Abstract
Purpose
The aim of this paper is to demonstrate how informatics applications can support the assessment and visualization of older adults’ wellness. A theoretical framework is presented that informs the design of a technology enhanced screening platform for wellness. We highlight an ongoing pilot demonstration in an assisted living facility where a community room has been converted into a living laboratory for the use of diverse technologies (including a telehealth component to capture vital signs and customized questionnaires, a gait analysis component and cognitive assessment software) to assess the multiple aspects of wellness of older adults.
Methods
A demonstration project was introduced in an independent retirement community to validate our theoretical framework of informatics and wellness assessment for older adults. Subjects are being recruited to attend a community room and engage in the use of diverse technologies to assess cognitive performance, physiological and gait variables as well as psychometrics pertaining to social and spiritual components of wellness for a period of eight weeks. Data are integrated from various sources into one study database and different visualization approaches are pursued to efficiently display potential correlations between different parameters and capture overall trends of wellness.
Results
Preliminary findings indicate that older adults are willing to participate in technology-enhanced interventions and embrace different information technology applications given appropriate and customized training and hardware and software features that address potential functional limitations and inexperience with computers.
Conclusion
Informatics can advance health care for older adults and support a holistic assessment of older adults’ wellness. The described framework can support decision making, link formal and informal caregiving networks and identify early trends and patterns that if addressed could reduce adverse health events.
Keywords: Health promotion, Aging, Informatics, Wellness, Function
1. Introduction
Older adults vary in the development and progression of chronic disease and decline at differing rates in areas of well-being. To help them remain independent, clinicians’ emphasis is on predicting and if possible, minimizing such losses. Functional independence in mobility is essential for independence in health and safety-related activities of daily living [1]. The cognitive faculties that prompt and guide human activities are equally important in preserving independence. As cognitive impairment increases over time, as in dementia, dependence in activities of daily living and inability to be left alone safely may lead to institutionalization increasing societal costs in monetary and human terms [2]. Several efforts have been developed to address a single aspect of older adults’ well-being focusing on one or more specific physiological/functional, social, spiritual or cognitive/mental parameters. In order to support aging in place, however, a holistic approach is needed to assess older adults’ overall wellness. To date, methodologies are lacking that address the holistic and multidimensional assessment of wellness. In this context, identifying problems while they are still small can provide a window of opportunity for interventions that will alleviate problem areas before they become catastrophic. Technology applications have the potential to introduce tools that enable non-obtrusive monitoring and assessment of physiological, functional, cognitive, mental or other parameters of wellness.
The aim of this paper is to demonstrate how informatics applications can support the assessment and visualization of older adults’ wellness. Specifically, we introduce a theoretical framework that informs the design of a technology enhanced screening platform for wellness and describe the methodological approaches. Finally, we present an ongoing pilot demonstration in an assisted living facility where a community room has been converted into a living laboratory for the use of diverse technologies (including a telehealth component to capture vital signs and customized questionnaires, a gait analysis component and cognitive assessment software) to assess the multiple aspects of wellness of older adults and discuss lessons learned.
2. Background
2.1. Wellness
Halbert Dunn defined wellness as “an integrated method for functioning which is oriented toward maximizing the potential of which the individual is capable. It requires that the individual maintain a continuum of balance and purposeful direction within the environment where he/she is functioning [3].” In this definition, Dunn used the term “integrated” to indicate that wellness is affected by multiple components and its assessment includes diverse interrelated parameters. Dunn’s definition originated from the World Health Organization’s definition of health as “a state of complete physical, mental and social well-being, and not merely the absence of disease and infirmity [4].”
Dunn emphasized that the concept of wellness embodied the preventive aspects of disease, disability and social break-down. He highlighted the need to quantify wellness and calls for longitudinal studies that will “permit us to direct the flow of humanity in this way. A new type of preventive medicine can emerge-a preventive medicine which will help us to direct the flow of events and which will allow us to take in time those steps necessary to raise the level of wellness and prevent people from drifting into chronic disease (p. 205) [3]. In this same work, Dunn called for measures to develop understanding and methods of adjustment in one’s life in order to assess and improve wellness in family and community living [3].
Since the in-depth examination of wellness by Dunn, several researchers have further analyzed and highlighted the need to view wellness as a holistic complex concept that is affected by several parameters and the need to support aging following an integrated assessment of internal and external factors for each individual. Hoyman explored the multidimensional unit of health and wellness further by emphasizing that human health needs to examine the whole person in their environment and suggesting that four dimensions are addressed: (1) physical well-being/fitness; (2) mental and cognitive health; (3) social well-being; and (4) spiritual well-being [5]. Since its inception, the Dunn framework of wellness has been tested [6] and informed several health promotion initiatives for older adults [6,7].
2.2. A framework for a technology enhanced assessment of older adults’ wellness
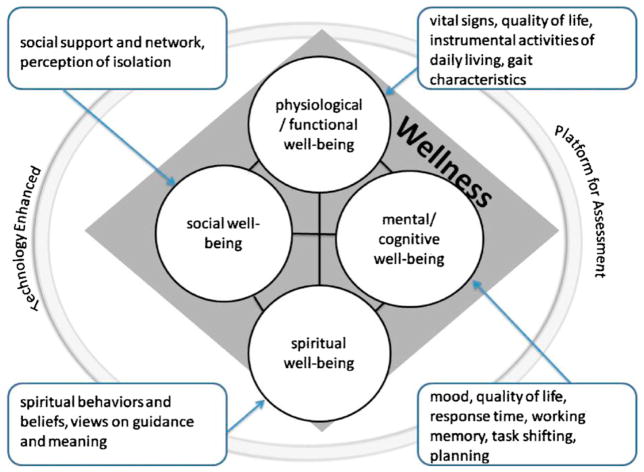
Technology introduces new ways to routinely and unobtrusively assess and identify patterns of elder wellness. Our work is informed by Hoyman and Dunn’s theories as we aim to examine wellness holistically and how the dimensions interrelate (see Fig. 1).
