Abstract
The Centers for Disease Control and Prevention recently established a new reference value (≥ 5 μg/dL) as the standard for identifying children with elevated blood lead levels (EBLs). At present, 535 000 US children aged 1 to 5 years (2.6%) are estimated to have EBLs according to the new standard, versus 0.8% according to the previous standard (≥ 10 μg/dL). Because EBLs signify the threshold for public health intervention, this new definition increases demands on lead poisoning prevention efforts. Primary prevention has been proven to reduce lead poisoning cases and is also cost effective; however, federal budget cuts threaten the existence of such programs. Protection for the highest-risk children necessitates a reinstatement of federal funding to previous levels.
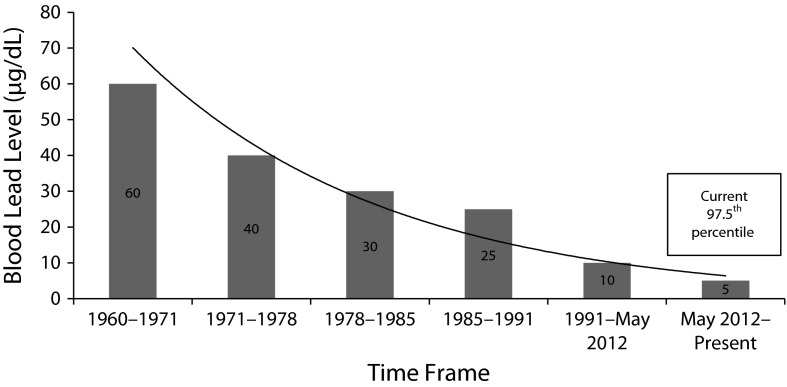
In May 2012, officials of the Centers for Disease Control and Prevention (CDC) announced that they had accepted the recommendations set forth by the Advisory Committee on Childhood Lead Poisoning Prevention (ACCLPP) for (1) the discontinuation of the term blood lead “level of concern,” to acknowledge that there is no safe level of lead exposure, and (2) the use of a new reference value for the identification of children with elevated blood lead levels (EBLs).1 The level of concern, previously defined as 10 micrograms of lead per deciliter of blood, was established by the CDC as the EBL that should initiate a public health response and had been previously unchanged since 1991.2 By contrast, the new reference value is 5 micrograms per deciliter.1 Figure 1 depicts the decline in CDC-recommended blood lead level (BLL) action levels, a drop of more than 90% over the past several decades.3,4 Regardless of the action level of the time, childhood EBLs have long been targeted for complete elimination.5–9
FIGURE 1—
Trends in Centers for Disease Control and Prevention’s childhood blood lead level of concern: United States, 1960–2014.
LEAD EXPOSURE OUTCOMES
Despite the previous acceptance of 10 micrograms per deciliter as a level of concern for the identification of children being exposed to lead, it is important to note that the level of concern was never intended to describe the threshold for adverse effects of lead exposure2; research has continually shown that no amount of lead exposure is safe.7,10–14 Research suggests that BLLs below 10 micrograms per deciliter cause negative health consequences, including cognitive, auditory, speech, and behavioral impairments that may be irreversible and may also result in high societal costs, such as increased health care costs, increased incidence of violent crime, increased need for special education services, reduced school and work performance, and reduced lifetime earning potential.2,10,15–17
In addition, the National Toxicology Program's 2012 monograph concluded that there is sufficient evidence to suggest that children with even lower BLLs (< 5 μg/dL) may experience decreases in IQ and academic achievement, as well as a higher incidence of attention-related and other behavioral problems.18 Research also suggests that the potential risk of IQ loss may be more profound at BLLs below 10 micrograms per deciliter than above, indicating the possibility of a supralinear dose–response relationship.4,11 The National Toxicology Program also recognized that limited evidence associates low-level blood lead concentrations with decreased prenatal cognitive function, decreased glomerular filtration rate, and delayed puberty.18 Furthermore, research suggests that children with BLLs well below the previous 10 micrograms per deciliter standard can benefit from aggressive public health interventions.16
New Blood Lead Reference Value
In an effort to provide for the earlier identification of children who are being exposed to lead (by living or staying for long periods in environments with lead hazards) and to minimize the documented adverse effects of low-level blood lead, the ACCLPP recommended using a new reference value as the standard for identifying children with EBLs. The new reference value is based on the 97.5th percentile of BLL concentrations for US children aged 1 to 5 years, which is currently equivalent to 5 micrograms per deciliter.15,19 It was further recommended that this reference value be reevaluated every 4 years with data from the most recent childhood population–based blood lead surveys, expected from the National Health and Nutritional Examination Survey (NHANES).15
Data from the 2007 to 2010 NHANES cycle provide a nationally representative, weighted estimate for the number of US children with EBLs; data suggest that 535 000 US children aged 1 to 5 years currently have BLLs at or above 5 micrograms per deciliter.12 The estimate of 535 000 children represents 2.6% of the US population of children aged 1 to 5 years; by contrast, for the same data cycle, only 0.8% of US children aged 1 to 5 years had BLLs at or above 10 micrograms per deciliter.12 Thus, lowering the blood lead reference value to at or above 5 micrograms per deciliter multiplies the number of children identified with EBLs.
