Abstract
Inorganic nanomaterials have a wide array of physical and structural properties that make them attractive candidates for imaging and therapeutic delivery. Nanoparticle platforms have been intensely studied for these applications, and examples are starting to enter the clinic. This review looks at why inorganic particles provide promising platforms for biomedicine, and what issues need to be addressed for them to reach their potential.
Keywords: inorganic nanomaterials, bio-nano interface, drug delivery, up converting nanoparticles, theranostic, imaging agent
1. Introduction
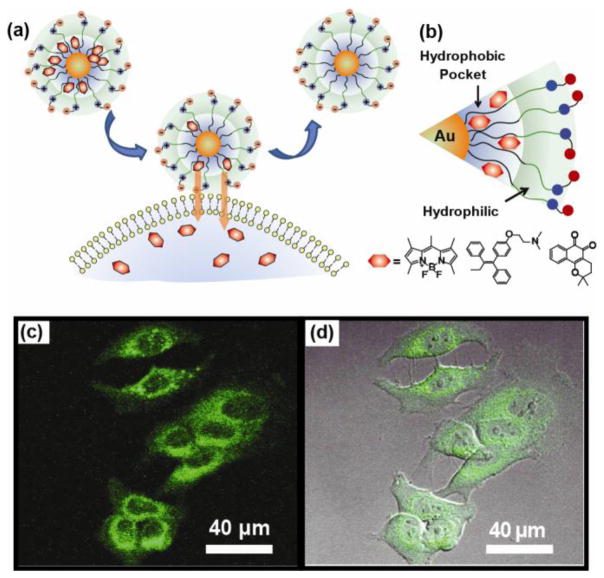
Inorganic nanoparticles come in a wide variety of sizes [1–3] and shapes [4], and possess an array of physical properties that arise from the quantum properties of their core materials [5, 6]. The diversity of both structure and properties enables new strategies for the design of therapeutics and imaging agents [7, 8] (Fig. 1), with examples of nanoparticle-based systems starting to enter the clinic. New issues that arise from the interactions of these materials with biosystems, however, balance the promise of nanomaterials [9–13]. Some of these issues are insurmountable, some require research to overcome, and some provide new directions that were unexpected yet potentially quite powerful.
Fig. 1.
Use of the core properties and structure of nanoparticle in biomedicine
This review takes a look at the current status of inorganic nanoparticles as imaging and therapeutic agents. Our goal is to both highlight the promise of these materials and to provide areas where questions remain and better understanding is required.
2. Nanoparticle Cores—Physics in Action
The core sizes of smaller nanoparticles impart unique properties arising from quantum confinement [14]. Quantum dots (QDs) provide very stable fluorescent probes [15] that are size tunable and very resistant to photobleaching [16–19]. Tailoring the surface of QDs with suitable ligands may confer desirable properties such as high quantum yield and long-term stability under broad range of conditions (high electrolyte concentration, a broad pH range, and biogenic thiols). Mattoussi et al. have demonstrated that QDs capped with multidentate lipoic acid ligand possessing a zwitterionic head group bring out compact and highly biocompatible nanomaterials [20, 21]. These attributes have made QDs attractive materials for in vitro and in vivo imaging applications [22–24]. Extension of these studies to the clinic has been hampered by two major challenges. First, the core materials of these QDs are frequently fabricated using toxic heavy metals such as cadmium and lead [25–27]. While other less toxic QDs have been developed [28], they generally have excitation/emission wavelengths that are too short for practical use or present challenges in terms of functionalization. The other issue with QDs is that most are active in the visible range where tissue penetration is quite poor [29]. While this is not an issue in mice, where most of the organs are close to the surface, it is quite important for clinical imaging applications.
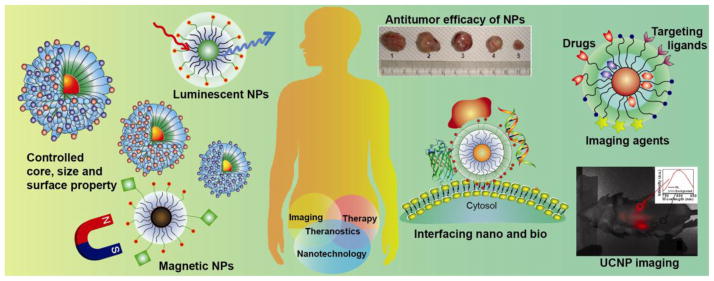
Upconverting particles (UCP) avoid many of the issues of QDs. First, these systems are often excited by near-infrared (NIR) or infrared radiation [30, 31]. UCPs are typically designed to emit visible light upon NIR-light excitation, with excitation occurring in the wavelength range where tissue has maximum transparency to allow the light source to penetrate more deeply into living tissues [32, 33]. Recently, Han et al. have used (α-NaYbF4:Tm3+)/CaF2 core/shell UCP for high contrast deep tissue bioimaging [34]. In their design, a 35-fold increase in the intensity of UC photoluminescence (PL) was obtained as a result of suppressing the quenching effect by heteroepitaxial growth of biocompatible CaF2 shell. Rat femoral bone under centimeter-deep soft tissues and pork tissue under 3.2 cm were successfully imaged (Fig. 2). Besides deep tissue penetration, an additional benefit of UCPs is that they can be made using less toxic materials such as lanthanides [35, 36]. UCPs, however, can have challenges in terms of surface modification, and are difficult to fabricate in “ultra-small” (<15 nm diameter) sizes [37].
Fig. 2.
(a) Bright-field image of the rat hind leg after embedding UCNP-loaded synthetic mesh and suturing muscle and skin. (b) PL image of the rat femur seven days after UCNP-loaded mesh implantation. Scale bar: 2 cm. (c) PL bright-field image of a cuvette filled with a suspension of UCNPs. (d) Bright-field image of the pork tissue with the cuvette under and a quarter coin placed aside indicating the thickness, (e) Merged UCPL/bright-field image of the pork tissue. (f) Side view of the pork tissue. Adapted from [34].