Fig. 1.
The framework for a technology enhanced assessment of older adults’ wellness based on Hoyman’s wellness model.
Physiological parameters including vital signs are basic health status indicators. The ongoing monitoring of physiological parameters can support disease management by detecting trends and patterns prior to the occurrence of adverse health events. Functional independence is essential for independence in activities of daily living related to health and safety. Mobility issues such as impaired gait and balance limit physical activity and contribute to functional decline [8]. As functional independence in mobility declines and overall activity levels decrease, older adults are at increased risk of falls, a major cause of disability and death [9]. Falls or their sequelae often force older adults to leave their homes or apartments and move to assisted living or nursing homes [10,11]. Older adults fear falling and the injuries or loss of independence that may result [12,13]. Health care personnel typically conduct fall risk assessments using instruments created for that purpose [9,14,15]. However, these assessments are conducted in clinical settings rather than real life settings, and in most cases do not lead to customized interventions or behavioral change.
The cognitive and mental faculties that prompt and guide our activities are equally important in preserving independence. Older adults with impaired cognition, such as those with Alzheimer’s disease or other dementia, may forget operating instructions for activities, including how to ask for assistance and recognize unsafe situations. Mental health is an essential component as studies have shown that depression is common in older adults [16].
Social parameters of well-being are critical in the older adult population. Social isolation is more prevalent in older adults because of their diminished vitality and health [17]. Some researchers report rates of social isolation as high as 35% in this population [18]. Research suggest that social support and social integration may provide health and survival benefits to older adults by strengthening coping and recovery when ill or via biological mechanisms that protect against illness [19,20].
Research indicates that spirituality has a positive impact on the health and well-being of older adults [21,22]. Spirituality refers to the most animating or vital issues of life, providing a sense of purpose and meaning in life [23]. Spiritual experiences offer an awareness of inner peace, harmony, hopefulness and compassion for others. In 2001, the Joint Commission on the Accreditation of Healthcare Organization (JCAHO) revised its accreditation standards to require the administration of a spiritual assessment. Spiritual assessments are now mandated in a number of settings, including hospitals, home care organizations, long-term care facilities, and certain behavioral health care organizations such as those providing addiction services [24].
2.3. Comprehensive assessment of wellness
Sets of variables or parameters that are sub-categories of wellness have been explored pair-wise to assess how they may interrelate. For example, functional decline has been found to correlate with cognitive decline in Parkinson’s disease (PD) and Alzheimer’s disease (AD) patients [25]. Similarly, improved functional ability as a result of structured strength and balance training has been found to increase cognitive function in frail, cognitive impaired elderly long-term care residents [26]. Social isolation was found to be associated with slower post-task recovery of systolic blood pressure, a higher cholesterol response to stress, and also with larger cortisol awakening responses and greater cortisol output over the day [27]. Scientific literature also indicates that spirituality may affect blood pressure, immune function, depression, and mortality [28]. These are only a few examples of an extensive body of literature that examines the relationship between distinct parameters. When examining older adults who are community dwelling or in long term care facilities, the emphasis needs to be on a multitude of parameters, as older adults have different and complex needs. The holistic view of wellness which is based on assessment of multiple parameters allows for a comprehensive examination of one’s well-being and potential barriers to wellness.
2.4. Visualization to support clinical decision making
Technological advances are enabling us to collect and store ever-increasing amounts of multivariable clinical data. As we increase the amount of data we collect, we need to ensure that the plethora of data sets does not become burdensome to clinicians, patients, families and other end users, but instead facilitates decision making. New and efficient methods of visualization are needed to help manage this abundance of information. The challenge of efficient visualization is a critical one as published studies suggest that the formats used to display information can have an impact on the quality and timeliness of clinical decisions, with the specific, optimal formats depending on the nature of the data and decision tasks [29,30]. Elting et al. found that data display formats influenced physician investigators’ decision to stop a clinical trial [31]. Specifically, they found that the accuracy of clinicians’ decision was affected by the type of data display with more correct decisions made with icon displays than with tables and bar graphs. Their findings indicate the importance that needs to be placed on the approach by which data are summarized and displayed in order to reduce the impact that factors unrelated to the actual data may have on clinical decision making.
Capturing overarching concepts such as wellness or quality of life requires the use of visualization tools that will most efficiently capture information both on a macro-level (assessing the overall pattern or status) and on a micro-level (examining trends for individual parameters over time). There are general recommendations or guidelines available as to how best to display quantitative information graphically, although these tend not to be empirically based [32]. While research efforts have explored the cognitive processing principles that underlie the interpretation of different graphical presentations [33], it remains unclear as to which type of presentation would best convey complex data such as wellness information. Inherent in determining which formats are best to convey the data is the need to consider the level of complexity that end users want from the data, for example, trends for a group over time, individual parameters and trends, variability between constructs within a patient or within patients or other descriptions. Therefore, it is important to explore the best visualization approach for wellness by assessing clinicians’ information needs and expectations as well as their feedback as to which visual tools can convey appropriate information and enhance clinical decision making.
2.5. A demonstration pilot approach
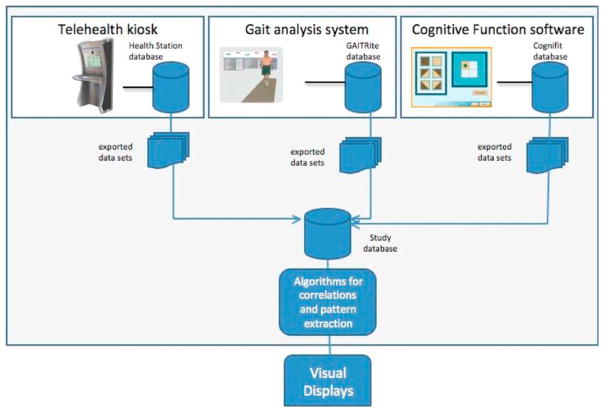
We describe an informatics application that utilizes diverse and innovative technologies (including a telehealth component to capture vital signs and customized questionnaires, cognitive assessment software and a gait analysis system) to assess older adults’ wellness. This platform pursues a holistic approach of wellness integrating data capturing physiological, functional, cognitive, mental, spiritual and social aspects of elders’ well-being. It also focuses on the synthesis of multiple data sources to provide a holistic assessment of wellness designed to enhance clinical decision making and support a personal health record system. It utilizes existing hardware systems and focuses on data integration, processing and visualization contributing to a better understanding of inter-operability of monitoring systems and maximizing knowledge generation using multiple data sources.
