Abstract
Background:
Regular follow up and amblyopia treatment are essential for good outcomes after pediatric cataract surgery.
Aim:
To study the regularity of follow-up after cataract surgery in children and to gauge the causes of poor compliance to follow up.
Subjects:
262 children (393 cataracts) who underwent cataract surgery in 2004-8.
Materials and Methods:
The children were identified and examined in their homes and a “barriers to follow-up” questionnaire completed. Demographic data collected, visual acuity estimated, and ocular examination performed.
Statistical Analysis:
SPSS version 19.
Results:
Of the 262 children, only 53 (20.6%) had been regularly following up with any hospital, 209 (79.4%) had not. A total of 150 (57.3%) were boys and the average age was 13.23 years (Std Dev 5 yrs). Poor follow up was associated with the older age group (P < 0.001), less education of mother (P = 0.012), father's occupation (P = 0.031), how much money spent on travel (P = 0.033) and was it paid or free surgery (P = 0.001). It was not related to gender, numbers of children in family, ordinal status of child, and social strata. Distance and cost were major barriers, as was the inability of the eye care center to communicate the importance of follow up. A prospective follow-up visit showed that 93 children needed Nd: YAG LASER capsulotomy, 5 needed low vision aids, 4 contact lens, and 162 a change of spectacles. The average visual acuity improved in 150 (38.8%) eyes >1 line with regular follow-up.
Conclusion:
Regular follow-up is important and improves vision; eye care practitioners need to take special efforts to ensure better follow-up.
Keywords: Barriers to follow-up, pediatric cataract, visual outcome
Cataract surgery in children is an important step to restore vision lost by pediatric cataract.[1] But the surgical intervention is just one step in a process to rehabilitate a child's vision. Proper postoperative medication, refractive correction, and amblyopia treatment are equally important.[1,2,3] While adult cataract surgery usually needs a 6-week follow-up, pediatric cataract surgeries need a longer follow-up to ensure proper anti-amblyopia treatment and spectacle compliance. India houses the largest population of blind and severely visually impaired children in the world and pediatric cataract forms a significant component of childhood blindness.[4,5,6,7] India may be home to the largest number of pediatric cataracts globally.[8] There are few studies from Nepal and India to document the outcome of pediatric cataract surgery but none with a follow up more than 1 year.[9,10,11] Studies from Mexico and Tanzania have demonstrated the predictors of good follow-up in children,[12,13] but there have been no such studies from India which has had one of the largest childhood blindness amelioration initiatives globally.[14] Neither is there any study about what happens to cataract-operated children if they do not attend regular follow-up. This study aimed to find the proportion of pediatric cataract-operated children who attended regular follow-up and the barriers which prevented others from doing so. We also studied the consequences of such a lack of follow-up.
Materials and Methods
The ethical committee of the institution approved the study. The study was completed between October 2010 and June 2011. From the medical records section, the case records of all 520 pediatric cataracts eyes who were operated for cataract surgery from 2004 to 2008 were obtained. The addresses of each and every child along with the phone numbers had been carefully recorded as they had been operated under the childhood blindness amelioration initiative undertaken by ORBIS International, India country office. The children were grouped according to talukas (sub-districts in Indian administration) and villages. A case-mapping exercise was conducted using various colored stickers to visualize the location of the children to be studied. A day-wise plan was made for community workers to visit the area and to identify and interview each child.
