Abstract
Objectives. We assessed the effectiveness of Circle of Life (COL), an HIV-preventive intervention developed specifically for American Indian and Alaska Native (AI/AN) middle school youths.
Methods. By partnering with a tribal community, we conducted a longitudinal wait-listed group randomized trial with 635 seventh and eighth graders in 13 schools of a Northern Plains tribe. We surveyed participants at baseline, 3 months, and 12 months from 2006 to 2007.
Results. COL was found to increase HIV knowledge in the short term, but had no effect on sexual activity compared with those who did not receive it. However, COL was found to be effective for delaying the onset of sexual activity, with the greatest reduction in risk occurring for those receiving COL at early ages.
Conclusions. Community partnership was key to successful project design, implementation, and analysis. The project confirmed the importance of the timing of interventions in early adolescence. COL may be a key resource for reducing sexual risk among AI/AN youths.
The HIV/AIDS epidemic in American Indian and Alaska Native (AI/AN) persons has received little attention to date. This population, less than 2% of the nation’s total, has yielded relatively small case numbers in national surveillance statistics.1 Yet, more than 25% of AI/AN individuals living with HIV were estimated to be undiagnosed, a level second only to Asians and Pacific Islanders.2 Once diagnosed with AIDS, AI/AN persons have the lowest survival rate at 12, 24, and 36 months compared with all other race groups.1 Moreover, for AI/AN individuals, the epidemic is disproportionately borne by youths, with 23.1% of all HIV diagnoses among this group occurring among those younger than age 25 years.1 Coupled with high levels of sexually transmitted infections (STIs), early age of first sexual activity, and early onset of substance use,3–5 AI/AN youths are vulnerable to HIV. Targeted prevention should begin at early ages.
However, few youth-focused HIV preventive interventions exist for the AI/AN population.6–8 None have been rigorously evaluated. We began discussions with our partners in a Northern Plains (NP) tribe about addressing HIV risk in their community. Our partners requested we focus prevention messages on young adolescents using a culturally meaningful HIV risk reduction intervention. Their requests mirrored research on sexual risk-taking among youths: persons initiating sexual intercourse at young ages are at greater risk of an STI9 and becoming pregnant10; report higher levels of sexual risk-taking11; and respond to culturally appropriate prevention content.12 Here, following standard guidelines for clustered randomized trials,13 we present the results of our effort to rigorously evaluate Circle of Life (COL), a theory-based HIV preventive intervention designed especially for AI/AN adolescents.
METHODS
The project employed community-based participatory research (CBPR) methods,14,15 an approach that has been well established in many community-based research initiatives. Although relatively new to randomized trials, the approach has demonstrated success in improved recruitment, retention, and program sustainability.16
Randomized trials in nonclinical settings within tribal communities are rare. This dearth is likely because of multiple factors, including challenges associated with working in rural and remote areas, small populations compromising statistical power, and general distrust of research in many tribal communities, a legacy of past research abuses.17–19 Through collaboration, we were able to integrate our partner community priorities and requests into project design and analysis in meaningful ways. Community partners requested that the intervention reach all participants, not just an experimental group; we implemented a wait-listed randomized design. The partners urged us to include as many youths as possible, not just those who were available at baseline; we modified our recruitment and analytical strategy to make sure that happened. Because of the sensitive nature of the project, they requested we speak in person with every parent or guardian in the consent process; we delayed intervention implementation by 6 months to make that happen. In short, responding to community priorities required us to alter parameters of the original design and timelines. We found creative and innovative ways to do this while maintaining scientific rigor; this openness and flexibility, in turn, contributed to ongoing community support and participation.
Setting and Design
The tribe we worked with in this project was rural and remote, distant from major population centers. (As a part of our partnership, we agreed not to disclose the community name, instead using the descriptor “Northern Plains tribe.”) Its small communities were scattered across some of the poorest counties in the nation, with striking gaps in income, education, and many health indicators.20,21 Despite the poor socioeconomic conditions and a long history of often brutal federal policies aimed at the destruction and disempowerment of AI/AN communities, the tribe has many strengths, with a long history of activism and strong cultural traditions.22
The project was a school-based group randomized trial (GRT), and we randomized at the school level to minimize contamination across youth attending the same school. We used a longitudinal wait-listed design so that youths at all schools would be exposed to the intervention within 12 months, a condition required by participating schools. Details of the overall project rationale and design are available elsewhere.23 In brief, the design allowed us to address 2 sets of hypotheses. The first set, and the focus here, concerned the overall intervention effect hypothesized to lower sexual risk among youths who received COL compared with those who did not receive it. These results focused on the baseline and 2 additional follow-up surveys—1 at 3 months and another at 12 months after the baseline. The other set of hypotheses concerned the differential effectiveness of COL across subgroups, utilizing data from 2 preintervention waves and 3 postintervention waves, to be described elsewhere.
