Abstract
Objectives. We examined sexual orientation differences in adolescent smoking and intersections with race/ethnicity, gender, and age.
Methods. We pooled Youth Risk Behavior Survey data collected in 2005 and 2007 from 14 jurisdictions; the analytic sample comprised observations from 13 of those jurisdictions (n = 64 397). We compared smoking behaviors of sexual minorities and heterosexuals on 2 dimensions of sexual orientation: identity (heterosexual, gay–lesbian, bisexual, unsure) and gender of lifetime sexual partners (only opposite sex, only same sex, or both sexes). Multivariable regressions examined whether race/ethnicity, gender, and age modified sexual orientation differences in smoking.
Results. Sexual minorities smoked more than heterosexuals. Disparities varied by sexual orientation dimension: they were larger when we compared adolescents by identity rather than gender of sexual partners. In some instances race/ethnicity, gender, and age modified smoking disparities: Black lesbians–gays, Asian American and Pacific Islander lesbians–gays and bisexuals, younger bisexuals, and bisexual girls had greater risk.
Conclusions. Sexual orientation, race/ethnicity, gender, and age should be considered in research and practice to better understand and reduce disparities in adolescent smoking.
Cigarette smoking continues to be the leading cause of preventable morbidity and premature mortality in the United States.1,2 Preventing adolescent smoking is essential to reducing the burden of cigarettes because smoking typically begins during adolescence.3,4 Approximately 88% of adult daily smokers began smoking before their 18th birthday.5 Research has shown that adolescents with a minority sexual orientation (i.e., lesbian, gay, and bisexual [LGB] youths and other adolescents who report same-sex attractions or behavior) are more likely than heterosexual adolescents to smoke cigarettes.6–12 In addition to variation in adolescent smoking by sexual orientation, research has documented variation by race/ethnicity, gender, and age–developmental period.13–17 For instance, national data from the United States collected in 2009 found that White (19.4%) and Hispanic (19.1%) high school students reported higher prevalence of current smoking than Asian (9.7%) and Black (9.1%) students.18 Risk for smoking is typically higher in male than female adolescents and in older than younger adolescents.16,19
Although research has shown how sexual orientation, race/ethnicity, gender, and age separately influence variations in adolescent smoking, limited data exist on how sexual orientation differences in adolescent smoking vary across sociodemographic factors such as race/ethnicity, gender, and age. A report published in 2011 by the Institute of Medicine, The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding, argued for the importance of examining the health of sexual minorities in the context of sociodemographic diversity to provide a more complete understanding of health disparities.20 Empirical evidence of this nature can improve understanding of the burden of smoking in specific population subgroups and identify high-risk subgroups to target for research, prevention, and cessation efforts.
Existing research to understand how smoking patterns of sexual minority youths vary across gender, age, and race/ethnicity is inconclusive and sometimes contradictory. In addition, few studies have used large, representative samples, which limits the ability to draw inferences about the entire population of sexual minority youths.21 Studies examining how sexual orientation differences in adolescent smoking vary by gender have been the most conclusive and have typically found larger disparities between sexual minority and heterosexual adolescent girls than between sexual minority and heterosexual adolescent boys.6,9,22,23 However, studies examining how sexual orientation differences in adolescent smoking vary by age have been inconclusive. One study of mostly White youths followed between ages 12 and 24 years found that smoking disparities were larger between sexual minorities and heterosexuals during younger than older ages.6 However, a study of Asian Americans and Pacific Islanders (APIs) found that smoking disparities were not present in adolescence but emerged in young adulthood.9
In addition, scant data exist on how sexual orientation and race/ethnicity jointly influence risk for adolescent smoking. This is an especially difficult area to investigate because studies with a sample size large enough to examine this question are rare. Some evidence suggests that sexual minority youths who belong to racial/ethnic minority groups are more likely to smoke cigarettes than their heterosexual peers of their same race/ethnicity. For instance, a study of college students found that Black, Asian, Hispanic, and multiracial LGB persons were more likely to smoke than their heterosexual racial/ethnic peers.24 This study also found that Black and Asian LGB persons were less likely to smoke than their White LGB peers, but the same was not true for Hispanics and multiracial LGB persons. However, the study did not describe statistical testing to examine whether race/ethnicity modified sexual orientation disparities in smoking.
Another important consideration is the multidimensional nature of sexual orientation (e.g., identity, attractions, behaviors), which in research with adolescents has most often been assessed as how respondents identify or the gender of their sexual attractions or partners. How sexual orientation is operationalized in studies may influence findings and conclusions, but studies infrequently include more than 1 dimension. Studies with adults12,25–27 and adolescents10,23,28 have shown differences in the magnitude of the sexual orientation disparities observed depending on which dimension is considered. For example, a study of Mexican youths aged 18 to 29 years found that self-identified LGB participants had approximately twice the odds of reporting current smoking than did heterosexuals, but differences between participants reporting only same-sex partners and those reporting only opposite-sex partners were negligible.23 Such disparate findings are likely to occur because the dimensions capture somewhat different populations with differing risk and protective factors.29
It is especially important to assess multiple dimensions of sexual orientation in adolescence because a same-sex orientation commonly develops during this period, and many adolescents with a same-sex orientation may not identify as LGB.30 In addition, when gender of sexual partners is used as an indicator of sexual orientation, only adolescents who have initiated sexual intercourse (approximately 48% of high school students in 200719) can be identified. Because adolescent smoking is a robust correlate of sexual activity,31 the degree to which the selection of a sexually active subgroup may influence sexual orientation findings warrants consideration. Finally, the extent to which the different dimensions may affect conclusions drawn about smoking disparities arising from sexual orientation when also considering intersections with race/ethnicity, gender, and age remain uncertain. To address these questions, we compared sexual orientation differences in smoking during adolescence with 2 dimensions of sexual orientation (identity and gender of lifetime sexual partners) and investigated how these differences were modified by race/ethnicity, gender, and age in Youth Risk Behavior Survey (YRBS) data pooled from 13 jurisdictions and 2 years.
METHODS
The YRBS is conducted biennially in high schools across the United States. A 2-stage, cluster sampling design is used to generate a representative sample of students in grades 9 through 12 in each jurisdiction in which the survey is administered. We pooled YRBS data collected in 2005 and 2007 from 14 jurisdictions. The analytic sample included observations from the 13 jurisdictions that asked questions on sexual orientation identity or gender of lifetime sexual partners (Boston, MA; Chicago, IL; Connecticut; Delaware; Maine; Massachusetts; Milwaukee, WI; New York City, NY; Rhode Island; San Diego, CA; San Francisco, CA; Vermont; and Wisconsin). Additional information about the characteristics of each jurisdiction and the procedures for pooling data are available elsewhere.32
We analyzed data from respondents aged 13 years or older who answered 1 or more questions about their sexual orientation identity or the gender of their lifetime sexual partners. After we excluded the few participants who were younger than 13 years and those who could not be classified on their sexual orientation, the unweighted analytic sample was 64 397. Of these participants, 58 319 (weighted percentage = 90.2%) were heterosexual and 6067 (weighted percentage = 9.8%) were sexual minority (i.e., LBG, unsure of sexual orientation identity, or reported same-sex or both-sex partners).
Measures
Sexual orientation.
We used 2 sexual orientation measures. We assessed sexual orientation identity with the question, “Which of the following best describes you?” Response options were heterosexual, gay or lesbian, bisexual, and unsure. We assessed self-reported gender of lifetime sexual partners with the question, “During your life, with whom have you had sexual contact?” (Some questionnaires used “intercourse” in place of “contact.”) Response options were never had sexual contact, females, males, and females and males. We used this question and participants’ self-reported gender to create a sexual orientation indicator with 3 categories: opposite-sex partners only, same-sex partners only, and both-sex partners. Only individuals who reported sexual partners were able to be classified on their sexual orientation with the gender of sexual partners variable, but the sexual orientation identity variable included all respondents who answered the identity question regardless of whether they reported sexual partners.
Smoking.
We evaluated 5 smoking variables. The survey asked, “How old were you when you smoked a whole cigarette for the first time?” Response options were never smoked a whole cigarette, 8 years or younger, 9 or 10 years, 11 or 12 years, 13 or 14 years, 15 or 16 years, and 17 years or older. We dichotomized ever smoked a whole cigarette into never versus ever smoked. We categorized age at first smoking cigarettes in accordance with methods necessary for survival analysis. We censored students who had not smoked a whole cigarette at their current age. Coding for the other response options was 7.5 for the 8 years or younger response, the midpoint for the responses spanning 2 years (e.g., 9.5 for the 9–10 years category), and 17.5 for the 17 years or older response. To assess whether participants had ever smoked daily, we used the question, “Have you ever smoked cigarettes daily, that is, at least one cigarette every day for 30 days.”
We calculated number of cigarettes smoked in the past 30 days by multiplying responses from questions assessing number of days when respondents smoked and number of cigarettes smoked per day. We assessed number of days smoked with the question, “During the past 30 days, on how many days did you smoke cigarettes?” Response options were 0, 1 or 2, 3 to 5, 6 to 9, 10 to 19, 20 to 29, and all 30 days. We assessed number of cigarettes smoked per day with the question, “During the past 30 days, on the days you smoked, how many cigarettes did you smoke per day?” Response options were did not smoke cigarettes during the past 30 days and less than 1 (coded as 0.5), 1, 2 to 5, 6 to 10, 11 to 20, and more than 20 cigarettes per day. We first assigned midpoint values to categories with ranges (e.g., 1.5 for the 1- or 2-day response option). We then multiplied the 2 values to get a continuous measure of the total number of cigarettes smoked (range = 0.8–630; mean = 95.6; SE = 2.6).