3. The interface between nanoparticles and biosystems
What is on the surface of a nanoparticle dictates how that particle interacts with biosystems [38]. Much of the work on nanomaterials has focused on non-interactive “stealth” coatings designed to minimize interactions of nanomaterials with cells and the immune system. The most popular coatings are poly(ethylene glycol) (PEG)-based. These polymers are relatively good at minimizing interactions with biosystems [39] (Fig. 3), however recent studies have shown that PEG polymers can cause inflammation through complement activation [40–42]. Zwitterionic coatings, i.e. ones featuring paired cationic and anionic centers are rapidly increasing in popularity [43–45], though the immune system effects of these coverages are not fully understood.
Fig. 3.
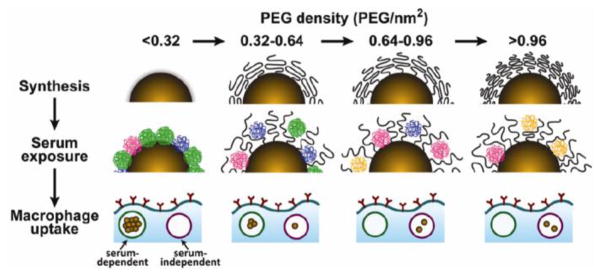
Schematic illustration showing how PEG density affects the adsorption of serum proteins to gold nanoparticles. As PEG density increases, the amount of serum proteins adsorbed to the gold NP surface decreases and as a result macrophage uptake is driven mainly by a less efficient serum-independent mechanism. Adapted from [39].
Understanding the behavior of nanomaterials in vivo is complicated by the fact that serum proteins adsorb to the surface of particles, generating a “protein corona” [46, 47]. The composition of this corona is dictated by the surface of the particle [48, 49], but generally provides a barrier between the particle and the bio-environment. While complicating the behavior of nanomaterials, the corona plays a useful role, reducing the damage to red blood cells that can be caused by nanoparticles. For example, Rotello et al. have used a library of gold NPs (AuNPs) with different surface hydrophobicity to investigate the effect of surface functionality on hemolysis [50]. Although in the absence of serum media a linear hemolytic behavior with increasing hydrophobicity was observed, in the presence of plasma proteins no hemolysis was observed within 30 min (Fig. 4).
Fig. 4.
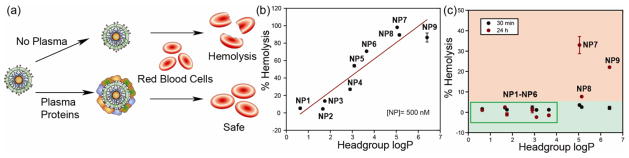
(a) Schematic illustrating that the formation of a plasma protein corona on the NP surface protects red blood cells from NP-mediated hemolysis. (b) Hemolysis percentage of NP1–NP9 versus headgroup logP in the absence of plasma proteins. (c) Hemolysis percentage of NP1–NP9 versus headgroup logP in the presence of plasma proteins. Adapted from [50].
4. Biomedical applications of nanomaterials
4.1. Inorganic nanomaterials in imaging
Imaging strategies are key tools for diagnosing a wide range of diseases. Magnetic resonance imaging (MRI) is one of the most useful techniques, and one where nanomaterials can provide unique imaging agents [51, 52]. Superparamagnetic iron oxides nanoparticles (SPIONs) provide effective MRI contrast agents that rely on the magnetic nature of the core [53]. These systems have been explored extensively in vivo, with tumor targeting ligands used to image tumors [54, 55]. While potentially quite useful, the relaxation mechanism induced by SPIONs causes targeted tissue to have reduced signal, the opposite of more desirable “turn on” agents such as gadolinium.
In addition to the UCPs described above, AuNPs provide optical imaging agents, exploiting the size and shape dependent optical properties of nanoscale gold. Nanospheres, nanocages [56], nanorods [57] and nanoshells [58] made from AuNPs have all been used as contrast agents in preclinical investigations. In one strategy, photoacoustic imaging with nanoparticles was combined with deep tissue imaging provided by ultrasound (Fig. 5) [59].
Fig. 5.
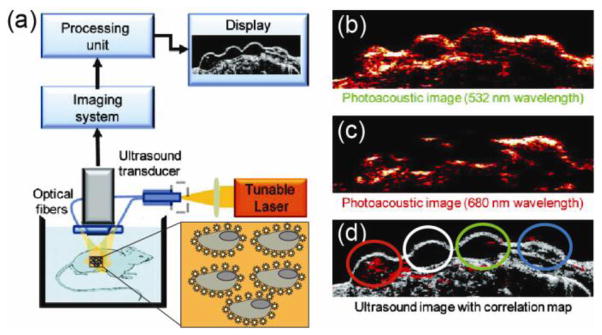
(a) Scheme for ultrasound and photoacoustic imaging system. (b) Photoacoustic image at 532 nm wavelength. (c) Photoacoustic image at 680 nm wavelength (d) Ultrasound of gelatin implants in mouse tissue ex vivo. The cells with targeted AuNPs (red), control cells (white), the cells mixed with mPEG-SH coated Au NPs (green), and NIR dye (blue) are shown on the ultrasound image. Adapted from [59].
4.2. Application of inorganic nanomaterials in drug delivery
The size, shape [60], and surface properties [61] of nanoparticles make them promising platforms as drug delivery vehicles [62, 63]. Two strategies are used for these vectors: covalent attachment and non-covalent association. Covalent attachment has the advantages of being able to control release through attachment chemistry (e.g. release of thiol-based payloads via glutathione release inside the cells) [64] and the fact that the dissociation of the carrier and payload requires a chemical reaction, making the systems stable in solution. On the other hand, covalent attachment of drugs generally (but not always) requires conversion from the particle-bound prodrug to the free drug [65, 66]. Additionally, a number of covalent carrier systems for biomolecules (e.g. siRNA) have a large proportion of the delivered particle trapped in endosomes where it is not active [67].
