Abstract
Objectives. We examined critical budget and priority criteria for state health agencies to identify likely decision-making factors, pressures, and opportunities in times of austerity.
Methods. We have presented findings from a 2-stage, mixed-methods study with state public health leaders regarding public health budget- and priority-setting processes. In stage 1, we conducted hour-long interviews in 2011 with 45 health agency executive and division or bureau leaders from 6 states. Stage 2 was an online survey of 207 executive and division or bureau leaders from all state health agencies (66% response rate).
Results. Respondents identified 5 key criteria: whether a program was viewed as “mission critical,” the seriousness of the consequences of not funding the program, financing considerations, external directives and mandates, and the magnitude of the problem the program addressed.
Conclusions. We have presented empirical findings on criteria used in state health agency budgetary decision-making. These criteria suggested a focus and interest on core public health and the largest public health problems with the most serious ramifications.
The governmental public health enterprise continues to face myriad financial and other challenges, including eroding infrastructure, lack of political support, and increasing health problems associated with behavioral health. Since the 2008 economic downturn, thousands of public health jobs have been eliminated, growth has been stifled, and the public health workforce has continued to shrink because of attrition and retirement.1,2 During times of scarcity, the means of allocating resources is of particular interest and importance. However, the characterization and study of resource allocation decision-making is more common in health care compared with public health, where knowledge is limited, especially among national health care systems in developed nations.3–8 Globally, there is a growing interest in the systematic setting of priorities in health care and public health in developing countries, where funds are in shorter supply.4,9–18 A much greater proportion of total health dollars in the United States are spent on health care compared with public health, which is about 3% of total health spending by some estimates.19 This emphasis on spending for health care has created a dearth in research on setting of priorities and budgets in public health; we are not aware of any studies that have examined criteria use in public health priority setting at state health agencies (SHAs), although a few have examined priority setting in local health departments (LHDs). Two studies in particular indicated that the most important priority-setting criteria employed in LHDs were funding availability, mandates, being the sole provider, the size and scope of consequences, politics, and public interest or acceptability.20,21 In 2011, the Association of State and Territorial Health Officials (ASTHO) released their Profile of State Public Health, Volume 2, providing the first collection of revenue and expenditure data that allowed for meaningful comparisons of public health spending across SHAs. These were the first data available in recent years regarding actual spending by SHAs, but these data sets did not capture processes: how SHAs set budgets and why they give priority to the areas they do. We focused on 1 particular component of the priority-setting process—criteria use—because of the critical role criteria were found to play in setting budgets and priorities more broadly in the course of this study, and as reported elsewhere.22
METHODS
Our methods used in this project were described extensively elsewhere.22 We used an exploratory mixed-methods process, in which findings from semistructured interviews informed the creation of a survey instrument, which, in turn, led to an integrated analyses of the 2 stages.23 Our study22 was guided by the research question: what are the factors considered and tradeoffs made in budget and priority setting in state health agencies?
The specific aims of this project included:
Explore and describe state public health agency budget- and priority-setting processes at the executive level and within preparedness, environmental health sciences, and maternal or child health (MCH) divisions, including how political, economic, legal, and other factors affect the process;
Understand how and the degree to which decision-makers’ discretionary budget authority affects the budget-setting process; and
Compare and contrast public health agency budget-setting and programmatic-spending processes between executive and division director levels.
For stage 1, we conducted semi-structured interviews in spring 2011 with 45 practitioners across 6 SHAs, which were selected to assure variation with regard to geography, agency structure (i.e., standalone public health agency or superagency), and governance type (i.e., centralized, mixed, shared, and decentralized). Respondents represented executive leadership (chief executive officers, chief financial officers, senior deputies) and division or bureau leadership (environmental health, MCH, and preparedness directors). Legislative liaisons were also represented. We decided to include both executive leadership and division directors to better understand the relative importance of criteria by position in the organization’s hierarchy. The specific divisions were selected because of (1) high-frequency presence across agencies, and (2) differences in types of services provided, (e.g., substantial direct services [MCH]) versus mainly population-based services (preparedness and environmental health). Interviews were transcribed and verified, and then independently coded thematically by 2 researchers. Data were managed and analyzed with NViVo 9 (QSR International, Cambridge, MA).
For stage 2, we conducted a national survey of practitioners in fall 2011 in all 50 SHAs and District of Columbia. The same positions were targeted for the survey stage as the interview stage: chief executives, chief financial officers, senior deputies, legislative liaisons, and directors of environmental health, preparedness, and MCH. Survey questions were adapted from Baum et al.20 and from Platanova et al.21 Additional criteria were generated from the stage 1 interviews and compared against priority-setting lists generated in Platanova et al.21 and Baum et al.,20 respectively, and were refined throughout pretesting.
We piloted both the stage 1 interview instrument and pretested the stage 2 survey with 9 former state public health leaders. During pilot interviewing, questions were tested for relevance and accessibility. In pretesting, criteria were examined for conceptual distinctiveness. Nineteen criteria (and 1 “other” option) constituted the final list for the survey.