Covariates.
Variables for examining statistical interactions with sexual orientation were age (13–18 years or older); race/ethnicity, coded as non-Hispanic White, non-Hispanic Black, Hispanic, API, or other (which included non-Hispanic multiracial and American Indian/Alaskan Native, collapsed because of small sample sizes); and gender (male vs female).
Statistical Analyses
Descriptive analyses compared percentages and means of the smoking variables by the 2 sexual orientation dimensions and the intersecting factors of race/ethnicity, gender, and age. We examined sexual orientation identity and gender of sexual partners in separate analyses because 5 of the 13 jurisdictions assessed only 1 dimension, and we wanted to use all available data. For age at first smoking, we generated cumulative incidence plots. We used multivariable regression models to estimate the main effects of sexual orientation and the interactive effects of sexual orientation with race/ethnicity, gender, and age. For age at first smoking, we used Cox proportional hazards regression to estimate hazard ratios (HRs). For binary variables (ever smoking, ever smoking daily, smoking in the past month), we used logistic regression to estimate odds ratios (ORs). For number of cigarettes smoked in the past month, which was continuous, we used linear regression to estimate unstandardized regression parameters. We restricted analyses estimating the number of cigarettes smoked in the past month to adolescents who reported smoking in the past month. We included age at first sexual intercourse in the multivariable statistical models to evaluate associations between gender of sexual partners and the smoking variables because of the potential confounding effects of general sexual activity.
To account for the YRBS sampling design and for the pooling of data across 13 locations and 2 years, we performed analyses with SAS-callable SUDAAN version 11.0.1 (Research Triangle Institute, Research Triangle Park, NC), a software program that uses Taylor series linearization to adjust for design effects of complex sample surveys. Analyses took into account all stages of clustering (location, year, stratum, and primary sampling unit). We applied sample weights to all analyses. We estimated confidence intervals (CIs) with 95% certainty. We excluded approximately 14.5% of the sample because respondents' sexual orientation could not be classified.
In any particular analysis, we excluded participants if they were missing data on covariates or smoking variables, either because they did not answer a question or because it was not asked in a particular jurisdiction. Missing data from unanswered questions were generally minimal and ranged from 0.6% for age to 5.4% for age at first smoking. Sexual minority youths (8.4%) were more likely than sexual majority youths (5.3%), adolescent boys (6.2%) were more likely than adolescent girls (4.6%), and racial/ethnic minorities (Blacks = 8.5%; Hispanics = 7.4%; APIs = 6.5%) were more likely than Whites (3.1%) not to report their age at first smoking (all, P < .001). Those who did not answer the age at first smoking question were less likely than other respondents to report that they smoked in the past month (P < .001); this association was similar for heterosexuals and sexual minorities.
RESULTS
Table 1 displays the weighted percentages, means, and standard errors of the smoking variables in the overall sample and by subgroups according to race/ethnicity, gender, and age across the 2 sexual orientation measures. In the vast majority of cases, smoking was more prevalent among sexual minorities than heterosexuals both overall and across race/ethnicity, gender, and age subgroups.
TABLE 1—
Smoking Variables Across Sexual Orientation Dimensions Overall and by Race/Ethnicity, Gender, and Age: Youth Risk Behavior Survey, United States, 2005 and 2007
| Sexual Orientation Identity |
Gender of Lifetime Sexual Partners |
||||||
| Variable | Heterosexual | Lesbian/Gay | Bisexual | Unsure | Opposite Sex Only | Same Sex Only | Both Sexes |
| Ever smoked a whole cigarette | |||||||
| Total, no. | 51 613 | 664 | 1992 | 1421 | 28 120 | 1057 | 1921 |
| Total, % (SE) | 31.9 (0.6) | 59.8 (3.8) | 62.0 (1.8) | 36.4 (2.5) | 44.6 (0.7) | 55.7 (2.4) | 68.6 (1.9) |
| Race/ethnicity, % (SE) | |||||||
| API | 21.5 (1.3) | 66.9 (7.4) | 65.8 (6.2) | 22.7 (4.6) | 44.0 (2.3) | 68.6 (7.7) | 64.5 (8.3) |
| Black | 23.4 (0.9) | 61.2 (7.9) | 47.8 (4.4) | 37.3 (7.4) | 30.1 (1.1) | 39.6 (5.2) | 47.6 (5.1) |
| Hispanic | 34.6 (1.1) | 62.4 (6.7) | 62.5 (3.4) | 43.5 (4.5) | 45.2 (1.3) | 51.8 (4.9) | 71.5 (3.0) |
| Other | 31.4 (1.9) | 46.1 (13.2) | 66.1 (8.5) | 26.1 (8.6) | 45.7 (2.3) | 62.4 (8.7) | 58.2 (8.6) |
| White | 36.1 (0.9) | 57.4 (6.5) | 67.3 (2.8) | 38.7 (3.6) | 50.0 (0.9) | 64.8 (3.3) | 75.1 (2.2) |
| Gender, % (SE) | |||||||
| Female | 30.5 (0.7) | 64.4 (5.0) | 65.6 (2.1) | 33.7 (3.1) | 44.7 (0.9) | 55.6 (3.4) | 72.2 (2.0) |
| Male | 33.3 (0.7) | 57.1 (5.1) | 50.1 (3.9) | 39.1 (3.8) | 44.5 (0.8) | 55.7 (3.2) | 57.7 (3.6) |
| Age, y, % (SE) | |||||||
| 13 | NA | NA | NA | NA | NA | NA | NA |
| 14 | 20.3 (1.1) | 45.0 (11.4) | 58.1 (5.6) | 25.6 (6.1) | 36.8 (1.9) | 47.9 (9.0) | 59.2 (8.6) |
| 15 | 27.5 (0.9) | 55.4 (7.6) | 61.1 (3.7) | 36.0 (4.7) | 39.9 (1.2) | 51.6 (5.1) | 63.3 (3.8) |
| 16 | 34.2 (0.9) | 62.2 (6.8) | 59.3 (3.6) | 36.3 (4.6) | 44.8 (1.1) | 52.9 (4.6) | 65.2 (3.2) |
