Abstract
Background:
Postpartum depression is endangering the health of mothers and has negative impacts on the evolution of social communication and newborns evolution. This study was conducted to determine the effects of Fordyce Happiness program on the postpartum depression.
Materials and Methods:
This quasi-experimental intervention carried out on postpartum mothers that referred to 4 health centers in Isfahan. A total of 133 mothers were selected by convenient sampling and then randomly allocated in two groups (63 and 70 mothers for intervention and control respectively). Maternal depression 3 times before, immediate and 1 months after intervention in both groups was evaluated with Beck Depression Inventory-II-Persian standardized questionnaires. Educational sessions based on the Fordyce happiness program were conducted for intervention group. Data was analyzed in SPSS17 (SPSS Inc, Chicago, Illinois) descriptive and analytic statistical tests at significance level of 0.05.
Results:
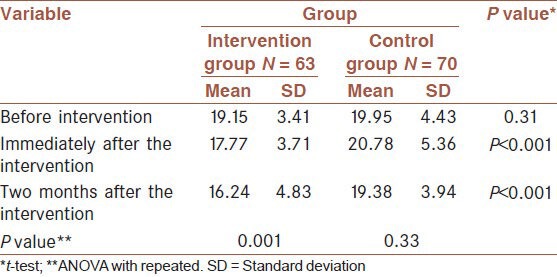
No significant differences in demographic variables between the two groups (P ≥ 0.05). No significant differences in depression scores in the two groups before training. However after 2 months a significant difference in depression score was observed between two groups (control group: 19.38 ± 3.94; intervention group: 16.24 ± 4.8; P < 0.001). Furthermore in intervention group showed significant differences in depression scores before and after intervention (19.15 ± 3.41 and 16.24 ± 4.83; P < 0.001). However in the control group had not any significant change.
Conclusion:
Fordyce happiness program was effective in reducing postpartum depression in our study. With attention to the effectiveness and low cost of this program, it is recommended that this program might be considered for all mothers after childbirth in health centers or other community-based settings.
Keywords: Fordyce happiness program, mothers, postpartum depression
INTRODUCTION
Obstetric and postpartum is the most critical stages of women's lives, which can affect the heavily feelings and thoughts of women.[1] During pregnancy and postpartum mood changes that made them very sensitive to emotional stimuli and sometimes caused mental problems.[2] The highest rates of psychiatric disorder in women 15-44 years old occurs in the first 2 months after delivery. Regarding mental disorder after delivery postpartum have been identified three major phenomena such as blues, postpartum depression and postpartum psychosis.[3] Symptoms of postpartum depression includes depressed mood, mental confusion, sleep and eating disorders, feelings of guilt and of inadequacy for caring neonate.[4]
Diagnostic Statistical Manual Mental Disorders-IV knows depression after the birth starting at 4 weeks after postpartum. Given the severity of the disorder that may continue up to 3-6 months and in rare cases up to 12 months after birth[5] The overall prevalence of postpartum depression is 10-15%.[6] However, there is evidence that Asian women are at greater risk.[7] Prevalence of postpartum depression in Iran has been reported 27.3% in 2004.[8]
Etiology of postpartum depression is still unknown. However, biological factors are involved such as estrogen levels drop suddenly after delivery, drop in progesterone, increased urinary excretion of cortisol and thyroid antibodies, prolactin and oxytocin and β endorphins.[9]
It is worth noting that most studies has been reported commonly risk factors associated with paranoid personality disorder, were factors such as maternal age, professional status and income instability, marital discord and crisis in the 1st years before the birth.[9]
Maternal depression in the 1st weeks and months after childbearing may undermine the relationship between mother and child and can lead to the emergence of behavioral problems later in childhood.[10]
One of the factors that lead to decrease postpartum depression and therefore coping with stress is happiness.[11] Happiness is an inner sense with inner sources that has as well as outer effect. Happiness is degree of judge or extent of a quality of life and utility of person's. Happiness means that how likes person his/her life's.[12]
The most common mode of our mental state is happiness. Barriers to access and experience that we are happy or put away negative acquired processes. When we discover an inherent positive feelings and keeps us from barriers that getting it out of the way, we achieve experience more meaningful and beautiful life. These positive emotions are not simply changing with other events and things, but their influence in our lives are inevitable. Attention to this state allows us to be more alive and unpretentious. What's the status of this positive outlook justified or not.[13]
Maeland has identified three different meanings for Health: Absence of disease, personal characteristics and mode of relaxation, well-being and happiness.[14] Human desire for happiness is easy to engage in social activities. Therefore, happiness is expressed by the social glue is ties that attached to each other.[15]
Happy people have high self-esteem, self-respect and self-love, These people have paid much attention to ethics and behave rationally.[16]
Lack of happiness can be stressful and stress can cause serious illness.[17,18] Happiness is necessary for mental development and is useful because it helps to cope with stress. Some experts believe that the first condition for the establishment of health, is happiness.[19] Those who are happy, feel more security, easier to decide, have more collaborative spirit and are more satisfied with their lives.[20]
Lama and Katler (2003) believes that the first step to gain to happiness, is learned it and can be taught to people to learn how to be happy.[21] One way rejoicing education model, is Fordyce happiness.