Furthermore, more recent data are available that are based, not on representative estimates, but rather on blood lead tests actually performed. In 2011, the CDC reported that of the approximately 3.5 million US children younger than 72 months who were screened for lead, more than 19 500 (0.56% of tested children) had BLLs of 10 micrograms per deciliter or higher, and more than 184 000 tested children (5.2%) had confirmed BLLs between 5 and 9 micrograms per deciliter.20 These more recent data support the findings of previous NHANES cycles: a substantially larger number of children have BLLs of 5 micrograms per deciliter or higher than have BLLs of 10 micrograms per deciliter or higher. Consequently, because the EBL value signifies the threshold at which public health intervention is recommended, lowering the EBL reference value considerably increases the demands put on lead poisoning prevention programs and other public health entities (e.g., increased need for EBL case management, blood lead tests, surveillance and education, and environmental investigations).19
The CDC agreed with the ACCLPP recommendation for the discontinuation of the use of the term level of concern; experts abandoned this terminology because it implies that a level of lead exposure may exist that is not of concern, and data suggest otherwise.15 However, because of resource constraints, the CDC could only “concur in principle” with the recommendation for the use of the 97.5th percentile of BLL concentrations (currently 5 μg/dL) as the childhood EBL reference value.15 Current data from the 2007 to 2010 NHANES cycle indicate that more than half a million children have BLLs of 5 micrograms per deciliter or higher, so simply agreeing in principle may not adequately protect the health of a large number of lead-exposed children.12
Trends in Blood Lead Levels
Lead exposure in the United States has consistently fallen over the past few decades, primarily because of policy changes, federal regulations, and public health efforts.2,7,16,21,22 In 2009, the number of US children aged 6 years or younger with BLLs above 10 micrograms per deciliter was estimated to be less than 1%; by contrast, in 1991, 9% of US children had BLLs above 10 micrograms per deciliter.6,16 NHANES data, presented in Table 1, demonstrate a decreasing trend in both the geometric mean BLL and the percentage of US children aged 1 to 5 years with BLLs of 5 micrograms per deciliter or higher since 1988.
TABLE 1—
Trends in Blood Lead Levels for US Children Aged 1–5 Years: National Health and Nutritional Examination Survey, 1988–2010
| Measure | 1988–1991 | 1991–1994 | 1999–2002 | 2003–2006 | 2007–2010 |
| BLL, μg/dL, geometric mean | 3.6 | 2.7 | 1.9 | 1.6 | 1.3 |
| BLL ≥ 5 μg/dL, % | 31.40 | 20.90 | 8.60 | 4.10 | 2.60 |
| BLL ≥ 5 μg/dL, no. | 2232 | 2392 | 1621 | 1879 | 1653 |
Although NHANES data demonstrate a downward trend in BLLs overall, disparities among racial/ethnic and income groups still exist.7,12,13 Data from 1998 to 2004 demonstrate that mean BLLs, as well as the distribution of higher BLLs, continue to be greater among non-Hispanic Black children.7,12 Moreover, declines in BLLs continue to be slower among lower-income children.7,12 In addition, despite the declines, the overall geometric mean BLL for all children continues to be well above the estimated natural body burden of lead, which existed prior to anthropogenic increases in lead availability.14 Further, in light of the evidence that associates low-level lead exposure (BLL < 5 μg/dL) with a myriad of adverse health effects, the historical decline may not be adequate for the protection of public health.18 Therefore, despite the overall decreasing trend in BLLs, the data imply that large lead exposures still exist and that many US children continue to suffer from these exposures.6,11
BLOOD LEAD SURVEILLANCE
National surveillance is necessary for continued understanding of the magnitude of the childhood lead poisoning problem. National blood lead surveillance data can identify children being exposed to lead and are available from the CDC for 1997 to 2011 (with data for children with BLLs of 5–9 μg/dL available only for 2010 and 2011).20 Surveillance data provide insight into the number of children tested for lead exposure each year, in each state that reports data to the CDC (in 2011, 33 states, plus Washington, DC, and New York City), as well as the number of children younger than 72 months residing in each state.20 This allows for calculation of the percentage of young children who received the recommended blood lead test; for example, in 2011, the total lead-screening rate for reporting states was only 14.5%.20 In addition to relatively low screening rates, the surveillance data are limited by differences in individual state reporting requirements and only include data for children who presented with BLLs.20 Furthermore, despite federal regulation mandating blood lead tests for all children enrolled in Medicaid (because they are considered to be a high-risk group for lead poisoning), only a fraction of enrolled children are actually tested.2,6,7 Improved national surveillance would provide critical insight to inform public health professionals and policymakers on the continuing need for primary prevention.
