Abstract
Objectives. We determined the impact of smoke-free municipal public policies on hospitalizations for chronic obstructive pulmonary disease (COPD).
Methods. We conducted a secondary analysis of hospital discharges with a primary diagnosis of COPD in Kentucky between July 1, 2003, and June 30, 2011 using Poisson regression. We compared the hospitalization rates of regions with and without smoke-free laws, adjusting for personal and population covariates, seasonality, secular trends over time, and geographic region.
Results. Controlling for covariates such as sex, age, length of stay, race/ethnicity, education, income, and urban–rural status, among others, we found that those living in a community with a comprehensive smoke-free law or regulation were 22% less likely to experience hospitalizations for COPD than those living in a community with a moderate–weak law or no law. Those living in a community with an established law were 21% less likely to be hospitalized for COPD than those with newer laws or no laws.
Conclusions. Strong smoke-free public policies may provide protection against COPD hospitalizations, particularly after 12 months, with the potential to save lives and decrease health care costs.
Chronic obstructive pulmonary disease (COPD) is a serious, chronic, progressive lower respiratory disorder characterized by airflow limitation with varying degrees of chronic bronchitis and emphysema. The primary risk factor for COPD is cigarette smoke, with either direct exposure (firsthand smoking) or indirect exposure through secondhand smoke.1–3 COPD is a leading cause of physician office visits4 and emergency department visits,5 and it is a primary cause of hospitalization in older adults.4 COPD is also associated with more comorbidities,6 reduced quality of life,7 decreased functional status,8 depression,7 and cognitive deficits.9 In 2010, the economic burden associated with COPD was approximately $50 billion, including $29.5 billion for direct care, $8 billion in indirect morbidity costs, and $12.4 billion for indirect mortality costs.10 The health care costs associated with COPD for the next 2 decades are projected to be $800 billion.11 Although many states and local US communities have enacted comprehensive smoke-free workplace laws, southern, rural tobacco-growing states and locales lag behind in smoking cessation rates and protection of workers from exposure to secondhand smoke.
The worldwide prevalence of COPD is estimated at 10.1%.12 By comparison, the prevalence of COPD in southeastern Kentucky, a rural tobacco-growing state, is nearly double at 19.6%.13 COPD is currently the third leading cause of death in Kentucky and the United States,14,15 and 9.3% of Kentucky adults have been told by a provider that they have COPD.16 Kentucky is a national leader in smoking prevalence, with 29% of adults reporting current tobacco use.17 One fourth (25%) of Kentucky high school students and 12% of middle school students are current cigarette smokers.18 As of December 1, 2013, 66% of Kentuckians were regularly exposed to secondhand smoke in workplaces and public places.19
Previous studies have shown a decrease in hospitalization20–22 and mortality rates23 for respiratory diseases after smoke-free legislation. As of June 30, 2011, communities in 28 Kentucky counties had enacted smoke-free laws or adopted Board of Health regulations limiting exposure to some degree. The first ordinance was implemented in Lexington-Fayette County in April 2004,24 with the majority of public policies taking effect in 2008–2011. The most comprehensive ordinances and regulations, 100% smoke-free workplace and 100% smoke-free enclosed public place laws, were implemented in communities in 16 counties, covering more than 30% of the state’s population. Moderate smoke-free ordinances and 100% smoke-free enclosed public place laws including restaurants and bars, but not all workplaces, were in effect in 3 counties. Communities in 9 counties had enacted weak smoke-free laws or regulations, protecting workers and patrons in some public and workplace venues with significant exemptions (e.g., age restrictions, enclosed smoking rooms, restaurants only). Laws or regulations in 11 of the 28 counties covered the entire county. Although some additional counties had very limited smoking restrictions that applied only to municipal buildings (not 100% public policies), we did not include these laws in the study. Given the prevalence of smoking and COPD in Kentucky, and the presence of local smoke-free public policies in some counties, we aimed to determine the impact of smoke-free laws in Kentucky on hospitalizations for COPD exacerbation. We hypothesized that areas with comprehensive smoke-free laws would have lower COPD-related hospitalizations than those with moderate–weak laws and those without laws, controlling for sex, age, length of stay, race/ethnicity, education, income, urban–rural status, primary care physician supply, heart disease, diabetes, smoking rate, quit attempt rate, seasonality, and region of residence. A secondary aim was to determine whether duration of law influenced COPD hospitalizations, controlling for these covariates. We hypothesized that communities with established laws would exhibit lower rates of COPD hospitalization than those with newer or no laws.