Three hundred fifty-five potential respondents were contacted based on rosters from ASTHO (including ASTHO peer networks for senior deputies, chief financial officers, legislative liaisons, environmental health directors, and preparedness directors) and the Association of Maternal Child Health Programs, which collectively represented practitioners from the targeted positions. We used introductory screening survey questions to determine eligibility—whether they served in a targeted position, whether their responsibilities included setting budgets and priorities, and whether they had gone through the budget-setting process. Descriptive statistics were generated, and bivariate comparisons were conducted between executives and division directors using either the Pearson χ2 or Fisher exact test, as appropriate. This study was done as a collaboration between Johns Hopkins investigators and ASTHO; ASTHO staff assisted with interview and survey instrument creation, and ASTHO partially funded this work.
RESULTS
Forty-five interviews were conducted in stage 1. Three potential respondents declined participation, and 2 respondents from the chief financial officer member list were not interviewed because they were not involved in the budget decision-making process. Twenty-three interview respondents were women (51%). Interview respondents had served in their current position for a mean of 4.2 years (median 3 years).
In the survey stage, 16 individuals were disqualified based on the previously described eligibility criteria, and 27 were excluded because they were no longer in the targeted position, resulting in a final potential respondent pool of 312. We received survey responses from 207 individuals (response rate of 66%) representing 48 states and the District of Columbia. Demographic characteristics for survey respondents are reported in Table 1. Forty-nine percent of survey respondents were women, 53% reported having a master’s degree, and 21% had a professional degree (MD, JD) as their highest level of educational attainment. A master’s degree was the most common level of education reported by both executives (45%) and division directors (59%); however, executives more frequently reported a professional degree (30% vs 15% for division directors). Survey respondents reported serving a median of 3.5 years in their current position. Executive survey respondents reported a mean agency-wide budget of $566.4 million (median $280 million) compared with division directors, who reported a mean division budget of $77.2 million (median $22 million). Executives reported having an average of 1055 staff agency employees working under them (median 426) and division directors reported an average division size of 104 staff employees (median 50).
TABLE 1—
Demographic Characteristics of Respondents for Interview and Survey Stages: Budget- and Priority-Setting Criteria at State Health Agencies, United States, 2011
| Interview Stage Total |
Survey Stage Total |
|||||
| Characteristics | Division Director | Executive | Total | Division Director | Executive | Total |
| No. of respondents | 18 | 24 | 45 | 111 | 86 | 207 |
| Gender | ||||||
| Female | 11 | 11 | 23 | 53% | 41% | 48% |
| Male | 7 | 13 | 22 | 38% | 48% | 42% |
| No response | 9% | 10% | 10% | |||
| Experience, y | ||||||
| Mean time in position | 3.6 | 4.6 | 4.2 | 4.9 | 4.7 | 4.8 |
| Median time in position | 3.0 | 3.5 | 3.0 | 4.0 | 3.0 | 3.5 |
Note. Executive and Division Director columns may not add to total as other nonexecutive or division director staffers (i.e., legislative liaisons) were included in the total number of respondents.
Interview Data
In the stage 1 interviews, identification of priority-setting criteria occurred in 2 ways. First, criteria were identified when spontaneously mentioned in response to any of the interview questions (for instance, criteria that were mentioned when answering general questions about the priority-setting process). Second, respondents were asked directly, through an open-ended question, what criteria they used while setting budgets and priorities. Interview respondents identified more than 30 distinct criteria used in setting budgets and priorities. Responses were grouped thematically and are presented in Table 2.
TABLE 2—
Priority-Setting Criteria From Interview Data: Budget- and Priority-Setting Criteria at State Health Agencies, United States, 2011
| Criterion | No. Selecting Criterion as Priority |
| Top-tier criteria | |
| Political interests | 23 |
| Magnitude of problem | 17 |
| Is a mandatory match or mandated service | 17 |
| Mission critical | 16 |
| Seriousness of consequence | 16 |
| Delivery by others | 14 |
| Meets federal priorities/guidance | 12 |
| Previous allocation and results | 12 |
| Availability of funds | 11 |
| Prevention and protection | 11 |
| Impact on locals and partners | 10 |
| Second-tier criteria | |
| Unsustainable/crippling cuts | 8 |
| Impact on personnel | 8 |
| Maximize/leverage dollars for other programs (e.g., matching funds) | 8 |
| Emergent issues | 7 |
| Affects a targeted group | 7 |
| Aligned with strategic plan | 6 |
| Affects technical expertise/capacity | 6 |
| Cost-effectiveness | 6 |
| Means of correcting | 5 |
| Strength of evidence | 4 |
| Community interests | 3 |
| Immediate benefit | 3 |
| Equity promoting | 2 |
| Population based | 2 |
| New or expanding program versus maintaining effort | 2 |
| Special interests | 1 |
In addition, top criteria were ascertained through interview questions regarding the differentiation of top priorities from all agency or division priorities; that is, respondents were asked which criteria were the most important in determining what would be a top agency priority. Respondents reported that an agency’s programmatic or strategic top priorities usually had some sort of special term associated with them, for example “building blocks,” “exceptional items,” or “tier 1 items.” Table 2 lists the “second-tier” criteria; these criteria were not reported as a top priority criterion, but were mentioned by respondents. The number of participants who discussed a particular criterion is reported in parenthesis.