Currently, state and local childhood lead poisoning prevention programs (CLPPPs) are charged with increasing lead-screening rates, reporting surveillance data to the CDC, identifying and providing case management for children with EBLs, and implementing housing-based primary prevention strategies.2,23 The CDC was authorized to create CLPPPs in response to the Lead Contamination Control Act of 1988. The act allowed the CDC to fund nearly 60 state and local health departments in their efforts to eliminate childhood lead poisoning23; however, the status of many of these programs has recently been threatened by drastic funding cuts.24
In 2000, the National Center for Healthy Housing published the findings of a survey of all state CLPPPs.25 Among the key recommendations highlighted in the report were that (1) programs without a currently effective system to identify new EBL cases need to make the establishment of such a system a high priority, and (2) programs should have case closure criteria that include the reduction of a child’s BLL and the control of environmental lead hazards.25 Levin et al. suggest that in addition to screening and mediating environmental hazards after an EBL case presents, to be most effective CLPPPs need to increase their focus on primary prevention.13 Although surveillance is an essential component, simply identifying EBL cases will not inherently reduce the risk of childhood lead poisoning.6,13,20
PREVENTION
With primary prevention, lead exposure sources are eliminated prior to the poisoning of a child, typically by addressing high-risk housing (e.g., housing built prior to the residential lead-based paint [LBP] ban of 1978; the older the housing, the higher the risk).6,13,26,27 In its 2000 report, the President’s Task Force on Environmental Health Risks and Safety Risks to Children proposed that addressing the highest-risk (pre-1960) housing with lead hazard screening and interim controls would result in the virtual elimination of residential LBP within 10 years.8 Had the proposed primary prevention activities necessary to reach this goal been implemented in 2000, it was estimated that the LBP hazards in 18.4 million housing units could have been removed by 2010.8
Jacobs et al., examining nationally representative housing data from 1998 to 2000, estimated that 24 million US homes contained substantial LBP hazards.27 Of those homes, approximately 1.2 million units were occupied by low-income families with children younger than 6 years.27 The same study also found that interior dust lead hazards (a major pathway of lead exposure and strong predictor of EBLs) were also found in an estimated 15.5 million units (16% of US housing).27 Although lead is a multimedia contaminant and has alternative exposure sources, the principal cause of EBLs in children remains exposure to deteriorating LBP and the associated dust; these exposure sources can be greatly reduced through primary prevention activities.6,7,13,16,27
Although the Jacobs et al. study found that from 1990 to 2000 the number of housing units with LBP declined, much lead hazard control work still needs to be done; it was estimated that approximately 25% of US homes with children younger than 6 years still harbor LBP hazards.2,27 From 2005 to 2006, the US Department of Housing and Urban Development (HUD) conducted the American Healthy Homes Survey to measure the levels of several contaminants in US homes. The survey produced an estimate of 37.1 million homes (34.9% of all homes) with some LBP, of which 23.2 million (21.9%) had more than 1 LBP hazard; the large majority of homes with LBP (93%) were built prior to 1978.28 In addition, approximately 3.6 million homes with children younger than 6 years had 1 or more LBP hazards, including 1.1 million low-income households (< $30 000/year); further, the low-income households were more likely than their higher-income counterparts to have LBP hazards (29% vs 18%).28
Although controlling LBP hazards in older housing is an essential component, primary prevention also includes reducing the exposure hazards associated with lead-contaminated dust, soil, water, pottery, imported toys and trinkets, folk remedies, and so on.2,12,13,27 Addressing atypical sources of lead exposure during primary prevention activities is critical, because many children with EBLs have poorly defined sources of lead exposure, and higher BLLs are often indicative of multiple sources of exposure.28 The CDC supports primary prevention and recommends that all sources of lead in children’s environments be controlled or eliminated to protect their health.13,15
Even if the goal of primary prevention were to be realized, EBL case identification and case management (secondary prevention activities) would need to continue.6 The CDC recognizes the importance of CLPPPs as an integral component in such responses.13 Currently, CLPPP case management and medical recommendations for children with detectable BLLs may differ by the concentration of blood lead.6 In addition, depending on the state or municipality, environmental investigation for lead hazards is prompted by different BLLs.2 It is unclear whether new and specific interventions will be recommended for children with BLLs between 5 and 10 micrograms per deciliter; however, the CDC has indicated that the current reference value of greater than or equal to 5 micrograms per deciliter will be used to identify children with EBLs in need of case management.19
FEDERAL FUNDING
Despite the paradigm shift to primary prevention in the public health arena, historically, federal funding has not adequately followed the shift and, rather, has often threatened secondary prevention efforts as well. The estimated $230 million needed annually for 10 years to eliminate lead hazards in all pre-1960 housing (as proposed in 2000 by the President’s Task Force on Environmental Health Risks and Safety Risks to Children) has never been allocated.8 Shortfalls in funding to support the primary prevention of lead poisoning have always existed and have worsened in recent years.