METHODS
We obtained case data for all patients discharged from any Kentucky hospital dated between July 1, 2003, and June 30, 2011, from the centralized statewide administrative database (Comp Data). Deidentified records included primary discharge diagnoses,25 dates of admission and discharge, sex, age, and county of residence. We determined length of stay using service dates; hospitalizations shorter than 24 hours were coded as 0.5 day. Length of stay was log-transformed to minimize the impact of extreme high values. We compiled local smoke-free laws and regulations from the Smoke-free Ordinance database at the Kentucky Center for Smoke-free Policy on July 1, 2011. We coded laws and regulations as comprehensive or moderate–weak and defined them as established if they had been enacted at least 1 year before a particular quarter and as newer if they had been in effect less than 1 year. The rationale for the 12-month cutpoint was a prior study demonstrating that those living in communities with established laws of 18 months or longer were more likely to be former smokers and report a longer time since their last cigarette than those in communities with newer laws enacted within 6 to 8 months.26
Selection of Cases
We reviewed primary diagnosis to determine whether the event qualified for inclusion in the study. Selection of cases was limited to those in patients with a primary discharge diagnosis of chronic bronchitis (diagnostic-related group 491), emphysema (diagnostic-related group 492), or chronic airway obstruction not classified elsewhere (diagnostic-related group 496).27,28
We chose diagnosis at discharge as the criterion for inclusion because it is a more accurate reflection of the true condition than the admission diagnosis. We included in the analysis all patients with the relevant International Classification of Diseases, Ninth Revision29 codes who were (1) aged 45 years or older, (2) residents of Kentucky, and (3) discharged between July 1, 2003, and June 30, 2011.
Region of Residence
We classified the 120 counties in the state of Kentucky into 1 of 58 regions, using a modification of the classification scheme used by the University of Kentucky Markey Cancer Control Program and College of Public Health under the direction of the Kentucky Department for Public Health.30 The purpose of the classification was to combine counties that are similar in terms of demographics, socioeconomic factors, health indicators, and geographical proximity.
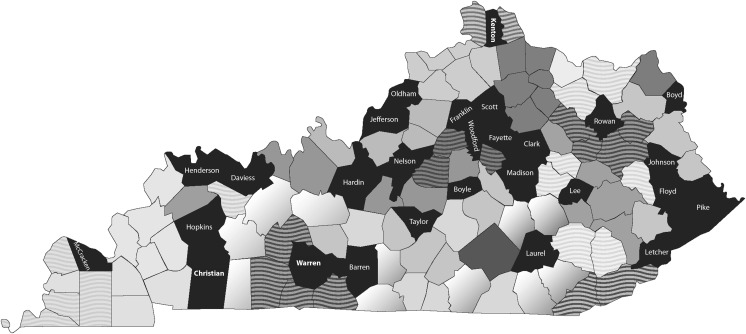
We modified the original classification scheme so that counties with smoke-free ordinances or regulations would each form their own region for the purpose of analysis (Figure 1). Geographic pooling was necessary because of the limited number of COPD hospitalizations per quarter in the smaller counties, nearly all of which do not have smoke-free policies and could be combined with proximal counties without policies. We classified counties with 1 or more smoke-free policies, whether at the city or the county level, as having this type of policy given that most ordinances in Kentucky counties either cover the entire county or are in the largest city as in previous studies.31,32
FIGURE 1—
Smoke-free ordinances and regulations by county: Kentucky, July 1, 2011.
Note. Black indicates county with a smoke-free law. Shading indicates county groups used for the analysis.
Population Demographics and Other Covariates
We used census information and data from the Behavioral Risk Factor Surveillance System to estimate population-level values for median income, education, race/ethnicity, and adult smoking and quit attempt rates. We obtained county-level median income from the 2009 Census, percentage Hispanic33 from the 2010 Census,34 percentage with any postsecondary education from the 2000 Census, and 3-year aggregate estimates for county-level adult smoking and quit attempt rates from the 2001–2011 Behavioral Risk Factor Surveillance System surveys. For each year of COPD cases, we used the 3-year aggregate smoking and quit attempt rates based on that year and the 2 previous years to estimate county-level adult smoking and quit attempts. For example, we used the 2001–2003 aggregate to estimate these rates for 2003, and so on. We used 2003 Rural Urban Continuum codes to describe the rurality of counties; 1 to 3 denoted urban and 4 to 9 denoted rural.35 County-level estimates were weighted to form region-level estimates for median income, smoking and quit attempt rates, and average Rural Urban Continuum codes for each of the 58 region of residence categories; the weighting was done using annual census estimates for county population size.
Other covariates included physician supply (number of primary care physicians per 100 000) by county36 and comorbidities of heart disease37 and diabetes,38 and we created weighted region-level estimates. Higher levels of primary care physician supply39 and smoking cessation40 may be associated with fewer COPD admissions. Comorbidities may contribute to higher admissions for COPD.
Statistical Methods
Descriptive statistics summarized the patient population. We modeled quarterly rates for COPD hospitalizations over the 8-year study period using Poisson regression, with the negative binomial distribution specified to allow for over- or underdispersion. The regression model included the fixed effects of sex, age (with 3 categories: 45–64, 65–84, and ≥ 85 years), and urban status of region. We developed 2 models, 1 with law strength and the other with law duration; these indicator variables were fixed effects, and we included the interaction between smoking rate and each of the 2 strength variables (comprehensive and moderate–weak) and 2 duration variables (established and new) in each corresponding model. We used the log of the estimated population size as an offset variable in the models, with population estimates specific to the year, sex, and age category of the patients; we included in both models the covariates length of stay, race/ethnicity, education, income, urban–rural status, primary care physician supply, heart disease, diabetes, smoking rate, and quit attempt rate.