Fordyce (1983) has developed a program to increase the happiness of the community consists of 14 elements. This program has eight cognitive element and six elements of behavioral. She believes that with educating these components, individuals are able to increase their happiness.[22]
A study by Moradi et al. (2007) conducted a study with used Fordyce methods to increase happiness of teachers in Isfahan city discovered positive impact on the business practices of teachers happily.[22]
Considering the negative consequences of the postpartum depression for the mother and child and the impact of Fordyce happiness program on different groups in literature reviews and with regard to the novelty of present study to observed the effect of Fordyce happiness model on postpartum depression, the research was perform this study in 2011-2012 years in Isfahan and promising results for a way to control and reduce postpartum depression in the mothers.
MATERIALS AND METHODS
This quasi-experimental intervention carried out in 2011-2012 on the postpartum mothers that referred to 4 health centers in Isfahan. A total of 133 mothers were selected by convenient sampling and then randomly allocated in two groups (63 and 70 mothers for intervention and control respectively). Inclusion criteria: included was mothers experiences delivery in the last 4-8 weeks, having depression score above 16, minimum age 17 years and maximum 35 years and literate mothers. “Exclusion criteria were: mothers with past history of depression, history of infertility or recurrent abortion, fetal abnormality in past or current pregnancy and a premature or stillbirth and depression score below 16 were not included in the study. Also participants who became suicidal or psychotic which needed medications were excluded”.
In this study data 3 times before, immediate after and 2 months after intervention in both groups were evaluated with the demographic questionnaire and Persian-language version of the Beck Depression Inventory (BDI-II-Persian) by self-report method.
Demographic questionnaire has contains 8 questions including age, occupation, education, income adequacy, unwanted pregnancy, history of premenstrual syndrome (PMS), satisfaction with infant gender, history of abortion and Persian-language version of the BDI-II-Persian has contains 21 questions in a Likert scale of 4°, which was graded as 0-3. Maximum and minimum scale score was of 63 and zero.
This questionnaire showed distribution in patients with these conditions to each of questions in order to: Social isolation, lack of assertiveness, lack of decision making, flexibility, fatigue, loss of appetite, weight loss, health concerns, reduced sexual interest, sadness, pessimism, sense of failure, dissatisfaction, guilt, expectation of punishment, self-hate, self-blame, suicidal ideas, crying, changing attitudes about body image, insomnia and feeling of displeasure.
The scale range is as follows: 0-9 normal, 10-19 mild depression, 20-29 moderate depression and 30-63 severe depression.
In a study by Ghassemzadeh et al. BDI-II-Persian had high internal consistency (Cronbach's alpha = 0.87) and acceptable test-retest reliability (r = 0.74).[23]
In this study, after the mothers were divided randomly into two groups and after doing pre-test, education was conducted for mothers of intervention group in meeting room in one of the health centers. The education was done by trained instructor and dominates on Fordyce happiness program and its duration was eight sessions and each session about 1-1.5 h. (two sessions in a week) and conducted with Lecture, discussion and question - response methods. Hence half time of each session was devoted to presentations of the meeting and after a rest period, the second half of the training session was devoted for group discussion on the subject and question and answer exercises. At the end of each session, assignment was offered to all women in out of positions of educational topics for exercise.