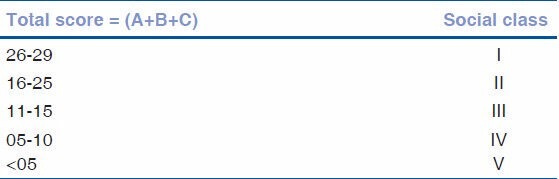
The “barriers to follow-up” questionnaire was designed using the questionnaire used by Rapid Assessment for Avoidable Blindness (RAAB) India study and more questions were added considering the pediatric population that was to be studied.[15] A brain storming session was conducted with all the participants (ophthalmologists, optometrists, social workers, and administrators) to come up with ideas regarding the information that would need to be collected by the social workers of the ORBIS supported pediatric ophthalmology department. The “barriers to follow-up questionnaire” was then translated into the regional language, Marathi, by two independent translators. The Marathi translations were once again translated back into English to check whether the content had been changed or lost during the translation. The questionnaire was then validated by a team of external reviewers. The community workers were again oriented to the questionnaire and various methods to administer it including direct questioning, catching the information during discussion or group discussions. To determine whether the parent's education, occupation, and socio-economic status had any effect on follow-up, the Kuppusamy classification for measuring socio-economic status was included in the questionnaire.[16] This has been enclosed as Apppendix A. The 2007 urban version was used to calculate the socio-economic class of the children's families, even though the children hailed from rural, peri-urban, and urban areas.
A training schedule was developed for the participating team. It stressed the significance of childhood blindness and pediatric cataract to the social workers.[17] They were trained how to use the “barriers to follow-up” questionnaire; how to use and complete the pediatric vision function questionnaire; and how they could help the pediatric ophthalmologists in collecting patient history and capturing data. Further training was imparted to enter the data in excel sheets and ways to maintain data accuracy and validity. Following the training, a pilot study was conducted in a nearby village of Savli, where 37 children, a sample size of 10%, were identified and counseled. A fortified training was then again conducted for the participating staff.
Children who could be traced were transported in a vehicle to the pediatric ophthalmology department of the hospital along with their parents for a comprehensive eye examination. The children underwent a complete ocular examination – visual acuity estimation, slit lamp examination, orthoptic evaluation, cycloplegic refraction, fundoscopy, tonometry, and stereopsis testing. Those needing Nd: YAG LASER posterior capsulotomy, other eye cataract or strabismus surgery, spectacles, and/or low vision aids were provided the same by the hospital free of cost.
In spite of house visits and counseling, 74 children did not visit examination center. A detailed program was made for house visits of these children by pediatric ophthalmologist, along with an optometrist and community workers, who visited these children at their home with the required equipments, such as portable visual acuity charts, portable slit lamp, Keratometer and A-scan, and examined these children.
Children who had attended an eye clinic at least once in the past year were considered to have a regular follow-up, those who did not were considered to have been poorly compliant for follow-up. Statistical analysis was performed using SPSS version 19.
Results
A total of 374 children (520 eyes) had been operated for pediatric cataract surgery by the hospital's pediatric ophthalmology department from 2004 to 2008 during the project with ORBIS International. Out of these, 262 (70.1%) children/393 pediatric cataract-operated eyes could be traced and were examined. 150/262 (57.3%) were males. Their ages ranged from 3 to 22 years. One hundred thirty-one (50%) had bilateral cataracts that were operated upon. The affected siblings had none to six siblings in the family. The ordinal status of the operated children in their family was as follows: Eldest 92 (35.1%), middle 65 (24.8%), and youngest 105 (40.1%). Thirty-nine (14.9%) children had another sibling who was similarly affected, of these 10 had two similarly (with cataract) affected siblings. Ninety-seven (37.2%) were operated as paid patients (paid >Rs. 3500), 92 (35.3%) as subsidized ones (paid <3500 but >0 rupees), and 72 (27.6%) as completely free. The average sum spent by parents was rupees 2306.5 (Std Dev 177).
The average age of children was 13.2 years (Std Dev 4.96). Out of 262 children, age groups of 0-5 years were 12 (4.6%), 6-10 years were 59 (22.5%), 11-15 years were 94 (35.9%), and 16-21 years were 97 (37.0%). They all aged <16 years at the time of surgery.
The socio-economic status of the children's family by the Kuppusamy classification was: Class I -highest socio-economic class were 2 (0.8%), class II were 13 (5.0%), class III were 75 (28.6%), class IV were 161 (61.5%), and 11 (4.2%) were from class V (poorest).
Of the 262 children, only 53 (20.6%) had been regularly following up with the hospital, 209 (79.4%) had not. Table 1 demonstrates the causes of non-attendance of follow-up after pediatric cataract surgery. The children or their parents did not consider attending the follow-up visit as a priority. The second most common cause was the lack of affordability.