The models also contained an indicator for time (i.e., quarter) to assess secular trends unrelated to law implementation; this variable was treated as continuous in the models, with July–September 2003 numbered 1 and April–June 2011 numbered 32. We added 3 indicator variables to the models to account for season of the year (January–March, April–June, July–September; we used October–December as the reference). In addition to including variables to account for secular trends over time and seasonal variations in COPD, we also included region of residence; this factor accounts for population differences among regions in the state that may influence COPD hospitalizations. We determined model goodness of fit using the deviance statistic. Data analyses were conducted using SAS for Windows, version 9.3 (SAS Institute, Cary, NC); we used an α level of .05 throughout.
RESULTS
From July 2003 through June 2011, 146 218 Kentucky residents aged 45 years and older were discharged for COPD from hospitals in the state. As shown in Table 1, the majority of eligible discharges were women (58%) between the ages of 65 and 84 years (53%). The length-of-stay geometric mean was 1.3 days (geometric SD = 0.7). Table 2 provides an overview of the descriptive characteristics of the 58 regions in the state, with region sorted by annual rate of COPD per 10 000 residents aged 45 years and older, ranging from high to low; the range was from 69.8 to 4.9 annual hospitalizations per 10 000 at-risk individuals ages 45 years and older. The regions with the highest COPD rates tended to have higher Rural Urban Continuum codes and higher smoking rates than those with lower COPD rates near the bottom of the table. In addition, counties with smoke-free laws tended to be clustered among the more urban counties with the lowest COPD hospitalization rates. Both Poisson regressions based on the negative binomial distribution fit the data well; the ratio of the deviance statistic to the degrees of freedom was 1.1 for both models, close to the null value of 1. The deviance per degrees of freedom for the analogous model based on the Poisson distribution was approximately twice the size (2.0 for both), underscoring the superior fit of the negative binomial.
TABLE 1—
Sex and Age Distributions of Primary COPD Cases (n = 146 218): Kentucky; July 1, 2003–June 30, 2011
| Demographic Factor | No. (%) |
| Sex | |
| Male | 60 984 (41.7) |
| Female | 85 234 (58.3) |
| Age, y | |
| 45–64 | 59 352 (40.6) |
| 65–84 | 77 996 (53.3) |
| ≥ 85 | 8870 (6.1) |
Note. COPD = chronic obstructive pulmonary disease. Primary COPD cases included all records with primary diagnosis International Classification of Diseases, Ninth Revision29 codes beginning with 491, 492, or 496 that met inclusion criteria.
TABLE 2—
Summary of Region of Residence: Kentucky, July 1, 2003–June 30, 2011
| Counties in Region | No. of Counties in Region | Annual COPD Rate per 10 000 at Risk | Smoke-Free Law Implementation Date | Strength of Smoke-Free Law | Weighted Average RUC code | Weighted Averagea Smoking Rate (%) |
| Breathitt, Owsley, Perry, Wolfe | 4 | 69.8 | 7.4 | 31.6 | ||
| Clay, Leslie | 2 | 49.1 | 7.7 | 33.1 | ||
| Letcher | 1 | 47.6 | July 2006 | Mod–weak | 9.0 | 29.7 |
| Floyd | 1 | 44.9 | November 2009 | Comp | 7.0 | 29.6 |
| Bell, Harlan | 2 | 44.5 | 7.0 | 29.8 | ||
| Lee | 1 | 43.7 | August 2008 | Mod–weak | 9.0 | 35.8 |
| Johnson | 1 | 41.6 | January 2007 | Mod–weak | 7.0 | 24.1 |
| Pike | 1 | 31.6 | November 2007 | Mod–weak | 7.0 | 29.7 |
| Carter, Knott, Lawrence, Martin | 4 | 29.9 | 7.1 | 30.2 | ||
| Metcalfe, Monroe, Wayne | 3 | 27.5 | 8.0 | 28.7 | ||
| Knox | 1 | 24.6 | 7.0 | 28.6 | ||
| Casey, Clinton, Cumberland, Hart, McCreary | 5 | 24.6 | 8.7 | 29.8 | ||
| Jackson, Rockcastle | 2 | 23.4 | 7.9 | 29.2 | ||
| Ballard, Fulton, Graves, Hickman | 4 | 22.4 | 7.5 | 24.0 | ||
| Estill, Magoffin, Powell | 3 | 22.3 | 6.9 | 26.8 | ||