Outlines of the intervention program includes
First session: Definition of depression and symptoms of postpartum depression, definition of happiness, the necessity and importance through review of studies on happiness.
Second session: Techniques to increase physical activity — being productive and doing something useful and meaningful techniques.
Third Session: Techniques of principles for better planning and organization - techniques for off the concerns — techniques to reduce the demands and wishes.
Fourth Session: Creativity increased techniques-moment living in the present techniques.
Fifth Session: social enhancement techniques — being real techniques.
Sixth Session: Techniques for increase intimacy as the primary source of happiness, prioritizing happiness, techniques and in valuing of great happiness.
Seventh Session: Techniques of expression and optimistic enhancement.
Eighth Session: An overview of all techniques, conducted a post-test (immediately) and determination time of post-test (2 months later).
At the end of program, a summary of all happiness techniques overviewed with help of mothers and were asked questions about the current level of happiness and optimism of those. If they had questions about them, were answered by instructor. Then they were completed the BDI-II-Persian. Women for their participation in the program were acknowledged and time of follow-up session was set up for 2 months later.
BDI-II-Persian depression questionnaire was used to complete in control group. The results were reviewed and analyzed with statistical tests for the effectiveness of the Fordyce happiness program.
Data obtained from before and after of intervention in the two groups analyzed with using Chi-square tests, Mann-Whitney and Kruskal-Wallis in SPSS software version 17.
Ethical consideration
Ethics approval was obtained from vice-chancellery for research in Isfahan University of Medical Sciences. The participants in the intervention group were intimated with details of the study and were asked to read and sign a consent form and were assured of the confidentiality. Participation to study was voluntary; participants were given the opportunity to leave the study if they become uncomfortable. The control group was given the opportunity to participate in the Fordyce happiness program after the study was completed. Also, mothers who had severe depression were referred to a psychiatrist and counselor.
RESULTS
According to the findings obtained from this study, Chi-square and U-Mann Whitney test showed no significant differences in demographic variables between two groups (P ≥ 0.05) [Table 1].
Table 1.
Demographic and obstetric characteristics of the intervention and control groups
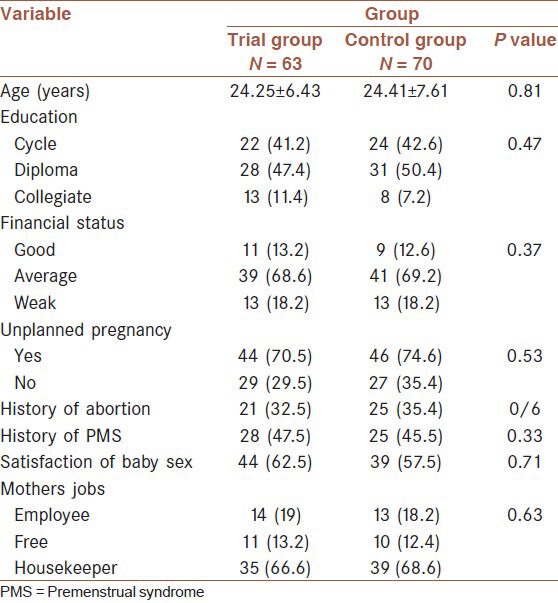
Among the demographic characteristics, Chi-square test showed statistical significant relationship between postpartum depression and other characters such as education level (P = 0.001) mothers job (P = 0.047), financial status (P = 0.01), unplanned pregnancy (P = 0.003), history of PMS (P = 0.021) and satisfaction of baby's gender (P = 0.037).
Mean age of the samples was 24.32 years (mean in intervention group 24.25 and control 24.41). 41.8% of samples were educated in cycle, 47.7% diploma and 12.5% had a college education. There was no significant difference between two groups in education level. This subject indicates that lower educational levels correlated with postpartum depression of mothers.
Majority of them had housekeeping Jobs (87.6%) and their husbands jobs was free (67%) and the economic status of women according to their self-report were moderated (59.9%), respectively.