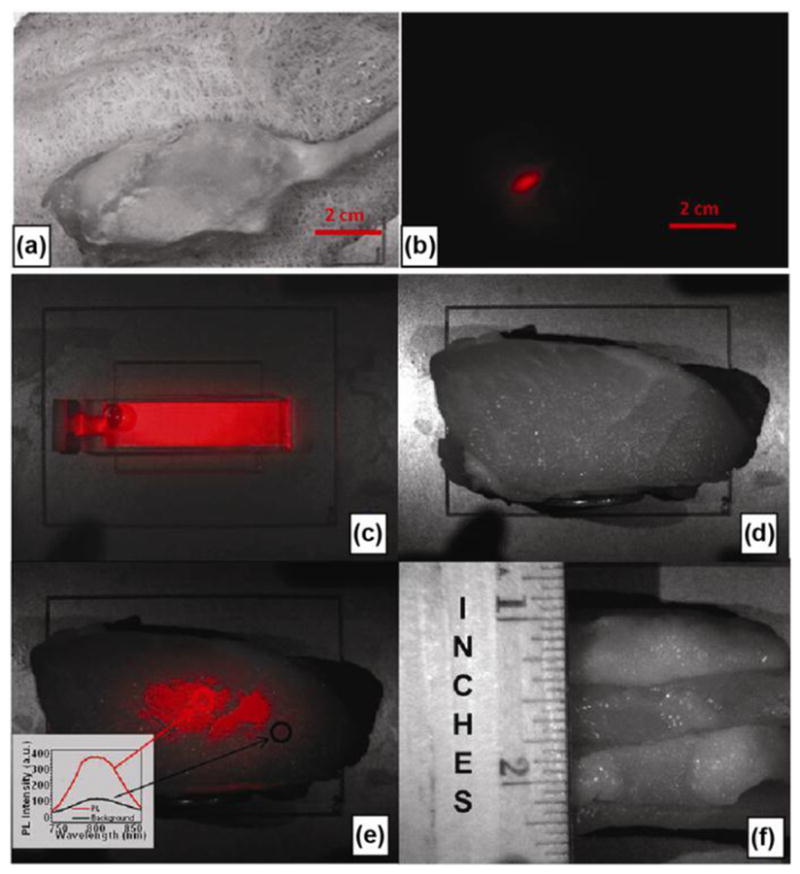
Non-covalent supramolecular complexes provide a means of delivering unmodified drugs. For instance, Rotello et al. have used hydrophobic pockets of AuNP monolayers to encapsulate highly hydrophobic dyes/drugs and deliver them into MCF-7 cells through cell membrane mediated release (Fig. 6) [68]. Non-covalent strategies, however, require careful tuning to prevent either premature or overly slow payload release.
Fig. 6.
(a) Payload delivery to cell through monolayer-membrane interactions. (b) Schematic illustration of guest molecules (bodipy, tamoxifen and lapachone) trapped in the hydrophobic pocket of NPs. Confocal laser scanning microscopy images of MCF-7 cell treated with bodipy encapsulated NPs (c) green channel, (d) overlapped with bright field. Adapted from [68].
One of the ways for NPs to improve drug efficacy is the release of the cargo on the targeting site by using a wide range of release stimuli. Design of “smart” surface functionalities is a general method adopted to obtain stimuli-responsive NPs. Stimuli-responsive carriers can be designed from NPs that respond either to an internal stimulus (such as a change in pH, glutathione (GSH) or enzymatic cleavage) or to an external stimulus (such as an applied magnetic field or exposure to a specific wavelength of light) [69]. These stimuli are used as triggers to break covalent bonds between the carrier and cargo, or to destabilize non-covalent interactions, facilitating the release of cargo once the carrier has reached the destination.
The efficiency of both covalent and non-covalent delivery systems can be enhanced through targeting [70]. Targeting comes in two forms: passive and active targeting. Passive targeting takes advantage of physical properties that arise from particle size. Inorganic NPs are generally in the correct size range to take advantage of the enhanced permeation and retention (EPR) effect [71, 72]. The EPR effect relies on the leaky nature of tumor vasculature to concentrate nanomaterials in tumors. On it’s own, the EPR effect provides a modest enhancement in therapeutic concentration at tumor sites—helpful but not game changing [73, 74].
Active targeting focuses on cell surface molecules, in particular receptors that are overexpressed on tumor cells [75, 76]. Active targeting has been effective in vivo, however translation to the clinic has been less rapid than one would expect for a “silver bullet” approach. There are a number of challenges that arise with active targeting. Foremost, even though receptor overexpression can be substantial in tumor cells, there are many more healthy cells than tumor cells in the typical patient, where tumor sizes of 1–10 g are normal. This challenge in lab-to-clinic translation is exacerbated by the large tumor burdens typically used in mouse models—often equivalent to human tumors of over 1 kg.
4.3. Theragnostic applications of inorganic nanomaterials
One of the burgeoning areas in delivery is the field of theragnostics—the combination of imaging and therapeutic modalities [77]. This approach can be quite powerful, providing tumor visualization and treatment at the same time [78]. As an example, Jon et al. have used doxorubicin (Dox) loaded thermally cross-linked (TCL) SPIONs as a drug-delivering MR contrast agent (Fig. 7a) [79]. After 4.5 hours of injection, darkening was noticeable due to accumulation of TCL-SPIONs in the vicinity of tumor (Fig. 7b). In addition, the highest tumor growth inhibition was observed when the mouse was injected with Dox@TCL-SPIONs compared to mice treated with 5% glucose, TCL-SPION, Dox (0.64 mg kg−1) and Dox (5 mg kg−1) (Fig. 7c). As with all multifunctional systems, however, it can be challenging to balance the different functions. As an example, imaging and delivery have very different requirements, and balancing limits of detection for imaging with payload amount is non-trivial. Additionally, multiple functions increase the potential for failure—simplicity is a virtue in pharmaceutical design.
