Abstract
More than two decades of research has revealed a network of proteases that orchestrates cartilage degradation in osteoarthritis. This network includes not only metalloproteinases that degrade the major macromolecules in cartilage, aggrecan and type II collagen, but also serine proteases and cysteine proteases, such as cathepsin K. The current review summarizes the role of proteases in osteoarthritis progression, based on studies in genetically engineered mouse models. In addition, a brief overview of the biochemical characteristics and features of several key proteases in this network is provided, with the aim of increasing our understanding of how they function. Collectively, based on the data published to date, it can be concluded that at least three enzymes stand out as major targets for osteoarthritis drug development: ADAMTS-5, MMP-13, and cathepsin K. Mice that lack these enzymes are protected from cartilage damage and, to a varying degree, from bone changes in surgical models of osteoarthritis. In vivo studies with selective small molecule inhibitors targeting these proteases have been performed in various animal models. Going forward, mouse models will provide a tremendous opportunity for testing the therapeutic effects of protease inhibitors, not just on progression of structural damage to the joint, but also on associated pain.
Keywords: Protease, Osteoarthritis, Mouse models, Murine models, Genetically engineered mouse models, ADAMTS-5, MMP-13, Cathepsin K
Introduction
Enzymes that hydrolyze peptide bonds represent 1.7% of the human genome and constitute one of the largest protein families in the human body (second only to the ubiquitin ligase family and ahead of the protein kinases) [1]. The more than 600 members of the human “degradome” (= a complete set of proteases in an organism [1]) partake in virtually every biological pathway involved in the cell cycle, wound healing, immune response, blood coagulation, and other physiological and pathological processes. Proteases often act in tightly controlled networks or cascades, and dysregulation of their activities underlies many diseases, including cancer, neurodegenerative and cardiovascular disease, and arthritis [2]. They therefore represent a vast pool of putative targets for drug development. Some of the most successful drugs on the market are, in fact, protease inhibitors [3]; captopril, for example, an anti-hypertensive drug that targets the metalloprotease, angiotensin-converting enzyme, has been on the market since 1981. As of 2010, it was estimated that 5–10% of all drugs in development were targeting proteases [3].
Osteoarthritis (OA), the most common form of arthritis affecting the knees, hips, and hands, is characterized by biochemical and cellular changes in all joint tissues, including cartilage, subchondral bone, synovium, meniscus, ligaments, and fat pad [4]. A hallmark of these pathological changes is the turnover of connective tissues: subchondral bone sclerosis, bone cysts, osteophytes, synovial inflammation, fibrosis, and, foremost, loss of articular cartilage. It is therefore no surprise that proteases have received major attention as targets for the development of drugs that may halt the progression of structural damage to the joint. Such drugs are not yet available.
In this review, we focus on a network of key proteases active in OA cartilage. We provide a basic overview of their biochemical characteristics and discuss insights gained from mouse models regarding their role in OA pathology. Based on studies in genetically engineered mouse models (GeMMs), three proteases stand out as targets in OA: ADAMTS-5, MMP-13, and cathepsin K (catK). Progress made to date on the development of selective inhibitors of these enzymes will be reviewed briefly.