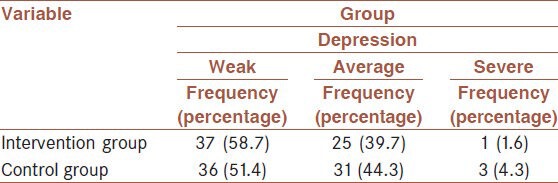
The frequency of depression among mothers showed that most mothers had mild depression in both groups [Table 2].
Table 2.
Distribution of maternal depression in both groups
Furthermore, independent t-test showed that there was no significant difference in depression score between two groups before intervention. But after the intervention, there was significant difference in depression score between two groups. The intervention group scores after intervention was better than the control group scores (16.24 ± 4.83 in intervention and 19.38 ± 3.94 in control respectively) (P < 0.001). Paired t-test showed significant differences in depression scores before and after the intervention group (P < 0.001). But the control group did not change significantly [Table 3].
Table 3.
Mean maternal depression at different times
DISCUSSION
The findings showed that, most mothers have average depression based on scores of the BDI-II-Persian. With regard the negative result of postpartum depression on child development and family processes attempt to identify related factors is inevitable.
The results of this study indicated that among demographic characteristics the educational levels and postpartum depression have statistical significant relationship. Hassan Zahraee results confirm these findings.[24] Also results of Tannous et al. and Segre et al. study confirm these findings that indicate lower education is associated with postpartum depression.[25,26] Education level as an effective component in better control and management of problems can be regarded as an indicator for health care providers. Therefore, health care providers in their plans and programs should be considering more attention to these high risk and sensitive groups.
In this study, significant relationship was shown between women job and postpartum depression symptoms but postpartum depression frequency was higher in employed women. This finding contrasts with that of Mazhari and Nakhaee study that postpartum depression was higher in housekeepers.[27]
This incompatible finding may be due to different working conditions for women.
In this study, there was not statistical significant relationship between postpartum depression and age. Although in some studies, low mother age is known risk factors and high mother age protective factors for postpartum depression.[2]
In contrast, in some communities, such as our community, high mother age was with number of children, Unwanted pregnancy and unwillingness to accept responsibility for taking care of other children in the imposition of financial problems following the birth of a new child,[25] Economic status is an independent variable that in the study is referred to as a risk factor,[2] also, in the study shown significant relationship between family income and maternal depression.
The results showed significant relationship between unplanned pregnancy and the postpartum depression. Some researchers believe that delivery is known one of pathologic stress to mothers. However, if this is the problem of unwanted pregnancy maternal multiply function conflict in the unwanted pregnancies that lead to a state of acceptance and rejection of infant. There are physical and psychological side-effects for women.[2]
Another important finding of the present study is the effects of Fordyce happiness program on postpartum depression.
Fordyce happiness intervention lead to significant differences in depression scores in the two groups’ intervention and control.
Mansouri in her studies showed that Fordyce happiness program was effectiveness training in reducing symptoms of PMS and increased happiness of women with PMS. Training eight sessions of Fordyce happiness program was effective to decrease the symptoms of PMS, anxiety, symptoms of PMS, irritable PMS symptoms, the physical symptoms of PMS and increased happiness[28] Mansouri findings coincide with the findings of this study focuses on the effectiveness of these programs and to control the transient symptoms of hormone imbalance can be used to greatly that health care providers can use this technique to learn and quick to help mothers at risk for mental disorders.
Alison study showed that the education of happiness lead to reduction depressed mood and increased happiness on New Zealand's Canterbury University students[29] In this regard it should be noted that mothers after childbirth if participated to this programs to control his depression, can be happier and have higher capacity to be more successful in their life.
Another study that conducted in 2007 by Bitsko et al. delights the effect of happiness program on quality of life and depression in adolescents with leukemia in Virginia in United States. Eight sessions of training happiness programs decrease depressive symptoms and improve quality of life in adolescents with leukemia in Virginia, USA.[30] This study was obtained outcomes such as study of Bitsko that focus on putting eight sessions.