| 17 | 36.9 (0.9) | 58.6 (6.0) | 63.5 (3.8) | 39.0 (5.7) | 46.8 (1.0) | 63.4 (4.4) | 72.8 (3.1) |
| ≥ 18 | 40.9 (1.5) | 69.1 (9.6) | 73.5 (5.1) | 42.4 (7.0) | 50.5 (1.5) | 57.7 (6.2) | 82.6 (3.7) |
| Smoked in the past month | |||||||
| Total, no. | 52803 | 655 | 1961 | 1437 | 28455 | 1020 | 1903 |
| Total, % (SE) | 13.7 (0.4) | 33.1 (3.5) | 40.2 (2.0) | 17.9 (1.9) | 21.7 (0.5) | 29.6 (2.1) | 49.6 (2.1) |
| Race/ethnicity, % (SE) | |||||||
| API | 7.6 (0.8) | 36.6 (10.1) | 37.3 (7.1) | 12.9 (4.1) | 19.9 (1.9) | 33.3 (9.8) | 47.1 (9.0) |
| Black | 6.8 (0.6) | 17.3 (5.7) | 21.9 (4.4) | 7.5 (2.9) | 9.5 (0.8) | 15.8 (4.0) | 25.1 (4.7) |
| Hispanic | 11.6 (0.6) | 37.6 (6.2) | 31.7 (3.3) | 22.3 (4.3) | 17.4 (0.8) | 27.1 (4.2) | 45.3 (3.7) |
| Other | 15.5 (1.2) | 27.6 (10.5) | 43.4 (8.2) | 18.1 (7.9) | 26.0 (1.8) | 30.9 (9.3) | 40.6 (7.4) |
| White | 18.8 (0.6) | 39.3 (6.5) | 52.3 (3.0) | 23.1 (3.1) | 28.4 (0.7) | 36.7 (3.3) | 59.7 (2.6) |
| Gender, % (SE) | |||||||
| Female | 13.2 (0.5) | 33.0 (5.2) | 42.3 (2.2) | 16.9 (2.3) | 21.9 (0.7) | 28.5 (3.5) | 52.8 (2.2) |
| Male | 14.3 (0.5) | 33.1 (4.7) | 32.6 (4.2) | 18.8 (3.0) | 21.6 (0.6) | 30.5 (3.0) | 39.8 (3.7) |
| Age, y, % (SE) | |||||||
| 13 | NA | NA | NA | NA | NA | NA | NA |
| 14 | 7.4 (0.6) | 24.7 (11.1) | 32.8 (5.8) | 7.1 (3.1) | 15.7 (1.4) | 30.3 (7.8) | 40.9 (9.1) |
| 15 | 11.6 (0.6) | 36.1 (7.1) | 40.5 (4.3) | 15.8 (3.3) | 19.0 (0.9) | 28.1 (5.0) | 46.3 (4.2) |
| 16 | 14.8 (0.6) | 24.8 (5.5) | 40.0 (3.5) | 19.9 (3.8) | 21.5 (0.9) | 23.8 (4.1) | 44.7 (3.3) |
| 17 | 16.1 (0.6) | 31.9 (5.6) | 38.9 (4.5) | 19.3 (3.9) | 23.3 (0.8) | 32.8 (4.2) | 55.9 (3.5) |
| ≥ 18 | 18.9 (1.0) | 48.0 (12.0) | 50.3 (5.5) | 23.2 (5.7) | 26.1 (1.2) | 33.4 (5.2) | 58.9 (4.4) |
| Ever smoked daily | |||||||
| Total, no. | 35534 | 503 | 1422 | 947 | 20825 | 841 | 1402 |
| Total, % (SE) | 8.7 (0.3) | 29.7 (3.6) | 27.1 (1.8) | 10.9 (1.5) | 13.9 (0.4) | 18.9 (2.1) | 34.5 (2.1) |
| Race/ethnicity, % (SE) | |||||||
| API | 5.8 (0.7) | 32.2 (9.9) | 31.6 (7.4) | 6.0 (2.5) | 13.7 (1.7) | 30.0 (7.9) | 35.3 (9.5) |
| Black | 4.0 (0.4) | 32.6 (8.0) | 8.5 (3.1) | 7.1 (2.7) | 5.8 (0.7) | 10.8 (3.5) | 14.6 (3.9) |
| Hispanic | 6.2 (0.5) | 19.8 (4.9) | 19.7 (2.8) | 11.5 (2.9) | 9.6 (0.7) | 12.2 (3.2) | 24.6 (3.1) |
| Other | 7.3 (0.7) | 13.6 (7.0) | 26.0 (7.0) | 15.0 (7.5) | 15.6 (1.8) | 5.1 (2.9) | 29.7 (7.3) |
| White | 10.2 (1.2) | 34.8 (6.6) | 40.7 (3.4) | 16.2 (3.6) | 20.0 (0.8) | 26.3 (3.9) | 46.3 (3.0) |
| Gender, % (SE) | |||||||
| Female | 8.0 (0.4) | 33.9 (5.9) | 28.0 (2.4) | 9.2 (1.7) | 13.6 (0.6) | 18.3 (3.4) | 36.4 (2.5) |
| Male | 9.4 (0.4) | 27.3 (4.6) | 23.4 (3.8) | 12.7 (2.4) | 14.1 (0.6) | 19.3 (3.0) | 28.9 (3.5) |
| Age, y, % (SE) | |||||||
| 13 | NA | NA | NA | NA | NA | NA | NA |
| 14 | 4.7 (0.5) | 27.2 (14.6) | 20.0 (5.1) | 4.1 (2.4) | 9.5 (1.1) | 6.8 (4.6) | 28.8 (6.7) |
| 15 | 6.0 (0.4) | 35.7 (8.1) | 25.2 (3.5) | 7.4 (2.5) | 10.8 (0.8) | 23.8 (5.3) | 29.5 (3.8) |
| 16 | 9.1 (0.6) | 18.6 (5.5) | 28.6 (3.7) | 13.7 (3.1) | 13.3 (0.8) | 18.6 (3.9) | 32.0 (3.2) |
| 17 | 11.4 (0.5) | 25.6 (5.8) | 27.6 (3.6) | 8.3 (2.5) | 15.9 (0.7) | 16.7 (3.6) | 36.5 (3.6) |
| ≥ 18 | 12.8 (1.0) | 47.6 (8.6) | 34.5 (6.1) | 17.2 (5.6) | 17.8 (1.2) | 23.9 (5.8) | 50.7 (5.7) |
| No. cigarettes smokeda | |||||||
| Total, no. | 6899 | 217 | 744 | 271 | 6319 | 227 | 918 |
| Total, mean (SE) | 86.4 (3.2) | 148.6 (21.1) | 117.2 (9.0) | 116.4 (13.7) | 97.1 (2.9) | 111.3 (14.3) | 142.4 (8.3) |
| Race/ethnicity, mean (SE) | |||||||
| API | 122.1 (17.9) | 101.6 (34.9) | 177.0 (81.9) | 38.5 (17.3) | 116.0 (21.3) | 94.8 (34.3) | 241.2 (76.9) |
| Black | 59.3 (7.2) | 116.4 (32.8) | 70.7 (25.0) | 177.9 (68.1) | 79.2 (11.6) | 54.3 (20.4) | 88.6 (21.6) |
| Hispanic | 46.5 (5.1) | 152.2 (35.8) | 81.7 (14.4) | 78.8 (24.2) | 61.5 (5.7) | 106.7 (39.8) | 105.4 (15.6) |
| Other | 90.9 (8.6) | 122.5 (39.2) | 83.4 (16.4) | 173.0 (54.8) | 96.3 (9.3) | 47.4 (21.9) | 127.8 (18.7) |
| White | 100.4 (4.1) | 155.0 (34.7) | 135.7 (11.2) | 131.4 (23.9) | 106.8 (3.3) | 124.1 (20.7) | 155.8 (10.8) |
| Gender, mean (SE) | |||||||
| Female | 72.9 (3.1) | 128.6 (24.3) | 104.0 (8.8) | 89.7 (18.5) | 79.7 (3.2) | 141.3 (25.7) | 123.1 (8.7) |
| Male | 98.7 (4.9) | 162.1 (29.1) | 166.1 (27.9) | 141.1 (23.6) | 112.6 (4.3) | 88.3 (16.9) | 213.7 (24.5) |
| Age, y, mean (SE) | |||||||
| 13 | NA | NA | NA | NA | NA | NA | NA |
| 14 | 62.7 (10.0) | 135.3 (67.9) | 90.8 (22.7) | NA | 69.1 (11.4) | 47.8 (19.7) | 111.0 (18.6) |
| 15 | 71.2 (5.4) | 154.3 (38.7) | 92.5 (16.9) | 62.1 (20.2) | 79.3 (5.6) | 131.4 (43.8) | 114.1 (16.4) |
| 16 | 93.3 (5.3) | 117.7 (25.8) | 129.9 (17.7) | 100.0 (23.1) | 96.2 (5.8) | 127.5 (27.8) | 133.0 (14.7) |
| 17 | 105.3 (5.0) | 149.9 (45.8) | 111.9 (16.3) | 138.5 (34.7) | 104.4 (4.4) | 79.7 (14.0) | 154.6 (15.6) |
| ≥ 18 | 95.9 (8.7) | 164.9 (51.2) | 169.7 (27.0) | 175.2 (39.7) | 113.5 (8.2) | 164.6 (46.9) | 187.7 (20.4) |
Note. API = Asian/Pacific Islander; NA = not available (too few participants to reliably estimate). Numbers are unweighted. Percentages are weighted. Data came from 13 jurisdictions that asked questions on sexual orientation identity or gender of lifetime sexual partners: Boston, MA; Chicago, IL; Connecticut; Delaware; Maine; Massachusetts; Milwaukee, WI; New York City, NY; Rhode Island; San Diego, CA; San Francisco, CA; Vermont; and Wisconsin.
Among past-month smokers.
Sexual Orientation Identity
Main effects.