Across position type and state, 5 items were identified frequently as important criteria, as well as considerations that ultimately drove decision-making (Table 3); that is, they were consistently noted as the most important: how political interests and pressure bore on the issue, how many people were affected by the disease and program, whether the program or service was mandated in law or was part of a mandatory match (e.g., Medicaid match or a required match on a federal grant from the Centers for Disease Control and Prevention), whether a service was viewed as mission critical, and how serious were the consequences of the problem a program or service was meant to address. Interview respondents indicated that these criteria were used for the tough decisions on what to cut and what to preserve. Explanatory quotes for each of these criteria are presented in Table 3.
TABLE 3—
Illustrative Quotes of Top Five Priority-Setting Criteria, From Interview Data: Budget- and Priority-Setting Criteria at State Health Agencies, United States, 2011
| Top Criteria Employed During Budget Cuts | Illustrative Quote |
| Political interests | “Are we funding a program simply because it’s always been funded and it’ll always get packed in by legislature? So why are we hitting our heads against the wall? Is it a program that’s politically popular, but does it really provide the results that we think that another program that’s not as popular would produce, or is it just the program that we’ve been told not to eliminate, because we’ve been told not to eliminate it? Or is it a program that gets defunded because it’s not popular by a certain group that’s in power?” Chief Financial Officer |
| Magnitude of the problem | “We will look at what happens if we don’t do something for a year or two, is that going to be a huge problem or can we stop something and pick it back up without losing a lot of traction and not having a lot of negative Public Health impacts from that. And we’re also going to look at—this is a little bit back in the population base—what percentage of the population is at risk from the program or activities that we’re talking about.” Senior Deputy |
| Mandated match or service | “We had to go through and look at the responsibilities that are outlined in statute, align those back to our program areas and then make recommendations in accordance with the statute for discontinuation of activities.” Legislative Liaison |
| Mission critical | “We've gotten to the point where we can't do everything for everybody. The message [the legislature] sent was … pick the programs, get back to your true mission and we're going to fund those and, hopefully, other groups will come out of the woodwork … as a need develops that is not necessarily mission critical.” Chief Financial Officer |
| Seriousness of the consequences | “If you cut this program are you going to die next week? If you cut this program are you going to die in a year? If you cut this program are you going to die in five or ten years? … I had made that priority based on the optimism that some things would come back over time, that the economy cycles and we would have better times.” Senior Deputy |
Political Influence as Mutable Criterion or Immutable Constraint
Two distinct interpretations emerged from the stage 1 interviews in terms of respondents’ perspectives on priority-setting considerations. Specifically, respondents were likely to either (1) weigh competing criteria against each other, or (2) view some criteria as immutable constraints that had to be managed during the budget-setting process. Under the former view, even the most important criterion was considered in relation to others. For example, where political interests were among the most important criteria, they were weighed against other important considerations, such as cost-effectiveness or how many individuals would be affected by a program.