Findings of other researchers suggested that mothers with depression after delivery have been unable to applied effective coping strategies to adapt with their problem. Therefore, they must use behavioral-cognitive interventions strategies for success in this field.[31]
This study carried out with the aim of management postpartum depression in mothers. Due to ease of implementation, effectiveness, availability and low costs of financing needed as a current challenges in health care system, would recommend the use of such program as a safe and free of any risk for the mother and the child and family.
There are several limitations involved in this study which must be addressed. Initially, the more serious concern is about the validity and accuracy of self-reported data regarding postpartum depression; further researches must use combination of self-report and clinical interview used to diagnose postpartum depression. Due to the small sample size, generalization of the results must be interpreted with caution and continued research should include larger sample sizes to draw more accurate conclusions. Another limitation of this study is not addressing the underlying factors of postpartum depression; future studies should focus on life crises, social support and marital satisfaction.
CONCLUSIONS
Based on the results of this study, Fordyce happiness program was effective in reducing postpartum depression. So with consider that this program to be effective and without being charged for women, it is recommended that this program be considered for all mothers after childbirth in health centers or other community based settings.
ACKNOWLEDGMENT
This article resulted from a project in Isfahan University of Medical Sciences. Project's number was 290372. We would like to acknowledge of family health personnel in selected health centers and all mothers participating in this study for their devotional corporation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Pazandeh F, Sheikhan Z, Someah NS. 1st ed. Tehran: Tohfeh Publication; 2007. Psychological Health and Woman; p. 70. [Google Scholar]
- 2.Korja R, Savonlahti E, Haataja L, Lapinleimu H, Manninen H, Piha J, et al. Attachment representations in mothers of preterm infants. Infant Behav Dev. 2009;32:305–11. doi: 10.1016/j.infbeh.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 3.McGarry J, Kim H, Sheng X, Egger M, Baksh L. Postpartum depression and help-seeking behavior. J Midwifery Womens Health. 2009;54:50–6. doi: 10.1016/j.jmwh.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 4.O’Hara MW. The nature of postpartum depressive disorders. In: Murray L, Cooper PJ, editors. Postpartum Depression and Child Development. New York: Guilford Press; 1997. pp. 3–31. [Google Scholar]
- 5.Cunningham FG, Williams JW. 22nd ed. New York: McGraw Hill; 2005. Williams Obstetrics; pp. 1241–4. [Google Scholar]
- 6.Bloch M, Rotenberg N, Koren D, Klein E. Risk factors for early postpartum depressive symptoms. Gen Hosp Psychiatry. 2006;28:3–8. doi: 10.1016/j.genhosppsych.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 7.Werrett J, Clifford C. Validation of the Punjabi version of the Edinburgh postnatal depression scale (EPDS) Int J Nurs Stud. 2006;43:227–36. doi: 10.1016/j.ijnurstu.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 8.Behbodi Z. Master's Thesis. Tehran: School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences; 2001. Prevalence of postpartum depression in women referred to health centers for cane effective factors-martyr Beheshti University of Medical Sciences affiliated to Tehran University. [Google Scholar]
- 9.McCoy SJ, Beal JM, Shipman SB, Payton ME, Watson GH. Risk factors for postpartum depression: A retrospective investigation at 4-weeks postnatal and a review of the literature. J Am Osteopath Assoc. 2006;106:193–8. [PubMed] [Google Scholar]
- 10.Henderson C, Macdonald S. 13th ed. New York: Baillière Tindall; 2004. Mayes’ Midwifery: A Textbook for Midwives; p. 743. (925-9). [Google Scholar]
- 11.Steptoe A, Wardle J. Positive affect and biological function in everyday life. Neurobiol Aging. 2005;26(Suppl 1):108–12. doi: 10.1016/j.neurobiolaging.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 12.Veenhoven R. The utility of happiness. Soc Indic Res. 1988;20:254. [Google Scholar]