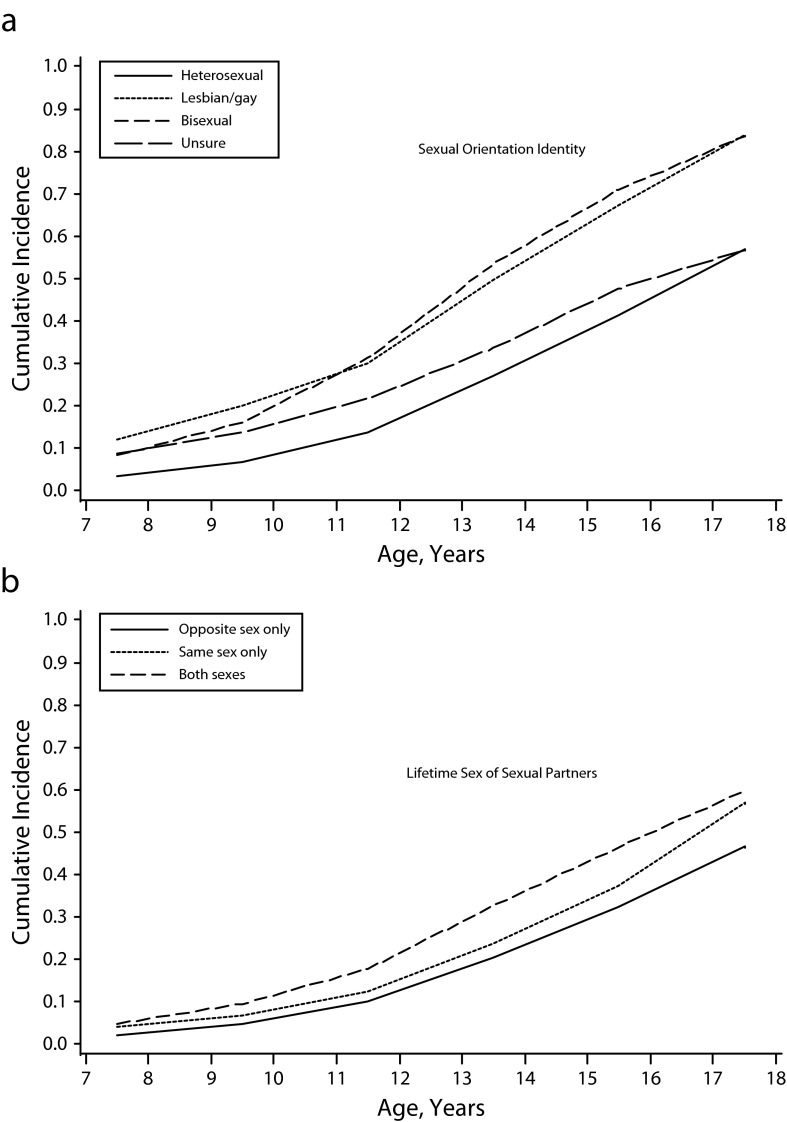
Models including only main effects and adjusting for age, race/ethnicity, and gender showed that lesbians–gays (HR = 2.14; 95% CI = 1.75, 2.61), bisexuals (HR = 2.33; 95% CI = 2.13, 2.55), and those unsure of their sexual orientation (HR = 1.27; 95% CI = 1.05, 1.54) reported a younger age at first smoking (Figure 1). Lesbians–gays (OR = 3.16; 95% CI = 2.24, 4.47), bisexuals (OR = 3.65; 95% CI = 3.11, 4.27), and unsure respondents (OR = 1.32; 95% CI = 1.04, 1.68) were also more likely than heterosexuals to report ever smoking. Odds of ever smoking daily and of past-month smoking were also higher among lesbian–gay (ever, OR = 4.80; 95% CI = 3.29, 7.00; past month, OR = 3.15; 95% CI = 2.28, 4.34), bisexual (ever, OR = 4.19; 95% CI = 3.46, 5.08; past month, OR = 4.41; 95% CI = 3.74, 5.19), and unsure (ever, OR = 1.47; 95% CI = 1.05, 2.04; past month, OR = 1.50; 95% CI = 1.15, 1.95) adolescents than among heterosexuals. Among past-month smokers, lesbian–gay (b = 60.8; 95% CI = 18.7, 102.9), bisexual (b = 40.6; 95% CI = 23.1, 58.1), and unsure (b = 30.9; 95% CI = 1.8, 60.0) adolescents smoked more cigarettes than did heterosexuals.
FIGURE 1—
Cumulative incidence plots of age at first smoking by (a) sexual orientation identity and (b) lifetime sex of sexual partner: Youth Risk Behavior Survey, United States, 2005 and 2007.
Note. Data came from 13 jurisdictions that asked questions on sexual orientation identity or gender of lifetime sexual partners: Boston, MA; Chicago, IL; Connecticut; Delaware; Maine; Massachusetts; Milwaukee, WI; New York City, NY; Rhode Island; San Diego, CA; San Francisco, CA; Vermont; and Wisconsin.
Interactions with race/ethnicity, gender, and age.
Tests for interactions of sexual orientation identity with race/ethnicity, gender, and age revealed novel patterns (models with interaction terms displayed in Table 2). Three of 5 smoking indicator disparities between lesbian–gay and heterosexual Black adolescents were larger than those between lesbian–gay and heterosexual White adolescents. Disparities between LGB and heterosexual adolescents also appeared to be larger among API than White adolescents across most of the smoking indicators, although not all were statistically significant. In addition, bisexual female youths appeared to be at relatively greater risk for smoking on several indicators. Age at first smoking was relatively younger and ever smoking and smoking in the past month were relatively more prevalent in female than male bisexuals, but the reverse was true for female and male heterosexuals. Smoking disparities between bisexuals and heterosexuals were larger at younger than older ages.
TABLE 2—
Results of Multivariate Analyses of Interactions of Sexual Orientation Identity With Race/Ethnicity, Gender, and Age on Cigarette Smoking: Youth Risk Behavior Survey, United States, 2005 and 2007
| Variable | Model 1: Age First Smoked, HRa (95% CI) | Model 2: Ever Smoked, ORb (95% CI) | Model 3: Ever Smoked Daily, ORb (95% CI) | Model 4: Smoked in Past Month, ORb (95% CI) | Model 5: No. Cigarettes Smoked in Past Month,c bd (95% CI) |
| Sexual orientation | |||||
| Heterosexual (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Lesbian/gay | 2.54 (1.14, 5.66) | 2.40 (0.69, 8.39) | 6.20 (1.38, 27.83) | 3.99 (1.08, 14.69) | 67.8 (−114.3, 249.9) |
| Bisexual | 2.51 (1.74, 3.62) | 3.79 (1.93, 7.46) | 6.72 (2.89, 15.61) | 5.86 (2.76, 12.44) | 50.1 (−24.6, 124.8) |
| Unsure | 1.95 (1.12, 3.39) | 2.24 (1.11, 4.51) | 1.33 (0.66, 8.11) | 1.42 (0.62, 3.23) | 36.0 (−109.3, 181.2) |
| Race/ethnicity | |||||
| White (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| API | 0.58 (0.51, 0.66) | 0.49 (0.42, 0.58) | 0.41 (0.32, 0.53) | 0.36 (0.29, 0.45) | 20.8 (−16.1, 57.6) |
| Black | 0.63 (0.57, 0.69) | 0.54 (0.48, 0.61) | 0.28 (0.21, 0.36) | 0.31 (0.26, 0.38) | −38.7 (−54.0, −23.4) |
| Hispanic | 0.98 (0.89, 1.08) | 0.97 (0.85, 1.10) | 0.45 (0.36, 0.55) | 0.58 (0.51, 0.66) | −51.5 (−63.6, −39.4) |
| Other | 0.93 (0.82, 1.05) | 0.88 (0.74, 1.05) | 0.82 (0.64, 1.05) | 0.85 (0.70, 1.04) | −7.9 (−24.8, 9.1) |
| Female | 0.91 (0.86, 0.97) | 0.90 (0.84, 0.97) | 0.87 (0.77, 0.99) | 0.95 (0.87, 1.04) | −25.7 (−35.7, −15.7) |
| Age | 0.94 (0.91, 0.97) | 1.27 (1.23, 1.32) | 1.33 (1.25, 1.40) | 1.26 (1.20, 1.31) | 8.7 (3.4, 14.1) |
| Orientation × race/ethnicity | |||||
| Lesbian/gay × API | 2.31 (1.37, 3.92) | 2.76 (1.19, 6.43) | 1.92 (0.61, 6.06) | 2.13 (0.72, 6.25) | −67.9 (−167.0, 31.2) |
| Lesbian/gay × Black | 1.64 (1.00, 2.68) | 2.06 (0.88, 4.81) | 3.13 (1.21, 8.05) | 1.00 (0.36, 2.80) | 4.4 (−89.2, 98.0) |
| Lesbian/gay × Hispanic | 1.15 (0.76, 1.72) | 1.34 (0.64, 2.81) | 1.06 (0.56, 2.46) | 1.65 (0.80, 3.42) | 53.6 (−43.0, 150.2) |
| Lesbian/gay × Other | 0.93 (0.36, 2.40) | 0.77 (0.25, 2.40) | 0.38 (0.10, 1.49) | 0.68 (0.21, 2.20) | −43.5 (−153.5, 66.4) |
| Bisexual × API | 1.62 (1.13, 2.33) | 2.07 (1.06, 4.03) | 1.64 (0.74, 3.60) | 1.53 (0.75, 3.09) | 2.5 (−154.1, 159.0) |
| Bisexual × Black | 0.96 (0.74, 1.24) | 0.82 (0.54, 1.25) | 0.49 (0.22, 1.11) | 0.82 (0.48, 1.39) | −28.0 (−84.3, 28.3) |
| Bisexual × Hispanic | 0.85 (0.70, 1.04) | 0.82 (0.56, 1.19) | 0.79 (0.49, 1.29) | 0.71 (0.49, 1.02) | −5.2 (−41.4, 31.0) |
| Bisexual × other | 1.12 (0.80, 1.56) | 1.17 (0.57, 2.39) | 0.67 (0.33, 1.38) | 0.89 (0.44, 1.81) | −44.3 (−91.0, 2.4) |
| Unsure × API | 0.78 (0.46, 1.31) | 0.85 (0.45, 1.62) | 0.70 (0.22, 2.22) | 1.13 (0.47, 2.72) | –121.8 (−196.1, −47.6) |
| Unsure × Black | 1.51 (0.84, 2.71) | 1.62 (0.79, 3.30) | 1.28 (0.54, 3.00) | 0.74 (0.33, 1.64) | 68.8 (−64.0, 201.7) |
| Unsure × Hispanic | 1.17 (0.81, 1.69) | 1.26 (0.77, 2.05) | 1.48 (0.63, 3.52) | 1.58 (0.83, 3.02) | 4.3 (−65.5, 74.1) |
| Unsure × other | 0.72 (0.32, 1.62) | 0.64 (0.27, 1.54) | 1.15 (0.33, 3.99) | 0.85 (0.27, 2.65) | 54.3 (−69.6, 178.3) |
| Orientation × gender | |||||
| Lesbian/gay × female | 1.22 (0.87, 1.71) | 1.47 (0.80, 2.69) | 1.52 (0.67, 3.46) | 1.31 (0.68, 2.52) | −5.8 (−75.6, 64.0) |
| Bisexual × female | 1.43 (1.11, 1.84) | 2.12 (1.43, 3.14) | 1.53 (0.79, 2.97) | 1.66 (1.06, 2.61) | −35.2 (−85.3, 14.8) |
| Unsure × female | 0.78 (0.57, 1.08) | 0.81 (0.53, 1.22) | 0.73 (0.41, 1.30) | 0.74 (0.46, 1.20) | −19.4 (−79.7, 41.0) |
| Orientation × age | |||||
| Lesbian/gay × age | 0.91 (0.77, 1.07) | 0.95 (0.73, 1.24) | 0.84 (0.62, 1.13) | 0.89 (0.66, 1.19) | −3.6 (−38.9, 31.7) |
| Bisexual × age | 0.92 (0.86, 1.00) | 0.87 (0.76, 1.00) | 0.85 (0.71, 1.00) | 0.87 (0.75, 1.00) | 6.0 (−9.3, 21.4) |
| Unsure × age | 0.91 (0.79, 1.05) | 0.88 (0.74, 1.03) | 0.91 (0.67, 1.24) | 1.03 (0.86, 1.25) | 1.6 (−27.8, 31.1) |
Note. API = Asian/Pacific Islander; CI = confidence interval; HR = hazard ratio; OR = odds ratio. Data came from 13 jurisdictions that asked questions on sexual orientation identity or gender of lifetime sexual partners: Boston, MA; Chicago, IL; Connecticut; Delaware; Maine; Massachusetts; Milwaukee, WI; New York City, NY; Rhode Island; San Diego, CA; San Francisco, CA; Vermont; and Wisconsin.