Conversely, other respondents described a few criteria, typically political influence or pressure, mandatory match, and availability of financial resources, as essentially a constraint within which they had to operate. In their view, these criteria were more absolute in the priority-setting deliberations. Respondents could not proceed with priority setting if political interests were not satisfied. In some cases, respondents attempted to reconcile the conflict between political reality and public health considerations by artificially separating the decision spaces. For instance, 1 respondent discussed attempting to move beyond this political constraint by setting politics aside during decision-making so he could focus more on the issue from a public health perspective:
I know that I’m going to have to make the call out to the stakeholders and say, just want you to hear from me before you see it in the newspaper but when the governor’s budget comes out, it’s likely to include this particular reduction. And so I know that there’s going to be political pressure out there but I really try to separate my own decisions from that.—Senior Deputy
Another respondent mentioned attempting to set the constraint of limited resources aside when trying to identify top priorities. However, in general, constraints were seen as non-negotiable. As illustrated in the following quote, respondents often expressed concern that public health considerations took a back seat to political reality:
[My state] just elected a very conservative senator, and he just wants to eliminate all of these programs and to stop doing things because his concern is—I mean he has got a point—but his concern is the Federal deficit, period… . Here it is just not possible to move against that… . We can talk internally. We can make discussions and proposals, but they have to go to the Governor’s office. The Governor’s office looks at them, they sort them out, they make their decisions which are heavily politically influenced and then they tell us what we can or cannot support. It is as simple as that, what bills, what programs we can or cannot support or put forward to our Legislature. That is it. You don’t—I mean if you want your job—I guess you don’t go beyond that. So it is very much politically controlled here.—Senior Deputy
Results From the National Survey
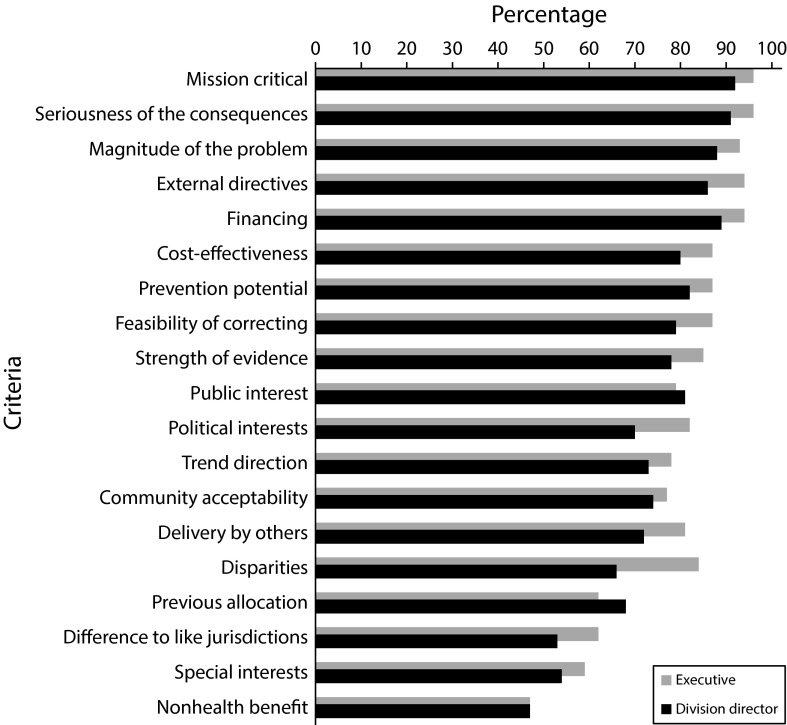
To quantify the relative importance of these criteria, the 19 most frequently mentioned criteria (plus an “other” option) were rated by survey respondents on a 4-point Likert scale for how important a given criterion was to setting health priorities in the respondent’s area of responsibility. The responses options included not important, somewhat important, moderately important, and extremely important. Figure 1 reports results based on position type. Executives included chief executive officers, chief financial officers, and senior deputies (range = 81–83); division heads included environmental health, MCH, and preparedness directors (range = 106–108).
FIGURE 1—
Percentage of survey respondents rating criteria as moderately or extremely important in priority setting, by level: Budget- and Priority-Setting Criteria at State Health Agencies, United States, 2011.
Respondents rated 16 criteria as moderately important or higher on average. Either moderately or extremely important were cited most frequently on whether the program was essential or mission critical (94%), the seriousness of the consequences of the problem a program or service was meant to address (93%), external directives or mandates (90%), availability of funds (90%), and how many people were affected (91%). A more detailed description of these criteria is available as a supplement to the online version of this article at http://www.ajph.org.
Several statistically significant differences arose when executive responses were compared with division directors. Overall, executives tended to rate the criteria as more important compared with division directors. Specifically, 82% of executives said that whether a program or service was mission critical was extremely important for priority setting compared with 63% of division directors (P = .005; data not shown). Seriousness of the consequences was rated extremely important by 73% of executives and 59% of division directors (P = .041; data not shown). The criterion, delivery by others, was rated as extremely important by 44% of executives compared with 26% of division directors (P = .008; data not shown).
Disparities
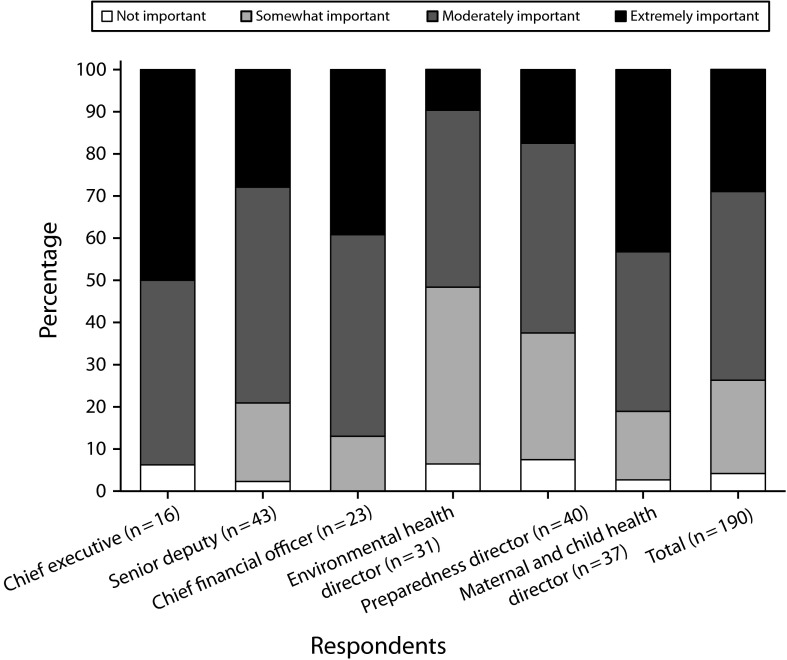
Disparities were rated as moderately or extremely important by 84% of executives compared with 66% of division directors (P = .004). Figure 2 presents the distribution of responses to this particular criterion by position. Environmental health directors and preparedness directors responded differently compared with MCH directors and executive positions—52% of environmental health directors and 63% of preparedness directors rated the disparities criterion as moderately or extremely important (compared with 81% of MCH directors).