Table 1.
Causes for not attending a regular follow-up
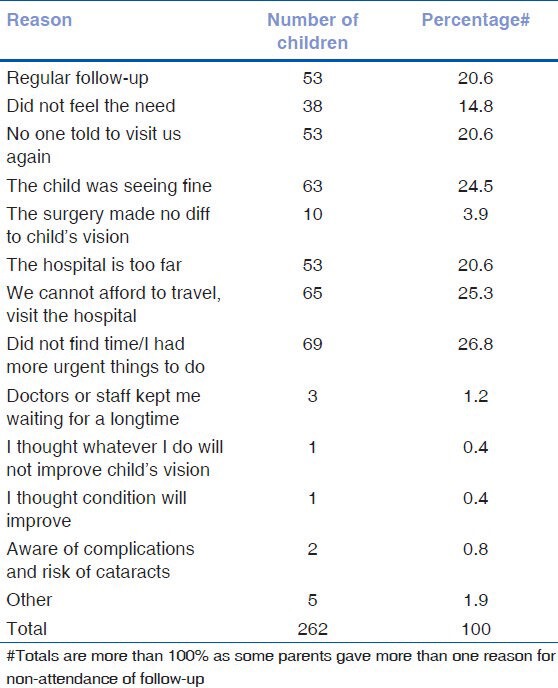
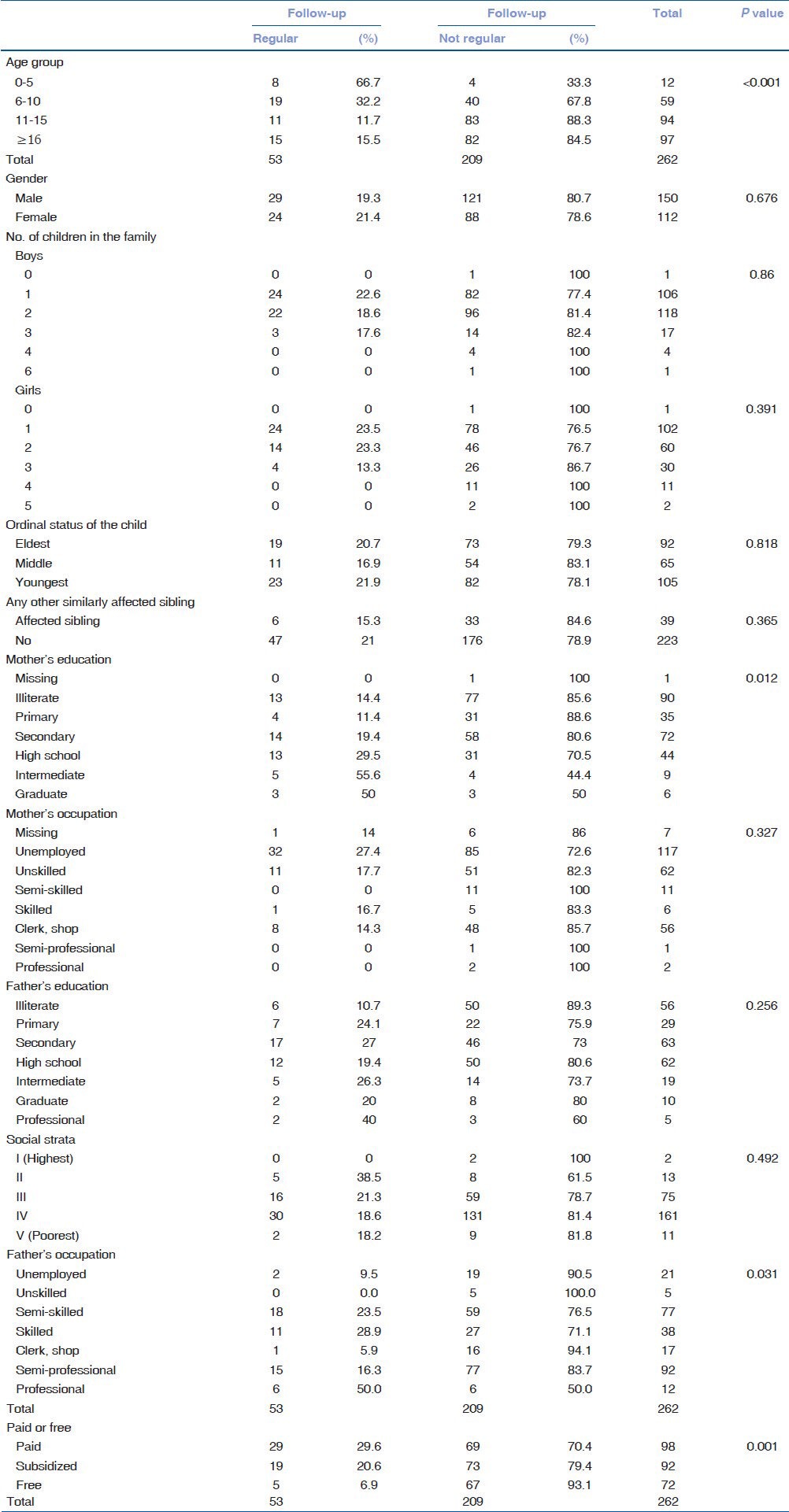
Table 2 shows the association of follow-up regularity with demographic factors.
Table 2.
Correlates of factors responsible for follow-up: Regular (Compliant) or not regular (Non-compliant)
Of the 262 children, 243 needed some kind of clinical intervention during the prospective follow-up visit. 103 eyes underwent Nd: YAG LASER capsulotomy and 33 needed surgery for strabismus or surgical capsulotomy; 173 children were dispensed new spectacles, 4 were given low vision aids, and 3 dispensed cosmetic contact lenses. Only 19 