| Caldwell, Crittenden, Livingston, Lyon, Union | 5 | 22.2 | 6.9 | 25.1 | ||
| Henderson | 1 | 20.4 | March 2007 | Mod–weak | 2.0 | 26.6 |
| Boyd | 1 | 19.4 | October 2006 | Comp | 2.0 | 23.3 |
| Bath, Elliott, Menifee, Morgan | 4 | 19.0 | 8.0 | 31.2 | ||
| Grayson, Muhlenberg, Ohio, Todd | 4 | 17.7 | 6.3 | 27.4 | ||
| Allen, Butler, Logan, Simpson | 4 | 17.6 | 6.4 | 26.2 | ||
| McCracken | 1 | 16.9 | April 2007 | Mod–weak | 5.0 | 20.3 |
| Fleming, Lewis | 2 | 16.8 | 7.5 | 28.6 | ||
| Adair, Edmonson, Garrard, Green, Lincoln, Russell | 6 | 16.8 | 6.8 | 28.4 | ||
| Pulaski | 1 | 16.3 | 5.0 | 25.5 | ||
| Breckinridge, Hancock, Larue, Marion, Mercer | 5 | 15.5 | 5.7 | 25.9 | ||
| Christian | 1 | 15.2 | January 2011 | Mod–weak | 3.0 | 25.4 |
| Webster | 1 | 14.9 | 2.0 | 25.1 | ||
| Bourbon, Bracken, Harrison, Nicholas, Pendleton, Robertson | 6 | 14.3 | 3.5 | 26.3 | ||
| Whitley | 1 | 14.3 | 7.0 | 31.2 | ||
| Mason | 1 | 14.1 | 6.0 | 24.1 | ||
| Carroll, Gallatin, Grant, Henry, Owen, Trimble | 6 | 13.8 | 2.7 | 28.2 | ||
| Taylor | 1 | 13.3 | September 2009 | Comp | 7.0 | 25.5 |
| Laurel | 1 | 12.9 | August 2009 | Comp | 7.0 | 28.6 |
| Boyle | 1 | 12.5 | August 2008 | Comp | 7.0 | 19.9 |
| Franklin | 1 | 12.2 | August 2006 | Mod–weak | 4.0 | 24.6 |
| Greenup | 1 | 11.9 | 2.0 | 23.5 | ||
| Carlisle, Calloway, Marshall, Trigg | 4 | 11.8 | 6.5 | 22.2 | ||
| Hardin | 1 | 11.7 | December 2006 | Comp | 3.0 | 23.8 |
| Barren | 1 | 11.3 | June 2010 | Comp | 6.0 | 25.1 |
| Montgomery | 1 | 10.9 | 6.0 | 26.7 | ||
| Hopkins | 1 | 10.7 | February 2009 | Mod–weak | 4.0 | 22.6 |
| Rowan | 1 | 10.4 | August 2006 | Comp | 7.0 | 26.0 |
| Nelson | 1 | 10.1 | June 2010 | Comp | 1.0 | 25.3 |
| Warren | 1 | 9.2 | April 2011 | Comp | 3.0 | 22.7 |
| McLean | 1 | 9.1 | 3.0 | 24.0 | ||
| Jefferson | 1 | 9.1 | November 2005 | Variesb | 1.0 | 22.5 |
| Kenton | 1 | 8.6 | April 2011 | Mod–weak | 1.0 | 25.0 |
| Daviess | 1 | 8.4 | January 2006 | Mod–weak | 3.0 | 21.6 |
| Clark | 1 | 8.2 | January 2009 | Comp | 2.0 | 29.6 |
| Boone, Campbell | 2 | 7.9 | 1.0 | 19.5 | ||
| Anderson, Jefferson, Washington | 3 | 7.8 | 4.0 | 23.6 | ||
| Madison | 1 | 7.4 | June 2007 | Comp | 4.0 | 21.0 |
| Scott | 1 | 7.4 | October 2005 | Comp | 2.0 | 16.6 |
| Bullitt, Meade, Shelby, Spencer | 4 | 7.1 | 1.0 | 27.2 | ||
| Woodford | 1 | 5.5 | August 2008 | Comp | 2.0 | 17.1 |
| Oldham | 1 | 5.1 | May 2007 | Mod–weak | 1.0 | 16.3 |
| Fayette | 1 | 4.9 | April 2004 | Variesc | 2.0 | 17.1 |
Note. Comp = comprehensive; COPD = chronic obstructive pulmonary disease; Mod–weak = moderate–weak; RUC = rural–urban continuum.
Weighted averages were determined using population estimates of the counties included in the region.
Moderate–weak, then strengthened to comprehensive starting July 2007.
Moderate–weak, then strengthened to comprehensive starting November 2008.
Adjusting for all patient characteristics, population covariates, and seasonal and trend factors, the relative risk of a COPD hospitalization in communities with comprehensive smoke-free policies was 0.781 compared with communities having moderate–weak laws or no laws restricting smoking in public places (χ2 = 6.65, P = .01; 95% confidence interval = 0.647, 0.942; Table 3). For the second model, used to test the effect of duration of law on COPD exacerbations, the relative risk of a COPD hospitalization in communities with established laws was 0.789 compared with communities with new or no laws (χ2 = 9.91, P = .002; 95% confidence interval = 0.680, 0.914). In both models, the protective factors for decreased risk of COPD hospitalization were being male, being younger (45–64 years), and living in a community with higher levels of postsecondary education. Conversely, those living in areas with a larger percentage of Hispanics and those with more primary care physicians were at greater risk of experiencing a COPD exacerbation leading to hospitalization.