Participants
We invited all middle schools of the NP tribe teaching seventh or eighth grade classes to participate in the project. All schools (n = 13) agreed to participate, and no school withdrew at any point during the project. Schools widely varied in size, with enrollments ranging from 9 to 228 middle school students, and in structure, including 4 public, 2 private, and 7 federally operated or contracted schools. These schools were evenly divided across the study arms, although the control arm had 1 more federally operated school than did the COL arm. Distances between the schools were often great, up to 2 hours driving time.
To be eligible for the study, youths had to be attending seventh or eighth grade in fall 2006 at a participating school, have a parent or guardian actively consent to their participation, and provide their own written assent. We did not exclude youths on the basis of race or ethnicity, although virtually all youth attending these schools were American Indian.
Typically, randomized designs are based on participants with baseline data. However, youths in these communities often have difficulty attending school regularly, and our partners requested that we not exclude youths if they were not available for every survey. We agreed to include participants who completed at least 1 survey across the 3 waves, regardless of participation in the baseline survey.24–26 All surveys were collected in paper-and-pencil format at the schools and took about 40 minutes to complete. Youths were paid $10 or the equivalent in gifts for each survey. All survey data were double entered to minimize data entry error.
Intervention
COL is an HIV- and STI-prevention intervention developed specifically for middle-school AI/AN youths. The 30-hour, theory-based curriculum was developed by ORBIS Associates in Washington, DC, an AI/AN-owned and operated not-for-profit educational organization. The curriculum underwent extensive review from AI/AN communities and organizations, representing a vast array of parental, educational, and health expert perspectives. At its core, the curriculum was based on the learning approaches of AI/AN people while integrating theories of behavior change, including social cognitive theory and theory of planned behavior.27,28 Specifically, the curriculum used the Medicine Wheel, a traditional symbol and an embodiment of AI/AN epistemological approaches29 (data available as a supplement to the online version of this article at http://www.ajph.org). The Wheel is divided into 4 equal parts, representing the physical, spiritual, mental, and emotional aspects of life. Each part touches the other and represents balance and harmony. In the curriculum, volition appears in the center, representing one’s ability to make choices and affect the 4 parts of the Wheel. The curriculum is not abstinence-only, but presents safer sex material in age-appropriate ways with flexibility for parent or school modification.
Qualified community members were hired and trained to teach the course. Quality of implementation was reviewed by a supervisor at weekly meetings. Although specific schedules required flexibility in COL implementation, the curriculum was completed in all first-round intervention schools within 3 months, in fall 2006. Wait-listed schools were provided the instruction in fall 2007, in a similar manner. Data collection points were fall 2006, winter 2007, and fall 2007 (before the implementation of COL in the wait-listed schools).
Comparison schools proceeded with instruction as usual. As a part of our agreement with the schools, we did not require that specific alternative instructional materials be used. Approximately one-third of the students in these schools received a health class.
Objectives and Outcomes
The project assessed the impact of the curriculum on HIV/STI knowledge and sexual risk behaviors of middle-school AI youths. We hypothesized that those youths who received COL would know more about HIV/STI risk and would be less likely to report ever having had sex and having had sex in the last 12 months compared with those who had not yet received COL (youth in wait-listed schools).
We also expected that those receiving COL would be significantly more likely to delay onset of sexual activity compared with those who did not receive the curriculum. For those who had had sex, we hypothesized that they would be more likely to have used a condom at last occurrence of sex compared with those who did not have COL instruction. For all outcomes, we expected variation by gender and by age. However, we had no a priori suppositions about direction or magnitude of effects of COL across these groups.
Sample Size and Power
Many tribal communities are small and consequently have a finite number of units—and participants—available for sampling. Thus, our approach to sampling for this project was comprehensive. Based on previous research, we anticipated about an 85% retention rate of the estimated 735 seventh and eighth graders for the 12-month comparison period, yielding a final estimated sample of about 600. Using data from earlier work with the same schools, we calculated intraclass correlations for sexual behavior outcomes and for sexual risk knowledge across schools. We used Optimal Design Software30 to calculate that with 13 schools at the cluster level, α at 0.05, and an average behavioral intraclass correlation = 0.016, we would have 80% power to find a minimal detectible effect size (MDES) of 0.33 for behavioral outcomes, and for knowledge (average intraclass correlation = 0.084), an MDES of 0.55.31 Given these results, our findings were conservative. That is, with the finite sample available in this community, we might not have been able to detect effects when they were present. However, for any effects found to be significant, we could be confident in those results.
