.Skeen S, Lund C, Kleintjes S, Fisher A MHAPP Research Programme Consortium. Meeting the millennium development goals in Sub-saharan Africa: What about mental health? Int Rev Psychiatry. 2010;22:624–31. doi: 10.3109/09540261.2010.535509. [DOI] [PubMed] [Google Scholar]
- 7.Botha UA, Koen L, Joska JA, Parker JS, Horn N, Herimg LM, et al. The revolving door phenomenon in psychiatry: Comparing low-frequency and high-frequency users of psychiatric inpatient services in a developing country. Soc Psychiatry Psychiatr Epidemiol. 2010;45:461–8. doi: 10.1007/s00127-009-0085-6. [DOI] [PubMed] [Google Scholar]
- 8.Bachrach LL. Deinstitutionalization: Promises, problems, and prospects. In: Knudsen HC, Thornicroft G, editors. Mental Health Service Evaluation. Cambridge: Cambridge University Press; 1996. pp. 3–18. [Google Scholar]
- 9.Lamb HR, Bachrach LL. Some perspectives on deinstitutionalization. Psychiatr Serv. 2001;52:1039–45. doi: 10.1176/appi.ps.52.8.1039. [DOI] [PubMed] [Google Scholar]
- 10.Bachrach LL. A conceptual approach to deinstitutionalization. Hosp Community Psychiatry. 1978;29:573–8. doi: 10.1176/ps.29.9.573. [DOI] [PubMed] [Google Scholar]
- 11.Joyce AS, Wild TC, Adair CE, McDougall GM, Gordon A, Costigan N, et al. Continuity of care in mental health services: Toward clarifying the construct. Can J Psychiatry. 2004;49:539–50. doi: 10.1177/070674370404900805. [DOI] [PubMed] [Google Scholar]
- 12.Adair CE, McDougall GM, Mitton CR, Joyce AS, Wild TC, Costigan N, et al. Continuity of care and health outcomes among persons with severe mental illness. Psychiatr Serv. 2005;56:1061–9. doi: 10.1176/appi.ps.56.9.1061. [DOI] [PubMed] [Google Scholar]
- 13.Mitton CR, Adair CE, McDougall GM, Marcoux G. Continuity of care and health care costs among persons with severe mental illness. Psychiatr Serv. 2005;56:1070–6. doi: 10.1176/appi.ps.56.9.1070. [DOI] [PubMed] [Google Scholar]
- 14.Kampman O, Illi A, Poutanen P, Leinonen E. Four-year outcome in non-compliant schizophrenia patients treated with or without home-based ambulatory outpatient care. Eur Psychiatry. 2003;18:1–5. doi: 10.1016/s0924-9338(02)00006-8. [DOI] [PubMed] [Google Scholar]
- 15.Hollingsworth EJ. Use of Medicaid for mental health care by clients of community support programs. Community Ment Health J. 1994;30:541–9. doi: 10.1007/BF02188591. [DOI] [PubMed] [Google Scholar]
- 16.Hunt AM, da Silva A, Lurie S, Goldbloom DS. Community treatment orders in Toronto: The emerging data. Can J Psychiatry. 2007;52:647–56. doi: 10.1177/070674370705201005. [DOI] [PubMed] [Google Scholar]
- 17.Unutzer J, Simon G, Pabiniak C, Bond K, Katon W. The use of administrative data to assess quality of care for bipolar disorder in a large staff model HMO. Gen Hosp Psychiatry. 2000;22:1–10. doi: 10.1016/s0163-8343(99)00057-2. [DOI] [PubMed] [Google Scholar]
- 18.Foster EM. Do aftercare services reduce inpatient psychiatric readmissions? Health Serv Res. 1999;34:715–36. [PMC free article] [PubMed] [Google Scholar]
- 19.Dieterich M, Irving CB, Park B, Marshall M. Intensive case management for severe mental illness. Cochrane Database Syst Rev. 2010;6:CD007906. doi: 10.1002/14651858.CD007906.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zanjani F, Bush H, Oslin D. Telephone-based psychiatric referral-care management intervention health outcomes. Telemed J E Health. 2010;16:543–50. doi: 10.1089/tmj.2009.0139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van den Berg N, Grabe HJ, Freyberger HJ, Hoffmann W. A telephone- and text-message based telemedical care concept for patients with mental health disorders--study protocol for a randomized, controlled study design. BMC Psychiatry. 2011;11:30. doi: 10.1186/1471-244X-11-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reda S, Makhoul S. Prompts to encourage appointment attendance for people with serious mental illness. Cochrane Database Syst Rev. 2001;2:CD002085. doi: 10.1002/14651858.CD002085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marshall M, Lockwood A. Assertive community treatment for people with severe mental disorders. Cochrane Database Syst Rev. 2002;2:CD001089. doi: 10.1002/14651858.CD001089. [DOI] [PubMed] [Google Scholar]
- 24.Burns T, Knapp M, Catty J, Healey A, Henderson J, Watt H, et al. Home treatment for mental health problems: A systematic review. Health Technol Assess. 2001;5:1–139. doi: 10.3310/hta5150. [DOI] [PubMed] [Google Scholar]
- 25.Burns T, Catty J, Watt H, Wright C, Knapp M, Henderson J. International differences in home treatment for mental health problems. Results of a systematic review. Br J Psychiatry. 2002;181:375–82. doi: 10.1192/bjp.181.5.375. [DOI] [PubMed] [Google Scholar]
