Abstract
A 65-year-old lady presented with decreased vision in left eye since seven months. Vision was 6/9 in right eye and 6/36 in left. Examination revealed idiopathic, full-thickness macular hole in left eye; confirmed by optical coherence tomography (OCT). Patient underwent phacoemulsification with intraocular lens (IOL) implantation, vitrectomy, internal limiting membrane (ILM) peeling and 14% C3F8 gas injection. OCT repeated after six weeks revealed type II closure with cuff of subretinal fluid. Four weeks later, patient underwent fluid–gas exchange with 14% C3F8 gas and postoperative positioning. OCT was repeated after two weeks, which showed complete closure of the macular hole. OCT can help in selection of eyes for re-surgery that stand a better chance for hole closure. Macular holes with cuff of subretinal fluid are probably more likely to close on re-surgery than those without. However, larger studies with longer follow-up are required to validate this finding.
Keywords: Internal limiting membrane, macular hole, optical coherence tomography, re-surgery, vitrectomy
Surgical treatment of idiopathic, full-thickness macular hole by vitreous surgery was first described by Kelly and Wendel in 1991.[1] Since then there has been a refinement in the surgical technique to improve the functional and anatomical outcomes. Currently, the standard technique consists of pars plana vitrectomy, internal limiting membrane (ILM) peeling and gas tamponade. The current success rate of primary surgery is 80-100%.[2,3,4] There can be several reasons for failure of hole closure viz duration of hole, size of hole, incomplete ILM peeling, traction from the residual epiretinal membrane and difficulties in postoperative positioning.[1,5,6,7,8] In the cases of failed primary surgery, pre- and post-operative configuration of the macular hole visualized by optical coherence tomography (OCT) could probably help in correlating anatomical and functional outcome and also help in selection of cases for re-surgery. We present a case report in which a persistent idiopathic macular hole was successfully closed two weeks following re-surgery after the failure of primary surgery, twelve weeks before. To the best of our knowledge, this is the first report of its kind from India.
Case Report
A 65-year-old lady presented with diminution of vision associated with distortion of images in the right eye since the past seven months. On examination, her best corrected visual acuity (BCVA) was 6/9, N6 in the right eye and 6/36, N36 in the left eye. Biomicroscopic examination revealed nuclear sclerosis grade 2 with posterior subcapsular cataract in both eyes. Left fundus revealed an idiopathic, full-thickness macular hole in the left eye [Fig. 1a] confirmed on OCT [Fig. 1b]. Hole formation factor (HFF) was noted to be 0.80 and the basal diameter was 949 microns. Right eye fundus was normal. The patient underwent phacoemulsification with intraocular lens (IOL) implantation, vitrectomy, ILM peeling and 14% C3 F8 gas injection in the left eye. The patient was advised postoperative prone positioning (12-14 h per day for two weeks). On a follow-up six weeks after surgery, fundus examination revealed type II macular hole closure, confirmed on OCT [Fig. 2]. HFF was noted to be 0.80 while the basal diameter was reduced to 923 microns. BCVA was 6/36, N18 in the left eye. Retreatment options were explained to the patient . Four weeks later, patient underwent re-surgery; fluid–gas exchange with 14% C3 F8 gas injection was done and postoperative prone positioning as before, was advised. Repeat ILM peeling was not required as ILM re-proliferation was not noted at the time of re-surgery. On a follow-up two weeks after re-surgery, left eye revealed complete closure of the hole [Fig. 3a, b], confirmed on OCT. BCVA improved to 6/36, N12 in the left eye.
Figure 1.