We used a computerized random number generator to assign 6 schools to receive COL in fall 2006 and the remaining 7 to receive COL in fall 2007. Most participants (n = 541) were enrolled before randomization. However, because we committed to be inclusive of eligible youth who missed a baseline survey, some youths were recruited after arm assignment. Given the long distances between schools on the reservation, it was unlikely that a youth’s enrollment at any given school was related to the randomization status of the school. Among those parents contacted, 98% gave consent for their child’s participation in the research.
Statistical Methods
Data management and analyses were conducted using SPSS, Stata, and Mplus.32–34 Baseline demographic characteristics equivalence between the COL and the comparison groups was assessed using the χ2 test for categorical variables and 1-way analysis of variance for continuous variables. Because of missing data at any given wave, we tested for differences in project participation between groups at each wave and for youths completing different numbers of surveys. We imputed data using the multiple imputation procedures in Stata, which uses an iterative chained equations procedure.35 We tested adjusted proportions and means at baseline using both nonimputed and imputed data, adjusted for clustering. We ran simple regression models within Stata’s multiple imputation estimating procedures to test for parameter differences across groups.
To test effectiveness, we used multilevel mixed-effects linear and generalized linear regression models to control for baseline characteristics, individual autocorrelation across time, and clustering in schools.36,37 We used logit link function for dichotomous outcomes (xtmelogit) and linear regression (xtmixed) for continuous outcomes; both types of models were estimated for multiple imputed data (mi estimate).38 For the mixed effects regression models, we also tested each outcome for gender and age effects separately. To test the effects of COL on age at first sexual activity, we used Mplus to estimate discrete-time survival analysis (DTSA) models.39 We categorized youths by the age at which they received COL and explored differential effects by age (in years) at time of intervention. Wide age-for-grade variation for seventh and eighth graders existed. Age at intervention ranged from 11.9 to 17.3 years, with 94% of the COL group receiving the intervention between the ages of 12 and 14 years. Thus, we were able to compare age-related risk of initiation of sexual activity across 4 groups: students who received the COL intervention when they were 12 years old (n = 86), 13 years old (n = 155), 14 years and older (n = 73), and those in the comparison group (n = 321). We also tested effects separately for girls and boys. In all DTSA analyses, we used a “sandwich-estimator” (type = complex) in Mplus, version 7) to adjust for clustering at the school level.40 For missing data, we used full information maximum likelihood procedures, which have been shown to provide unbiased and efficient estimates for missing data.41 All analyses were conducted using intention-to-treat principles.
Measures
For the present analyses, we used demographic characteristic measures, HIV/STI risk knowledge measures, and items on reported sexual behavior. All items were reviewed by community members, and modifications were made to the wording of some items to align them with the local vernacular. Demographic measures included gender (0 = male/1 = female) and age (in years).
Knowledge of HIV/STI risk.
Knowledge of HIV/STI risk was assessed using a series of 12 questions based on previous work in the field,42 and adapted slightly through community review. The questions measured the accuracy of students’ knowledge about HIV/STIs. The percentage of these items answered correctly at each wave was a student’s knowledge score. Unanswered questions were counted as wrong.
Sexual behaviors.
Sexual behavior items were derived from national survey items.43,44 Because youths do not always understand the term “sex” in medically accurate ways, we defined anal, oral, and vaginal sex for youths before asking a question about sex. We asked “Have you ever had sex in your lifetime with a boy or a man…?” and then “…with a girl or a woman…?” of all youth, regardless of gender. We combined responses into a variable indicating “ever had sex” (0 = no, 1 = yes). We also asked if they had had sexual activity in the last 12 months, similarly coded. Among those who had reported sexual activity, youths reporting using a condom at last sex were coded 1, otherwise 0. Students who answered they had ever had sex were also asked how old they were the first time they had sex. If an adolescent reported having already engaged in sexual activity at baseline and reported an age of first sexual experience, we used that age report as the age of initiation. If sexual activity was reported at baseline but no age of first experience was reported, we used age at baseline as the best available estimate of age of first sex. If an adolescent reported no history of sexual activity at baseline or if data were missing, we went to the subsequent wave and followed the same process of determining age of first sex. Adolescents who reported no history of sexual activity at any wave of data collection were coded as missing on age of first sex.
To utilize DTSA to model age-related risk of sexual initiation, we recoded age at first sex into a series of dummy variables, each representing whether sexual activity had been initiated at each age for ages 10 to 14 years. For each age, adolescents were coded 0 if they had not yet initiated sex, 1 if they initiated sex at that age, and a missing value flag (9) if they had initiated sex before that age.