The HUD Office of Healthy Homes and Lead Hazard Control (OHHLHC) is 1 of the principal federal programs contributing to the primary prevention of childhood lead poisoning. Since 1991, the office has provided grant funding to state and local agencies for lead hazard control in low-income housing; in 2005 it provided $139 million through several grants for such efforts.2 In fiscal year (FY) 2013 and again in FY 2014, HUD requested $120 million for this lead control program, including $90 million for lead hazard control programs and $4 million for lead technical studies grants.29 Should HUD receive funds for the coming year that match 2012 appropriations, the agency aims to maintain its focus on making homes safer for children and working toward the federal goal of eliminating childhood lead poisoning.
Like HUD, the CDC is a pivotal federal program in the prevention of childhood lead poisoning, responsible for surveillance, clinical guidance, and blood laboratory quality control.30 To date, the lead program at the CDC has served nearly 1 million US children with BLLs of concern (≥ 10 μg/dL, the previous guideline) and screened millions more.24 In 2011 alone, CDC grant recipients screened more than 3.5 million children for lead exposure and provided case management for nearly 30 000 children in need.20,24 Stimulated in part by the 2009 Surgeon General’s Call to Action to Promote Healthy Homes, the CDC also expanded its lead poisoning prevention programs into a Healthy Homes Initiative that implements primary prevention strategies for several home-based health and safety hazards.2,31 At the initiative's height, CDC grants funded 34 state healthy homes programs, as well as separate programs in the District of Columbia and Puerto Rico.32,33 However, as with CLPPPs, the status of state healthy homes programs has drastically changed for the worse.
In response to federal budget allocations, the CDC has been forced to propose steep budget cuts to environmental health programs, including the Healthy Homes and Lead Poisoning Prevention Program branch. In FY 2012, the federal allocation to this branch was reduced from $29 million to slightly less than $2 million, with an enacted budget of slightly more than $2.5 million.1,34 To respond to this dramatic cut, the CDC proposed the creation of a multifaceted Healthy Home and Community Environments program to essentially combine CLPPP activities with those of the existing National Asthma Control Program.33 As proposed, the effectiveness of both federally funded programs will be severely compromised; the FY 2013 President’s budget ($27.3 million) for both activities is only slightly more than the FY 2012 budget was for the asthma management program alone ($25.3 million).34 The populations served, as well as the goals and the methods of the 2 programs, are distinct. Thus, it is feared that this will result in the failure to advance either childhood lead poisoning prevention or asthma control efforts.24
The President's budget message for FY 2014, recently released by the Office of Management and Budget, indicates the current administration’s budget priorities.35 The President’s budget recommended $47.6 billion toward HUD programs and $80.1 billion to the Department of Health and Human Services (home of the CDC); however, it contained no specific mention of lead poisoning or other home-based primary prevention programs, and congressional appropriations may vary greatly from the President’s proposals.35
Like HUD, the CDC has recently provided justification to Congress for its FY 2014 budget request (almost $5 million for the Healthy Homes and Lead Poisoning Prevention Program branch specifically).34 The CDC maintains that this increase in funding over FY 2012 (by ∼$2.5 million) will allow it to provide expertise to support state and local health departments currently using the Healthy Homes and Lead Poisoning Prevention Surveillance System software. However, the CDC acknowledged in the justification that appropriations of this amount would not support extramural activities.34 This budget request mirrors the response the CDC gave to the ACCLPP recommendation that the “CDC should develop and help implement a nationwide primary prevention policy”; the CDC agreed “in principle,” but also recognized that the “implementation of primary-prevention programs is not currently practicable.”15 Through its response, the CDC acknowledged that without adequate funding, it cannot further advance primary prevention.
The CDC, HUD, and the Environmental Protection Agency compose a 3-legged support system necessary to fully address the problem of lead poisoning.30 By essentially cutting off the CDC leg, federal budget cuts have threatened the entire system. Without adequate funding, the CDC will be challenged to meet its missions of screening children for lead poisoning, tracking disease incidence, and providing education to clinicians, public health professionals, and the general public. As a consequence, the lead hazard control activities of HUD, the regulatory functions of the Environmental Protection Agency (responsible for standards of exposure, training professional lead workers, implementing and enforcing mandates, etc.), and the educational components of all of the organizations will also fail to perform optimally.24,30 In light of the documented cost savings and health benefits, as well as the nonhealth benefits, of primary prevention activities, the failure of the federal government to adequately fund all aspects of the support system defies logic.