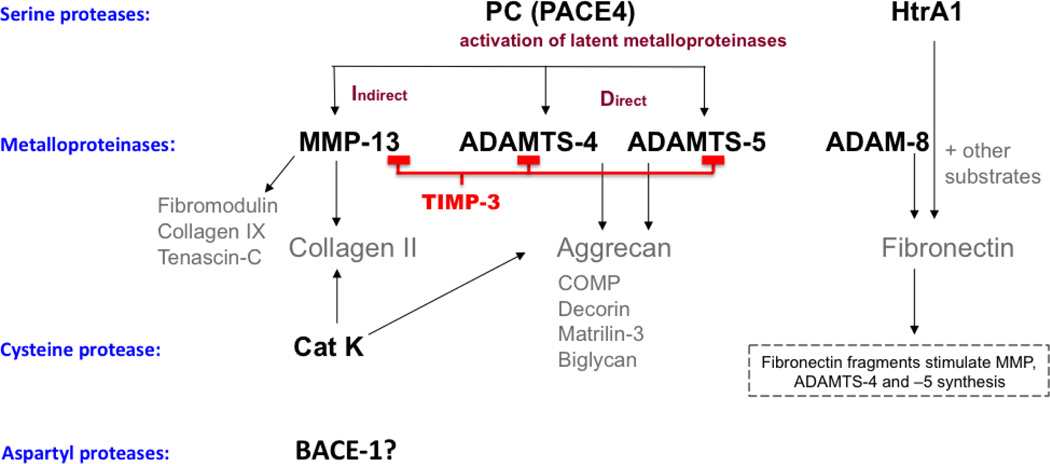
A Network of Proteases Is Active In Osteoarthritis
Progressive loss of articular cartilage through enzymatic degradation of the extracellular matrix (ECM) is central to OA pathology (for a detailed review of proteases in OA cartilage, see [5]). Focus has long been on metalloproteinases, because they are responsible for the degradation of the major macromolecules in cartilage, aggrecan and type II collagen (CII) (Fig. 1). From many older studies investigating the effects of broad-spectrum protease inhibitors on cytokinestimulated cartilage degradation in vitro, it is clear that not only metalloproteinases, but also serine and cysteine proteases, are involved in these pathways [6–8]. Figure 1 summarizes a network of the major proteases implicated in cartilage degradation, and reveals a prominent role for serine, metallo- and cysteine proteases. Protease research has mainly centered on cartilage degradation. Cartilage loss is radiologically manifested as joint space narrowing, which is the parameter by which OA progression is monitored and the primary endpoint for evaluating efficacy of disease-modifying OA drugs (DMOADs) [9]. However, cartilage damage is but a part of OA pathology, and it is not totally understood how changes in articular cartilage are related to changes in meniscus, subchondral bone, and synovium (recently well discussed in [10]). On a molecular level, proteases can be produced by tissues other than cartilage, and their degradation products may affect all joint tissues. It is, therefore, clearly important to study these proteases in vivo, and GeMMs provide a potent tool for validating their role in overall OA pathology and progression.
Figure 1. Network of proteases in OA cartilage degradation.
Key proteases from different classes are shown, mainly based on ex vivo human and bovine cartilage explant studies. ADAMTS-4/5 and MMP-13 are the main metalloproteases responsible for degrading aggrecan and type II collagen, respectively [79, 80]. These enzymes can also act on other putative substrates, the degradation of which may contribute to the weakening of the cartilage matrix [81]. These metalloproteases are synthesized as catalytically inactive zymogens, and it has been shown that the proforms of ADAMTS-4/5 are activated by proprotein convertases (PC) [82–84], with PACE4 identified as the major PC in human OA cartilage [78]. Tissue inhibitor of metalloprotease (TIMP)-3 is an endogenous inhibitor of MMP-13 [85] and ADAMTS-4/5 [86]. The cysteine protease, cathepsin K (catK), can also degrade collagen and aggrecan [87, 88]. ADAM8 can cleave fibronectin [89], as can HtrA1 (high temperature requirement A1) [90], and fibronectin fragments further induce the release of catabolic enzymes by chondrocytes [91–93]. HtrA1 can cleave many substrates in vitro, including aggrecan, fibromodulin, and decorin [94, 95]. To date, a role for aspartyl proteases has not been reported, although it was recently shown that selective inhibition of the membrane-anchored aspartyl protease, BACE-1 (beta-secretase), primarily known for its role in Alzheimer’s disease through cleavage of amyloid precursor protein, blocked cytokine-induced aggrecan loss from bovine and human cartilage explants. The mechanism of action is not yet understood [96].
Biochemical Characteristics Of OA Proteases
A brief overview of the key biochemical features of the major proteases in Fig. 1 is provided, in order to better understand how they function and cleave matrix proteins as well as the rationale and ongoing strategies for developing inhibitors against these enzymes.