RESULTS
In total, 635 youths contributed 1 or more surveys. Of these, 61% (n = 385) participated in all 3 surveys, and 87% participated in 2 or more. We had 541 (85%) participate at baseline, 557 (87%) at wave 2, and 477 (75%) at wave 3 (data available as a supplement to the online version of this article at http://www.ajph.org). No significant differences existed between the COL and comparison groups in the number of participants at each wave (P = .904, P = .112, and P = .345, for baseline, wave 2, and wave 3, respectively), the number who contributed a baseline survey and those who did not (P = .908), or the number of youths who contributed 1, 2, or 3 surveys (P = .754).
Baseline Data
In Table 1, we present results for equivalence tests between COL and comparison groups. We found no statistical differences at baseline in unadjusted, adjusted for clustering, or multiply imputed samples (where relevant). Overall, youths of both groups scored approximately 7 correct of the 12 possible items (58%). About 15% of the sample reported they had been sexually active. Of those sexually active youths, the average age at first sex was just under 13 years of age, with about 78% reporting condom use at last sex.
TABLE 1—
Equivalence of Baseline Characteristics, Adjusted for Clusters and for Multiple Imputed Sample: HIV-Preventive Intervention for American Indian Middle School Youths, Northern Plains Region, 2006–2007
|
P |
|||||
| Characteristics | No. | COL | Control | Adjusted for Cluster | Multiply Imputed Sample and Adjusted for Clustera |
| Female, % | 635 | 48.79 | 45.17 | .21 | … |
| Age, y, mean | 635 | 12.98 | 13.08 | .18 | … |
| HIV/STD knowledge, % | 493 | 6.94 | 7.07 | .767 | .709 |
| Ever had sex, % | 499 | 12.80 | 17.67 | .218 | .244 |
| Age at first sex, y,b mean | 69 | 12.70 | 12.50 | .6 | .942 |
| Had sex in last 12 mo, % | 499 | 7.72 | 10.29 | .429 | .364 |
| Condom at last sex,b % | 73 | 80.65 | 76.19 | .338 | .348 |
Source. Circle of Life (COL), 2006–2009.
Total imputed sample sizes are n = 314 (COL) and n = 321 (control). Percentages and means are based on actual responses.
Number responding to question out of 76 who reported having had sex.
Estimation Results
Table 2 displays results for generalized estimating equation models of knowledge and sexual behaviors controlling for baseline and clustering of schools and using multiply imputed samples. Overall, those who received COL scored significantly higher on knowledge questions than did the comparison group (P = .007) at the 3-month follow-up, but the effect was not sustained at the 12-month follow-up. In the models estimated separately, the same patterns appeared for boys (P = .019), but not for girls, and also for older youths (P = .027) but not for younger youths. For outcomes of ever had sex, sex within the last 12 months, or condom at last sex, no statistical differences emerged between the COL and comparison groups.
TABLE 2—
Linear and Generalized Linear Estimates of Circle of Life Effect on Sexual Behavior at 3- and 12-Month Follow-Up, Overall and by Sex and Age: HIV-Preventive Intervention for American Indian Middle School Youths, Northern Plains Region, 2006–2007
| Wave 2 (3 mo)a |
Wave 3 (12 mo)a |
|||
| b (95% CI) | P | b (95% CI) | P | |
| HIV/STI knowledge | 0.718 (0.200, 1.236) | .007 | 0.083 (−0.115, 0.281) | .409 |
| Girls | 0.538 (−0.193, 1.269) | .149 | 0.340 (−0.453, 1.134) | .399 |
| Boys | 0.876 (0.146, 1.606) | .019 | 0.401 (−0.369, 1.171) | .306 |
| Age 11–12 y | 0.744 (−0.274, 1.763) | .151 | 0.423 (−0.563, 1.410) | .4 |
| Age 13–16 y | 0.692 (0.079, 1.304) | .027 | 0.354 (−0.380, 1.090) | .34 |
| Ever had sex | −0.091 (−0.751, 0.570) | .788 | 0.158 (−0.473, 0.789) | .624 |
| Girls | −0.406 (−1.575, 0.762) | .495 | −0.516 (−1.638, 0.606) | .367 |
| Boys | −0.121 (−0.970, 0.728) | .78 | 0.413 (−0.402, 1.229) | .321 |
| Age 11–12 y | 0.090 (−1.600, 1.782) | .914 | −0.072 (−1.837, 1.694) | .937 |
| Age 13–16 y | −0.110 (−0.839, 0.618) | .766 | 0.119 (−0.589, 0.828) | .74 |
| Had sex in last 12 mo | −0.153 (−1.029, 0.723) | .732 | 0.461 (−0.388, 1.310) | .287 |
| Girls | −0.369 (−1.860, 1.122) | .628 | 0.135 (−1.409, 1.679) | .864 |
| Boys | −0.255 (−1.397, 0.888) | .662 | 0.664 (−0.405, 1.733) | .223 |
| Age 11–12 y | 1.119 (−1.214, 3.452) | .347 | 0.075 (−1.936, 2.086) | .942 |
| Age 13–16 y | −0.407 (−1.388, 0.574) | .416 | 0.543 (−0.413, 1.499) | .265 |
| Condom at last sex | 0.817 (−0.837, 2.471) | .333 | −0.580 (−2.044, 0.883) | .437 |
| Girls | 1.247 (−2.037, 4.530) | .457 | −0.498 (−3.391, 2.394) | .736 |
| Boys | 0.675 (−1.301, 2.652) | .503 | −0.704 (−2.589, 1.181) | .464 |
| Age 11–12 y | 2.931 (−0.981, 6.843) | .142 | 1.386 (−1.975, 4.748) | .419 |
| Age 13–16 y | 0.458 (−1.429, 2.346) | .634 | −1.070 (−2.759, 0.619) | .214 |
Note. CI - confidence interval; STI = sexually transmitted infection.