FIGURE 2—
Survey respondents’ rating of the relative importance of the disparities criterion to priority setting in their area of responsibility: Budget- and Priority-Setting Criteria at State Health Agencies, United States, 2011.
As part of our analysis of the interview data, we examined the notion of how division directors saw their role as different from their peers (i.e., MCH vs environmental health vs preparedness directors); these data potentially had effects on the differences observed in the survey data with respect to the importance of disparities criteria. The 26 division director stage 1 interview respondents were asked how they thought the means of serving their constituency differed from the other division directors. For example, a director of environmental health was asked: “Is there anything unique about the types of people you serve or the way that you serve them that means you think about priority setting differently than you would if you were in charge of maternal child health or emergency preparedness?”
Thirteen said they felt the considerations were different, 7 said they were not, and 6 said they were not sure. Among those who felt there was a difference, the key distinctions were (1) prevalence of direct or clinical services offered by MCH compared with population-oriented services offered by preparedness and environmental health; and (2) a perception that MCH focused on the most vulnerable subgroups, whereas preparedness and environmental health focused on the population more broadly, which included vulnerable subgroups, as illustrated by the following 2 quotes:
I think we, when you talk about preparedness and the people we serve, a) we serve everyone and what we’ve been trying to do because preparedness, emergency preparedness is really, really new compared to classic public health programs and how you serve the people. With even WIC the population is fairly well-defined. Chronic diseases you’re looking at a different population. Children with special health care needs, you’re looking at a different population. And we are trying to tailor preparedness to fit everyone and fit everyone whether they have special needs, doesn’t matter what age they are, or what their financial situation is. How do we protect their health and safety for any sort of emergency event?—Preparedness Director
I think the people we serve really are the most vulnerable. They often are people that have fewer resources, may be isolated, may lack transportation, really tend to be the most vulnerable and so we try to recognize that, with the methods that we use for service delivery as well as with the message that we use to provide information where—public health is definitely population based as is environmental health and I imagine preparedness, but we tend to serve people who may be the last to hear about it as opposed to the first.—MCH Director
Criteria and the Use of Decision-Support Tools
Decision support tools can help to formalize resource allocation decision-making through a set of weighted criteria and processes for considering and valuing pertinent information.24–32 Both stage 1 interview and stage 2 survey respondents reported infrequent use of decision support tools. In the interviews, 1 of the 6 SHAs reported systematic use of a priority-setting framework to aid in their decision-making. Respondents from this agency reported favorable impressions of the tool and described its use to provide additional perspectives, rather than treating it as deterministic (i.e., the rank-order list may or may not be followed precisely). Respondents from 2 state agencies did not report any use of tools, and in 3 agencies, some individual respondents reported using tools, whereas others reported no tool use. Beyond the respondents from 1 SHA that systematically used tools, 9 individual respondents from the other SHAs reported they used some sort of tool or list of criteria (e.g., return on investment; strengths, weaknesses, opportunities, and threats [SWOT] analysis; priority-setting during strategic planning), and 1 said they used a formal tool, but did not specify which type.
Stage 2 survey respondents were asked how often they used decision or prioritization tools during resource allocation in the past year (corresponding to fiscal year 2011), and results also suggested relatively low tool use. Only 29% of all respondents indicated use of tools quite or very often, whereas 42% said they rarely or never used tools during the past year. Executives (86%) were more likely to indicate any level of tool use than division directors (74%; P = .049). Sixty-six percent of environmental health directors and 65% of preparedness directors indicated any tool use during resource allocation in the past year. Ninety percent of MCH directors indicated any tool use. Among executives, senior deputies (91%), chief financial officers (75%), and chief executive officers (87.5%) indicated any tool use in the past year.