children did not need any kind of intervention. So the prospective follow-up program was greatly beneficial to the children.
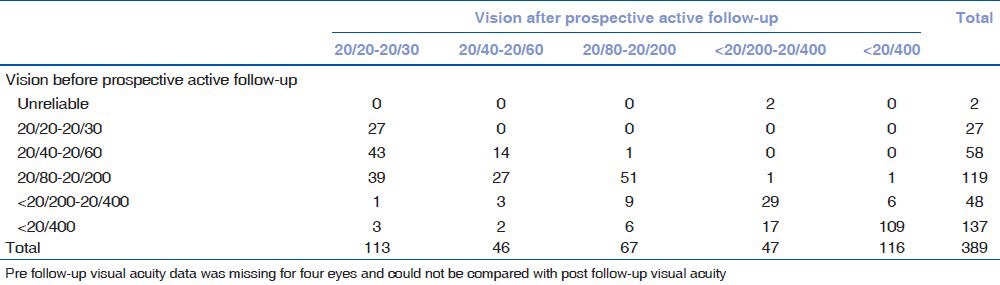
Table 3 compares the presenting vision (of the children) when they were examined for the follow-up visits with the visual acuity after active follow-up. While only 27 (6.9%) operated eyes had >20/30 visual acuity at presentation, it improved to 113 (29%) having visual acuity >20/30 after the prospective follow-up and interventions. 150 (38.8%) eyes gained more than one line of visual acuity, mostly due to a simple refraction and dispensing of spectacles and Nd: YAG LASER capsulotomy.
Table 3.