Source. Circle of Life, 2006–2009.
All estimates based on multiply imputed samples.
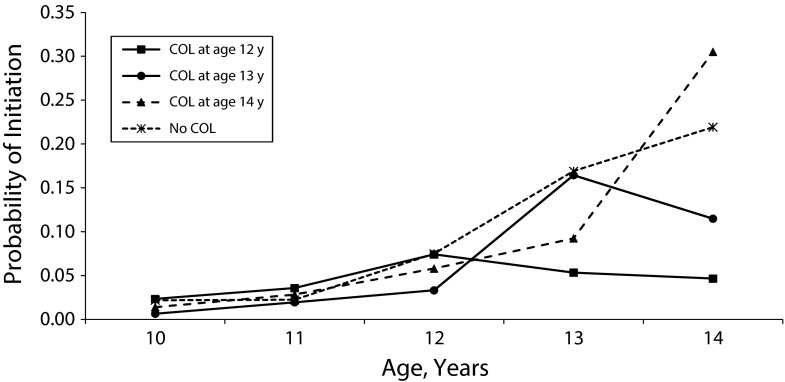
The DTSA analysis of onset of sexual initiation showed significant differences by age at receiving COL (Figure 1). Adolescents who received the intervention when they were 12 years old (solid line) showed a statistically significant pattern of reduced risk of sexual onset compared with those who received the intervention when they were older and those who did not receive it at all. Once the intervention was introduced starting at age 12 years, the hazard curves for initiation of sexual activity began to diverge. We compared a model in which the hazards for initiation of sexual activity at ages 10, 11, and 12 years were constrained equally across COL groups to a model in which these hazards were freely estimated across groups. Using the scaling correction factor to compute a χ2 difference based on log-likelihood values, the fit was not significantly different across models (χ2 [9] = 8.53; P = .48).45 By contrast, a model in which hazards were constrained across groups for sexual initiation at ages 13 and 14 years provided a significantly poorer fit to the data than did the fully unconstrained model (χ2 [12] = 24.31; P = .02) and the model constraining hazards at ages 10, 11, and 12 years (χ2 [3] = 10.77; P = .01). Further analyses using odds ratio comparisons for specific ages confirmed these results (data available as a supplement to the online version of this article at http://www.ajph.org). The risk of initiating sexual activity was comparable across all youths in the study until they were introduced to the COL intervention, at which point risk trajectories diverged, and those exposed to the intervention showed decreased risk of initiation. The degree of divergence—and reduction in risk—was inversely related to age at intervention. Youths who received COL earlier showed the greatest reduction in risk over time.
FIGURE 1—
Hazard estimates for sexual initiation by timing of Circle of Life (COL) intervention, adjusted for school cluster: HIV-Preventive Intervention for American Indian Middle School Youths, Northern Plains Region, 2006–2007
Including gender as a covariate in the DTSA model revealed significantly greater risk of sexual initiation overall among boys compared with girls (gender effect on hazard = 0.53; P < .001). However, further tests45 showed that gender differences in the effectiveness of the intervention were not related to age at which the intervention was delivered.
DISCUSSION
Using generalized estimating equations, we found that the intervention had a short-term effect on HIV knowledge. The effect appeared to be most powerful for boys and for older youths, which might indicate that COL could be revised for girls and younger audiences. It might also indicate the need for a booster or ongoing education in this area to sustain increases in knowledge over time, which is often a first step in the path to behavior change.46 We found no effect of COL overall, by gender, or by age on sexual activity or condom use.