Estimated from Cox proportional hazards regression.
Estimated from logistic regression.
Among past-month smokers.
Estimated from linear regression.
Gender of Sexual Partners
Main effects.
The magnitude of sexual orientation disparities was smaller for gender of sexual partners than for sexual orientation identity. Sexual minority adolescents reported a younger age for first smoking (Figure 1) and a greater likelihood of ever smoking than sexual majority adolescents: respondents who reported only same-sex partners had an HR of 1.31 (95% CI = 1.17, 1.47) for age and an OR of 1.73 (95% CI = 1.41, 2.12) for smoking, and respondents with partners of both sexes had an HR of 1.78 (95% CI = 1.62, 1.95) for age and an OR of 2.61 (95% CI = 2.17, 3.13) for smoking in models including only main effects and adjusting for age, gender, race/ethnicity, and age at first sexual intercourse. Ever smoking daily and past-month smoking were also more prevalent among adolescents who reported only same-sex partners (daily smoking, OR = 1.47; 95% CI = 1.09, 2.00; past month, OR = 1.56; 95% CI = 1.26, 1.93) or both-sex partners (daily smoking, OR = 2.98; 95% CI = 2.47, 3.60; past month, OR = 3.31; 95% CI = 2.77, 3.95) than among adolescents who reported only opposite-sex partners. Among past-month smokers, number of cigarettes smoked was greater in adolescents reporting both-sex partners (b = 42.3; 95% CI = 27.7, 56.9), but lower among adolescents reporting only same-sex partners (b = 11.6; 95% CI = −0.7, 22.2) than among adolescents reporting only opposite-sex partners.
Interactions with race/ethnicity, gender, and age.
We observed few significant interactions of gender of sexual partners with race/ethnicity or age (Table 3). The only consistent findings concerned gender. Adolescents girls with both-sex partners were at relatively greater risk for smoking on most indicators. In addition, among past-month smokers, female respondents with same-sex partners smoked a disproportionately larger number of cigarettes than did male respondents with same-sex partners; gender differences among adolescents with only opposite-sex partners were much smaller.
TABLE 3—
Results of Multivariate Analyses of Interactions of Gender of Lifetime Sexual Partners With Race/Ethnicity, Gender, and Age on Cigarette Smoking: Youth Risk Behavior Survey, United States, 2005 and 2007
| Variable | Model 1: Age First Smoked, HRa (95% CI) | Model 2: Ever Smoked, ORb (95% CI) | Model 3: Ever Smoked Daily, ORb (95% CI) | Model 4: Smoked in Past Month, ORb (95% CI) | Model 5: No. Cigarettes Smoked in Past Month,c bd (95% CI) |
| Gender of lifetime sexual partners | |||||
| Opposite sex only (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Same sex only | 1.11 (0.71, 1.75) | 1.65 (0.74, 3.69) | 2.10 (0.70, 6.63) | 1.86 (0.75, 4.60) | −15.8 (−110.5, 79.0) |
| Both sexes | 1.16 (0.81, 1.68) | 1.32 (0.68, 2.58) | 2.70 (1.11, 6.60) | 2.53 (1.16, 5.51) | 76.7 (3.7, 149.7) |
| Race/ethnicityf | |||||
| White (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| API | 0.85 (0.74, 0.97) | 0.78 (0.64, 0.95) | 0.60 (0.44, 0.82) | 0.61 (0.48, 0.78) | 6.6 (−33.9, 47.1) |
| Black | 0.43 (0.39, 0.47) | 0.31 (0.27, 0.35) | 0.16 (0.12, 0.20) | 0.19 (0.15, 0.23) | −50.2 (−71.4, −29.0) |
| Hispanic | 0.74 (0.68, 0.80) | 0.65 (0.58, 0.74) | 0.31 (0.26, 0.38) | 0.41 (0.36, 0.47) | −55.1 (−66.4, −43.9) |
| Other | 0.80 (0.70, 0.92) | 0.71 (0.57, 0.87) | 0.58 (0.43, 0.77) | 0.74 (0.60, 0.91) | −12.1 (−28.9, 4.7) |
| Female | 1.03 (0.98, 1.09) | 1.08 (0.99, 1.18) | 1.06 (0.93, 1.21) | 1.09 (0.99, 1.21) | −23.4 (−33.3, −13.4) |
| Age | 0.88 (0.85, 0.91) | 1.20 (1.14, 1.25) | 1.31 (1.23, 1.39) | 1.20 (1.15, 1.27) | 15.2 (10.0, 20.3) |
| Gender of partners × race/ethnicity | |||||
| Same sex × API | 1.39 (0.93, 2.08) | 1.58 (0.71, 3.51) | 2.02 (0.75, 5.43) | 1.37 (0.53, 3.54) | −56.3 (−147.0, 34.4) |
| Same sex × Black | 1.12 (0.78, 1.60) | 0.89 (0.52, 1.52) | 1.61 (0.64, 4.04) | 1.14 (0.57, 2.30) | −26.8 (−86.3, 32.7) |
| Same sex × Hispanic | 0.92 (0.67, 1.25) | 0.70 (0.41, 1.18) | 0.95 (0.44, 2.03) | 1.24 (0.72, 2.14) | 14.0 (−64.9, 92.8) |
| Same sex × other | 0.96 (0.66, 1.41) | 1.01 (0.44, 2.32) | 0.18 (0.05, 0.63) | 0.81 (0.32, 2.02) | –85.9 (–147.8, −24.0) |
| Both sexes × API | 1.14 (0.73, 1.78) | 0.73 (0.35, 1.54) | 0.93 (0.40, 2.19) | 1.07 (0.50, 2.28) | 32.5 (−95.1, 160.1) |
| Both genders × Black | 0.99 (0.73, 1.34) | 0.75 (0.47, 1.22) | 0.89 (0.44, 1.79) | 0.90 (0.52, 1.56) | −39.4 (−87.5, 8.6) |
| Both genders × Hispanic | 1.10 (0.92, 1.32) | 1.14 (0.77, 1.68) | 1.01 (0.64, 1.60) | 1.19 (0.81, 1.74) | −10.5 (−45.8, 24.8) |
| Both genders × other | 0.90 (0.56, 1.44) | 0.57 (0.26, 1.28) | 0.71 (0.32, 1.58) | 0.54 (0.27, 1.08) | −31.1 (−72.9, 10.8) |
| Gender of partners × gender | |||||
| Same sex × female | 1.10 (0.87, 1.39) | 1.06 (0.70, 1.62) | 1.17 (0.60, 2.27) | 0.96 (0.58, 1.56) | 73.7 (11.1, 136.3) |
| Both genders × female | 1.29 (1.05, 1.60) | 2.08 (1.45, 2.98) | 1.72 (1.05, 2.82) | 1.87 (1.34, 2.62) | −39.5 (−86.9, 7.9) |
| Gender of partners × age | |||||
| Same sex × age | 1.02 (0.92, 1.14) | 1.02 (0.85, 1.23) | 0.89 (0.70, 1.12) | 0.95 (0.78, 1.15) | 0.4 (−21.0, 21.7) |
| Both genders × age | 1.05 (0.97, 1.14) | 1.06 (0.90, 1.23) | 0.94 (0.78, 1.13) | 0.96 (0.82, 1.12) | 0.9 (−10.9, 12.7) |
Note. API = Asian/Pacific Islander; CI = confidence interval; HR = hazard ratio; OR = odds ratio. Models adjusted for age at first sexual intercourse. Data came from 13 jurisdictions that asked questions on sexual orientation identity or gender of lifetime sexual partners: Boston, MA; Chicago, IL; Connecticut; Delaware; Maine; Massachusetts; Milwaukee, WI; New York City, NY; Rhode Island; San Diego, CA; San Francisco, CA; Vermont; and Wisconsin.