COSTS AND BENEFITS OF PRIMARY PREVENTION
Primary prevention of childhood lead poisoning is a cost-effective approach and therefore the ideal approach. The cost of environmental disease, including childhood lead poisoning, has been assessed in the literature; recently, Trasande and Liu estimated that in 2008 alone, the cost of childhood lead poisoning was more than $50 billion ($5.9 million in direct health care costs and $50.9 billion in lost economic productivity). In their estimation, the cost of lead poisoning exceeded the combined costs associated with methylmercury toxicity, asthma, intellectual disability, autism, attention deficit hyperactivity disorder, and childhood cancer by more than $25 billion.36 Furthermore, the costs associated with case management, medical diagnosis, and treatment of children with BLLs between 5 and 10 micrograms per deciliter have not yet been fully assessed and may be considerable.16 Many of the costs associated with childhood lead poisoning might be largely avoided through the implementation of cost-effective primary prevention activities.
In federally subsidized housing, HUD’s regulatory impact analysis predicted that the monetized benefits (i.e., improved lifetime earnings for children living in or visiting units with LBP hazards) from the first year of HUD’s final rule on LBP (effective November 15, 1999) would be more than $1.1 billion. Subtracting the costs (> $250 million) of hazard reduction work (e.g., paint stabilization, window replacement, soil cover, dust cleanup), would still result in estimated first-year net benefits of $890 million.37 In 2002, Grosse et al. published their findings on economic gains resulting from the decrease in BLLs from 1976 to 1999.38 By projecting improvements in worker productivity, as a result of higher IQs attributable to less lead exposure than previous generations, the authors estimated that the economic benefit of reducing BLLs ranged from $110 billion to $319 billion annually, with a base case estimate of $213 billion. Although the reduction in mean BLLs from 1976 to 1999 was larger than that of recent years, cost savings associated with reducing lead exposure are expected to continue to be high, particularly in light of the savings incurred by avoiding other adverse health effects associated with exposure to lead (e.g., hypertension, low birth weight, and infant mortality).38
In another study, Brown found that lifetime economic savings of more than $46 000, related to medical care, special education, and lost productivity, may be expected from the abatement of environmental lead hazards, per building abated.10 An analysis by Gould found that the conservative estimate for the net economic savings of lead hazard control programs was somewhere between $181 and $269 billion, essentially a savings (related to medical treatment, lifetime earnings, tax revenue, special education, and criminal activity) of up to $221 for each dollar invested.16 Another study estimated the net benefits if 1 cohort of children (newborn to 6 years) had BLLs of less than 1 microgram per deciliter, as a result of increased primary prevention aimed at children and pregnant women; the study found that savings could be as high as $50 000 per child ($1.2 trillion lifetime total) and, moreover, could contribute an additional 4.8 million quality-adjusted life-years for society as a whole.39
In 2000, a federal task force conservatively estimated that following a 10-year plan (2001–2010) to reduce LBP hazards in pre-1960, low-income housing could result in a net benefit of $8.9 billion. These predicted savings would stem from avoided medical costs and special education and increased lifetime earnings, attributable to the reduction of associated BLLs. This 10-year plan was also predicted to produce market benefits from the creation of 2.3 million lead-safe homes8; however, the plan was never implemented. Nevin et al. found that, in addition to health benefits, lead-safe window replacement could also lower annual energy costs in pre-1960 homes with single-pane windows by 15% to 25% ($130–$486 per housing unit), which could reduce total national residential energy use by 5% or more.40 Furthermore, depending on home size and the number of windows replaced, housing market value was estimated to increase by $5900 to $14 300 per unit.40
The literature contains several cost–benefit analyses that support the notion that lead hazard control costs far less than the monetized benefits.22 Cost–benefit analyses of lead hazard control programs also demonstrate that the value of lead hazard control is comparable to other successful public health interventions, such as vaccination programs.11,16 For example, 1 study found that the net savings of a routine vaccination program from direct and societal costs were $9.9 billion and $43.3 billion, respectively, which is akin to savings from the primary prevention of lead poisoning.41 Research further suggests that many early childhood education programs are also cost effective and may produce societal benefits similar to lead poisoning primary prevention programs42; however, lead-associated deficits, which place undue demands on early education programs, could be avoided through successful primary prevention of lead poisoning. Furthermore, it is likely that the return on an initial investment in lead poisoning primary prevention will only increase over time, because thousands more children will be recognized as having EBLs according to the new 5 micrograms per deciliter reference value.