If we had stopped with these analyses, we would have concluded that COL was not particularly effective in this population, although low power at the school level would have tempered this conclusion. However, the DTSA approach clearly showed COL to be effective for delaying the onset of sexual activity when it was delivered to young adolescents. Given that delays in sexual initiation might avert deleterious health outcomes,9 an intervention producing results such as those revealed here is most promising. Testing the moderating effect of age on intervention effectiveness will be critical in future research focused on the highly dynamic period of early adolescence.
To our knowledge, this was the first GRT of an HIV-preventive intervention among American Indian youths. We worked closely with tribal partners to build trust and collaboration across the life of the project. The tribe’s requests regarding the conduct of this study brought many challenges, but also indisputably improved our ability to work in the community and to maximize participation and support. They also compelled us to think carefully and creatively about design, implementation, and analysis.
The project was not without limitations. First, the study was conducted with only 1 tribe. We could not presume to generalize to other tribes. However, with the extensive input by many tribal groups and educational experts in its development, COL might hold promise in its applicability in other communities. We encountered constraints in statistical power because of finite numbers of clusters (schools) and youths within them. Calculations indicated that the project was likely underpowered and thus limited our ability to detect effects. To the extent we found significant results, we are confident that COL was effective for those outcomes.
This project overall offered innovation and substantive promise in research on HIV-preventive interventions within cultural context. With the increased attention to community-based approaches to HIV prevention,47–49 COL could be a part of a “toolbox” for AI/AN youth populations. More broadly, the project overwhelmingly showed the importance of using developmentally sensitive analyses that could highlight issues about the timing of interventions and reaching young at-risk populations. Prevention messages might be strongest before the tumultuous years of later adolescence.
Acknowledgments
This work was funded through an award from the National Institute of Mental Health (R01 MH069086; C. E. K., PI) and the Office of Adolescent Health (TP2AH000003; C. E. K., PI).
We would like to thank the schools and the tribal community for their ongoing support; parents, guardians, and youths who gave so generously of their time; and project staff who made it all happen.
Note. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the Department of Health and Human Services or the Office of Adolescent Health.
Human Participant Protection
This project was approved by the tribe and by the Colorado multiple institutional review board. During the project, the community formed a tribal research review board, and this project subsequently was reviewed and approved annually by that entity. The project was also regularly reviewed by a community advisory group and a data safety and monitoring committee.
References
- 1.Centers for Disease Control and Prevention. HIV/AIDS Surveillance Report, 2010; vol. 22. 2012. Available at: http://www.cdc.gov/hiv/surveillance/resources/reports/2010report/pdf/2010_HIV_Surveillance_Report_vol_22.pdf. Accessed April 15, 2012.
- 2.Campsmith ML, Rhodes PH, Hall HI, Green TA. Undiagnosed HIV prevalence among adults and adolescents in the United States at the end of 2006. J Acquir Immune Defic Syndr. 2010;53(5):619–624. doi: 10.1097/QAI.0b013e3181bf1c45. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention, Indian Health Service. Indian Health Surveillance Report–Sexually Transmitted Diseases, 2009. Atlanta, GA: US Department of Health and Human Services; 2012. [Google Scholar]
- 4.Everett-Jones S, Shaughnessy L, Branum C. Youth Risk Behavior Survey of High School Students Attending Bureau Funded Schools. Washington, DC: Bureau of Indian Affairs Office of Indian Education Programs in conjunction with the Centers for Disease Control and Prevention; 2001. [Google Scholar]
- 5.Beauvais F, Jumper-Thurman P, Burnside M. The changing patterns of drug use among American Indian students over the past 30 years. Am Indian Alsk Native Ment Health Res. 2008;15(2):15–24. doi: 10.5820/aian.1502.2008.15. [DOI] [PubMed] [Google Scholar]
- 6.Baldwin JA, Rolf JE, Johnson J, Bosers J, Benally C, Trotter RT. Developing culturally sensitive HIV/AIDS and substance abuse prevention curricula for Native American youth. J Sch Health. 1996;66:322–327. doi: 10.1111/j.1746-1561.1996.tb03410.x. [DOI] [PubMed] [Google Scholar]
- 7.Northwest Portland Area Indian Health Board. Project Red Talon: Native Voices. 2012. Available at: http://www.npaihb.org/epicenter/project/native_voices_project. Accessed April 3, 2012.
- 8.National Coalition of STD Directors, Centers for Disease Control and Prevention, Indian Health Service, Mercer University School of Medicine. NativeSTAND. 2011. Available at: http://www.nativestand.com/index.php/content/index/about_us. Accessed April 3, 2012.