- 26.Sharifi V, Amini H, Tehranidoost M, Yasamy MT, Jalali-Roudsari M, Roozbeh SP. Home care program for severe mental disorders; A preliminary report. Iran J Psychiatry. 2006;1:31–4. [Google Scholar]
- 27.Kelly M, Newstead L. Family intervention in routine practice: It is possible! J Psychiatr Ment Health Nurs. 2004;11:64–72. doi: 10.1111/j.1365-2850.2004.00689.x. [DOI] [PubMed] [Google Scholar]
- 28.Mottaghipour Y, Woodland L, Bickerton A, Sara G. Working with families of patients within an adult mental health service: Development of a programme model. Australas Psychiatry. 2006;14:267–71. doi: 10.1080/j.1440-1665.2006.02261.x. [DOI] [PubMed] [Google Scholar]
- 29.Adeponle AB, Thombs BD, Adelekan ML, Kirmayer LJ. Family participation in treatment, post-discharge appointment and medication adherence at a Nigerian psychiatric hospital. Br J Psychiatry. 2009;194:86–7. doi: 10.1192/bjp.bp.108.052217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jacob KS, Sharan P, Mirza I, Garrido-Cumbrera M, Seedat S, Mari JJ, et al. Mental health systems in countries: Where are we now? Lancet. 2007;370:1061–77. doi: 10.1016/S0140-6736(07)61241-0. [DOI] [PubMed] [Google Scholar]
- 31.Mottaghipour Y, Sharifi V, Salesian N, Seddigh A, Alaghband-rad J, Shahrivar Z, et al. Development and evaluation of culturally appropriate services for families of patients with first-episode psychosis in Iran. Schizophr Res. 2006;86:S149–50. [Google Scholar]
- 32.Malakouti SK, Nojomi M, Panaghi L, Chimeh N, Mottaghipour Y, Joghatai MT, et al. Case-management for patients with schizophrenia in Iran: A comparative study of the clinical outcomes of mental health workers and consumers’ family members as case managers. Community Ment Health J. 2009;45:447–52. doi: 10.1007/s10597-009-9197-4. [DOI] [PubMed] [Google Scholar]
- 33.Navidian A, Pahlavanzadeh S, Yazdani M. The effectiveness of family training on family caregivers of inpatients with mental disorders. Iran J Psychiatr Clin Psychol. 2010;16:99–106. [Google Scholar]
- 34.text revision. 4th edition. Washington, DC: American Psychiatric Association; 2000. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Diseases (DSM-IV) [Google Scholar]
- 35.Karamlou S, Mazaheri A, Mottaghipour Y. Effectiveness of family psycho-education program on family environment improvement of severe mental disorder patients. J Behav Sci. 2010;4:13–4. [Google Scholar]
- 36.Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: Reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–35. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- 37.Barekatain M, Tavakkoli M, Molavi H. Standardization, reliability, and validity of Young mania rating scale in Iran. J Psychol. 2007;11:150–66. [Google Scholar]
- 38.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–76. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 40.Patterson DA, Lee MS. Field trial of the global assessment of functioning-modified. Am J Psychiatry. 1995;152:1386–8. doi: 10.1176/ajp.152.9.1386. [DOI] [PubMed] [Google Scholar]
- 41.Guy W. Clinical Global Impressions Scale (CGI) In: Rush AJ, editor. Handbook of Psychiatric Measures. Washington, DC: American Psychiatric Association; 2000. pp. 100–2. [Google Scholar]
- 42.Nedjat S, Montazeri A, Holakooie K, Mohammad K, Reza M. Psychometric properties of the Iranian interview-administered version of the World Health Organization's Quality Of Life Questionnaire: A population-based study. BMC Health Serv Res. 2008;8:61. doi: 10.1186/1472-6963-8-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pai S, Channabasavanna SM, Raghura R. Home care for chronic mental illness in Bangalore: An example in the prevention of repeated hospitalization. Br J Psychiatry. 1985;147:175–9. doi: 10.1192/bjp.147.2.175. [DOI] [PubMed] [Google Scholar]
- 44.Gilis LS, Koch A, Jovi M. The value and cost effectiveness of home visiting programme for psychiatric patients. S Afr Med J. 1990;77:309–10. [PubMed] [Google Scholar]
- 45.Segre LS, Stasik SM, O’Hara MW, Arndt S. Listening visits: An evaluation of the effectiveness and acceptability of a home-based depression treatment. Psychother Res. 2010;20:712–21. doi: 10.1080/10503307.2010.518636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Malakouti K, Norouzi M. The role of follow-up and mental health programs in rehabilitation of chronic mental patients. Andishe va Raftar. 1985;2:41–54. [Google Scholar]
- 47.Malakouti K, Nouri-Ghasemabadi R, Nasr-Esfahani M, Esna-ashari R. The role of continuous care team on outpatient treatment of chronic psychiatric patients. Andishe va Raftar. 2001;4:5–13. [Google Scholar]