Fig. 7.
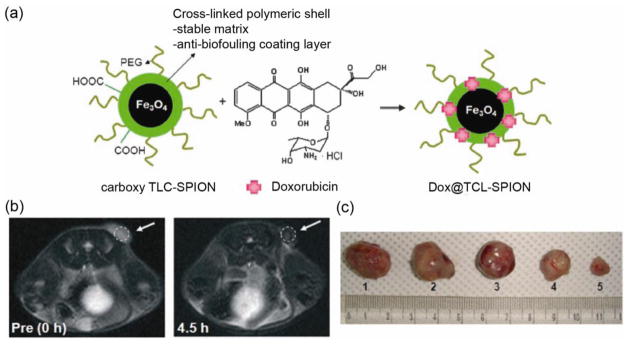
(a) Schematic illustrating doxorubicin loading into TLC-SPIONs. (b) Images taken at 0 and 4.5 h at level of tumor on the right back of mouse. (c) Changes in tumor volume when mice were treated with (1) 5% glucose, (2) TCL-SPION, (3) Dox (0.64 mg kg−1) and (4) Dox (5 mg kg−1) and (5) Dox@TCL-SPION (0.64 mg Doxkg−1). Adapted from [79].
4.4. Additional challenges in translation of nanoparticles to the clinic
Nanoparticles have challenges that arise from their novel structures, such as the corona effects described above. There are other challenges with these systems, however, that arise from our experimental approaches. First, there is the issue of characterization [80]. Many studies using nanomaterials feature poorly characterized particles (Fig. 8). As a result, it is difficult to differentiate artifacts from real effects caused by nanomaterials in biological systems, compromising also the reproducibility of the results [81]. Given the rigorous characterization and quality control that is required for the clinic, it can be hoped that there will be a “trickle down” effect that will foster enhanced characterization of nanomaterials for in vitro and in vivo studies [82, 83].
Fig. 8.
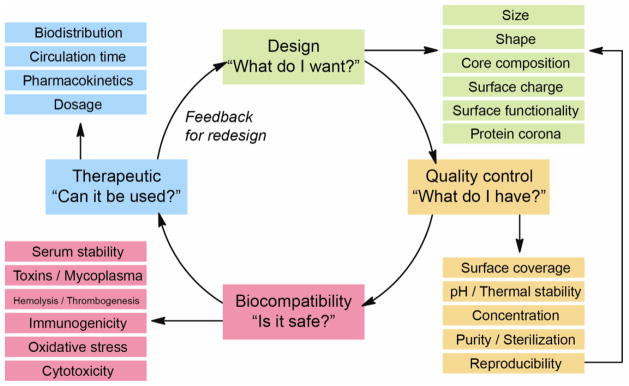
Characterization cycle in nanomaterials research.
Perhaps the most significant challenge to creation of effective nanotherapeutics arises from the combinatorial approach of the research in nanotechnology. Particles come in different sizes and shapes, surface coverages have different structures/charges/lengths, and targeting ligands can have different attachment strategies and densities on the particle. Each of these parameters is important, and will affect the behavior of the resulting vehicle (Fig. 8) [84]. Current research tends to focus on one parameter at a time, for example particle size or targeting functionality. As a result we still have a fairly weak understanding of structure-function correlations for nanomaterials, an issue that will need to be addressed if we are to generate systems that are optimized for function and suitable for the clinic [85].
5. Conclusions
Nanoparticles provide highly promising platforms for therapeutics and imaging agents. Proper engineering of core and surface properties enable us to tune parameters such as toxicity, penetration depth, and uptake. For examples of core modifications, gold nanoparticles provide low toxicity for delivery applications, while upconverting nanoparticles provide less toxic analogs of quantum dots for imaging applications. In terms of surfaces, we are rapidly gaining experience in creation of surfaces with desired interactions, but the study is still quite empirical, making generalization challenging.
Like all new technologies, however, there are growing pains in nanomedicine. One thing that should be kept in mind is that effective use of any tool requires understanding of how it works. If the potential impact of nanomaterials in medicine is to be realized, we must balance our pursuit of novel applications with strong effort applied to understanding the fundamentals of nanoparticle interactions with biosystems. In this way, combinatorial designs could be used to fabricate multifunctional platforms for various applications besides helping discovery and understanding of principles lying underneath.
Highlights.
Inorganic nanoparticles provide platforms for biomedicine.
Numerous nanoparticle systems with useful properties have been developed.
Characterization is a very important but often neglected topic in nanomedicine.
We do not yet have an integrated understanding of nanobiosystems.
Lack of fundamental understanding means limited predictive capabilities.