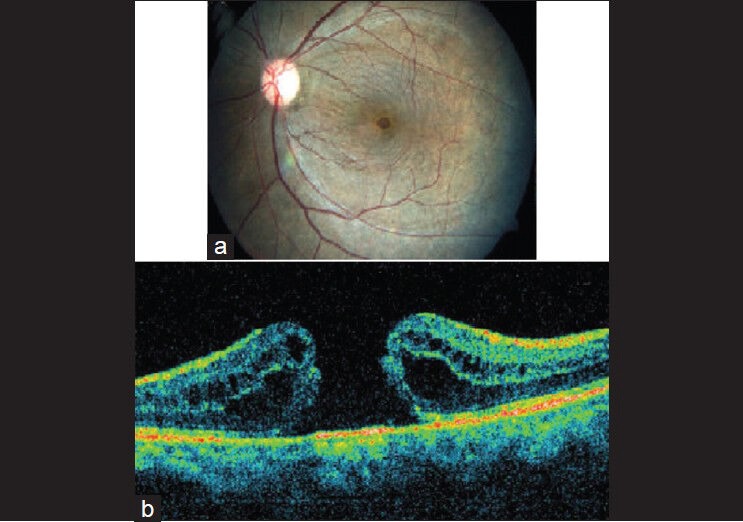
Baseline (a) Color fundus photo of the left eye showing a full-thickness macular hole (b) OCT scan is confirmatory of macular hole
Figure 2.
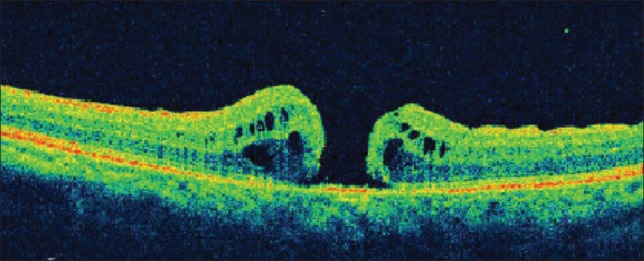
Six weeks after primary surgery. OCT showing type 2 closure of macular hole with cuff of subretinal fluid at the edges of the hole. Basal diameter of the macular hole is reduced
Figure 3.
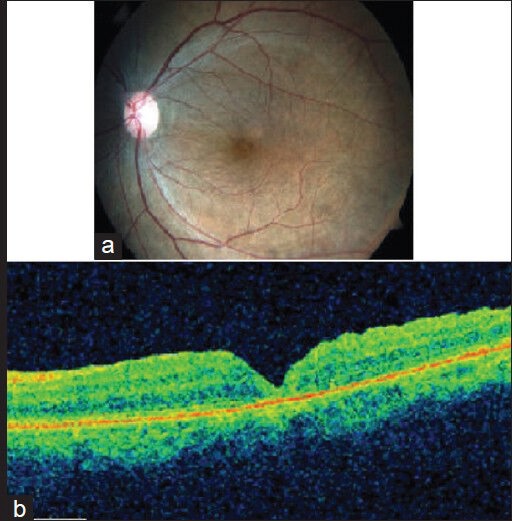
Two weeks after repeat surgery (a) Color fundus photo showing completely closed macular hole (b) OCT is confirmatory of type 1 closure of the macular hole
Discussion
The exact cause of failure of closure of idiopathic macular hole after primary surgery is still uncertain. It may be affected by various factors such as advanced macular hole stage,[1,5,6,7] duration of the macular hole and poor patient compliance with postoperative positioning.[1] Usually, reoperation for a failed macular hole surgery has a lower success rate than primary surgery. In the cases of failed primary surgery, OCT can help in prognosticating the outcome of the second surgery.[9] It has been shown that macular holes with cuff of subretinal fluid were more likely to close than those without the cuff.[9]
The pathogenesis of hole closure primarily involves centripetal movement of retinal tissue to occupy the fovea. In the case of a macular hole with a cuff of subretinal fluid (SRF), there will not be any adhesion between the macular hole edges and the underlying retinal pigment epithelium (RPE). With the use of an intraocular tamponade, there is a higher likelihood of closure of such a macular hole. Conversely, in the case of macular hole without the cuff of SRF, the macular hole edges and RPE will be stuck together, considerably reducing the chances of hole closure.[9] Kusuhara et al. described macular hole index as the ratio of the hole height to the base diameter, which refers to the perpendicular and horizontal dimensions of the hole visualized by OCT.[10] They found that the visual outcome of primary macular hole surgery is positively correlated with a higher index that indicates a smaller horizontal and a greater perpendicular hole dimension. The findings of primary surgery may not be comparable to the results of re-operation. However, Hillenkemp et al. found that a greater perpendicular hole dimension as seen in the holes “with cuff” seems to be a positive prognostic factor.[9]