- 9.Kaestle CE, Halpern CT, Miller WC, Ford CA. Young age at first sexual intercourse and sexually transmitted infections in adolescents and young adults. Am J Epidemiol. 2005;161(8):774–780. doi: 10.1093/aje/kwi095. [DOI] [PubMed] [Google Scholar]
- 10.Buston K, Williamson L, Hart G. Young women under 16 years with experience of sexual intercourse: who becomes pregnant? J Epidemiol Community Health. 2007;61(3):221–225. doi: 10.1136/jech.2005.044107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sandfort TGM, Orr M, Hirsch JS, Santelli J. Long-term health correlates of timing of sexual debut: results from a national US study. Am J Public Health. 2008;98(1):155–161. doi: 10.2105/AJPH.2006.097444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Collins C, Diallo DD. A prevention response that fits America’s epidemic: community perspectives on the status of HIV prevention in the United States. J Acquir Immune Defic Syndr. 2010;55(suppl 2):S148–S150. doi: 10.1097/QAI.0b013e3181fbcb22. [DOI] [PubMed] [Google Scholar]
- 13.Campbell MK, Elbourne DR, Altman DG. CONSORT statement: extension to cluster randomised trials. BMJ. 2004;328(7441):702–708. doi: 10.1136/bmj.328.7441.702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wallerstein N, Duran B. In: The conceptual, historical, and practice roots of community based participatory research and related participatory traditions. Community Based Participatory Research for Health. Minkler M, Wallerstein N, editors. San Francisco, CA: Jossey-Bass; 2003. pp. 27–52. [Google Scholar]
- 15.Israel BA, Schulz AJ, Parker EA, Becker AB, Allen AJ, III, Guzman R. In: Critical issues in developing and following community based participatory research principles. Community Based Participatory Research for Health. Minkler M, Wallerstein N, editors. San Francisco, CA: Jossey-Bass; 2003. pp. 53–76. [Google Scholar]
- 16.De Las Nueces D, Hacker K, DiGirolamo A, Hicks LS. A systematic review of community-based participatory research to enhance clinical trials in racial and ethnic minority groups. Health Serv Res. 2012;47(3 pt 2):1363–1386. doi: 10.1111/j.1475-6773.2012.01386.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Manson SM, Garroutte E, Goins RT, Henderson PN. Access, relevance, and control in the research process: lessons from Indian country. J Aging Health. 2004;16(5 suppl):58S–77S. doi: 10.1177/0898264304268149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gone JP. Research reservations: response and responsibility in an American Indian community. Am J Community Psychol. 2006;37(3-4):333–340. doi: 10.1007/s10464-006-9047-2. [DOI] [PubMed] [Google Scholar]
- 19.Mello MM, Wolf LE. The Havasupai Indian tribe case–lessons for research involving stored biologic samples. N Engl J Med. 2010;363(3):204–207. doi: 10.1056/NEJMp1005203. [DOI] [PubMed] [Google Scholar]
- 20.US Census Bureau. United States Census 2010. 2012. Available at: http://www.census.gov. Accessed October 15, 2012.
- 21.Barnes PM, Adams PF, Powell-Griner E. Health characteristics of the American Indian or Alaska Native adult population: United States, 2004–2008. Natl Health Stat Report. 2010;20:1–22. [PubMed] [Google Scholar]
- 22.Sarche MC, Whitesell NR. Child development research in North American Native Communities—looking back and moving forward: introduction. Child Dev Perspect. 2012;6(1):42–48. [Google Scholar]
- 23.Kaufman CE, Mitchell C, Beals J et al. Circle of life: rationale, design, and baseline results of an HIV prevention intervention among Young American Indian adolescents of the Northern Plains. Prev Sci. 2010;11(1):101–112. doi: 10.1007/s11121-009-0153-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brown CH, Wang W, Kellam SG et al. Methods for testing theory and evaluating impact in randomized field trials: intent-to-treat analyses for integrating the perspectives of person, place, and time. Drug Alcohol Depend. 2008;95(suppl 1):S74–S104. doi: 10.1016/j.drugalcdep.2007.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Duncan GJ. When to promote, and when to avoid, a population perspective. Demography. 2008;45(4):763–784. doi: 10.1353/dem.0.0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harel O, Pellowski J, Kalichman S. Are we missing the importance of missing values in HIV prevention randomized clinical trials? Review and recommendations. AIDS Behav. 2012;16(6):1382–1393. doi: 10.1007/s10461-011-0125-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.ORBIS Associates. Circle of Life HIV/AIDS and STD Prevention Curriculum: Wellness Education for American Indian and Alaska Native Middle School Students. Washington, DC: ORBIS Associates; 2002. [Google Scholar]
- 28.Kaufman CE, Litchfield A, Schupman E, Mitchell CM. Circle of Life HIV/AIDS-prevention intervention for American Indian and Alaska Native Youth. Am Indian Alsk Native Ment Health Res. 2012;19(1):140–153. doi: 10.5820/aian.1901.2012.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.LaFrance J, Nichols R. Indigenous Evaluation Framework: Telling our story in our place and time. 2009. Available at: http://indigeval.aihec.org/Shared%20Documents/0-Intro_Contents.pdf. Accessed August 25, 2011.