TABLE 3—
Negative Binomial Regressions for Primary COPD Hospitalization Cases Among Patients Aged 45 Years or Older: Kentucky, July 1, 2003–June 30, 2011
| With Strength of Law |
With Duration of Law |
|||
| Variable | RR (95% CI) | P | RR (95% CI) | P |
| Personal characteristics | ||||
| Sex | ||||
| Male | 0.893 (0.878, 0.908) | < .001 | 0.893 (0.878, 0.908) | < .001 |
| Female | … | … | … | … |
| Age, y | ||||
| 45–64 | 0.392 (0.380, 0.404) | < .001 | 0.392 (0.380, 0.404) | < .001 |
| 65–84 | 1.217 (1.184, 1.251) | < .001 | 1.217 (1.184, 1.251) | < .001 |
| ≥ 85 | … | … | … | … |
| Log of length of stay | 0.823 (0.771, 0.879) | < .001 | 0.826 (0.774, 0.882) | < .001 |
| Regional characteristics | ||||
| Percentage Hispanic | 1.524 (1.248, 1.861) | < .001 | 1.524 (1.248, 1.861) | < .001 |
| Percentage of adults with any postsecondary education | 0.682 (0.559, 0.832) | < .001 | 0.682 (0.559, 0.832) | < .001 |
| Median incomea | 0.968 (0.900, 1.040) | .4 | 0.969 (0.901, 1.042) | .4 |
| Urban | 2.808 (0.381, 20.688) | .3 | 2.825 (0.384, 20.810) | .3 |
| Primary care provider supply | 1.026 (1.013, 1.039) | < .001 | 1.026 (1.013, 1.039) | < .001 |
| Heart disease rate | 0.772 (0.689, 0.866) | < .001 | 0.770 (0.687, 0.864) | < .001 |
| Diabetes rate | 7.013 (4.671, 10.527) | < .001 | 7.031 (4.685, 10.552) | < .001 |
| Adult smoking rateb | 0.998 (0.992, 1.004) | .5 | 0.998 (0.992, 1.004) | .5 |
| Quit attempt rate | 1.002 (1.000, 1.003) | .1 | 1.001 (1.000, 1.003) | .1 |
| Quarter of year | ||||
| January–March | 1.186 (1.160, 1.213) | < .001 | 1.186 (1.160, 1.213) | < .001 |
| April–June | 0.942 (0.921, 0.964) | < .001 | 0.943 (0.922, 0.965) | < .001 |
| July–Sept | 0.790 (0.771, 0.809) | < .001 | 0.790 (0.772, 0.809) | < .001 |
| October–December | … | … | … | … |
| Time (quarter number) | 1.001 (1.000, 1.003) | .1 | 1.001 (0.999, 1.002) | .3 |
| Comprehensive law | 0.781 (0.647, 0.942) | .01 | … | … |
| Moderate–weak law | 0.883 (0.753, 1.035) | .1 | … | … |
| Established law (≥ 12 mo) | … | … | 0.789 (0.680, 0.914) | .002 |
| New law (< 12 mo) | … | … | 0.847 (0.678, 1.058) | .1 |
| Comprehensive × smoking rate | 1.010 (1.002, 1.019) | .01 | … | … |
| Moderate–weak × smoking rate | 1.003 (0.997, 1.010) | .4 | … | … |
| Established law × smoking rate | … | … | 1.010 (1.004, 1.017) | .001 |
| New law × smoking rate | … | … | 1.003 (0.995, 1.012) | .5 |
Note. CI = confidence interval; COPD = chronic obstructive pulmonary disease; RR = relative risk. Fifty-seven indicators for region of residence were included in the model.
Weighted median income in $1000s for region of residence from 2009 US Census.
Weighted 3-year aggregate adult smoking rate for region of residence from Behavioral Risk Factor Surveillance System.
DISCUSSION
Controlling for personal and population factors, those living in a community with a comprehensive smoke-free law or regulation were 22% less likely to experience hospitalization for COPD than those living in a community with a moderate–weak law or without a law. Moreover, those living in a community with an established law (in place for > 12 mo) were 21% less likely to have a COPD hospitalization than those in communities with new laws (< 12 months) or no laws. The effect of smoke-free laws on COPD is more subtle than for some other diseases and may take longer to be significant.21 A smoke-free law in Prince Edward Island, Canada, did not result in reduced hospitalization rates for COPD, but this finding may have been attributable to the limited time period postlaw as well as the rural nature of the area, limiting residents’ exposure to public places covered by the law.23 By contrast, the smoke-free law in Beaumont, Texas, resulted in a 36% decline in COPD exacerbation hospitalizations among Whites only.22 Similarly, a 38% reduction in COPD mortality occurred after Ireland’s comprehensive smoke-free workplace law, but only among women.41 A meta-analysis conducted on the relationship between smoke-free legislation and hospital admissions found a decreased risk for respiratory diseases.20
Smoke-free public policies, particularly when they are comprehensive and have been in place for at least 1 year, may provide protection against exacerbations of COPD that lead to hospitalizations, with potential to save lives and decrease health care costs. The results of this research support previous findings that respiratory health improves as a result of smoke-free laws. In a previous study, the investigators reported a 22% decline in emergency visits for asthma after enactment in Lexington, Kentucky, of a smoke-free law covering all enclosed public places.42 Hahn et al. also found a 56% drop in hair nicotine levels in a sample of smoking and nonsmoking bar and restaurant workers after Lexington implemented a smoke-free law.43 Smoking and nonsmoking workers were less likely to report colds and sinus infections after the law went into effect.