2.6. Platform architecture
The platform integrates three existing components, GAITRite (a software application that captures functional parameters), a telehealth kiosk (a community health kiosk that assesses physiological parameters and includes individualized questionnaires assessing social and spiritual well-being) and CogniFit (a software application that assesses cognitive parameters) (See Fig. 2 for system architecture).
Fig. 2.
The system architecture.
Health station (Health anywhere, Inc.) is a site-based health management platform designed to be installed at specialized locations. Health station provides users secure access to their patient profile with the ability to capture relevant vital sign data into their personal health record, and to view pertinent nutritional or educational content. This platform is well adapted for screening and early detection, assessment, and wellness promotion purposes. The kiosk comes with standard wireless medical devices, namely a blood pressure and heart rate monitor, glucometer, pulse oximeter and weight scale. It operates over regular phone lines, DSL, WiFi and broadband. Each user who is registered with the system receives a unique ID card that can be swiped to identify the resident prior to any session. Thus the kiosk can be used by multiple users from a single location and provide personalized monitoring.
CogniFit (CogniFit Inc.) is a brain fitness web-based software solution. This system includes a series of steps that enable the assessment and over time the improvement of several key cognitive abilities including awareness, divided attention, eye–hand coordination, speed of processing and response time, visual perception, visual scanning and working memory. This software system has been tested for reliability and validity [34]. There are significant and strong relationships between the system’s assessment and the full Cambridge Neuropsychological Test Automated Battery (CANTAB) [34]. In addition, the software system has been used in a wide range of populations for research purposes including persons with multiple sclerosis, older adults with insomnia, and older adults at risk for cognitive decline in addition to its widespread commercial use [34–36].
GAITRite (CIR Systems Inc.) includes an electronic walkway and a software system. Encapsulated within the electronic walkway are sensor pads. Each sensor pad has an active area of 24 in.2 and contains 2304 sensors arranged in a 48 × 48 grid pattern. The sensors are placed on .5 in. centers. Multiple sensor pads are connected to form the desired length of the walkway. As the subject ambulates across the walkway, the pressure exerted by the feet onto the walkway activates the sensors. The walkway senses not only the geometry of the activating objects but also the relative arrangement between them in a two dimensional space. Furthermore, the walkway senses the vertical component of the relative pressure exerted by the objects. Special algorithms build into the software system enable the data collected from the walkway to support extensive gait analysis. The algorithms isolate the objects and identify them as footprints.
The software system calculates and provides for each subject and each session (a) a footprint analysis (including identification of the quadrilateral, heel, mid and toe areas, the centroids and twelve quadrilaterals); (b) spatial parameters (including line of progression, stride length, step length, step/extremity ratio); (c) temporal definitions (including step time, gait cycle time, ambulation time, velocity, stride velocity); and (d) switching levels. This system has been used extensively in research studies and has demonstrated high reliability and validity [37–39]. There is a high degree of agreement between the electronic walkway and the gold standard 3D motion capture systems for both healthy and diseased older adult populations [40–43].
2.7. Setting
The setting for our pilot study is a retirement community in Seattle, WA. It consists of a mix of approximately 150 private apartment homes for persons 62 and older which have the ability to be converted into assisted living residences as needed. Within this facility, a community room accessible to all residents has been converted into a “living laboratory” to evaluate the aforementioned informatics application to aid in the assessment and enhancement of older adults’ wellness.
2.8. Subjects
Eligibility criteria for study participants included: (1) age of 65 years or older; (2) residents of the participating facility; (3) able to speak, read and write English; (4) independent in activities of daily living (ADL) as assessed by the Katz Instrument of Activities of Daily Living scale [44]; (5) ambulatory (but may use assistive devices); (6) able to provide informed consent; (7) not planning to leave the area for approximately two months after consent; (8) adequate visual acuity to read computer screen.
2.9. Procedures and measures
All procedures were approved by the Institutional Review Board (IRB) of the University of Washington and the participating facility. Subjects were asked to participate in the study for two months. Information sessions were conducted at the facility asking for interested persons to provide phone contact information for follow-up. After determining that participants meet the eligibility criteria, they were asked to attend an initial visit to provide informed consent. At the initial visit, individuals also completed the Subject Information Form (SIF) which includes demographic items, co-morbid health conditions [45] and current medications, and a series of computerized questionnaires (see Table 1).
Table 1.
Data collection parameters for wellness.