Estimated from Cox proportional hazards regression.
Estimated from logistic regression.
Among past-month smokers.
Estimated from linear regression.
DISCUSSION
The etiology of adolescent smoking is complex and involves many risk and protective factors across individual, family, peer, and societal contexts.33 Thus, several theoretical frameworks have been applied to explain diversity in adolescent smoking.31 In regard to sexual minorities, researchers have applied stress theory, which argues that sexual minorities smoke to cope with difficulties arising from their stigmatized sexual orientation.34–37 In support of this model, studies have found that stressors such as discrimination and victimization,38–42 negative reactions from others to disclosing a same-sex orientation,43 concealing a same-sex orientation,44 and living in communities lacking LGB-supportive policies45 are linked with greater smoking prevalence among sexual minority youths.
More generally, researchers have applied several other theories to explain adolescent smoking (e.g., social learning theory,46,47 ecological systems theory,48,49 theory of planned behavior,49,50 problem behavior theory,51,52 and self-medication theory53,54). Evidence suggests that multiple theories in conjunction, rather than any 1 in isolation, more fully explain adolescent smoking.55 Evidence also suggests that exposure to risk and protective factors identified by these theories, and their influence on adolescent smoking, vary across race/ethnicity, gender, and age.17,56–68 Consequently, future research to improve understanding of how sexual orientation, race/ethnicity, gender, and age intersect to influence adolescent smoking will benefit from integrating these multiple theories.
Our finding that sexual minority adolescents were more likely than heterosexuals to smoke cigarettes corroborates previous literature.6,7,9–12 We extended the literature by examining how race/ethnicity, gender, and age modified sexual orientation disparities in adolescent smoking in data pooled from 13 jurisdictions across the United States. For both sexual orientation dimensions examined, we found elevated smoking risk for sexual minorities across race/ethnicity, gender, and age subgroups. However, relative risk between these groups varied, and it appeared that bisexual adolescent girls, younger bisexuals, Black gays and lesbians, API sexual minorities, and adolescent girls reporting both-sex partners were at especially elevated risk. Although smoking was more prevalent among White than racial/ethnic minority adolescents, in some instances sexual orientation disparities were accentuated in Black lesbian–gay and API sexual minority adolescents. In other words, the smoking patterns of these youths were higher than or more similar to their White sexual minority peers and less comparable to their heterosexual peers of the same race/ethnicity. In support of this finding, a community study found that Black lesbians were more likely than Black heterosexual women and White lesbians to smoke.69 Future research should examine smoking in Black lesbian–gay, API sexual minority, bisexual female, and younger bisexual adolescents to verify these findings as well as to identify reasons for this potentially elevated risk.
Our finding that risk for adolescent smoking varied across sexual orientation, race/ethnicity, gender, and age underscores the importance of considering risk and protective factors that are specific to subgroups. Future research should test the extent to which minority stress theory and other theories relevant to adolescent smoking explain disparities arising from sexual orientation and intersecting sociodemographic characteristics. Although our sample size was not adequate for comparing the experiences of subgroups at the intersections of multiple factors (e.g., Hispanic, young, bisexual), future research will benefit from an intersectional approach, which seeks to explain how multiple social statuses and inequalities operate jointly to influence health and argues that identities are better understood in combination.70 As an example, because acculturation is known to affect smoking risk differently for male and female adolescents,71–74 acculturation would be important to consider in future research to understand influences of sexual orientation, race/ethnicity, and gender in ethnic minorities.
Our study also extended the literature by examining how findings varied across 2 dimensions of sexual orientation. In general, smoking disparities were larger when we categorized respondents by sexual orientation identity rather than gender of sexual partners. We found differences in how race/ethnicity, gender, and age modified sexual orientation disparities in smoking depending on the dimension examined (e.g., disparities were relatively larger in younger adolescents identifying as bisexual, but not among younger adolescents reporting both-sex partners). These findings support the importance of considering multiple dimensions of sexual orientation to understand how sexual orientation affects adolescent smoking risk. Our disparate findings derived from the sexual orientation dimension likely occurred because the gender of sexual partners variable excluded the approximately 40% of the sample who reported no sexual partners, whereas the sexual orientation identity variable included all respondents who answered the question regardless of their sexual experience. In addition, a subanalysis with the 8 jurisdictions that included both sexual orientation indicators on the questionnaire showed that self-identified heterosexuals were more likely to be excluded from the gender of sexual partners analyses because they were more likely to report no sexual partners (43%) than were lesbian–gay (24%) and bisexual (20%) participants (P < .001).
Limitations
Because some racial/ethnic subgroups were small, power was limited, and we had to collapse groups. Research with larger sample sizes is necessary to confirm our findings and provide more detailed information about intersections of sexual minority and racial/ethnic minority statuses. In addition, most jurisdictions that included questions about sexual orientation were located in the Northeast or the western region of the United States, where civil rights for sexual minorities are more widespread than in other regions. Urban locations were also overrepresented, because 6 of the 13 jurisdictions were large metropolitan cities. Thus, findings may not be representative of the entire country.
Because data were self-reported, bias could have been introduced if accuracy of reporting smoking was related to sexual orientation, if misclassification of heterosexuals into a sexual minority category was significant, or if nonresponse was differentially related to sexual orientation and smoking. Nonetheless, the YRBS is a methodologically rigorous and long-standing surveillance system that is an important source for understanding health behaviors during adolescence.
Conclusions
Our findings provide more evidence that sexual minority adolescents of all races/ethnicities, genders, and ages are more likely than their heterosexual peers to smoke cigarettes and that they should be the focus of research, prevention, and cessation efforts. A multipronged approach is needed to reach adolescents displaying the full spectrum of smoking behaviors—from nonsmokers at risk for initiating smoking to daily smokers. Despite compelling epidemiological evidence of disparities in smoking risk among sexual minority youths, the 2012 surgeon general’s report Preventing Tobacco Use Among Youth and Young Adults5 overlooks this population, and few smoking prevention and cessation programs specifically target this group.
A qualitative study of 30 diverse LGB and transgender youths (aged 16–24 years) and 30 adults knowledgeable about LGB and transgender youths suggested strategies to address smoking in this population.75 Participants emphasized that youths should be involved in planning and implementing interventions and that interventions should go beyond smoking and address positive identity formation and adjustment, healthy coping strategies, and social support. To reduce the burden of smoking, it is imperative that prevention and cessation efforts targeting the general population of youths be evaluated for effectiveness among sexual minority youths. In addition, specific programs targeting this population should be designed and evaluated.
Evaluation of cessation programs for LGB and transgender adults have revealed quit success rates similar to or better than programs targeting the general population.76–78 Although research shows that LGB and transgender–specific programs are effective, it is unclear how findings generalize to youths. Smoking prevention and cessation interventions that consider the specific psychosocial and cultural experiences of subgroups of sexual minority youths may be most effective,76 but empirical evidence is necessary to clarify this issue.
Acknowledgments
This project was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R21HD051178) and by the IMPACT LGBT Health and Development Program at Northwestern University. Heather L. Corliss was supported by the National Institute on Drug Abuse (career development award DA023610).
We are grateful to Brian Mustanski, associate professor in the Department of Medical Social Sciences, Northwestern University Feinberg School of Medicine, and to Aimee Van Wagenen, program manager, and Judith Bradford, director, Center for Population Research in LGBT Health, Fenway Institute, for their work on this project. Assistance from the Centers for Disease Control and Prevention (CDC) Division of Adolescent and School Health, and the work of the state and local health and education departments who conduct the Youth Risk Behavior Survey made the project possible.
Note. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, the CDC, or any agencies involved in collecting the data.
Human Participant Protection
Institutional review board approval was not necessary because de-identified data were used. Data use agreements were obtained from all departments of health that required them for access to YRBS data.