CONCLUSIONS
Childhood lead poisoning continues to be a prominent public health issue. It is an entirely preventable disease—if sufficient resources are invested.10 The activities undertaken by CLPPPs are widely seen as some of the most successful public health achievements.22,43 Childhood lead poisoning prevention activities have contributed to a decline in the percentage of children with EBLs (as defined by the previous ≥ 10 μg/dL standard), but continued declines may depend on future funding.13,43 In addition, childhood lead poisoning prevention activities have been estimated to save more than $200 billion annually.43 By substantially reducing the resources available to federal, state, and local lead poisoning prevention programs, the federal government is inadvisably targeting public health measures that have proved to be effective. Undoubtedly, this failure to recognize the importance of these public health services will be felt most profoundly by the nation’s high-risk children.
By ignoring the cost-effective approach of primary prevention and by failing to adequately fund lead poisoning prevention activities in general, the federal government is essentially committing an environmental injustice. Programs that assess and mediate environmental lead hazards reduce population-wide risk. Severely defunding—effectively eliminating—such programs will disproportionately burden poor and minority children.44 Furthermore, when environmental lead hazards are not addressed, the risk of lead poisoning increases for children who subsequently live in contaminated environments.10 To properly protect these high-risk children and prevent legacy lead poisoning, primary prevention activities should be expanded, rather than restricted by federal funding constraints.
Georges C. Benjamin, executive director of the American Public Health Association, expressed concern for the lack of financial support for lead poisoning prevention:
These [recent ACCLPP] recommendations should be a wake-up call to members of Congress that they are missing opportunities to protect the health of our nation’s children. Appropriate funding for lead poisoning programs must be reinstated.1
We agree with Benjamin and with some of the nation’s authorities on lead poisoning prevention (e.g., the National Center for Healthy Housing, the National Safe and Healthy Housing Coalition), who argue that lead poisoning prevention should be funded as a distinct line item and returned at minimum to $29 million, similar to the appropriations of FY 2011.24
The recommendations set forth by ACCLPP, despite the best efforts of federal, state, and local programs, cannot be achieved without proper funding. The CDC itself has supported the primary prevention of childhood lead poisoning, but the current federal budget has severely limited its ability to perform these vital activities. The United States failed to reach its Healthy People 2010 objective for the elimination of childhood lead poisoning, perhaps in part because of inadequate financial investment in prevention.13 Without federal support for these vital programs, we are also destined to fail to meet the same goal set for 2020.9
Those involved in federal funding decisions should reconsider their sizable cuts to lead poisoning prevention. The federal government and its agencies should demonstrate their support of public health through allocation of resources and support for related research; at minimum, programs with demonstrated efficacy that serve the highest-risk populations (low-income and minority children) should be refunded. With a newly acknowledged reference level (≥ 5 μg/ dL) for the identification of children with EBLs, the need for a public health response to these cases will increase dramatically; this highlights the importance of adequate funding to support vital operations. Now more than ever, our nation’s children need us to do more than simply support lead poisoning prevention “in principle.”
Human Participant Protection
No protocol approval was required because no human participants were involved.
References
- 1. American Public Health Association. CDC accepts advisory committee recommendation to replace “level of concern” for lead poisoning with new reference value: renews commitment to primary prevention of lead poisoning. 2012. Available at: http://apha.org/about/news/pressreleases/2012/cdc+advisory+new+reference+value.html. Accessed May 21, 2012.
- 2.Centers for Disease Control and Prevention Advisory Committee on Childhood Lead Poisoning Prevention. Interpreting and managing blood lead levels < 10 μg/dL in children and reducing childhood exposures to lead: recommendations of CDC’s Advisory Committee on Childhood Lead Poisoning Prevention. MMWR Recomm Rep. 2007;56(RR-8):1–16. [PubMed] [Google Scholar]
- 3. Agency for Toxic Substances and Disease Registry. Lead toxicity. 2007. Available at: http://www.atsdr.cdc.gov/csem/csem.asp?csem=7&po=0. Accessed April 17, 2013.
- 4.Lanphear BP, Hornung R, Khoury J et al. Low-level environmental lead exposure and children’s intellectual function: an international pooled analysis. Environ Health Perspect. 2005;113(7):894–899. doi: 10.1289/ehp.7688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Centers for Disease Control and Prevention. Eliminate elevated blood lead levels in children. Available at: http://www.healthypeople.gov/2010/document/html/objectives/08-11.htm Accessed February 24, 2014.
- 6.American Academy of Pediatrics Committee on Environmental Health. Lead exposure in children: prevention, detection, and management. Pediatrics. 2005;116(4):1036–1046. doi: 10.1542/peds.2005-1947. [DOI] [PubMed] [Google Scholar]
- 7.Jones RL, Homa DM, Meyer PA et al. Trends in blood lead levels and blood lead testing among US children aged 1 to 5 years, 1988–2004. Pediatrics. 2009;123(3):e376–e385. doi: 10.1542/peds.2007-3608. [DOI] [PubMed] [Google Scholar]
- 8. President’s Task Force on Environmental Health Risks and Safety Risks to Children. Eliminating childhood lead poisoning: a federal strategy targeting lead paint hazards. 2000. Available at: http://www.cdc.gov/nceh/lead/about/fedstrategy2000.pdf. Accessed April 17, 2013.