| Measure | Source/instrument | Frequency | Performance | |
|---|---|---|---|---|
| Functional/physiological parameters | Activities of daily living | Self-report Katz instrument of activities of daily living (ADLs) scale | At baseline and exit (at 8 weeks) | Reliability 0.87 to 0.94 [46,47] good construct and content validity [48]. |
| Instrumental activities of daily living | Self-report Lawton instrumental activities of daily living (IADLs) scale | At baseline and exit (8 weeks) | Inter-rater reliability .85. The validity was tested in 180 subjects, all correlations significant at .01 or .05 level [49] | |
| Health-related quality of life | CDC HRQOL-4 self-report (health station) | Monthly | Good construct & concurrent validity [50]; test–retest reliability 0.58–0.75 & strong internal validity [51] | |
| Blood pressure, weight, heart rate, oxygen saturation, finger stick blood glucose | Health station peripherals | Weekly | FDA approved class II medical devices. Meters will be tested by staff to ensure quality control against high/low standards. | |
| Height | Assessed by staff | At baseline | ||
| Gait speed | GAITRite | Weekly | CV% 3.5% | |
| Stride length | CV% R: 3.5% L: 3.1% | |||
| Stride width | CV% 15.2% [52] | |||
| Double limb support time | ICC 44–57% [37] | |||
| Stride to stride variability | ICC 91–99% [53] | |||
| Cognitive/mental parameters | Speed of processing and response time; working memory; task shifting; planning | CogniFit | 3 times a week | Internal consistency 0.70, test–retest reliability 0.80 [34] 72 |
| Mood assessment | Patient health questionnaire (PHQ-2): a two item tool to assess the frequency of depressed mood and anhedonia. | At baseline and exit | Sensitivity of 83% and a specificity of 92% for major depression [54] | |
| Social well-being | Social support | Multidimensional scale of perceived social support (MSPSS): 12-item tool to measure one’s perception of social support from family, friends or others | At baseline and exit | Cronbach’s alpha 0.88 test–retest reliability 0.85 [55] |
| Spiritual well-being | Spiritual perspectives | Self-report spiritual perspective scale (SPS): 10-item tool to measure the extent to which individuals hold spiritual beliefs and engage in spiritually related behaviors [56] | At baseline and exit | Cronbach’s alpha 0.93–0.95; test–retest 0.57–0.68 [56] |
During the next 8 weeks subjects visit the living laboratory three times a week to provide cognitive assessment data (for approx. 20 min per session); during one of these sessions each week they also provide physiological/functional data (which requires approx. 5 min) and walk on the GaitRite mat to enable collection of gait related datasets (see Table 1). The parameters were chosen because they can be easily assessed in a cost-effective manner within residential settings by older adults themselves with no or minimal assistance and can serve as indicators for the underlying wellness components (per our theoretical framework).
The platform integrates data from the three components (Health station, GAITRite and CogniFit) into one database (the study database) (see Fig. 2). All three existing systems store collected data in secure web servers with the capability to export datasets in multiple formats including SPSS and Excel files. These datasets are imported into the study database weekly (the subject identification number is used across all three components to link all datasets for each subject). The study database has been developed as a web-based application system using Oracle 8 and ASP 3.0. To facilitate the visualization of data, we use a PHP script to take database data and generate the displays in Scalable Vector Graphics (SVG), an Extensible Markup Language (XML) application for representing vector graphics information. The SVG is then rendered in a web browser using the Adobe SVG plug-in. The interactive effects and calculations in the interactive graphical modality are implemented as client-side JavaScript, which manipulates the Document Object Model (DOM) of the SVG as part of a high-fidelity visualization prototype.
The design of visualization approaches is currently ongoing and is driven by two key characteristics: (1) an intensive, highly integrated partnership among the research team and prospective users; and (2) an extremely nimble and efficient approach to data collection, analysis, and use in design. This approach interrogates the concept of a “release” by proposing to produce a more fluid evolution of successive versions of an application. This fluid evolution mirrors the success that web-based software development has experienced by continually releasing new versions of a site with incremental changes to an initial alpha release [57,58]. The design process is characterized by a convergence of analysis and synthesis as hypothesis-building during design. We are using a cyclical design process model, the design cycle conceptualized by Dr. Roesler [59], which coordinates three pools of design expertise: field studies—what is interesting; ideation—what is promising; and detailed design—what is required. In this pilot study we are focusing on the detailed design and soliciting feedback from end users (including health care providers and older adults) to create working prototypes of visualization interfaces for wellness.
The benefit of using this design cycle method compared to the conventional iterative Human Computer Interaction approach [60–62] is that it facilitates a continuous cyclical process where iterative loops can be connected between any of its stages where required. In the conventional model of iterative refinement of a given prototype, designers can find themselves locked in, both procedurally and psychologically, by the constraints imposed by earlier choices and efforts [59,63,64]. Expanding the iterative loop allows us to adapt the positive aspects of the conventional iterative design model (insight and improvement based on prototyping) and integrate these with the strength of visualization and mock-up techniques during design ideation and observation, so that insight from low fidelity prototyping can re-direct explanatory models, and design ideation to lead to wholly revised low-cost prototypes. Our approach will enable the team to easily and flexibly roll back to an earlier, different design concept and take a different design direction for the next prototype.
2.10. Preliminary findings
In our pilot study we recruited 27 subjects (9 male and 18 female) with an average age of 88.2 years (age range 78–94 years). The majority of subjects reported a high educational level with 52% having a graduate degree; 32% had earned an undergraduate degree, 12% completed community college, and 4% had a high school diploma. Responses were diverse in terms of prior experience with computers, with 12% of all participants being highly comfortable, 52% moderately comfortable, 28% slightly comfortable. Two subjects (8%) reported having no prior experience with computers. Comfort with computers correlated with educational level (r = 0.4). Overall participants reported limited, if any, engagement in spiritual activities. Social support available to participants was primarily from family members, and was rated as high. Friends were perceived as providing social support to a much lesser extent, as many persons noted that contact with those they classified as friends was limited due to relocation to the facility or death of friends.
The mean number of chronic health conditions reported by participants was 4.2 (ranging from 0 chronic conditions to 9). The most common health conditions reported were cancer (48%), high blood pressure (44%) and cardiac arrhythmias (44%). Despite the presence of multiple chronic conditions participants generally rated their overall health as excellent (17%) or very good (67%), on the CDC-HRQOL-4 questionnaire. Only twelve percent of participants rated their health as good (8%), or poor (4%). During their participation, 15% of all subjects experienced a fall, and 11% had an unplanned visit to the emergency room or the hospital indicating that health status was not stable for all participants during the pilot study.
In terms of cognitive performance, an increased number of chronic diseases negatively correlated with planning (r = −.52, p = 0.016). Additionally, increased age was negatively correlated with cognitive tasks associated with divided attention (r = −.48, p = .029), planning (r = −.53, p = .013), and spatial perception (r = −.718, p < 0.0005). In comparing cognitive performance by gender, males were significantly better able than females to task shift (p = 0.03).