Acknowledgments
This work was supported by grants from the NIH (EB014277 and GM077173).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Auffan M, Rose J, Bottero JY, Lowry GV, Jolivet JP, Wiesner MR. Towards a definition of inorganic nanoparticles from an environmental, health and safety perspective. Nat Nanotechnol. 2009;4:634–641. doi: 10.1038/nnano.2009.242. [DOI] [PubMed] [Google Scholar]
- 2.Jiang W, Kim BYS, Rutka JT, Chan WCW. Nanoparticle-mediated cellular response is size-dependent. Nature Nanotechnol. 2008;3:145–150. doi: 10.1038/nnano.2008.30. [DOI] [PubMed] [Google Scholar]
- 3.Rejman J, Oberle V, Zuhorn IS, Hoekstra D. Size-dependent internalization of particles via the pathways of clathrinand caveolae-mediated endocytosis. Biochem J. 2004;377:159–169. doi: 10.1042/BJ20031253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cho EC, Zhang Q, Xia YN. The effect of sedimentation and diffusion on cellular uptake of gold nanoparticles. Nat Nanotechnol. 2011;6:385–391. doi: 10.1038/nnano.2011.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dreaden EC, Neretina S, Qian W, El-Sayed MA, Hughes RA, Preston JS, Mascher P. Plasmonic enhancement of nonradiative charge carrier relaxation and proposed effects from Enhanced radiative electronic processes in semiconductor-gold core-shell nanorod arrays. J Phys Chem C. 2011;115:5578–5583. [Google Scholar]
- 6.Yen CW, Hayden SC, Dreaden EC, Szymanski P, El-Sayed MA. Tailoring plasmonic and electrostatic field effects to maximize solar energy conversion by bacteriorhodopsin, the other natural photosynthetic system. Nano Lett. 2011;11:3821–3826. doi: 10.1021/nl2018959. [DOI] [PubMed] [Google Scholar]
- 7.Popovic Z, Liu WH, Chauhan VP, Lee J, Wong C, Greytak AB, Insin N, Nocera DG, Fukumura D, Jain RK, Bawendi MG. A nanoparticle size series for in vivo fluorescence imaging. Angew Chem Int Ed. 2010;49:8649–8652. doi: 10.1002/anie.201003142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Erogbogbo F, Yong KT, Hu R, Law WC, Ding H, Chang CW, Prasad PN, Swihart MT. Biocompatible magnetofluorescent probes: luminescent silicon quantum dots coupled with superparamagnetic iron(III) oxide. ACS Nano. 2010;9:5131–5138. doi: 10.1021/nn101016f. [DOI] [PubMed] [Google Scholar]
- 9.Stark WJ. Nanoparticles in biological systems. Angew Chem Int Ed. 2011;50:1242–1258. doi: 10.1002/anie.200906684. [DOI] [PubMed] [Google Scholar]
- 10.Moyano DF, Rotello VM. Nano meets biology: structure and function at the nanoparticle interface. Langmuir. 2011;27:10376–10385. doi: 10.1021/la2004535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mirshafiee V, Mahmoudi M, Lou K, Cheng JJ, Kraft ML. Protein corona significantly reduces active targeting yield. Chem Commun. 2013;49:2557–2559. doi: 10.1039/c3cc37307j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saha K, Kim ST, Yan B, Miranda OR, Alfonso FS, Shlosman D, Rotello VM. Surface functionality of nanoparticles determines cellular uptake mechanisms in mammalian cells. Small. 2013;9:300–305. doi: 10.1002/smll.201201129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Verma A, Stellacci F. Effect of surface properties on nanoparticle–cell interactions. Small. 2010;6:12–21. doi: 10.1002/smll.200901158. [DOI] [PubMed] [Google Scholar]
- 14.Irrera A, Artoni P, Iacona F, Pecora EF, Franzo G, Galli M, Fazio B, Boninelli S, Priolo F. Quantum confinement and electroluminescence in ultrathin silicon nanowires fabricated by a maskless etching technique. Nanotechnology. 2012;23:075204. doi: 10.1088/0957-4484/23/7/075204. [DOI] [PubMed] [Google Scholar]
- 15.Grieve K, Mulvaney P, Grieser F. Synthesis and electronic properties of semiconductor nanoparticles/quantum dots. Curr Opin Colloid Interface Sci. 2000;5:168–172. [Google Scholar]
- 16.Zhan NQ, Palui G, Grise H, Tang HL, Alabugin I, Mattoussi H. Combining ligand design with photoligation to provide compact, colloidally stable, and easy to conjugate quantum dots. ACS Appl Mater Interfaces. 2013;5:2861–2869. doi: 10.1021/am302788q. [DOI] [PubMed] [Google Scholar]
- 17.Zhong XH, Han MY, Dong ZL, White TJ, Knoll W. Composition-tunable ZnxCd1-xSe nanocrystals with high luminescence and stability. J Am Chem Soc. 2003;125:8589–8594. doi: 10.1021/ja035096m. [DOI] [PubMed] [Google Scholar]
- 18.Dabbousi BO, Rodriguez-Viejo J, Mikulec FV, Heine JR, Mattoussi H, Ober R, Jensen KF, Bawendi MG. (CdSe)ZnS core–shell quantum dots: synthesis and characterization of a size series of highly luminescent nanocrystallites. J Phys Chem B. 1997;101:9463–9475. [Google Scholar]
- 19.Xu BB, Zhang YL, Zhang R, Wang L, Xiao XZ, Xia H, Chena QD, Sun HB. Programmable assembly of CdTe quantum dots into microstructures by femtosecond laser direct writing. J Mater Chem C. 2013;1:4699–4704. [Google Scholar]
- 20.Zhan N, Palui G, Safi M, Ji X, Mattouss H. Multidentate zwitterionic ligands provide compact and highly biocompatible quantum dots. J Am Chem Soc. 2013;135:13786–13795. doi: 10.1021/ja405010v. [DOI] [PubMed] [Google Scholar]