- 9. US Department of Health and Human Services. Healthy People 2020: topics and objectives. Environmental health. 2013. Available at: http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=12. Accessed April 17, 2013.
- 10.Brown MJ. Costs and benefits of enforcing housing policies to prevent childhood lead poisoning. Med Decis Making. 2002;22(6):482–492. doi: 10.1177/0272989X02238298. [DOI] [PubMed] [Google Scholar]
- 11.Brown MJ, Margolis S. Lead in drinking water and human blood lead levels in the United States. MMWR Surveill Summ. 2012;61(suppl):1–9. [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. Blood lead levels in children aged 1–5 years—United States, 1999–2010. MMWR Morb Mortal Wkly Rep. 2013;62(13):245–248. [PMC free article] [PubMed] [Google Scholar]
- 13.Levin R, Brown MJ, Kashtock ME et al. Lead exposure in US children, 2008: implications for prevention. Environ Health Perspect. 2008;116(10):1285–1293. doi: 10.1289/ehp.11241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith DR, Flegal AR. The public health implications of humans’ natural levels of lead. Am J Public Health. 1992;82(11):1565–1566. doi: 10.2105/ajph.82.11.1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Centers for Disease Control and Prevention. CDC response to Advisory Committee on Childhood Lead Poisoning prevention recommendations in “Low level exposure harms children: a renewed call of primary prevention.” 2012. Available at: http://www.cdc.gov/nceh/lead/ACCLPP/CDC_Response_Lead_Exposure_Recs.pdf. Accessed May 22, 2012.
- 16.Gould E. Childhood lead poisoning: conservative estimates of the social and economic benefits of lead hazard control. Environ Health Perspect. 2009;117(7):1162–1167. doi: 10.1289/ehp.0800408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Needleman HL, Gunnoe C, Leviton A et al. Deficits in psychologic and classroom performance of children with elevated dentine lead levels. N Engl J Med. 1979;300(13):689–695. doi: 10.1056/NEJM197903293001301. [DOI] [PubMed] [Google Scholar]
- 18. National Toxicology Program. NTP monograph on health effects of low-level lead. 2012. Available at: http://ntp.niehs.nih.gov/NTP/ohat/Lead/Final/MonographHealthEffectsLowLevelLead_prepublication_508.pdf. Accessed April 17, 2013.
- 19. Centers for Disease Control and Prevention. Lead. What do parents need to know to protect their children? 2012. Available at: http://www.cdc.gov/nceh/lead/ACCLPP/blood_lead_levels.htm. Accessed April 17, 2013.
- 20. Centers for Disease Control and Prevention. CDC’s national surveillance data (1997–2011). 2013. Available at: http://www.cdc.gov/nceh/lead/data/national.htm. Accessed April 17, 2013.
- 21.Bernard SM, McGeehin MA. Prevalence of blood lead levels ≥ 5 μg/dL among US children 1 to 5 years of age and socioeconomic and demographic factors associated with blood of lead levels 5 to 10 μg/dL, Third National Health and Nutrition Examination Survey, 1988–1994. Pediatrics. 2003;112(6 pt 1):1308–1313. doi: 10.1542/peds.112.6.1308. [DOI] [PubMed] [Google Scholar]
- 22.Jacobs DE, Kelly T, Sobolewski J. Linking public health, housing, and indoor environmental policy: successes and challenges at local and federal agencies in the United States. Environ Health Perspect. 2007;115(6):976–982. doi: 10.1289/ehp.8990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Centers for Disease Control and Prevention. CDC’s childhood lead poisoning prevention program. 2009. Available at: http://www.cdc.gov/nceh/lead/about/program.htm. Accessed May 26, 2012.
- 24. Written statement of David E. Jacobs, PhD, CIH, research director, National Center for Healthy Housing, CDC’s childhood lead poisoning prevention program to the Subcommittee on Labor, Health and Human Services, Education and Related Agencies Committee on Appropriations, US House of Representatives, March 28, 2012. Available at: http://www.nchh.org/Portals/0/Contents/Senate%20Testimony%20Jacobs%202012_3_28-2012_final.pdf. Accessed April 17, 2013.
- 25.McLaine P, Gaitens J. Another link in the chain: state policies and practices for case management and environmental investigation for lead-poisoned children, update. 2001. Available at: http://www.afhh.org/res/res_pubs/Link_in_Chain_Update.pdf. Accessed May 22, 2012. [Google Scholar]
- 26. US Government Printing Office. Electronic code of federal regulations. Title 16 CFR Part 1303. 2013. Available at: http://www.ecfr.gov/cgi-bin/text-idx?c=ecfr&tpl=/ecfrbrowse/Title16/16cfr1303_main_02.tpl. Accessed April 17, 2013.