The amount of assistance needed for subjects to operate the technology decreased over time. Most users became independent in very short time (approximately 1 week) requiring only occasional or no assistance thereafter. Alerts generated by the telehealth kiosk led to medication adjustments for one subject and closer monitoring of blood pressure in three subjects (two due to previously undiagnosed hypertension and one due to labile blood pressure). Focus group sessions assessed participants’ overall attitudes and perceptions. Subjects were very accepting of the technology pointing out its ease of use and the opportunity to engage meaningfully in cognitive performance activities and monitoring of vital signs. Participants also commented on the opportunity to socialize and interact with other residents in a community setting. None of the participants had privacy concerns about the use of technology in a community room or the electronic capture and transmission of health related data.
3. Lessons learned
3.1. Technology acceptance
In our study, older adults have embraced the diverse technology tools and appreciated the potential value for their wellness. In our initial presentation of the study, approximately 50% of all attendees (N = 65) expressed interest in participating in the study even though remuneration was minimal and participant burden at this stage of our exploratory research may be elevated compared to later phases that would use a subset of currently measured variables. Participants have expressed strong positive impressions of the available technology, the ability to capture vital signs and transmit via Bluetooth, but also the opportunities that arise from a personal health record with information that can be shared at their discretion with their family and/or health care provider. As there are varying levels of computer experience among older adult participants, we pursued a gradual roll-out approach where technologies were introduced to participants in phases (e.g., participants first get introduced to the Health station and CogniFit and at a later point they are exposed to the GaitRite). It was necessary to have technical support available from research staff as well as diverse tools to account for user preferences (e.g., the two-button mouse has been challenging for some participants, others were more familiar with the mouse they have been using; as a result we provided multiple options for users to choose the tool they are most comfortable or familiar with). Our participants had different levels of comfort with and expertise in using the technology with some being able to operate all software and hardware by themselves and others requiring occasional assistance. Finally, older adults with specific health issues (e.g., tremor, use of hearing aids) require customized training and assistance.
3.2. Attrition
As the study requires subjects to be enrolled for a period of two months, attrition issues were anticipated. To address this, we made great effort to first screen residents and to maintain contact, via careful and personalized attention, including weekly in-person contact, as needed phone calls to subjects to maintain adherence to the research protocol to ensure minimum of dropout over the 2-month follow-up [65]. In the course of the study 7 participants discontinued participation prior to completion. Reasons for attrition varied and included: death of spouse (1), illness/hospitalization (3), and other time commitments (3).
3.3. Multi-user approach
The approach of this study was that of a multi-user community wellness setting. This model of a community setting has the advantages of being cost-effective (eliminating the need for monitoring equipment to be installed in every residence) as well as promoting social interactions among users (several new residents of the facility enrolled in the study partly to meet other participants). On the other hand, this multi-user approach bears scheduling logistical challenges for the use of hardware stations and the risk of privacy violations if personal health information is visible or otherwise accessible to others. To address these challenges, we introduced a sign up log for the equipment and the setting was designed to maximize privacy for each user.
3.4. Personal health record
The notion of a personal health record (PHR) system that is accessed, maintained and updated by patients themselves has not been widely explored with older adults. In our demonstration project, end users belong to the “oldest old” category (i.e., over the age of 85) and preliminary findings highlight the potential of PHR applications for older adults themselves but also their families, formal and informal caregiving networks. Older adults can choose other stakeholders who can have access rights to their overall wellness information, and the holistic assessment of wellness allows both health care providers and informal caregivers to be always informed of patterns and trends. A PHR system could ultimately support decision making in transitions of care as residents in facilities and their families often are faced with difficult decisions without full access to all relevant information as well as ultimately to potential prevention of adverse health events.
4. Conclusion
Informatics can play a significant role in advancing gerontology and geriatric care. Technology has the potential to address the challenge of rising costs for elder care. It can specifically target the limited resources, lack of continuity of care and care fragmentation, as well as healthcare workforce shortage that are well documented barriers to high quality geriatric care. Different tools can be utilized to assess information about older adults’ well-being but also make that information accessible to older adults themselves. PHR systems have not been extensively evaluated for older adults but can play a great role as they address a significant need to link the informal and formal caregiving networks. We propose a holistic approach to wellness that can identify areas for early and individualized interventions as well as enable facilities to identify gaps in programmatic offerings. Our demonstration project addresses data integration from several commercially available applications and supports different techniques to visualization of wellness. The visualization aspect is significant as it can reduce the burden of information overload (especially in cases of numerous and extensive data sets collected at a regular frequency) and enhance decision making and early trend detection.
Our pilot study confirms the feasibility of an informatics platform to assess older adults’ wellness and indicates end user acceptance. Our sample size in this study was not large enough to allow for more robust statistical techniques such as cluster analysis; however, findings indicate that wellness components appear to be correlated. This indicates that further research to enable a quantitative and holistic assessment of wellness is warranted.
The availability of wellness assessment informatics tools within a community setting or residential facility introduces new features for built environments targeting older adults with clear public health implications.
Perdue, Gostin and Stone discuss a recent shift in public health interest to the physical environment as a major factor in chronic disease rates and observe that a “beneficial impact of this new public health focus on the built environment is that it invites exploration of new solutions to some of the leading public health problems of today [66].” Brown et al. highlight in their work that some features of the built environment increase perceived social support that leads to reduction in psychological distress and can have a positive effect on mental health in elders [67]. Gerontological informatics interventions that link informal and formal caregiving networks may be new factors that contribute to future increases in perceived social support in elders on a population-level through wide-scale community-based interventions. One way to reach these population goals may be through interventions that synthesize community-level factors of the built environment, such as accessible and available community settings for health and wellness monitoring, and social context, such as community investment and fiscal policies. As Northridge, Sclar and Biswas reflect, “these types of interventions may have the greatest potential benefit for improved population health and well-being” [68] and informatics can play a significant role in facilitating the efforts to improve accessible and holistic health care services for older adults.