- 21.Zhu ZJ, Yeh YC, Tang R, Yan B, Tamayo J, Vachet W, Rotello VM. Stability of quantum dots in live cells. Nat Chem. 2011;3:963–968. doi: 10.1038/nchem.1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ballou B, Lagerholm BC, Ernst LA, Bruchez PM, Waggoner AS. Noninvasive imaging of quantum dots in mice. Bioconjugate Chem. 2004;15:79–86. doi: 10.1021/bc034153y. [DOI] [PubMed] [Google Scholar]
- 23.He Y, Zhong Y, Su Y, Lu Y, Jiang Z, Peng F, Xu T, Su S, Huang Q, Fan C, Lee ST. Water-dispersed near-infrared-emitting quantum dots of ultrasmall sizes for in vitro and in vivo imaging. Angew Chem Int Ed. 2011;50:5695–5698. doi: 10.1002/anie.201004398. [DOI] [PubMed] [Google Scholar]
- 24.Dubertret B, Skourides P, Norris DJ, Noireaux V, Brivanlou AH, Libchaber A. In vivo imaging of quantum dots encapsulated in phospholipid micelles. Science. 2002;298:1759–1762. doi: 10.1126/science.1077194. [DOI] [PubMed] [Google Scholar]
- 25.Cho SJ, Maysinger D, Jain M, Roder B, Hackbarth S, Winnik FM. Long-term exposure to CdTe quantum dots causes functional impairments in live cells. Langmuir. 2007;23:1974–1980. doi: 10.1021/la060093j. [DOI] [PubMed] [Google Scholar]
- 26.Pelley JL, Daar AS, Saner MA. State of academic knowledge on toxicity and biological fate of quantum dots. Toxicol Sci. 2009;112:276–296. doi: 10.1093/toxsci/kfp188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hardman R. A toxicologic review of quantum dots: toxicity depends on physicochemical and environmental factors. Environ Heal Perspect. 2006;114:165–172. doi: 10.1289/ehp.8284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hauck TS, Anderson RE, Fischer HC, Newbigging S, Chan WCW. In vivo quantum-dot toxicity assessment. Small. 2010;6:138–144. doi: 10.1002/smll.200900626. [DOI] [PubMed] [Google Scholar]
- 29.Smith AM, Gao X, Nie S. Quantum dot nanocrystals for in vivo molecular and cellular imaging. Photochem Photobiol. 2004;80:377–385. doi: 10.1562/0031-8655(2004)080<0377:QDNFIV>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 30.Li C, Lin J. Rare earth fluoride nano-/microcrystals: synthesis, surface modification and application. J Mater Chem. 2010;20:6831–6847. [Google Scholar]
- 31.Yan B, Boyer JC, Habault D, Branda NR, Zhao Y. Near infrared light triggered release of biomacromolecules from hydrogels loaded with upconversion nanoparticles. J Am Chem Soc. 2012;134:16558–16561. doi: 10.1021/ja308876j. [DOI] [PubMed] [Google Scholar]
- 32.Jayakumar MKG, Idris NM, Zhang Y. Remote activation of biomolecules in deep tissues using near-infrared-to-UV upconversion nanotransducers. Proc Natl Acad Sci USA. 2012;109:8483–8488. doi: 10.1073/pnas.1114551109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu Q, Yang T, Feng W, Li F. Blue-emissive upconversion nanoparticles for low-power-excited bioimaging in vivo. J Am Chem Soc. 2012;134:5390–5397. doi: 10.1021/ja3003638. [DOI] [PubMed] [Google Scholar]
- 34.Chen G, Shen J, Ohulchanskyy TY, Patel NJ, Kutikov A, Li Z, Song J, Pandey RK, Agren H, Prasad PN, Han G. (αNaYbF4:Tm3+)/CaF2 core/shell nanoparticles with efficient near-infrared to near-infrared upconversion for high-contrast deep tissue bioimaging. ACS Nano. 2012;6:8280–8287. doi: 10.1021/nn302972r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li Z, Zhang Y, Jiang S. Multicolor core/shell-structured upconversion fluorescent Nanoparticles. Adv Mater. 2008;20:4765–4769. [Google Scholar]
- 36.Yang Y, Shao Q, Deng R, Wang C, Teng X, Cheng K, Cheng Z, Huang L, Liu Z, Liu X, Xing B. In vitro and in vivo uncaging and bioluminescence imaging by using photocaged upconversion nanoparticles. Angew Chem Int Ed. 2012;51:3125–3129. doi: 10.1002/anie.201107919. [DOI] [PubMed] [Google Scholar]
- 37.Ostrowski AD, Chan EM, Gargas DJ, Katz EM, Han G, Schuck PJ, Milliron DJ, Cohen BE. Controlled synthesis and single-particle imaging of bright, sub-10nm lanthanide-doped upconverting nanocrystals. ACS Nano. 2012;6:2686–2692. doi: 10.1021/nn3000737. [DOI] [PubMed] [Google Scholar]
- 38.Alkilany AM, Lohse SE, Murphy CJ. The gold standard: gold nanoparticle libraries to understand the nano-bio interface. Acc Chem Res. 2013;46:650–661. doi: 10.1021/ar300015b. [DOI] [PubMed] [Google Scholar]
- 39.Walkey CD, Olsen JB, Guo HB, Emili A, Chan WCW. Nanoparticle size and surface chemistry determine serum protein adsorption and macrophage uptake. J Am Chem Soc. 2012;134:2139–2147. doi: 10.1021/ja2084338. [DOI] [PubMed] [Google Scholar]
- 40.Hamad I, Hunter AC, Rutt KJ, Liu Z, Dai H, Moghimi SM. Complement activation by PEGylated single-walled carbon nanotubes is independent of C1q and alternative pathway turnover. Mol Immunol. 2008;45:3797–3803. doi: 10.1016/j.molimm.2008.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Andersen AJ, Robinson JT, Dai HJ, Hunter AC, Andresen TL, Moghimi SM. Single-walled carbon nanotube surface control of complement recognition and activation. ACS Nano. 2013;7:1108–1119. doi: 10.1021/nn3055175. [DOI] [PubMed] [Google Scholar]
- 42.Hamad I, Al-Hanbali O, Hunter AC, Rutt KJ, Andresen TL, Moghimi SM. Distinct polymer architecture mediates switching of complement activation pathways at the nanosphere-serum interface: implications for stealth nanoparticle engineering. ACS Nano. 2010;4:6629–6638. doi: 10.1021/nn101990a. [DOI] [PubMed] [Google Scholar]