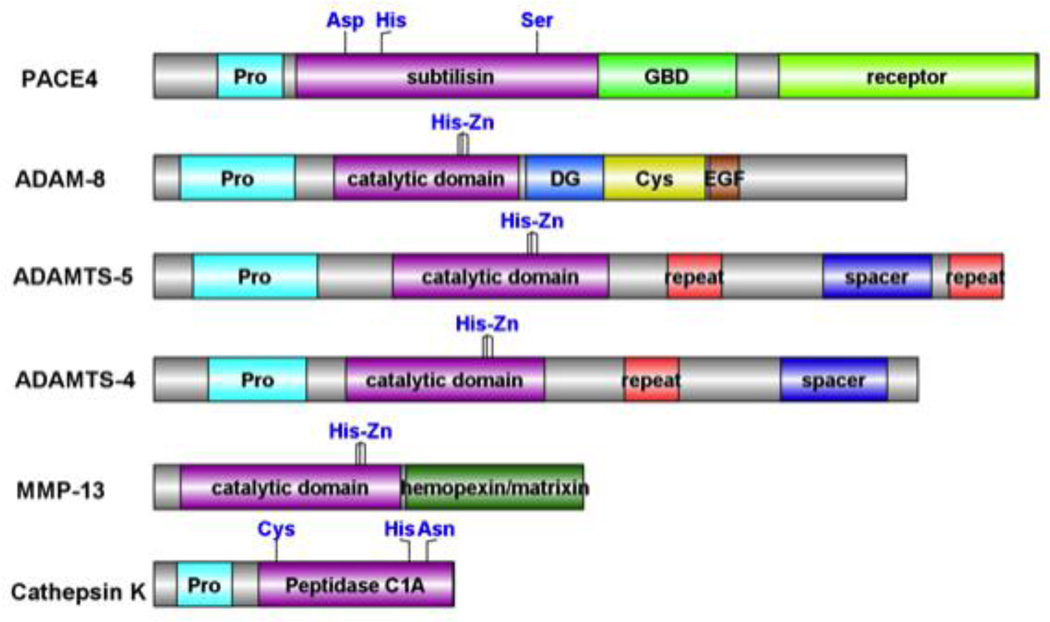
1. Domain Structure
Analysis of the domain structures of ADAMTS-4, ADAMTS-5, ADAM-8, MMP-13, catK and PACE-4 (Fig. 2) shows that these enzymes vary considerably in length, from about 330 amino acids (catK) to 970 amino acids (PACE4). The smaller enzymes like catK and MMP-13 contain fewer ancillary domains. CatK includes a propeptide domain and a peptidase C1 domain related to papain. Its active site contains cysteine, histidine and asparagine that make up its catalytic triad. Unlike the other enzymes, MMP-13 has a short propeptide domain, but it contains a typical metallopeptidase domain according to Pfam database (pfam.sanger.ac.uk) and a C-terminal hemopexin domain. ADAMTS-4 and ADAMTS-5 contain a propeptide and a catalytic domain and, in addition, an ADAMTS-spacer 1 domain and one or more thrombospondin type 1 repeats. For ADAM-8, there are three other domains, including a blood coagulation inhibitor/disintegrin segment, a cysteine-rich domain and an epidermal growth factor-like domain. Galactose-binding like domain and growth factor/receptor domains are found in PACE4, along with a pro-region and the subtilisin domain with the residues aspartic acid, histidine and serine as the catalytic triad. The size of the catalytic domain is similar for all the enzymes shown in Fig. 2 (200–250 residues), except for PACE4, which contains 340 residues. In general, larger enzymes contain more ancillary domains, which are important for matrix localization, substrate specificity, cell receptor signaling, and stability.
Figure 2. Domain structures of ADAMTS-4, ADAMTS-5, ADAM-8, MMP-13, cathepsin K and PACE4.
Pro, DG, Cys, EGF, and GBD indicate the propeptide, blood coagulation inhibitor/disintegrin, ADAM/cysteine-rich, epidermal growth factor-like domain and galactose-binding domain-like, respectively. The histidine-sites chelating zinc ion observed for ADAMTS-4, ADAMTS-5, ADAM-8, MMP-13 and the catalytic triad residues for cathepsin K and PACE4 are marked in blue. The sequence features were retrieved from the InterPro database of EMBL-EBI, and the accessions used included P29122 (PACE-4), P43235 (Cathepsin K), P78325 (ADAM-8), P45452 (MMP-13), Q9UNA0 (ADAMTS-5) and O75173 (ADAMTS-4). This graph was prepared using DOG [97].