Summary points.
Existing knowledge on challenges in delivering health care to older adults:
Sets of variables or parameters that are sub-categories of wellness have been explored pair-wise to assess how they may interrelate (e.g., functional decline and cognitive performance or physiological and social parameters). There is a lack of efforts to holistically assess wellness of older adults and investigate a multitude of parameters for diverse and complex needs within this population.
Information technology has been used in gerontology before, but concerns have been raised about user acceptance and satisfaction with new information tools.
Informatics applications have been traditionally introduced in a clinical setting or in one’s private home; the concept of community based informatics platforms has not been explored widely.
What this study added:
Older adults are willing to participate in technology-enhanced interventions and embrace different information technology applications given appropriate and customized training and hardware and software features that address potential functional limitations and inexperience with computers.
Informatics can support and facilitate the holistic assessment of older adults’ wellness.
The described framework of informatics based wellness assessment supports a holistic view of older adults’ needs, facilitates decision making, links formal and informal caregiving networks and can lead to identification of early trends and patterns that if addressed could reduce adverse health events.
References
- 1.Rose DJ. FallProof: A Comprehensive Balance and Mobility Training Program. Human Kinetics; Champaign, IL: 2003. [Google Scholar]
- 2.Caro J, Ward A, Ishak K, Migliaccio-Walle K, Getsios D, Papadopoulos G, Torfs K. To what degree does cognitive impairment in Alzheimer’s disease predict dependence of patients on caregivers? BMC Neurology. 2002;2:6. doi: 10.1186/1471-2377-2-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dunn HL. High-Level Wellness. R.W. Beatty, Ltd; Virginia: 1961. [Google Scholar]
- 4.World Health Organization. Preamble to the Constitution of the World Health Organization. International Health Conference; 1946; New York. 1946. p. 100. [Google Scholar]
- 5.Hoyman HS. Rethinking an ecologic-system model of man’s health, disease, aging, death. Journal of School Health. 1975;45(9):509–518. doi: 10.1111/j.1746-1561.1975.tb04527.x. [DOI] [PubMed] [Google Scholar]
- 6.Martin CA. Nursing for Wellness in Older Adults. 5. Lippincott Williams & Wilkins; Philadelphia: 2008. [Google Scholar]
- 7.Kleffel D. Rethinking the environment as a domain of nursing knowledge. ANS Advances in Nursing Science. 1991;14(1):40–51. doi: 10.1097/00012272-199109000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Myers AH, Young Y, Langlois JA. Prevention of falls in the elderly. Bone. 1996;18(Suppl 1):87S–101S. doi: 10.1016/8756-3282(95)00384-3. [DOI] [PubMed] [Google Scholar]
- 9.Tinetti ME. Clinical practice, preventing falls in elderly persons. New England Journal of Medicine. 2003;348(1):42–49. doi: 10.1056/NEJMcp020719. [DOI] [PubMed] [Google Scholar]
- 10.Aditya BS, Sharma JC, Allen SC, Vassallo M. Predictors of a nursing home placement from a non-acute geriatric hospital. Clinical Rehabilitation. 2003;17(1):108–113. doi: 10.1191/0269215503cr567oa. [DOI] [PubMed] [Google Scholar]
- 11.Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. New England Journal of Medicine. 1997;337(18):1279–1284. doi: 10.1056/NEJM199710303371806. [DOI] [PubMed] [Google Scholar]
- 12.Fletcher PC, Hirdes JP. Restriction in activity associated with fear of falling among community-based seniors using home care services. Age and Ageing. 2004;33(3):273–279. doi: 10.1093/ageing/afh077. [DOI] [PubMed] [Google Scholar]
- 13.Kressig RW, Wolf SL, Sattin RW, O’Grady M, Greenspan A, Curns A, Kutner M. Associations of demographic, functional, and behavioral characteristics with activity-related fear of falling among older adults transitioning to frailty. Journal of the American Geriatrics Society. 2001;49(11):1456–1462. doi: 10.1046/j.1532-5415.2001.4911237.x. [DOI] [PubMed] [Google Scholar]
- 14.Rubenstein LZ, Solomon DH, Roth CP, Young RT, Shekelle PG, Chang JT, MacLean CH, Kamberg CJ, Saliba D, Wenger NS. Detection and management of falls and instability in vulnerable elders by community physicians. Journal of the American Geriatric Society. 2004;52(9):1527–1531. doi: 10.1111/j.1532-5415.2004.52417.x. [DOI] [PubMed] [Google Scholar]
- 15.Tromp AM, Pluijm SM, Smit JH, Deeg DJ, Bouter LM, Lips P. Fall-risk screening test: a prospective study on predictors for falls in community-dwelling elderly. Journal of Clinical Epidemiology. 2001;54(8):837–844. doi: 10.1016/s0895-4356(01)00349-3. [DOI] [PubMed] [Google Scholar]
- 16.Blazer DG. Depression in Late Life. 3. Mosby Year Book; St. Louis: 2002. [Google Scholar]
- 17.Bondevik M, Skogstad A. The oldest old, ADL, social network, and loneliness. Western Journal of Nursing Research. 1998;20(3):325–343. doi: 10.1177/019394599802000305. [DOI] [PubMed] [Google Scholar]
- 18.Tremethick MJ. Alone in a crowd. A study of social networks in home health and assisted living. Journal of Gerontological Nursing. 2001;27(5):42–47. doi: 10.3928/0098-9134-20010501-10. [DOI] [PubMed] [Google Scholar]
- 19.Ford ES, Loucks EB, Berkman LF. Social integration and concentrations of C-reactive protein among US adults. Annals of Epidemiology. 2006;16(2):78–84. doi: 10.1016/j.annepidem.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 20.Loucks EB, Berkman LF, Gruenewald TL, Seeman TE. Relation of social integration to inflammatory marker concentrations in men and women 70 to 79 years. American Journal of Cardiology. 2006;97(7):1010–1016. doi: 10.1016/j.amjcard.2005.10.043. [DOI] [PubMed] [Google Scholar]