DISCUSSION
The notion that state public health leaders utilize criteria during budget setting is neither controversial nor novel. However, the nature of these criteria, competing considerations, and the way in which the criteria are employed have received relatively little attention. The study of these phenomena enhanced our understanding of budget- and priority-setting processes, which are of particular relevance and importance in the face of continued financial challenges. This was the first study, to our knowledge, that attempted to ascertain which criteria were used and by whom, at the SHA level and across several key divisions within SHAs. Although there was broad agreement on the relative importance of key criteria, there was no complete agreement among practitioners as to the top and competing considerations, which was not surprising, given differing economic, political, historical, and organizational contexts of states and perhaps differing priorities of individual practitioners. However, there was some consensus across practitioners from various SHAs and positions that certain criteria did matter most. These top criteria included: political interests, magnitude of the problem, as a mandatory match or mandated service (condensed to “external directives” in the survey), mission critical, and seriousness of consequences.
The top criteria from the survey responses included mission critical, seriousness of the consequences, magnitude of the problem, external directives, and financing. The top criteria largely overlapped between the interview and survey stages, with some difference in ordering, with the exception of political interests. This difference appears to be partially the result of (1) an importance versus frequency distinction (i.e., as outlined in results, many practitioners identified political considerations as an important criteria, but relatively few identified it as the most important criterion), and (2) a difference in importance rating between division directors versus executives. That the relative importance of these criteria was largely stable across position type and interview versus survey stages was noteworthy, given the difference in data collection methods (i.e., open-ended questions in the interviews vs closed questions in the survey).
Practitioners must weigh key public health priorities against external mandates, political interests, and more philosophical questions of whether the program is truly core or mission critical to their agency, all while struggling with their generally shrinking financial base. This study highlighted the criteria used in setting priorities in the context of national and statewide budget cuts. In this context, there were also additional constraints, namely, political considerations, which might exist even outside times of fiscal austerity. This is an important point worthy of further research. However, beyond political considerations, several key criteria might be common across states and position types.
Respondents viewed the relative importance of several criteria quite similarly across position types; however, there were a few exceptions, one of which was disparities. Environmental health and preparedness directors rated the relative importance considerably lower than the other respondents. This might be explained in part by a perception that these divisions focus on an entire population, rather than subgroups. However, this assumption and the drivers of underlying differences of opinion on this point ought to be explored further, particularly because vulnerable groups are notoriously hardest hit by emergencies and disasters, as well as environmental hazards.
Study findings also highlighted a key difference in responses between the role of the chief executive and division directors. This shed light on differences in positions, roles, and responsibilities, and offered insight into training needs and tools that could be developed for and targeted to specific positions. The chief executive must engage in highly complex negotiations, taking the entire health system into account. Although some might consider the scientific realm of public health to be more pure or valid, the political aspects of public health are critical. Without effective public health leader engagement in the political arena, there would be insufficient public health funding. Public health decisions have real political consequences as well—elimination of a minor program favored by a powerful appropriator might result in a loss of support for more critical funding areas or authorities. For chief executives, the seriousness of the consequences had both health-related and political dimensions. The findings also illuminated an important paradox for health officials. Although division directors could focus their attention and resources to specific programs, chief executives had to attend to the more general aspects of overall organizational capacity or infrastructure (what the Institute of Medicine report calls “foundational capabilities”), such as communications, partnership development, research, and information technology. The paradox was that this organizational infrastructure was critical to fund, but was typically a nonstarter in the political realm.
The study of criteria use in domestic public health resource allocation was limited. Some research was done on priority setting with regard to health systems outside of the United States. However, these findings did not translate well to the US system, given our tendency to parse out the individual from population issues and (for the most part) direct different sectors or government entities to address these issues. Public health, however, is responsible for both population health and providing safety net care, despite the Institute of Medicine's consistent recommendations that public health divest itself from the provision of individual clinical care.19,33,34 Because of this dual role, and dwindling resources, practitioners have been forced to make very difficult decisions as to the correct course of action to protect the public’s health. Further understanding of the criteria used for these decisions, particularly in times of scarcity, is critical to prepare for.
Limitations
Our project had several limitations. First, it was cross sectional in nature. Although interviews allowed us to ask respondents how they believed their use of criteria changed over time, we were not able to do so in the survey. Accordingly, we represented the relative importance of criteria only as a snapshot in time. Additionally, social desirability bias might have emerged because both the interview and survey data relied on self-report. There were no constraints on how many criteria could be rated of particular importance (e.g., “extremely important”); that is, respondents were not forced to rank-order criteria, so relative importance within rated importance categories was not known. However, because our aim was to explore practitioners’ experience while setting priorities, we believed the unconstrained, self-reported nature of the questions were appropriate, but we acknowledged that validity from self-report might be in question. We attempted to address concerns regarding credibility and dependability through extensive instrument pretesting with former health officials (9 pilot interviews for interview instrument, 9 cognitive interviews for survey instrument), and through member checking. Furthermore, because several dozen potential survey respondents had left their positions (and did not complete the survey), the potential impact of these types of individuals on survey results were not known. Studying these issues in those who have recently left public health practice might be warranted. Finally, our project was subject to certain limitations with respect to transferability and generalizability. With respect to the former, our interviews of 6 state health departments (of 51 total) represented approximately 12% of the population of interest. However, because of variation in political and legal contexts, and historical considerations, we used a complementary national survey to better quantify the differences we observed in interview data. A 66% response rate (207 individuals representing 48 states and District of Columbia) was robust, although, as discussed previously, nonresponse bias might be an issue.