References
- 1.Bartecchi CE, MacKenzie TD, Schrier RW. The human costs of tobacco use. N Engl J Med. 1994;330(13):907–912. doi: 10.1056/NEJM199403313301307. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Smoking-attributable mortality, years of potential life lost, and productivity losses—United States, 2000–2004. MMWR Morb Mortal Wkly Rep. 2008;57(45):1226–1228. [PubMed] [Google Scholar]
- 3.Breslau N, Fenn N, Peterson EL. Early smoking initiation and nicotine dependence in a cohort of young adults. Drug Alcohol Depend. 1993;33(2):129–137. doi: 10.1016/0376-8716(93)90054-t. [DOI] [PubMed] [Google Scholar]
- 4.Breslau N, Peterson EL. Smoking cessation in young adults: age at initiation of cigarette smoking and other suspected influences. Am J Public Health. 1996;86(2):214–220. doi: 10.2105/ajph.86.2.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Office on Smoking and Health. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; 2012. [PubMed] [Google Scholar]
- 6.Corliss HL, Wadler BM, Jun HJ et al. Sexual-orientation disparities in cigarette smoking in a longitudinal cohort study of adolescents. Nicotine Tob Res. 2013;15(1):213–222. doi: 10.1093/ntr/nts114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Easton A, Jackson K, Mowery P, Comeau D, Sell R. Adolescent same-sex and both-sex romantic attractions and relationships: implications for smoking. Am J Public Health. 2008;98(3):462–467. doi: 10.2105/AJPH.2006.097980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garofalo R, Wolf RC, Kessel S, Palfrey SJ, DuRant RH. The association between health risk behaviors and sexual orientation among a school-based sample of adolescents. Pediatrics. 1998;101(5):895–902. doi: 10.1542/peds.101.5.895. [DOI] [PubMed] [Google Scholar]
- 9.Hahm HC, Wong FY, Huang ZJ, Ozonoff A, Lee J. Substance use among Asian Americans and Pacific Islanders sexual minority adolescents: findings from the National Longitudinal Study of Adolescent Health. J Adolesc Health. 2008;42(3):275–283. doi: 10.1016/j.jadohealth.2007.08.021. [DOI] [PubMed] [Google Scholar]
- 10.Marshal MP, Friedman MS, Stall R, Thompson AL. Individual trajectories of substance use in lesbian, gay and bisexual youth and heterosexual youth. Addiction. 2009;104(6):974–981. doi: 10.1111/j.1360-0443.2009.02531.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Russell ST, Driscoll AK, Truong N. Adolescent same-sex romantic attractions and relationships: implications for substance use and abuse. Am J Public Health. 2002;92(2):198–202. doi: 10.2105/ajph.92.2.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Talley AE, Sher KJ, Littlefield AK. Sexual orientation and substance use trajectories in emerging adulthood. Addiction. 2010;105(7):1235–1245. doi: 10.1111/j.1360-0443.2010.02953.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blum RW, Beuhring T, Shew ML, Bearinger LH, Sieving RE, Resnick MD. The effects of race/ethnicity, income, and family structure on adolescent risk behaviors. Am J Public Health. 2000;90(12):1879–1884. doi: 10.2105/ajph.90.12.1879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wills TA, Cleary SD. The validity of self-reports of smoking: analyses by race/ethnicity in a school sample of urban adolescents. Am J Public Health. 1997;87(1):56–61. doi: 10.2105/ajph.87.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mermelstein R. Ethnicity, gender and risk factors for smoking initiation: an overview. Nicotine Tob Res. 1999;1(suppl 2):S39–S43. doi: 10.1080/14622299050011791. discussion S69–S70. [DOI] [PubMed] [Google Scholar]
- 16.Wallace JM, Jr, Bachman JG, O’Malley PM, Schulenberg JE, Cooper SM, Johnston LD. Gender and ethnic differences in smoking, drinking and illicit drug use among American 8th, 10th and 12th grade students, 1976–2000. Addiction. 2003;98(2):225–234. doi: 10.1046/j.1360-0443.2003.00282.x. [DOI] [PubMed] [Google Scholar]
- 17.Kandel DB, Kiros GE, Schaffran C, Hu MC. Racial/ethnic differences in cigarette smoking initiation and progression to daily smoking: a multilevel analysis. Am J Public Health. 2004;94(1):128–135. doi: 10.2105/ajph.94.1.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. Current tobacco use among middle and high school students—United States, 2011. MMWR Morb Mortal Wkly Rep. 2012;61(31):581–585. [PubMed] [Google Scholar]
- 19.Eaton DK, Kann L, Kinchen S et al. Youth risk behavior surveillance—United States, 2007. MMWR Surveill Summ. 2008;57(4):1–131. [PubMed] [Google Scholar]
- 20.Institute of Medicine. Washington, DC: National Academies Press; 2011. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. [PubMed] [Google Scholar]
- 21.Corliss HL, Cochran SD, Mays VM. Sampling approaches to studying mental health concerns in the lesbian, gay, and bisexual community. In: Meezan W, Martin JI, editors. Handbook of Research With Gay, Lesbian, Bisexual, and Transgender Populations. New York, NY: Routledge; 2009. pp. 131–158. [Google Scholar]
- 22.Marshal MP, Friedman MS, Stall R et al. Sexual orientation and adolescent substance use: a meta-analysis and methodological review. Addiction. 2008;103(4):546–556. doi: 10.1111/j.1360-0443.2008.02149.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ortiz-Hernández L, Tello BL, Valdés J. The association of sexual orientation with self-rated health, and cigarette and alcohol use in Mexican adolescents and youths. Soc Sci Med. 2009;69(1):85–93. doi: 10.1016/j.socscimed.2009.03.028. [DOI] [PubMed] [Google Scholar]
- 24.Blosnich JR, Jarrett T, Horn K. Racial and ethnic differences in current use of cigarettes, cigars, and hookahs among lesbian, gay, and bisexual young adults. Nicotine Tob Res. 2011;13(6):487–491. doi: 10.1093/ntr/ntq261. [DOI] [PubMed] [Google Scholar]
- 25.McCabe SE, Hughes TL, Bostwick W, Boyd CJ. Assessment of difference in dimensions of sexual orientation: implications for substance use research in a college-age population. J Stud Alcohol. 2005;66(5):620–629. doi: 10.15288/jsa.2005.66.620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McCabe SE, Hughes TL, Bostwick WB, West BT, Boyd CJ. Sexual orientation, substance use behaviors and substance dependence in the United States. Addiction. 2009;104(8):1333–1345. doi: 10.1111/j.1360-0443.2009.02596.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Scheer S, Parks CA, McFarland W et al. Self-reported sexual identity, sexual behaviors and health risks: examples from a population-based survey of young women. J Lesbian Stud. 2002;7(1):69–83. doi: 10.1300/J155v07n01_05. [DOI] [PubMed] [Google Scholar]
- 28.Russell ST. Substance use and abuse and mental health among sexual-minority youths: evidence from Add Health. In: Omoto AM, Kurtzman HS, editors. Sexual Orientation and Mental Health: Examining Identity and Development in Lesbian, Gay, and Bisexual People. Washington, DC: American Psychological Association; 2006. pp. 13–35. [Google Scholar]
- 29.Igartua K, Thombs BD, Burgos G, Montoro R. Concordance and discrepancy in sexual identity, attraction, and behavior among adolescents. J Adolesc Health. 2009;45(6):602–608. doi: 10.1016/j.jadohealth.2009.03.019. [DOI] [PubMed] [Google Scholar]
- 30.Saewyc EM. Research on adolescent sexual orientation: development, health disparities, stigma, and resilience. J Res Adolesc. 2011;21(1):256–272. doi: 10.1111/j.1532-7795.2010.00727.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tyas SL, Pederson LL. Psychosocial factors related to adolescent smoking: a critical review of the literature. Tob Control. 1998;7(4):409–420. doi: 10.1136/tc.7.4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mustanski B, Van Wagenen A, Birkett M, Eyster S, Corliss HL. Identifying sexual orientation health disparities in adolescents: analysis of pooled data from the Youth Risk Behavior Survey, 2005 and 2007. Am J Public Health. 2014;104(2):211–217. doi: 10.2105/AJPH.2013.301748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schepis TS, Rao U. Epidemiology and etiology of adolescent smoking. Curr Opin Pediatr. 2005;17(5):607–612. doi: 10.1097/01.mop.0000176442.49743.31. [DOI] [PubMed] [Google Scholar]
- 34.Blosnich J, Lee JGL, Horn K. A systematic review of the aetiology of tobacco disparities for sexual minorities. Tob Control. 2013;22(2):66–73. doi: 10.1136/tobaccocontrol-2011-050181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rosario M, Rotheram-Borus MJ, Reid H. Gay-related stress and its correlates among gay and bisexual male adolescents of predominantly Black and Hispanic background. J Community Psychol. 1996;24(2):136–159. [Google Scholar]
- 36.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hatzenbuehler ML. How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychol Bull. 2009;135(5):707–730. doi: 10.1037/a0016441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Blosnich JR, Horn K. Associations of discrimination and violence with smoking among emerging adults: differences by gender and sexual orientation. Nicotine Tob Res. 2011;13(12):1284–1295. doi: 10.1093/ntr/ntr183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bontempo DE, D’Augelli AR. Effects of at-school victimization and sexual orientation on lesbian, gay, or bisexual youths’ health risk behavior. J Adolesc Health. 2002;30(5):364–374. doi: 10.1016/s1054-139x(01)00415-3. [DOI] [PubMed] [Google Scholar]