- 43.Cheng G, Zhang Z, Chen SF, Bryers JD, Jiang SY. Inhibition of bacterial adhesion and biofilm formation on zwitterionic surfaces. Biomaterials. 2007;28:4192–4199. doi: 10.1016/j.biomaterials.2007.05.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang L, Xue H, Cao ZQ, Keefe A, Wang JN, Jiang SY. Multifunctional and degradable zwitterionic nanogels for targeted delivery, enhanced MR imaging, reduction-sensitive drug release, and renal clearance. Biomaterials. 2011;32:4604–4608. doi: 10.1016/j.biomaterials.2011.02.064. [DOI] [PubMed] [Google Scholar]
- 45.Yang W, Zhang L, Wang SL, White AD, Jiang SY. Functionalizable and ultra stable nanoparticles coated with zwitterionic poly(carboxybetaine) in undiluted blood serum. Biomaterials. 2009;30:5617–5621. doi: 10.1016/j.biomaterials.2009.06.036. [DOI] [PubMed] [Google Scholar]
- 46.Monopoli MP, Aberg C, Salvati A, Dawson KA. Biomolecular coronas provide the biological identity of nanosized materials. Nat Nanotechnol. 2012;7:779–786. doi: 10.1038/nnano.2012.207. [DOI] [PubMed] [Google Scholar]
- 47.Cedervall T, Lynch I, Lindman S, Berggard T, Thulin E, Nilsson H, Dawson KA, Linse S. Understanding the nanoparticle–protein corona using methods to quantify exchange rates and affinities of proteins for nanoparticles. Proc Natl Acad Sci USA. 2007;104:2050–2055. doi: 10.1073/pnas.0608582104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cedervall T, Lynch I, Foy M, Berggad T, Donnelly SC, Cagney G, Linse S, Dawson KA. Detailed identification of plasma proteins adsorbed on copolymer nanoparticles. Angew Chem Int Ed. 2007;46:5754–5756. doi: 10.1002/anie.200700465. [DOI] [PubMed] [Google Scholar]
- 49.Gessner A, Waicz R, Lieske A, Paulke BR, Mader K, Muller RH. Nanoparticles with decreasing surface hydrophobicities: influence on plasma protein adsorption. Int J Pharm. 2000;196:245–249. doi: 10.1016/s0378-5173(99)00432-9. [DOI] [PubMed] [Google Scholar]
- 50.Saha K, Moyano DF, Rotello VM. Protein coronas suppress the hemolytic activity of hydrophilic and hydrophobic nanoparticles. Mater Horiz. 2014;1:102–105. doi: 10.1039/C3MH00075C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Xie J, Liu G, Eden HS, Ai H, Chen X. Surface-engineered magnetic nanoparticle platforms for cancer imaging and therapy. Acc Chem Res. 2011;44:883–892. doi: 10.1021/ar200044b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Na HB, Song IC, Hyeon T. Inorganic nanoparticles for MRI contrast agents. Adv Mater. 2009;21:2133–2148. [Google Scholar]
- 53.Wei H, Insin N, Lee J, Han HS, Cordero JM, Liu W, Bawendi MG. Compact zwitterion-coated iron oxide nanoparticles for biological applications. Nano Lett. 2012;12:22–25. doi: 10.1021/nl202721q. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Huh YM, Jun YW, Song HT, Kim S, Choi JS, Lee JH, Yoon S, Kim KS, Shin JS, Suh JS, Cheon J. In vivo magnetic resonance detection of cancer by using multifunctional magnetic nanocrystals. J Am Chem Soc. 2005;127:12387–12391. doi: 10.1021/ja052337c. [DOI] [PubMed] [Google Scholar]
- 55.Cho EC, Glaus C, Chen JY, Welch MJ, Xia YN. Inorganic nanoparticle-based contrast agents for molecular imaging. Trends Mol Med. 2010;16:561–573. doi: 10.1016/j.molmed.2010.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tong L, Cobley CM, Chen J, Xia Y, Cheng JX. Bright three-photon luminescence from gold/silver alloyed nanostructures for bioimaging with negligible photothermal toxicity. Angew Chem Int Ed. 2010;49:3485–3488. doi: 10.1002/anie.201000440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tong L, Wei Q, Wei A, Cheng JX. Gold nanorods as contrast agents for biological imaging: optical properties, surface conjugation and photothermal effects. Photochem Photobiol. 2009;85:21–32. doi: 10.1111/j.1751-1097.2008.00507.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Park J, Estrada A, Sharp K, Sang K, Schwartz JA, Smith DK, Coleman C, Payne JD, Korgel BA, Dunn AK, Tunnell JW. Two-photon-induced photoluminescence imaging of tumors using near-infrared excited gold nanoshells. Opt Express. 2008;16:1590–1599. doi: 10.1364/oe.16.001590. [DOI] [PubMed] [Google Scholar]
- 59.Mallidi S, Larson T, Tam J, Joshi PP, Karpiouk A, Sokolov K, Emelianov S. Multiwavelength photoacoustic imaging and plasmon resonance coupling of gold nanoparticles for selective detection of cancer. Nano Lett. 2009;9:2825–2831. doi: 10.1021/nl802929u. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chithrani BD, Ghazani AA, Chan WCW. Determining the size and shape dependence of gold nanoparticle uptake into mammalian cells. Nano Lett. 2006;6:662–668. doi: 10.1021/nl052396o. [DOI] [PubMed] [Google Scholar]
- 61.Hauck TS, Ghazani AA, Chan WCW. Assessing the effect of surface chemistry on gold nanorod uptake, toxicity, and gene expression in mammalian cells. Small. 2008;4:153–159. doi: 10.1002/smll.200700217. [DOI] [PubMed] [Google Scholar]
- 62.Malmsten M. Inorganic nanomaterials as delivery systems for proteins, peptides, DNA, and siRNA. Curr Opin Colloid Interface Sci. 2013;18:468–480. [Google Scholar]