Conclusions
We examined attitudes and preferences regarding criteria used in setting state public health priorities and budgets. One of the main findings was that respondents reported holding several key, sometimes competing, criteria in tension—those related to compliance (meeting external mandates or political directives) and public health need. Further study is needed to better understand the relative weight or importance of these criteria during priority setting, because the majority of survey respondents indicated all criteria were moderately or extremely important to the process. More research is needed into understanding how the criteria are implemented, as well as the impact of priority-setting preferences on policy decision-making. Our project also characterized what respondents took to be a recent push, motivated by the economic and political landscape, to pare down public health, to reduce the scope of programs and services, such that SHAs focused on what was truly core to their mission. In some cases, public health might continue to provide a service, particularly if no other entity can do so as efficiently or effectively. In other cases, others might provide the service with public health, assuring the quality through oversight, licensing, or regulation. Hard times bring challenges, but also may bring opportunities. Our study and subsequent work would allow us to further understand resource allocation processes and increase use of and refine training and tools to support enhanced decision-making. As we transition to the future with health care reform and increased focus on population health, our study (and subsequent tools and additional research) will enhance our collective ability to make resource allocation decisions and, ultimately, better allocate scare resources.
Acknowledgments
This study was funded by Robert Wood Johnson Foundation, Association of State and Territorial Health Officials, and Johns Hopkins Preparedness and Emergency Response Research Center.
We would like to thank Joseph Berger for his research assistance, and Kate Smith and Thomas Burke for helpful suggestions that improved the quality of the research and article, and the Association of Maternal and Child Health Programs for member involvement and organizational support.
Human Participant Protection
Both stages of this project were approved by the Johns Hopkins School of Public Health institutional review board.
References
- 1.Association of State and Territorial Health Officials. Crystal City, VA: Association of State and Territorial Health Officials; 2012. Budget cuts continue to affect the health of Americans: Update March 2012. [Google Scholar]
- 2.National Association of County and City Health Officials. The District of Columbia: National Association of County and City Health Officials; 2012. Local health department job losses and program cuts: findings from the January 2012 survey. [Google Scholar]
- 3.Daniels N, Sabin JE. Accountability for reasonableness: an update. BMJ. 2008;337 doi: 10.1136/bmj.a1850. a1850. [DOI] [PubMed] [Google Scholar]
- 4.Daniels N, Sabin JE. Setting Limits Fairly: Can We Learn to Share Medical Resources? 2nd ed. New York, NY: Oxford University Press; 2008. [Google Scholar]
- 5.McCabe C, Claxton K, Tsuchiya A. Orphan drugs and the NHS: should we value rarity? BMJ. 2005;331(7523):1016–1019. doi: 10.1136/bmj.331.7523.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Groves T. Public disagrees with professionals over NHS rationing. BMJ. 1993;306(6879):673. [PubMed] [Google Scholar]
- 7.Hadorn DC. Setting health care priorities in Oregon. JAMA. 1991;265(17):2218–2225. [PubMed] [Google Scholar]
- 8.Hadorn D. The Oregon priority-setting exercise: cost-effectiveness and the rule of rescue, revisited. Med Decis Making. 1996;16(2):117–119. doi: 10.1177/0272989X9601600203. [DOI] [PubMed] [Google Scholar]
- 9.Youngkong S, Kapiriri L, Baltussen R. Setting priorities for health interventions in developing countries: a review of empirical studies. Trop Med Int Health. 2009;14(8):930–939. doi: 10.1111/j.1365-3156.2009.02311.x. [DOI] [PubMed] [Google Scholar]
- 10.Bryant JH, Khan KS, Hyder AA. Ethics, equity and renewal of WHO’s health-for-all strategy. World Health Forum. 1997;18(2):107–115. [PubMed] [Google Scholar]
- 11.Kapiriri L, Martin DK. Successful priority setting in low and middle income countries: a framework for evaluation. Health Care Anal. 2010;18(2):129–147. doi: 10.1007/s10728-009-0115-2. [DOI] [PubMed] [Google Scholar]