- 27.Jacobs DE, Clickner RP, Zhou JY et al. The prevalence of lead-based paint hazards in US housing. Environ Health Perspect. 2002;110(10):A599–A606. doi: 10.1289/ehp.021100599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. US Department of Housing and Urban Development. American Healthy Homes Survey: lead and arsenic findings. 2011. Available at: http://portal.hud.gov/hudportal/documents/huddoc?id=AHHS_REPORT.pdf. Accessed April 17, 2013.
- 29. US Department of Housing and Urban Development. FY 2014 congressional justifications. 2013. Available at: http://portal.hud.gov/hudportal/documents/huddoc?id=LEADHAZARDREDUCTION.pdf. Accessed April 17, 2013.
- 30. Children’s Health Protection Advisory Committee. Letter to Administrator Jackson regarding childhood lead poisoning. 2012. Available at: http://yosemite.epa.gov/ochp/ochpweb.nsf/content/chpac_childhood_lead_poison_letter.htm. Accessed April 17, 2013.
- 31. The Surgeon General's Call to Action to Promote Healthy Homes. Rockville, MD: US Office of the Surgeon General; 2009. Available at: http://www.ncbi.nlm.nih.gov/books/NBK44192. Accessed February 24, 2014.
- 32. Centers for Disease Control and Prevention. Healthy homes—state programs. 2011. Available at: http://www.cdc.gov/HealthyHomes/programs.html. Accessed May 21, 2012.
- 33. Centers for Disease Control and Prevention. Fiscal year 2013: justification of estimates for appropriations committees. 2012. Available at: http://www.cdc.gov/fmo/topic/Budget%20Information/appropriations_budget_form_pdf/FY2013_CDC_CJ_Final.pdf. Accessed May 21, 2012.
- 34. Centers for Disease Control and Prevention. Fiscal Year 2014: justification of estimates for appropriation committees. 2013. Available at: http://www.cdc.gov/fmo/topic/Budget%20Information/appropriations_budget_form_pdf/FY2014_CJ_CDC_FINAL.pdf. Accessed April 17, 2013.
- 35. Office of Management and Budget. Budget of the United States government: fiscal year 2014. 2013. Available at: http://www.whitehouse.gov/omb/budget/Overview. Accessed April 17, 2013.
- 36.Trasande L, Liu Y. Reducing the staggering costs of environmental disease in children, estimated at $76.6 billion in 2008. Health Aff (Millwood) 2011;30(5):863–870. doi: 10.1377/hlthaff.2010.1239. [DOI] [PubMed] [Google Scholar]
- 37. US Department of Housing and Urban Development. Economic analysis of the final rule on lead-based paint: requirements for notification, evaluation and reduction of lead-based paint hazards in federally-owned residential property and housing receiving federal assistance. 1999. Available at: http://portal.hud.gov/hudportal/documents/huddoc?id=DOC_25478.pdf. Accessed April 17, 2013.
- 38.Grosse SD, Matte TD, Schwartz J, Jackson RJ. Economic gains resulting from the reduction in children’s exposure to lead in the United States. Environ Health Perspect. 2002;110(6):563–569. doi: 10.1289/ehp.02110563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Muennig P. The social costs of childhood lead exposure in the post-lead regulation era. Arch Pediatr Adolesc Med. 2009;163(9):844–849. doi: 10.1001/archpediatrics.2009.128. [DOI] [PubMed] [Google Scholar]
- 40.Nevin R, Jacobs DE, Berg M, Cohen J. Monetary benefits of preventing childhood lead poisoning with lead-safe window replacement. Environ Res. 2008;106(3):410–419. doi: 10.1016/j.envres.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 41.Zhou F, Santoli J, Messonnier ML et al. Economic evaluation of the 7-vaccine routine childhood immunization schedule in the United States, 2001. Arch Pediatr Adolesc Med. 2005;159(12):1136–1144. doi: 10.1001/archpedi.159.12.1136. [DOI] [PubMed] [Google Scholar]
- 42.Reynolds AJ, Temple JA. Cost-effective early childhood development programs from preschool to third grade. Annu Rev Clin Psychol. 2008;4:109–139. doi: 10.1146/annurev.clinpsy.3.022806.091411. [DOI] [PubMed] [Google Scholar]
- 43.Centers for Disease Control and Prevention. Ten great public health achievements—United States, 2001–2010. MMWR Morb Mortal Wkly Rep. 2011;60(19):619–623. [PubMed] [Google Scholar]
- 44.Jacobs DE. Environmental health disparities in housing. Am J Public Health. 2011;101(suppl 1):S115–S122. doi: 10.2105/AJPH.2010.300058. [DOI] [PMC free article] [PubMed] [Google Scholar]