- 63.Duncan B, Kim C, Rotello VM. Gold nanoparticle platforms as drug and biomacromolecule delivery systems. J Control Release. 2010;148:122–127. doi: 10.1016/j.jconrel.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hong R, Han G, Fernandez JM, Kim BJ, Forbes NS, Rotello VM. Glutathione mediated delivery and release using monolayer protected nanoparticle carriers. J Am Chem Soc. 2006;128:1078–1079. doi: 10.1021/ja056726i. [DOI] [PubMed] [Google Scholar]
- 65.Nakanishi J, Nakayama H, Shimizu T, Ishida H, Kikuchi Y, Yamaguchi K, Horiike Y. Light regulated activation of cellular signaling by gold nanoparticles that capture and release amines. J Am Chem Soc. 2009;131:3822–3823. doi: 10.1021/ja809236a. [DOI] [PubMed] [Google Scholar]
- 66.Agasti SS, Chompoosor A, You CC, Ghosh P, Kim CK, Rotello VM. Photoregulated release of caged anticancer drugs from gold nanoparticles. J Am Chem Soc. 2009;131:5728–5729. doi: 10.1021/ja900591t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Guo S, Huang L. Nanoparticles escaping RES and endosome: challenges for siRNA delivery for cancer therapy. J Nanomater. 2011;2011:1–12. [Google Scholar]
- 68.Kim CK, Ghosh P, Pagliuca C, Zhu ZJ, Menichetti S, Rotello VM. Entrapment of hydrophobic drugs in nanoparticle monolayers with efficient release into cancer cells. J Am Chem Soc. 2009;131:1360–1361. doi: 10.1021/ja808137c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Timko BP, Dvir T, Kohane DS. Remotely triggerable drug delivery systems. Adv Mater. 2010;22:4925–4943. doi: 10.1002/adma.201002072. [DOI] [PubMed] [Google Scholar]
- 70.Huang X, Peng X, Wang Y, Shin DM, El-Sayed MA, Nie S. A reexamination of active and passive tumor targeting by using rod-shaped gold nanocrystals and covalently conjugated peptide ligands. ACS Nano. 2010;4:5887–5896. doi: 10.1021/nn102055s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Matsumura Y, Maeda H. A new concept for macromolecular therapeutics in cancer chemotherapy: mechanism of tumoritropic accumulation of proteins and the antitumor agent smancs. Cancer Res. 1986;46:6387–6392. [PubMed] [Google Scholar]
- 72.Perrault SD, Walkey C, Jennings T, Fischer HC, Chan WCW. Mediating tumor targeting efficiency of nanoparticles through design. Nano Lett. 2009;9:1909–1915. doi: 10.1021/nl900031y. [DOI] [PubMed] [Google Scholar]
- 73.Cheng Y, Meyers JD, Broome AM, Kenney ME, Basilion JP, Burda C. Deep penetration of a PDT drug into tumors by noncovalent drug-gold nanoparticle conjugates. J Am Chem Soc. 2011;133:2583–2591. doi: 10.1021/ja108846h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jain RK, Stylianopoulos T. Delivering nanomedicine to solid tumors. Nat Rev Clin Oncol. 2010;7:653–664. doi: 10.1038/nrclinonc.2010.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lu W, Xiong C, Zhang G, Huang Q, Zhang R, Zhang JZ, Li C. Targeted photothermal ablation of murine melanomas with melanocyte-stimulating hormone analog conjugated hollow gold nanospheres. Clin Cancer Res. 2009;15:876–886. doi: 10.1158/1078-0432.CCR-08-1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Choia CHJ, Alabia CA, Websterb P, Davisa ME. Mechanism of active targeting in solid tumors with transferrin-containing gold nanoparticles. Proc Natl Acad Sci USA. 2010;107:1235–1240. doi: 10.1073/pnas.0914140107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ma X, Zhao Y, Liang XJ. Theranostic nanoparticles engineered for clinic and pharmaceutics. Acc Chem Res. 2011;44:1114–1122. doi: 10.1021/ar2000056. [DOI] [PubMed] [Google Scholar]
- 78.Wang Y, Liu Y, Luehmann H, Xia X, Wan D, Cutler C, Xia Y. Radioluminescent gold nanocages with controlled radioactivity for real-time in vivo imaging. Nano Lett. 2013;13:581–585. doi: 10.1021/nl304111v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Yu MK, Jeong YY, Park J, Park S, Kim JW, Min JJ, Kim K, Jon S. Drug-loaded superparamagnetic iron oxide nanoparticles for combined cancer imaging and therapy in vivo. Angew Chem Int Ed. 2008;47:5362–5365. doi: 10.1002/anie.200800857. [DOI] [PubMed] [Google Scholar]
- 80.McMeil SE. Challenges for nanoparticle characterization. Methods Mol Biol. 2011;697:9–15. doi: 10.1007/978-1-60327-198-1_2. [DOI] [PubMed] [Google Scholar]
- 81.Clogston JF, Patri AK. Importance of physicochemical characterization prior to immunological studies. Frontiers in Nanobiomedical Research. 2013;1:25–52. [Google Scholar]
- 82.Lynch I, Ahluwalia A, Boraschi D, Byrne HJ, Fadeel B, Gehr P, Gutleb AC, Kendall M, Papadopoulos MG. The bio-nano-interface in predicting nanoparticle fate and behavior in living organisms: towards grouping and categorizing nanomaterials and ensuring nanosafety by design. Bio Nano Mat. 2013;14:195–216. [Google Scholar]
- 83.Dobrovolskaia MA, Germolec DR, Weaver JL. Evaluation of nanoparticle immunotoxicity. Nat Nanotech. 2009;4:411–414. doi: 10.1038/nnano.2009.175. [DOI] [PubMed] [Google Scholar]
- 84.Fourches D, Pu D, Tassa C, Weissleder R, Shaw SY, Mumper RJ, Tropsha A. Quantitative nanostructure-activity relationship modeling. ACS Nano. 2010;4:5703–5712. doi: 10.1021/nn1013484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Puzyn T, Leszczynska D, Leszczynski J. Toward the Development of “Nano-QSARs”: advances and challenges. Small. 2009;5:2494–2509. doi: 10.1002/smll.200900179. [DOI] [PubMed] [Google Scholar]