- 30. Optimal Design Software for Multi-level and Longitudinal Research [computer program]. Version 3.01. 2011. Available at: http://sitemaker.umich.edu/group-based/optimal_design_software. Accessed April 12, 2012.
- 31.Raudenbush SW. Statistical analysis and optimal design for cluster randomized trials. Psychol Methods. 1997;2(2):173–185. doi: 10.1037/1082-989x.5.2.199. [DOI] [PubMed] [Google Scholar]
- 32. PASW Statistics, 18.0 [computer program]. Version 14.0.1. Chicago, IL: SPSS, Inc.; 2009.
- 33.Stata Statistical Software: Release 11.0 [computer program] College Station, TX: Stata Corporation; 2009. [Google Scholar]
- 34.Muthén LK, Muthén BO. Mplus User’s Guide. 4th ed. Los Angeles, CA: Muthen & Muthen; 2006. [Google Scholar]
- 35.White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30(4):377–399. doi: 10.1002/sim.4067. [DOI] [PubMed] [Google Scholar]
- 36.Robinson GK. That BLUP is a good thing: the estimation of random effects. Stat Sci. 1991;6(1):15–32. [Google Scholar]
- 37.Breslow NE, Clayton DG. Approximate inference in generalized linear mixed models. J Am Stat Assoc. 1993;88(421):9–25. [Google Scholar]
- 38.Little RJ, Rubin DB. Statistical Analysis With Missing Data. 2nd ed. New York, NY: John Wiley; 2004. [Google Scholar]
- 39.Schwartz SJ, Phelps E, Lerner JV et al. Promotion as prevention: positive youth development as protective against tobacco, alcohol, illicit drug, and sex initiation. Appl Dev Sci. 2010;14(4):197–211. [Google Scholar]
- 40.Muthén LK, Muthén BO. Mplus User’s Guide. 7th ed. Los Angeles, CA: Muthén & Muthén; 1998-2012. [Google Scholar]
- 41.Allison PD. Missing data techniques for structural equation modeling. J Abnorm Psychol. 2003;112(4):545–557. doi: 10.1037/0021-843X.112.4.545. [DOI] [PubMed] [Google Scholar]
- 42.Carey MP, Carey KB, Kalichman SC. Risk for human immunodeficiency virus (HIV) infection among persons with severe mental illnesses. Clin Psychol Rev. 1997;17:271–291. doi: 10.1016/s0272-7358(97)00019-6. [DOI] [PubMed] [Google Scholar]
- 43.Kann L, Kinchen SA, Williams BI . Youth Risk Behavior Surveillance - United States 1999. Atlanta, GA: CDC; 2000. [PubMed] [Google Scholar]
- 44.Harris KM, Florey F, Tabor J, Bearman PS, Jones J, Udry JR. Chapel Hill, NC: Carolina Population Center; 2003. The National Longitudinal Study of Adolescent Health: Research Design. [Google Scholar]
- 45. Muthén L, Muthén BO. Chi-square difference testing using the Sartorra-Bentler scaled chi-square. Note on Mplus website. 2005. Available at: www.statmodel.com. Accessed January 8, 2013.
- 46.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall, Inc.; 1986. [Google Scholar]
- 47.Hankins CA, de Zalduondo BO. Combination prevention: a deeper understanding of effective HIV prevention. AIDS. 2010;24(suppl 4):S70–S80. doi: 10.1097/01.aids.0000390709.04255.fd. [DOI] [PubMed] [Google Scholar]
- 48.Morin SF, Kelly JA, Charlebois ED, Remien RH, Rotheram-Borus MJ, Cleary PD. Responding to the national HIV/AIDS strategy–setting the research agenda. J Acquir Immune Defic Syndr. 2011;57(3):175–180. doi: 10.1097/QAI.0b013e318222c0f9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Coates TJ. An expanded behavioral paradigm for prevention and treatment of HIV-1 infection. J Acquir Immune Defic Syndr. 2013;63(suppl 2):S179–S182. doi: 10.1097/QAI.0b013e318299eff0. [DOI] [PMC free article] [PubMed] [Google Scholar]