- 40.Jun HJ, Austin SB, Wylie SA et al. The mediating effect of childhood abuse in sexual orientation disparities in tobacco and alcohol use during adolescence: results from the Nurses’ Health Study II. Cancer Causes Control. 2010;21(11):1817–1828. doi: 10.1007/s10552-010-9609-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Remafedi G. Lesbian, gay, bisexual, and transgender youths: who smokes, and why? Nicotine Tob Res. 2007;9(suppl 1):S65–S71. doi: 10.1080/14622200601083491. [DOI] [PubMed] [Google Scholar]
- 42.Rosario M, Schrimshaw EW, Hunter J. Cigarette smoking as a coping strategy: negative implications for subsequent psychological distress among lesbian, gay, and bisexual youths. J Pediatr Psychol. 2011;36(7):731–742. doi: 10.1093/jpepsy/jsp141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rosario M, Schrimshaw EW, Hunter J. Disclosure of sexual orientation and subsequent substance use and abuse among lesbian, gay, and bisexual youths: critical role of disclosure reactions. Psychol Addict Behav. 2009;23(1):175–184. doi: 10.1037/a0014284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pachankis JE, Westmaas JL, Dougherty LR. The influence of sexual orientation and masculinity on young men’s tobacco smoking. J Consult Clin Psychol. 2011;79(2):142–152. doi: 10.1037/a0022917. [DOI] [PubMed] [Google Scholar]
- 45.Hatzenbuehler ML, Wieringa NF, Keyes KM. Community-level determinants of tobacco use disparities in lesbian, gay, and bisexual youth: results from a population-based study. Arch Pediatr Adolesc Med. 2011;165(6):527–532. doi: 10.1001/archpediatrics.2011.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Akers RL, Lee G. A longitudinal test of social learning theory: adolescent smoking. J Drug Issues. 1996;26(2):317–343. [Google Scholar]
- 47.Bahr SJ, Hoffmann JP, Yang X. Parental and peer influences on the risk of adolescent drug use. J Prim Prev. 2005;26(6):529–551. doi: 10.1007/s10935-005-0014-8. [DOI] [PubMed] [Google Scholar]
- 48.Ennett ST, Foshee VA, Bauman KE et al. A social contextual analysis of youth cigarette smoking development. Nicotine Tob Res. 2010;12(9):950–962. doi: 10.1093/ntr/ntq122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wiium N, Wold B. An ecological system approach to adolescent smoking behavior. J Youth Adolesc. 2009;38(10):1351–1363. doi: 10.1007/s10964-008-9349-9. [DOI] [PubMed] [Google Scholar]
- 50.Higgins A, Conner M. Understanding adolescent smoking: the role of the Theory of Planned Behaviour and implementation intentions. Psychol Health Med. 2003;8(2):173–186. [Google Scholar]
- 51.Jessor R. Risk behavior in adolescence: a psychosocial framework for understanding and action. J Adolesc Health. 1991;12(8):597–605. doi: 10.1016/1054-139x(91)90007-k. [DOI] [PubMed] [Google Scholar]
- 52.Park S, Weaver TE, Romer D. Predictors of the transition from experimental to daily smoking in late adolescence and young adulthood. J Drug Educ. 2010;40(2):125–141. doi: 10.2190/DE.40.2.b. [DOI] [PubMed] [Google Scholar]
- 53.Audrain-McGovern J, Rodriguez D, Kassel JD. Adolescent smoking and depression: evidence for self-medication and peer smoking mediation. Addiction. 2009;104(10):1743–1756. doi: 10.1111/j.1360-0443.2009.02617.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chaiton M, Cohen J, O’Loughlin J, Rehm J. Use of cigarettes to improve affect and depressive symptoms in a longitudinal study of adolescents. Addict Behav. 2010;35(12):1054–1060. doi: 10.1016/j.addbeh.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 55.Collins RL, Ellickson PL. Integrating four theories of adolescent smoking. Subst Use Misuse. 2004;39(2):179–209. doi: 10.1081/ja-120028487. [DOI] [PubMed] [Google Scholar]
- 56.White HR, Pandina RJ, Chen PH. Developmental trajectories of cigarette use from early adolescence into young adulthood. Drug Alcohol Depend. 2002;65(2):167–178. doi: 10.1016/s0376-8716(01)00159-4. [DOI] [PubMed] [Google Scholar]
- 57.Ellickson PL, Orlando M, Tucker JS, Klein DJ. From adolescence to young adulthood: racial/ethnic disparities in smoking. Am J Public Health. 2004;94(2):293–299. doi: 10.2105/ajph.94.2.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fulkerson JA, French SA. Cigarette smoking for weight loss or control among adolescents: gender and racial/ethnic differences. J Adolesc Health. 2003;32(4):306–313. doi: 10.1016/s1054-139x(02)00566-9. [DOI] [PubMed] [Google Scholar]
- 59.Johnson RA, Hoffmann JP. Adolescent cigarette smoking in US racial/ethnic subgroups: findings from the National Education Longitudinal Study. J Health Soc Behav. 2000;41(4):392–407. [PubMed] [Google Scholar]
- 60.West JH, Romero RA, Trinidad DR. Adolescent receptivity to tobacco marketing by racial/ethnic groups in California. Am J Prev Med. 2007;33(2):121–123. doi: 10.1016/j.amepre.2007.03.014. [DOI] [PubMed] [Google Scholar]
- 61.Wiehe SE, Aalsma MC, Liu GC, Fortenberry JD. Gender differences in the association between perceived discrimination and adolescent smoking. Am J Public Health. 2010;100(3):510–516. doi: 10.2105/AJPH.2009.169771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Griesler PC, Kandel DB. Ethnic differences in correlates of adolescent cigarette smoking. J Adolesc Health. 1998;23(3):167–180. doi: 10.1016/s1054-139x(98)00029-9. [DOI] [PubMed] [Google Scholar]
- 63.Griesler PC, Kandel DB, Davies M. Ethnic differences in predictors of initiation and persistence of adolescent cigarette smoking in the National Longitudinal Survey of Youth. Nicotine Tob Res. 2002;4(1):79–93. doi: 10.1080/14622200110103197. [DOI] [PubMed] [Google Scholar]
- 64.Mahabee-Gittens EM, Xiao Y, Gordon JS, Khoury JC. Continued importance of family factors in youth smoking behavior. Nicotine Tob Res. 2012;14(12):1458–1466. doi: 10.1093/ntr/nts078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mahabee-Gittens EM, Xiao Y, Gordon JS, Khoury JC. The dynamic role of parental influences in preventing adolescent smoking initiation. Addict Behav. 2013;38(4):1905–1911. doi: 10.1016/j.addbeh.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mermelstein R. Explanations of ethnic and gender differences in youth smoking: a multi-site, qualitative investigation. Nicotine Tob Res. 1999;1(suppl 1):S91–S98. doi: 10.1080/14622299050011661. [DOI] [PubMed] [Google Scholar]
- 67.Schultz ASH, Nowatzki J, Ronson G. Effects of household socialization on youth susceptibility to smoke: differences between youth age groups and trends over time. Am J Public Health. 2013;103(7):e39–e42. doi: 10.2105/AJPH.2013.301344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Unger JB, Rohrbach LA, Cruz TB et al. Ethnic variation in peer influences on adolescent smoking. Nicotine Tob Res. 2001;3(2):167–176. doi: 10.1080/14622200110043086. [DOI] [PubMed] [Google Scholar]
- 69.Hughes TL, Johnson TP, Matthews AK. Sexual orientation and smoking: results from a multisite women’s health study. Subst Use Misuse. 2008;43(8–9):1218–1239. doi: 10.1080/10826080801914170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bowleg L. The problem with the phrase women and minorities: intersectionality—an important theoretical framework for public health. Am J Public Health. 2012;102(7):1267–1273. doi: 10.2105/AJPH.2012.300750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Almeida J, Johnson RM, Matsumoto A, Godette DC. Substance use, generation and time in the United States: the modifying role of gender for immigrant urban adolescents. Soc Sci Med. 2012;75(12):2069–2075. doi: 10.1016/j.socscimed.2012.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hofstetter CR, Hovell MF, Jung KR, Raman R, Irvin V, Ni R. The first puff: forces in smoking initiation among Californians of Korean descent. Nicotine Tob Res. 2007;9(12):1277–1286. doi: 10.1080/14622200701704863. [DOI] [PubMed] [Google Scholar]
- 73.Lorenzo-Blanco EI, Unger JB, Ritt-Olson A, Soto D, Baezconde-Garbanati L. Acculturation, gender, depression, and cigarette smoking among US Hispanic youth: the mediating role of perceived discrimination. J Youth Adolesc. 2011;40(11):1519–1533. doi: 10.1007/s10964-011-9633-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sussman NM, Truong N. “Please extinguish all cigarettes”: the effects of acculturation and gender on smoking attitudes and smoking prevalence of Chinese and Russian immigrants. Int J Intercult Relat. 2011;35(2):163–178. [Google Scholar]
- 75.Remafedi G, Carol H. Preventing tobacco use among lesbian, gay, bisexual, and transgender youths. Nicotine Tob Res. 2005;7(2):249–256. doi: 10.1080/14622200500055517. [DOI] [PubMed] [Google Scholar]
- 76.Eliason MJ, Dibble SL, Gordon R, Soliz GB. The last drag: an evaluation of an LGBT-specific smoking intervention. J Homosex. 2012;59(6):864–878. doi: 10.1080/00918369.2012.694770. [DOI] [PubMed] [Google Scholar]
- 77.Harding R, Bensley J, Corrigan N. Targeting smoking cessation to high prevalence communities: outcomes from a pilot intervention for gay men. BMC Public Health. 2004;4:43. doi: 10.1186/1471-2458-4-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Walls NE, Wisneski H. Evaluation of smoking cessation classes for the lesbian, gay, bisexual, and transgender community. J Soc Serv Res. 2010;37(1):99–111. [Google Scholar]