Vision before follow-up and intervention compared to vision after the follow-up
Discussion
This study looked at the compliance to follow up and its effect on visual acuity after pediatric cataract surgery in India. The compliance was poor (only 53, 20.6% attended regular follow-up), especially among older children. Gender, family income, and number of children in the family did not affect follow up compliance. Families who had more than one pediatric cataract affected child also did not have better follow-up, a bit like patients with family history of glaucoma not getting a regular ocular examination done and not having glaucoma detected at an early stage.[18,19] Less educated mother were more likely to have children with poor follow up, as were fathers engaged in unskilled work or unemployed. Children who were accompanied by a parent during surgery had a slightly better follow-up as compared to those accompanied by grand-parents, other relatives or neighbors, but this was not statistically significant. Older children had moved for study, work, and marriage. Sixteen girls in the sample had married and many had not told their in-laws regarding their condition. Younger children were deemed to be parent's responsibility and had a better follow-up. Children who were operated upon completely free were more likely to have a poor follow-up. While the center catered to mostly poor and middle class families, the follow-up was equally poor across all socio-economic classes. A study from north India comparing pediatric cataract surgery in eye camps and tertiary care center found the follow-up to be poor in eye camps and hence the outcomes were sub-optimal.[20]
Barriers of cost and distance (indirect cost) kept the children away from the eye care center. This was similar to findings from Tanzania and Mexico[12,13] If donors or Governments spent so much in providing free or subsidized pediatric cataract surgery, it made sense to expend slightly more resources to ensure better follow up as was done in Kilimanjaro, Tanzania.[13] 53 (20.6%) reported that the eye care professionals did not ask them to visit again. Comparing with adult cataract surgeries around them (and Sangli district has a very high cataract surgical rate with regular diagnostic and follow ups eye camps), parents thought that the job was over once the surgery was performed and spectacles prescribed! Ophthalmologists, Optometrists, and Social workers should stress the need for a repeated and regular check up for such affected children, a bit like immunization workers explaining the need for a regular dose of a vaccine. Only 63 (24.5%) reported that they thought child was seeing well and thus may not need another visit. Thirty-eight (14.8%) said they did not feel the need, while 69 (26.8%) reported that they did not have the time to visit. Parents from poor families may have other priorities so it is incumbent on eye care workers to stress the advantages of a regular follow-up. The objective of creating a child friendly pediatric eye care center seems to have been achieved as very few (3, 1.8%) reported waiting time or staff behavior as a barrier.
The active follow-up showed that 243/262 (92.7%) children needed some kind of intervention and their visual acuity improved as a result. The study from north India also stressed how regular follow-up and amblyopia management was needed to improve outcomes.[20] More than 30,000 surgeries had been performed in India and Nepal under the childhood blindness initiative of ORBIS International.[14] These and all other pediatric cataracts operated in government, non-government, and private set-ups would benefit from such a follow-up initiative.
Hospitals should insist on anterior vitrectomy and primary posterior capsulotomy for all children till 7-8 years of age or even older keeping in view the poor follow-up and ubiquity of posterior capsular opacification (PCO). Or do a prophylactic Nd: YAG LASER capsulotomy ay 1 or 6 weeks follow-up.
The children, parents, and relatives should be counseled about the importance of regular examination and follow-up right at the time of surgery itself. We need to encourage involvement of both parents during the course of the treatment of their child, from identification to follow-up. There should be a continuous development of child-friendly ambience of pediatric unit and child-friendly attitude of trained staff as enablers for greater acceptance of pediatric ophthalmology services.
Busy practitioners and pediatric eye care centers which cater to children from far-away places should identify partner's in the child's vicinity who shall take responsibility for the follow-up which includes visual acuity estimation, slit-lamp examination, fundoscopy, cycloplegic refraction, and amblyopia treatment.
There is a need for more effective follow-up mechanism in the outreach strategy of pediatric eye care programs, one that shall address the issues of affordability and accessibility among beneficiaries. We could combine case identification and post-operative follow-up in each of the outreach initiatives to enhance timely follow-up. The eye care centers could sponsor an annual week for pediatric cataract follow-up. There is a need to design, develop, and use appropriate tools to record and monitor post-operative surgical outcomes and compliance to follow-up of all beneficiaries on a continuous basis. These would encourage the center and its staff to consider follow-up a priority. This is all the more important as pediatric cataract surgeries are more cost intensive than adult cataract ones, costing on an average Rs. 4500-Rs. 17,000 to the service provider.[21] A sub-optimal result would mean a lot of these efforts gone in vain.
In conclusion, this study demonstrated the need for a more active follow-up after pediatric cataract surgery. This could be done by patient education, subsidizing follow-up visits, and networking with other eye care practitioners. The end result would be a child with better visual acuity after pediatric cataract surgery.