Kentucky, with a long history of tobacco production, has relatively high smoking rates, in part because of weak state tobacco control laws.44 Tobacco has been 1 of the most important forces in the state economy and is a cultural icon. Tobacco is grown in 117 of 120 Kentucky counties,45 and the state produced 24.4% of all tobacco grown in the United States in 2007.46 Slightly more than half of Kentuckians live in these rural farming areas and have a lower per capita income than those in urban areas ($18 161 vs $23 555).34,47 Rural residents are less likely than their urban counterparts to restrict smoking at home, work, or public places, for the most part because of socioeconomic disparities.48 Given that such a high percentage of Kentuckians live in at-risk rural areas and lack the protective factor of income or smoke-free laws, the state faces a higher risk of COPD.
Limitations
First, we used county groups because some counties within Kentucky are very small, and they have very few COPD hospitalizations. Second, not all cases of COPD in the state may have been included in the data set. Patients may have died before reaching the hospital or those residing in Kentucky may have gone to a hospital in another state. Moreover, we did not have the ability to link cases to each other so we were unable to examine short-term readmissions. Third, case-specific smoking status would have been preferable over region-specific smoking rate, but these data were unavailable. Fourth, counties were considered smoke-free even if the entire county was not covered by a law (i.e., if a city within a county was smoke-free, we counted the entire county as smoke-free). Fifth, we were unable to control for environmental air quality, a risk factor for COPD, because these data were unavailable. Sixth, we were unable to simultaneously consider both strength and duration of law in a single model because of the relatively small number of community laws with combinations of strength and duration categories (e.g., comprehensive or established). Finally, adherence to (e.g., enforcement of) smoke-free laws may have more to do with population health outcomes than simply measuring existence of the law, which was beyond the scope of our study. Research is needed on adherence to smoke-free laws and impact on population health outcomes such as hospitalization for COPD.
Implications for Public Health
Policy outcomes research is needed to empower advocates and policymakers to enact healthy public policy. Health policy change creates a built environment in which the healthy choice is the easy choice.49,50 Policy change can be influenced by translating and disseminating research findings to the public, policymakers, and key health leaders. Our study found that comprehensive smoke-free policies can contribute to better health outcomes for COPD, which can in turn negate the risk factors of lower socioeconomic status that many living in rural, tobacco-growing communities face.
Acknowledgments
This work was supported by the Flight Attendant Medical Research Institute.
Human Participant Protection
This study was approved by the University of Kentucky Medical institutional review board.
References
- 1.Tetley TD. Inflammatory cells and chronic obstructive pulmonary disease. Curr Drug Targets Inflamm Allergy. 2005;4(6):607–618. doi: 10.2174/156801005774912824. [DOI] [PubMed] [Google Scholar]
- 2.Woodruff PG, Ellwanger A, Solon M, Cambier CJ, Pinkerton KG, Koth LL. Alveolar macrophage recruitment and activation by chronic second hand smoke exposure in mice. COPD. 2009;6(2):86–94. doi: 10.1080/15412550902751738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roth M. Pathogenesis of COPD. Part III. Inflammation in COPD. Int J Tuberc Lung Dis. 2008;12(4):375–380. [PubMed] [Google Scholar]
- 4.Mannino DM, Homa DM, Akinbami LJ, Ford ES, Redd SC. Chronic obstructive pulmonary disease surveillance—United States, 1971-2000. Respir Care. 2002;47(10):1184–1199. [PubMed] [Google Scholar]
- 5.Tsai CL, Clark S, Cydulka RK, Rowe BH, Camargo CA. Factors associated with hospital admission among emergency department patients with chronic obstructive pulmonary disease exacerbation. Acad Emerg Med. 2007;14(1):6–14. doi: 10.1197/j.aem.2006.07.034. [DOI] [PubMed] [Google Scholar]
- 6.Barr RG, Celli BR, Mannino DM et al. Comorbidities, patient knowledge, and disease management in a national sample of patients with COPD. Am J Med. 2009;122(4):348–355. doi: 10.1016/j.amjmed.2008.09.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Omachi TA, Katz PP, Yelin EH et al. Depression and health-related quality of life in chronic obstructive pulmonary disease. Am J Med. 2009;122(8):778.e9–778.e15. doi: 10.1016/j.amjmed.2009.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garcia-Aymerich J, Serra I, Gómez FP et al. Phenotype and Course of COPD Study Group. Physical activity and clinical and functional status in COPD. Chest. 2009;136(1):62–70. doi: 10.1378/chest.08-2532. [DOI] [PubMed] [Google Scholar]
- 9.Hung WW, Wisnivesky JP, Siu AL, Ross JS. Cognitive decline among patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2009;180(2):134–137. doi: 10.1164/rccm.200902-0276OC. [DOI] [PubMed] [Google Scholar]
- 10.Dalal AA, Christensen L, Liu F, Riedel AA. Direct costs of chronic obstructive pulmonary disease among managed care patients. Int J Chron Obstruct Pulmon Dis. 2010;5:341–349. doi: 10.2147/COPD.S13771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. American Thoracic Society. COPD will cost US $800+ billion over next 20 years, study predicts. 2009. Available at: http://www.thoracic.org/sections/publications/press-releases/conference/articles/2006/press-releases/copd-will-cost-us-800-billion-over-next-20-years-study-predicts.html. Accessed August 1, 2009.