OCT is a helpful tool to precisely measure macular hole size and visualize the detached cuff, objectively. Based on the configuration of macular hole and the indices as measured on OCT images, case selection for re-surgery in such eyes can be facilitated. Factors favoring re-surgery in this case were high HFF, reduced basal diameter of macular hole and the presence of ‘cuff of SRF’. Even though outcomes from a single case cannot be generalized, larger studies might validate our findings.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Kelly NE, Wendel RT. Vitreous surgery for idiopathic macular holes. Results of a pilot study. Arch Ophthalmol. 1991;109:654–9. doi: 10.1001/archopht.1991.01080050068031. [DOI] [PubMed] [Google Scholar]
- 2.Brooks J, Logan H. Macular hole surgery with and without internal limiting membrane peeling. Ophthalmology. 2000;107:1939–49. doi: 10.1016/s0161-6420(00)00331-6. [DOI] [PubMed] [Google Scholar]
- 3.Christmas NJ, Smiddy WE, Flynn HW., Jr Reopening of macular holes after initially successful repair. Ophthalmology. 1998;105:1835–8. doi: 10.1016/S0161-6420(98)91025-9. [DOI] [PubMed] [Google Scholar]
- 4.Sheidow TG, Blinder KJ, Holekamp N, Joseph D, Shah G, Grand MG, et al. Outcome results in macular hole surgery: An evaluation of internal limiting membrane peeling with and without indocyanine green. Ophthalmology. 2003;110:1697–701. doi: 10.1016/S0161-6420(03)00562-1. [DOI] [PubMed] [Google Scholar]
- 5.Tognetto D, Grandin R, Sanguinetti G, Minutola D, Di Nicola M, Di Mascio R, et al. Macular Hole Surgery Study Group. Internal limiting membrane removal during macular hole surgery: Results of A Multicenter Retrospective Study. Ophthalmology. 2006;113:1401–10. doi: 10.1016/j.ophtha.2006.02.061. [DOI] [PubMed] [Google Scholar]
- 6.Ryan EH, Gilbert HD. Results of surgical treatment of recent-onset full-thickness idiopathic macular holes. Arch Ophthalmol. 1994;112:1545–53. doi: 10.1001/archopht.1994.01090240051025. [DOI] [PubMed] [Google Scholar]
- 7.Smiddy WE, Feuer W, Cordahi G. Internal limiting membrane peeling in macular hole surgery. Ophthalmology. 2001;108:1471–8. doi: 10.1016/s0161-6420(00)00645-x. [DOI] [PubMed] [Google Scholar]
- 8.Yoshida M, Otsubo A, Kishi S. Incidence of reopening of macular hole after successful surgery with removal of internal limiting membrane. Jpn J Clin Ophthalmol. 2002;56:999–1003. [Google Scholar]
- 9.Hillenkamp J, Kraus J, Framme C, Jackson TL, Roider J, Gabel VP, et al. Retreatment of full-thickness macular hole: Predictive value of optical coherence tomography. Br J Ophthalmol. 2007;91:1445–9. doi: 10.1136/bjo.2007.115642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kusuhara S, Teraoka MF, Fuji S, Fujii S, Nakanishi Y, Tamura Y, et al. Prediction of postoperative visual outcome based on hole configuration by optical coherence tomography in eyes with idiopathic macular holes. Am J Ophthalmol. 2004;138:709–16. doi: 10.1016/j.ajo.2004.04.063. [DOI] [PubMed] [Google Scholar]