- 21.Koenig HG. Religion, well-being and health in the elderly: the scientific evidence for an association. In: Thorson JA, editor. Perspectives on Spiritual Well-Being and Aging 2000. Charles C. Thomas; Springfield, IL: 2000. pp. 84–97. [Google Scholar]
- 22.McFadden SH. Religion and well-being in aging persons in an aging society. Journal of Social Issues. 1995;51:161–175. [Google Scholar]
- 23.Lawler-Row KA, Elliott J. The role of religious activity and spirituality in the health and well-being of older adults. Journal of Health Psychology. 2009;14(1):43–52. doi: 10.1177/1359105308097944. [DOI] [PubMed] [Google Scholar]
- 24.Hodge DR. A template for spiritual assessment: a review of the JCAHO requirements and guidelines for implementation. Social Work. 2006;51(4):317–326. doi: 10.1093/sw/51.4.317. [DOI] [PubMed] [Google Scholar]
- 25.Sabbagh MN, Lahti T, Connor DJ, Caviness JN, Shill H, Vedders L, Mahant P, Samanta J, Burns RS, Evidente VG, et al. Functional ability correlates with cognitive impairment in Parkinson’s disease and Alzheimer’s disease. Dementia and Geriatric Cognitive Disorders. 2007;24(5):327–334. doi: 10.1159/000108340. [DOI] [PubMed] [Google Scholar]
- 26.Dorner T, Kranz A, Zettl-Wiedner K, Ludwig C, Rieder A, Gisinger C. The effect of structured strength and balance training on cognitive function in frail, cognitive impaired elderly long-term care residents. Aging Clinical and Experimental Research. 2007;19(5):400–405. doi: 10.1007/BF03324721. [DOI] [PubMed] [Google Scholar]
- 27.Grant N, Hamer M, Steptoe A. Social isolation and stress-related cardiovascular, lipid, and cortisol responses. Annals of Behavioral Medicine. 2009;37(1):29–37. doi: 10.1007/s12160-009-9081-z. [DOI] [PubMed] [Google Scholar]
- 28.Townsend M, Kladder V, Ayele H, Mulligan T. Systematic review of clinical trials examining the effects of religion on health. Southern Medical Journal. 2002;95(12):1429–1434. [PubMed] [Google Scholar]
- 29.Brundage M, Feldman-Stewart D, Leis A, Bezjak A, Degner L, Velji K, Zetes-Zanatta L, Tu D, Ritvo P, Pater J. Communicating quality of life information to cancer patients: a study of six presentation formats. Journal of Clinical Oncology. 2005;23(28):6949–6956. doi: 10.1200/JCO.2005.12.514. [DOI] [PubMed] [Google Scholar]
- 30.Hoeke JO, Bonke B, van Strik R, Gelsema ES. Evaluation of techniques for the presentation of laboratory data: support of pattern recognition. Methods of Information in Medicine. 2000;39(1):88–92. [PubMed] [Google Scholar]
- 31.Elting LS, Martin CG, Cantor SB, Rubenstein EB. Influence of data display formats on physician investigators’ decisions to stop clinical trials: prospective trial with repeated measures. British Medical Journal. 1999;318(7197):1527–1531. doi: 10.1136/bmj.318.7197.1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tufte ER. The Visual Display of Quantitative Information. Graphics Press; Cheshire, CT: 1983. [Google Scholar]
- 33.Cleveland WS, McGill R. Graphical perception: theory, experimentation and application to the development of graphical methods. Journal of American Statistical Association. 1984;79:531–554. [Google Scholar]
- 34.Haimov I, Hanuka E, Horowitz Y. Chronic insomnia and cognitive functioning among older adults. Behavioral Sleep Medicine. 2008;6(1):32–54. doi: 10.1080/15402000701796080. [DOI] [PubMed] [Google Scholar]
- 35.Korczyn AD, Peretz C, Aharonson V, Giladi N. 10th International Hong Kong/Springfield Pan-Asian Symposium on Advances in Alzheimer Therapy; Hong Kong. 2008. [Google Scholar]
- 36.Shatil E, Korczyn AD, Peretz C, Breznitz S, Aharonson V, Giladi N. Improving cognitive performance in elderly subjects using computerized cognitive training Alzheimer’s association. ICAD – International Conference on Alzheimer’s Disease; Chicago. 2008. [Google Scholar]
- 37.Bilney B, Morris M, Webster K. Concurrent related validity of the GAITRite walkway system for quantification of the spatial and temporal parameters of gait. Gait & Posture. 2003;17(1):68–74. doi: 10.1016/s0966-6362(02)00053-x. [DOI] [PubMed] [Google Scholar]
- 38.McDonough AL, Batavia M, Chen FC, Kwon S, Ziai J. The validity and reliability of the GAITRite system’s measurements: A preliminary evaluation. Archives of Physical Medicine and Rehabilitation. 2001;82(3):419–425. doi: 10.1053/apmr.2001.19778. [DOI] [PubMed] [Google Scholar]
- 39.Selby-Silverstein L, Besser M. Accuracy of the GAITRite system for measuring temporal-spatial parameters of gait. Physical Therapy. 1999;79:59. [Google Scholar]
- 40.Allali G, Assal F, Kressig RW, Dubost V, Herrmann FR, Beauchet O. Impact of impaired executive function on gait stability. Dementia and Geriatric Cognitive Disorders. 2008;26(4):364–369. doi: 10.1159/000162358. [DOI] [PubMed] [Google Scholar]
- 41.Callisaya ML, Blizzard L, Schmidt MD, McGinley JL, Srikanth VK. Sex modifies the relationship between age and gait: a population-based study of older adults. The Journals of Gerontology Series A, Biological Sciences and Medical Sciences. 2008;63(2):165–170. doi: 10.1093/gerona/63.2.165. [DOI] [PubMed] [Google Scholar]
- 42.Stokic DS, Horn TS, Ramshur JM, Chow JW. Agreement between temporospatial gait parameters of an electronic walkway and a motion capture system in healthy and chronic stroke populations. American Journal of Physical Medicine & Rehabilitation. 2009;88(6):437–444. doi: 10.1097/PHM.0b013e3181a5b1ec. [DOI] [PubMed] [Google Scholar]