- 12.Buist AS, McBurnie MA, Vollmer WM et al. BOLD Collaborative Research Group. International variation in the prevalence of COPD (the BOLD Study): a population-based prevalence study. Lancet. 2007;370(9589):741–750. doi: 10.1016/S0140-6736(07)61377-4. [DOI] [PubMed] [Google Scholar]
- 13.Methvin JN, Mannino DM, Casey BR. COPD prevalence in southeastern Kentucky: the burden of lung disease study. Chest. 2009;135(1):102–107. doi: 10.1378/chest.08-1315. [DOI] [PubMed] [Google Scholar]
- 14.Jemal A, Ward E, Hao Y, Thun M. Trends in the leading causes of death in the United States, 1970-2002. JAMA. 2005;294(10):1255–1259. doi: 10.1001/jama.294.10.1255. [DOI] [PubMed] [Google Scholar]
- 15.Miniño AM, Murphy SL, Xu J, Kochanek KD. Deaths: final data for 2008. Natl Vital Stat Rep. 2011;59(10):1–126. [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Chronic obstructive pulmonary disease among adults–United States, 2011. MMWR Morb Mortal Wkly Rep. 2012;61(46):938–943. [PubMed] [Google Scholar]
- 17. Centers for Disease Control and Prevention. Prevalence and trends data, Kentucky—2007: tobacco use. Available at: http://apps.nccd.cdc.gov/brfss/page.asp?yr=2007&state=KY&cat=TU#TU. Accessed March 16, 2009.
- 18.Jones KL. Kentucky Youth Tobacco Survey 2006. Frankfort, KY: Kentucky Department for Public Health, Tobacco Prevention and Cessation Program; 2006. [Google Scholar]
- 19. Kentucky Center for Smoke-Free Policy. Smoke-free ordinances and regulations in Kentucky. Available at: http://www.mc.uky.edu/TobaccoPolicy/KCSP. Accessed December 1, 2013.
- 20.Tan CE, Glantz SA. Association between smoke-free legislation and hospitalizations for cardiac, cerebrovascular, and respiratory diseases: a meta-analysis. Circulation. 2012;126(18):2177–2183. doi: 10.1161/CIRCULATIONAHA.112.121301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vander Weg MW, Rosenthal GE, Vaughan Sarrazin M. Smoking bans linked to lower hospitalizations for heart attacks and lung disease among Medicare beneficiaries. Health Aff (Millwood) 2012;31(12):2699–2707. doi: 10.1377/hlthaff.2011.0385. [DOI] [PubMed] [Google Scholar]
- 22.Head P, Jackson BE, Bae S, Cherry D. Hospital discharge rates before and after implementation of a city-wide smoking ban in a Texas city, 2004–2008. Prev Chronic Dis. 2012;9:E179. doi: 10.5888/pcd9.120079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gaudreau K, Sanford CJ, Cheverie C, McClure C. The effect of a smoking ban on hospitalization rates for cardiovascular and respiratory conditions in Prince Edward Island, Canada. PLoS ONE. 2013;8(3):e56102. doi: 10.1371/journal.pone.0056102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Greathouse LW, Hahn EJ, Okoli CT, Warnick TA, Riker CA. Passing a smoke-free law in a pro-tobacco culture: a multiple streams approach. Policy Polit Nurs Pract. 2005;6(3):211–220. doi: 10.1177/1527154405278775. [DOI] [PubMed] [Google Scholar]
- 25.Leon-Chisen N. Faye Brown’s ICD-9-CM Coding Handbook with Answers. Chicago, IL: AHA Press; 2010. [Google Scholar]
- 26.Hahn EJ, Rayens MK, Langley RE, Darville A, Dignan M. Time since smoke-free law and smoking cessation behaviors. Nicotine Tob Res. 2009;11(8):1011–1015. doi: 10.1093/ntr/ntp086. [DOI] [PubMed] [Google Scholar]
- 27.Faustini A, Stafoggia M, Cappai G, Forastiere F. Short-term effects of air pollution in a cohort of patients with chronic obstructive pulmonary disease. Epidemiology. 2012;23(6):861–879. doi: 10.1097/EDE.0b013e31826767c2. [DOI] [PubMed] [Google Scholar]
- 28.Blanchette CM, Dalal AA, Mapel D. Changes in COPD demographics and costs over 20 years. J Med Econ. 2012;15(6):1176–1182. doi: 10.3111/13696998.2012.713880. [DOI] [PubMed] [Google Scholar]
- 29.International Classification of Diseases, Ninth Revision. Geneva, Switzerland: World Health Organization; 1980. [Google Scholar]
- 30.Christian WJ, Huang B, Rinehart J, Hopenhayn C. Exploring geographic variation in lung cancer incidence in Kentucky using a spatial scan statistic: elevated risk in the Appalachian coal-mining region. Public Health Rep. 2011;126(6):789–796. doi: 10.1177/003335491112600604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pyles MK, Hahn EJ. Economic effects of smoke-free laws on rural and urban counties in Kentucky and Ohio. Nicotine Tob Res. 2012;14(1):111–115. doi: 10.1093/ntr/ntr123. [DOI] [PubMed] [Google Scholar]
- 32.Fernander AF, Rayens MK, Adkins S, Hahn EJ. Local smoke-free public policies, quitline call rate, and smoking status in Kentucky. Am J Health Promot. 2014 doi: 10.4278/ajhp.121129-QUAN-578. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cortes-Bergoderi M, Goel K, Murad MH et al. Cardiovascular mortality in Hispanics compared to non-Hispanic Whites: a systematic review and meta-analysis of the Hispanic paradox. Eur J Intern Med. 2013;24(8):791–799. doi: 10.1016/j.ejim.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 34. U.S. Census Bureau, 2010 Census of Population and Housing, Summary Population and Housing Characteristics CPH-1-19, Washington, DC: Kentucky U.S. Government Printing Office; 2012.