- 13.Karleson R. Tehran: Psychometrics Publications; 2001. Live Happily (Translate: Daramadi SH) [Google Scholar]
- 14.Maeland J. [Health and the quality of life. Concepts and definitions] Tidsskrift for den Norske laegeforening: tidsskrift for praktisk medicin, ny raekke. 1989;109:1311–5. [PubMed] [Google Scholar]
- 15.Rio J. 1 ed. Tehran: Froozesh 2005; 2013. Motivation and emotion. [Google Scholar]
- 16.Stephan GP. Benevolent unlimited love happiness and health: Rx “do uuto others”. J Sci Healthy. 2005;1:360–4. doi: 10.1016/j.explore.2005.06.005. [DOI] [PubMed] [Google Scholar]
- 17.Mazaheri MA. Effect of educational intervention on general health and depression in temporary employees. Int J Prev Med. 2012;3:504–9. [PMC free article] [PubMed] [Google Scholar]
- 18.Mazaheri MA, Darani FM, Eslami AA. Effect of a brief stress management intervention on work-related stress in employees of Isfahan Steel Company, Iran. J Res Med Sci. 2012;17:S87–92. [Google Scholar]
- 19.Borgonovi F. Doing well by doing good. The relationship between formal volunteering and self-reported health and happiness. Soc Sci Med. 2008;66:2321–34. doi: 10.1016/j.socscimed.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 20.Subramanian SV, Kim D, Kawachi I. Covariation in the socioeconomic determinants of self rated health and happiness: A multivariate multilevel analysis of individuals and communities in the USA. J Epidemiol Community Health. 2005;59:664–9. doi: 10.1136/jech.2004.025742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lama D, Katler H. Tehran: Rasa Publications, Publications Clear; 2003. Art of Happy Life (Translat: Anoshirvani SH) [Google Scholar]
- 22.Moradi M, Jafari SE, Abedi MR. Impact of education on ways to increase happiness Fordays education of teachers in Isfahan. J Med Purifi. 2007;66-7:57–62. [Google Scholar]
- 23.Ghassemzadeh H, Mojtabai R, Karamghadiri N, Ebrahimkhani N. Psychometric properties of a Persian-language version of the Beck Depression Inventory - Second edition: BDI-II-PERSIAN. Depress Anxiety. 2005;21:185–92. doi: 10.1002/da.20070. [DOI] [PubMed] [Google Scholar]
- 24.Zahraee RH. First Congress of Nursing and Mood Disorders. Tabriz University of Medical Sciences; Research Council; 2000. Related factor of postpartum depression. [Google Scholar]
- 25.Tannous L, Gigante LP, Fuchs SC, Busnello ED. Postnatal depression in Southern Brazil: Prevalence and its demographic and socioeconomic determinants. BMC Psychiatry. 2008;8:1. doi: 10.1186/1471-244X-8-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Segre LS, O’Hara MW, Arndt S, Stuart S. The prevalence of postpartum depression: The relative significance of three social status indices. Soc Psychiatry Psychiatr Epidemiol. 2007;42:316–21. doi: 10.1007/s00127-007-0168-1. [DOI] [PubMed] [Google Scholar]
- 27.Mazhari S, Nakhaee N. Validation of the Edinburgh Postnatal Depression Scale in an Iranian sample. Arch Womens Ment Health. 2007;10:293–7. doi: 10.1007/s00737-007-0204-x. [DOI] [PubMed] [Google Scholar]
- 28.Mansori Z. Tehran: Al-Zahra University. Faculty of Education and Psychology; 2006. Effects of cognitive training - The joy of behavioral symptoms of premenstrual syndrome in women of Isfahan. Thesis (MA) pp. 113–2. [Google Scholar]
- 29.Alison OP. A Thesis Submitted in Partial Fulfillment of the Requirements for the Degree of Master of Science in Psychology in the University of Canterbury; 2007. Can happiness be taught? The effect on subjective wellbeing of attending a course in positive psychology that includes the practice of multiple interventions; pp. 64–77. [Google Scholar]
- 30.Bitsko MJ, Stern M, Dillon R, Russell EC, Laver J. Happiness and time perspective as potential mediators of quality of life and depression in adolescent cancer. Pediatr Blood Cancer. 2008;50:613–9. doi: 10.1002/pbc.21337. [DOI] [PubMed] [Google Scholar]
- 31.Logsdon MC, McBride AB, Birkimer JC. Social support and postpartum depression. Res Nurs Health. 1994;17:449–57. doi: 10.1002/nur.4770170608. [DOI] [PubMed] [Google Scholar]