Acknowledgment
The clinical examination and data collection protocol was validated by Professor Clare Gilbert, (from the London School of Hygiene and Tropical Medicine/International Centre for Eye Health), Dr. Joan McLeod-Omnawale, ORBIS Director of Monitoring and Evaluation, Dr. Rupal Trivedi, Associate Professor, Storm Eye Institute, South Carolina, USA, Dr. H. Kishore, senior pediatric ophthalmologist, Al-Nahda Hospital, Muscat, Oman and Dr. Milind Killedar, pediatric ophthalmologist from Sangli, India. The final version was in concurrence of the authors with Dr. Lutful Hussain (from ORBIS Dhaka, Bangladesh). The authors thank Shrivallabh Sane for statistical analysis, Faiz Mushrif, Dr. Mohini Sahasrabudhe, Dr. Mitali Shah and Poonam Shinde for data collection and management.
Appendix A: Kuppusamy classification for calculating social status
Kuppusami’s method of classification (2007 revision)
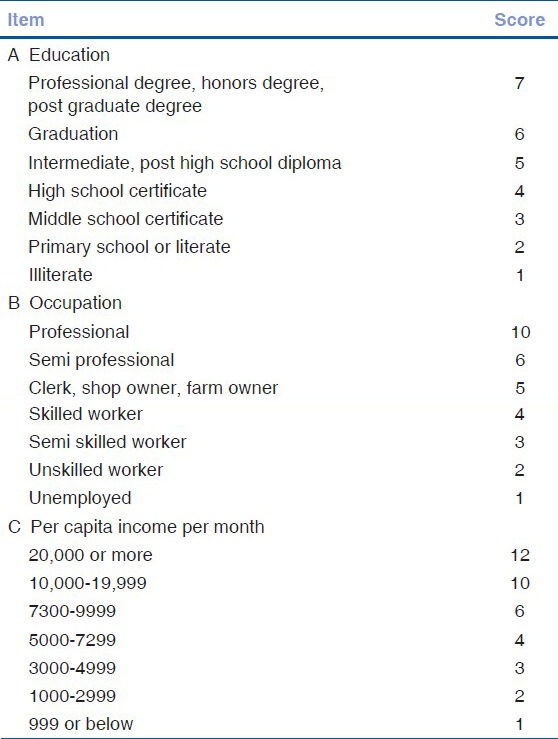
Calculation
Footnotes
Source of Support: USAID through the AED Operational research project under the A2Z child micronutrient program through the ORBIS International, New York.
Conflict of Interest: None declared.
References
- 1.Gilbert C, Foster A. Childhood blindness in the context of VISION 2020-the right to sight. Bull World Health Organ. 2001;79:227–32. [PMC free article] [PubMed] [Google Scholar]
- 2.Gogate P, Muhit M. Childhood blindness and cataract in developing countries. J Community Eye Health. 2009;22:4–5. [PMC free article] [PubMed] [Google Scholar]
- 3.Foster A, Gilbert C, Rahi J. Epidemiology of cataract in childhood: A global perspective. J Cataract Refract Surg. 1997;23:601–4. doi: 10.1016/s0886-3350(97)80040-5. [DOI] [PubMed] [Google Scholar]
- 4.Gogate P, Deshpande M, Sudrik S, Taras S, Kishore H, Gilbert C. Changing pattern of childhood blindness in Maharashtra, India. Br J Ophthalmol. 2007;91:8–12. doi: 10.1136/bjo.2006.094433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bhattacharjee H, Das K, Borah RR, Guha K, Gogate P, Purukayastha S, et al. Causes of childhood blindness in the northeastern states of India. Indian J Ophthalmol. 2008;56:495–9. [PMC free article] [PubMed] [Google Scholar]
- 6.Gogate P, Kishore H, Dole K, Shetty J, Gilbert C, Ranade S, et al. The pattern of childhood blindness in Karnataka, South India. Ophthalmic Epidemiol. 2009;16:212–7. doi: 10.3109/09286580902999405. [DOI] [PubMed] [Google Scholar]
- 7.Titiyal JS, Pal N, Murthy GV, Gupta SK, Tandon R, Vajpayee RB, et al. Causes and temporal trends of blindness and severe visual impairment in children in schools for the blind in North India. Br J Ophthalmol. 2003;83:941–5. doi: 10.1136/bjo.87.8.941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gilbert CE, Rahi JS, Quinn GE. Visual impairment and blindness in children. In: Johnson GJ, Weale R, Minassian DC, West SK, editors. The Epidemiology of Eye Disease. 2nd ed. London: Arnold; 2003. [Google Scholar]