- 35.US Department of Agriculture, Economic Research Service. Rural-Urban Continuum Codes. Washington, DC: Economic Research Service; 2003. [Google Scholar]
- 36.Health Resources and Services Administration. Health Professions: Primary Care Physicians/100K Population, Kentucky. Washington, DC: US Department of Health and Human Services; 2011. [Google Scholar]
- 37. Centers for Disease Control and Prevention, Division for Heart Disease and Stroke Prevention. Interactive atlas of heart disease and stroke tables, Kentucky, 2008-2010. Available at: http://nccd.cdc.gov/dhdspatlas/reports.aspx. Accessed November 27, 2013.
- 38. National Center for Chronic Disease Prevention and Health Promotion Division of Diabetes Translation. Diagnosed diabetes prevalence. 2004-2009. Available at: http://www.cdc.gov/diabetes/atlas/countydata/County_EXCELstatelistDM.html. Accessed November 21, 2013.
- 39.Laditka JN, Laditka SB, Probst JC. More may be better: evidence of a negative relationship between physician supply and hospitalization for ambulatory care sensitive conditions. Health Serv Res. 2005;40(4):1148–1166. doi: 10.1111/j.1475-6773.2005.00403.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kabir Z, Connolly GN, Koh HK, Clancy L. Chronic obstructive pulmonary disease hospitalization rates in Massachusetts: a trend analysis. QJM. 2010;103(3):163–168. doi: 10.1093/qjmed/hcp190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stallings-Smith S, Zeka A, Goodman P, Kabir Z, Clancy L. Reductions in cardiovascular, cerebrovascular, and respiratory mortality following the national Irish smoking ban: interrupted time-series analysis. PLoS ONE. 2013;8(4):e62063. doi: 10.1371/journal.pone.0062063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rayens MK, Burkhart PV, Zhang M et al. Reduction in asthma-related emergency department visits after implementation of a smoke-free law. J Allergy Clin Immunol. 2008;122(3):537–541.e3. doi: 10.1016/j.jaci.2008.06.029. [DOI] [PubMed] [Google Scholar]
- 43.Hahn EJ, Rayens MK, York N et al. Effects of a smoke-free law on hair nicotine and respiratory symptoms in restaurant and bar workers. J Occup Environ Med. 2006;48(9):906–913. doi: 10.1097/01.jom.0000215709.09305.01. [DOI] [PubMed] [Google Scholar]
- 44.Chaloupka F, Hahn E, Emery S. Policy levers for the control of tobacco consumption. KY Law J. 2002;90(4):1009–1042. [Google Scholar]
- 45.US Department of Agriculture. Kentucky Tobacco Facts. Washington, DC: National Agricultural Statistics Service; 2007. [Google Scholar]
- 46.US Department of Agriculture. Crop and Plants: Tobacco (All Classes) Washington, DC: National Agricultural Statistics Service; 2007. [Google Scholar]
- 47. US Bureau of the Census. 2007-2011 American Community Survey, 5-year estimates. Available at: https://www.census.gov/acs/www/data_documentation/2011_release. Accessed July 12, 2013.
- 48.McMillen R, Breen J, Cosby A. Rural-urban differences in the social climate surrounding environmental tobacco smoke: a report from the 2002 social climate survey of tobacco control. J Rural Health. 2004;20(1):7–16. doi: 10.1111/j.1748-0361.2004.tb00002.x. [DOI] [PubMed] [Google Scholar]
- 49. The Lancet Oncology. Healthy choice should be the easy choice. Lancet Oncol. 2012;13(8):743. [DOI] [PubMed]
- 50.Ashe M, Graff S, Spector C. Changing places: policies to make a healthy choice the easy choice. Public Health. 2011;125(12):889–895. doi: 10.1016/j.puhe.2011.04.010. [DOI] [PubMed] [Google Scholar]