- 43.Yang YR, Lee YY, Cheng SJ, Lin PY, Wang RY. Relationships between gait and dynamic balance in early Parkinson’s disease. Gait & Posture. 2008;27(4):611–615. doi: 10.1016/j.gaitpost.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 44.Katz S, Downs TD, Cash HR, Grotz RC. Progress in development of the index of ADL. The Gerontologist. 1970;10(1):20–30. doi: 10.1093/geront/10.1_part_1.20. [DOI] [PubMed] [Google Scholar]
- 45.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Medical Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 46.Ciesla JR, Shi L, Stoskopf CH, Samuels ME. Reliability of Katz’s activities of daily living scale when used in telephone interviews. Evaluation and the Health Professions. 1993;16(2):190–203. doi: 10.1177/016327879301600204. [DOI] [PubMed] [Google Scholar]
- 47.Hamrin E, Lindmark B. Evaluation of functional capacity after stroke as a basis for active intervention: a comparison between an Activity Index and the Katz Index of ADL. Scandinavian Journal of Caring Sciences. 1988;2(3):113–122. [Google Scholar]
- 48.Brorsson B, Asberg KH. Katz index of independence in ADL, Reliability and validity in short-term care. Scandinavian Journal of Rehabilitation Medicine. 1984;16(3):125–132. [PubMed] [Google Scholar]
- 49.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. The Gerontologist. 1969;9(3):179–186. [PubMed] [Google Scholar]
- 50.Ounpuu S, Chambers LW, Chan D, Yusuf S. Validity of the US behavioral risk factor surveillance system’s health related quality of life survey tool in a group of older Canadians. Chronic Diseases in Canada. 2001;22(3–4):93–101. [PubMed] [Google Scholar]
- 51.Andresen EM, Catlin TK, Wyrwich KW, Jackson-Thompson J. Retest reliability of surveillance questions on health related quality of life. Journal of Epidemiology and Community Health. 2003;57(5):339–343. doi: 10.1136/jech.57.5.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Menz HB, Latt MD, Tiedemann A, Mun San Kwan M, Lord SR. Reliability of the GAITRite walkway system for the quantification of temporo-spatial parameters of gait in young and older people. Gait & Posture. 2004;20(1):20–25. doi: 10.1016/S0966-6362(03)00068-7. [DOI] [PubMed] [Google Scholar]
- 53.Webster KE, Wittwer JE, Feller JA. Validity of the GAITRite walkway system for the measurement of averaged and individual step parameters of gait. Gait & Posture. 2005;22(4):317–321. doi: 10.1016/j.gaitpost.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 54.Kroenke K, Spitzer RL, Williams JB. The patient health questionnaire-2: validity of a two-item depression screener. Medical Care. 2003;41(11):1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 55.Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the multidimensional scale of perceived social support. Journal of Personal Assessment. 1990;55(3–4):610–617. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- 56.Reed PG. Spirituality and well-being in terminally ill hospitalized adults. Research in Nursing & Health. 1987;10(5):335–344. doi: 10.1002/nur.4770100507. [DOI] [PubMed] [Google Scholar]
- 57.Musser J. Web 2.0 Principles and Best Practices O’Reilly Radar. 2008. [Google Scholar]
- 58.Rico DF. Effects of agile methods on website quality for electronic commerce. Proceedings of the 41st Annual Hawaii International Conference on System Sciences; 2007; Hawaii. 2007. [Google Scholar]
- 59.Roesler A, Woods DD, Feil M. Inventing the Future of Cognitive Work. International Conference of the European Academy of Design; 2005; 2005. [Google Scholar]
- 60.Gould JD, Lewis C. Designing for usability: key principles and what designers think. Commununication of the Association for Computing Machinery. 1985;28(3):300–311. [Google Scholar]
- 61.Norman DA, Draper SW. User Centered System Design; New Perspectives on Human-Computer Interaction. L. Erlbaum Associates Inc; 1986. [Google Scholar]
- 62.Greenbaum J, Kyng M, editors. Design at Work: Cooperative Design of Computer Systems. L. Erlbaum Associates Inc; 1992. [Google Scholar]
- 63.Cooper A. The Inmates Are Running the Asylum. Macmillan Publishing Co., Inc; 1999. [Google Scholar]
- 64.Landay JA, Myers BA. Sketching interfaces: toward more human interface design. IEEE Computer. 2001;34(3):56–64. [Google Scholar]
- 65.Richmond TS, Thompson HJ, Kauder D, Robinson KM, Strumpf NE. A feasibility study of methodological issues and short-term outcomes in seriously injured older adults. American Journal of Critical Care. 2006;15(2):158–165. [PubMed] [Google Scholar]
- 66.Perdue WC, Gostin LO, Stone LA. Public health and the built environment: historical, empirical, and theoretical foundations for an expanded role. Journal of Law and Medicine Ethics. 2003;31(4):557–566. doi: 10.1111/j.1748-720x.2003.tb00123.x. [DOI] [PubMed] [Google Scholar]
- 67.Brown SC, Mason CA, Lombard JL, Martinez F, Plater-Zyberk E, Spokane AR, Newman FL, Pantin H, Szapocznik J. The relationship of built environment to perceived social support and psychological distress in Hispanic elders: the role of “eyes on the street”. The Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 2009;64(2):234–246. doi: 10.1093/geronb/gbn011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Northridge ME, Sclar ED, Biswas P. Sorting out the connections between the built environment and health: a conceptual framework for navigating pathways and planning healthy cities. Journal of Urban Health. 2003;80(4):556–568. doi: 10.1093/jurban/jtg064. [DOI] [PMC free article] [PubMed] [Google Scholar]