- 9.Thakur J, Reddy H, Wilson ME, Jr, Paudyal G, Gurung R, Thapa S, et al. Pediatric cataract surgery in Nepal. J Cataract Refract Surg. 2004;30:1629–35. doi: 10.1016/j.jcrs.2003.12.047. [DOI] [PubMed] [Google Scholar]
- 10.Khandekar R, Sudhan A, Jain BK, Shrivastav K, Sachan R. Pediatric cataract and surgery outcomes in Central India: A hospital based study. Indian J Med Sci. 2007;61:15–22. [PubMed] [Google Scholar]
- 11.Gogate P, Khandekar R, Srisimal M, Dole K, Taras S, Kulkarni S, et al. Cataracts with delayed presentation- Are they worth operating upon? Ophthalmic Epidemiol. 2010;17:25–33. doi: 10.3109/09286580903450338. [DOI] [PubMed] [Google Scholar]
- 12.Condan NG, Ruiz S, Suzuki M, Herrera V. Determinants of pediatric cataract program outcomes and follow up in a large series in Mexico. J Cataract Refract Surg. 2007;33:1775–80. doi: 10.1016/j.jcrs.2007.06.025. [DOI] [PubMed] [Google Scholar]
- 13.Erickson JR, Bronsard A, Mosha M, Carmichael D, Hall A, Courtright P. Predictors of poor follow-up in children that had cataract surgery. Ophthalmic Epidemiol. 2006;13:237–43. doi: 10.1080/09286580600672213. [DOI] [PubMed] [Google Scholar]
- 14. [Accessed on 2011 Dec 12]. www.orbis.org .
- 15.Neena J, Rachel J, Praveen V, Murthy GV Rapid Assessment of Avoidable Blindness India Study Group. Rapid assessment of avoidable blindness in India. PLoS ONE. 2008;3:e2867. doi: 10.1371/journal.pone.0002867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kumar N, Shekhar C, Kumar P, Kundu AS. Kuppuswamy's socioeconomic status scale-updating for 2007. Indian J Pediatr. 2007;74:1131–2. [PubMed] [Google Scholar]
- 17.Rahi JS, Gilbert CE, Foster A, Minassian D. Measuring the burden of childhood blindness. Br J Ophthalmol. 1999;83:387–8. doi: 10.1136/bjo.83.4.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fraser S, Bunce C, Wormald R, Brunner E. Deprivation and late presentation of glaucoma: Case control study. BMJ. 2001;322:639–43. doi: 10.1136/bmj.322.7287.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gogate P, Deshpande R, Chelerkar V, Deshpande S, Deshpande M. Is glaucoma blindness a disease of deprivation and ignorance? A case control study for late presentation of glaucoma in India. Indian J Ophthalmol. 2011;59:29–35. doi: 10.4103/0301-4738.73720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ram J, Sukhija J, Thapa BR, Arya VK. Comparison of hospital versus rural eye camp based pediatric cataract surgery. Middle East Afr J Ophthalmol. 2012;19:141–6. doi: 10.4103/0974-9233.92131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gogate P, Dole K, Ranade S, Deshpande M. Cost of pediatric cataract in Maharashtra, India. Int J Ophthalmol. 2010;10:1248–52. doi: 10.3980/j.issn.2222-3959.2010.02.22. [DOI] [PMC free article] [PubMed] [Google Scholar]