- 12.Rudan I, Kapiriri L, Tomlinson M, Balliet M, Cohen B, Chopra M. Evidence-based priority setting for health care and research: tools to support policy in maternal, neonatal, and child health in Africa. PLoS Med. 2010;7(7):e1000308. doi: 10.1371/journal.pmed.1000308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kapiriri L, Norheim OF, Martin DK. Fairness and accountability for reasonableness. Do the views of priority setting decision makers differ across health systems and levels of decision making? Soc Sci Med. 2009;68(4):766–773. doi: 10.1016/j.socscimed.2008.11.011. [DOI] [PubMed] [Google Scholar]
- 14.Nord E. The trade-off between severity of illness and treatment effect in cost-value analysis of health care. Health Policy. 1993;24(3):227–238. doi: 10.1016/0168-8510(93)90042-n. [DOI] [PubMed] [Google Scholar]
- 15.Williams A. The “fair innings argument” deserves a fairer hearing! Comments by Alan Williams on Nord and Johannesson. Health Econ. 2001;10(7):583–585. doi: 10.1002/hec.645. [DOI] [PubMed] [Google Scholar]
- 16.Nord E. Severity of illness and priority setting: worrisome lack of discussion of surprising finding. J Health Econ. 2006;25(1):170–172. doi: 10.1016/j.jhealeco.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 17.Blumberg LJ, Holahan J, Hadley J, Nordahl K. Setting a standard of affordability for health insurance coverage. Health Aff (Millwood) 2007;26(4):w463–473. doi: 10.1377/hlthaff.26.4.w463. [DOI] [PubMed] [Google Scholar]
- 18.Donaldson C. Economics, public health and health care purchasing: reinventing the wheel? Health Policy. 1995;33(2):79–90. doi: 10.1016/0168-8510(95)93670-v. [DOI] [PubMed] [Google Scholar]
- 19.Committee on Public Health Strategies to Improve Health, Institute of Medicine. For the Public’s Health: Investing in a Healthier Future. Washington, DC: National Academy Press; 2012. [PubMed] [Google Scholar]
- 20.Baum NM, DesRoches C, Campbell EG, Goold SD. Resource allocation in public health practice: a national survey of local public health officials. J Public Health Manag Pract. 2011;17(3):265–274. doi: 10.1097/PHH.0b013e318207599c. [DOI] [PubMed] [Google Scholar]
- 21.Platonova EA, Studnicki J, Fisher JW, Bridger C. Local health department priority setting: an exploratory study. J Public Health Manag Pract. 2010;16(2):140–147. doi: 10.1097/PHH.0b013e3181ca2618. [DOI] [PubMed] [Google Scholar]
- 22.Leider JP, Resnick B, Sellers K et al. Setting budgets and priorities at state health agencies. J Public Health Manag Pract. 2013 doi: 10.1097/PHH.0b013e318297369d. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 23.Creswell JW, Clark VLP. Designing and Conducting Mixed Methods Research. Thousand Oaks, CA: Sage Publications, Inc; 2007. [Google Scholar]
- 24.Honoré PA, Fos PJ, Smith T, Riley M, Kramarz K. Decision science: a scientific approach to enhance public health budgeting. J Public Health Manag Pract. 2010;16(2):98–103. doi: 10.1097/PHH.0b013e3181c87ace. [DOI] [PubMed] [Google Scholar]
- 25.Fos PJ, Miller DL, Amy BW, Zuniga MA. Combining the benefits of decision science and financial analysis in public health management: a county-specific budgeting and planning model. J Public Health Manag Pract. 2004;10(5):406–412. doi: 10.1097/00124784-200409000-00006. [DOI] [PubMed] [Google Scholar]
- 26. Sibbald SL. Successful priority setting: a conceptual framework and an evaluation tool. PhD Thesis, University of Toronto, 2009.
- 27.Vilnius D, Dandoy S. A priority rating system for public health programs. Public Health Rep. 1990;105(5):463–470. [PMC free article] [PubMed] [Google Scholar]
- 28.Simoes EJ, Land G, Metzger R, Mokdad A. Prioritization MICA: a web-based application to prioritize public health resources. J Public Health Manag Pract. 2006;12(2):161–169. doi: 10.1097/00124784-200603000-00008. [DOI] [PubMed] [Google Scholar]
- 29.Brownson RC, Baker EA, Leet TL, Gillespie KN. Evidence-Based Public Health. New York, NY: Oxford University Press New York; 2003. [Google Scholar]
- 30.National Association of County and City Health Officials. Washington, DC: National Association of County and City Health Officials; 1991. APEXPH annex: prioritization. [Google Scholar]
- 31.Bower CE. Hartford, CT: Connecticut Department of Public Health; 2009. Guide and template for comprehensive health improvement plan. Version 2.1. [Google Scholar]
- 32.Healthy People 2010. Setting health priorities and establishing objectives. Available at: http://www.phf.org/resourcestools/Documents/HP2010Toolkit2002.pdf. Accessed April 6, 2010.
- 33.Institute of Medicine (US) Committee for the Study of the Future of Public Health. The Future of Public Health. Vol. 88. Washington, DC: National Academies Press; 1988. [PubMed] [Google Scholar]
- 34.Institute of Medicine (US) Committee on Assuring the Health of the Public in the 21st Century. The Future of the Public’s Health in the 21st Century. Washington, DC: National Academy Press; 2003. [Google Scholar]