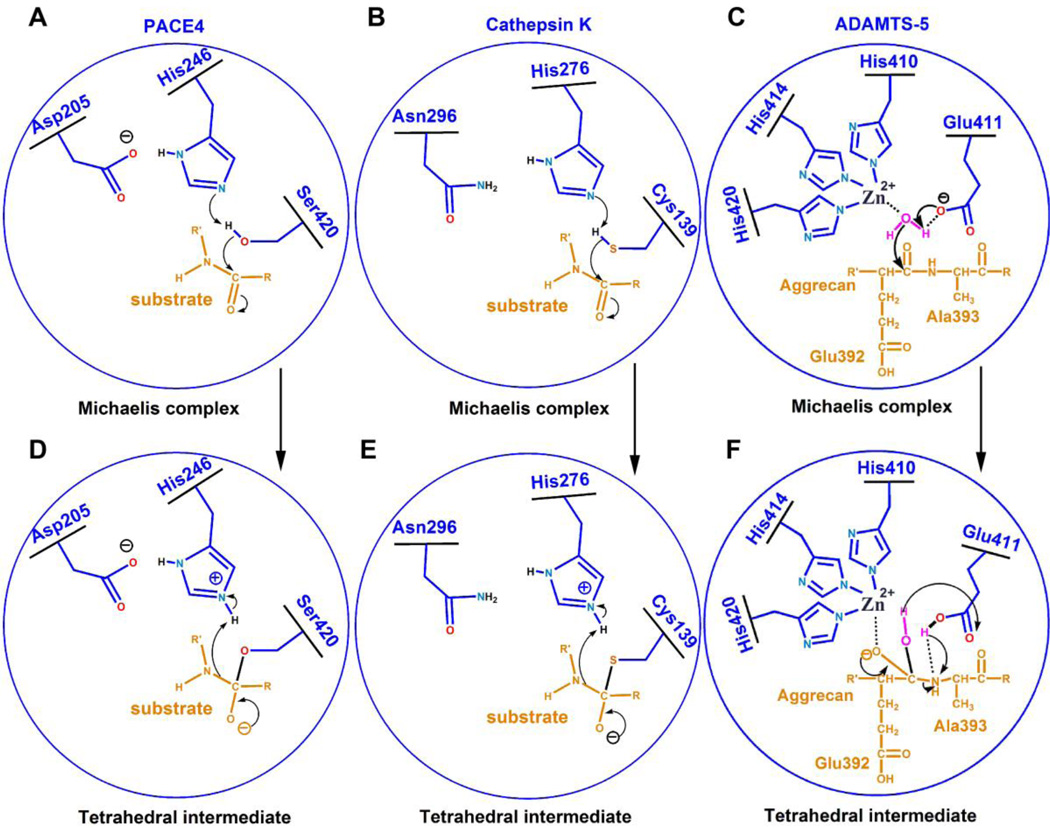
2. Mechanism Of Catalysis
All serine proteinases have a similar catalytic triad containing serine, histidine and aspartic acid. For PACE4, the catalytic triad is composed of Asp205, His246, and Ser420. A catalytic reaction by the serine protease PACE4 follows several steps, shown in Fig. 3A. First, the hydroxyl oxygen of Ser420 loses its hydrogen to His246. The nucleophilic oxygen attacks the scissile carbonyl bond, leading to the tetrahedral intermediate (Fig. 3D). Then, as the arrows indicate, the peptide bond is cleaved and the N-terminal portion of the substrate diffuses away. The remaining substrate is still temporarily covalently linked to Ser420, forming an acyl-enzyme intermediate. In the following step, a water molecule attacks the ester bond of the acyl-enzyme intermediate and a tetrahedral intermediate forms again. Finally, the tetrahedral intermediate disassembles, releasing the C-terminal portion of the substrate.
Figure 3. Schematic diagrams of the catalytic mechanism for serine-, cysteine- and metallo-proteinases.
The numbering of the residues involved in a catalytic reaction is in accord with PACE4 (serine proteinase, A and D), cathepsin K (cysteine proteinase, B and E) and ADAMTS-5 (metalloproteinase, C and F), respectively.
The catalytic mechanism of cysteine proteinases is very similar to serine proteinases except that its nucleophilic group is a mercapto sulfur of cysteine (Fig. 3B and E). The catalytic triad of catK is composed of Cys139, His276, and Asn296.
The catalytic mechanism of metalloproteinases is different from both serine and cysteine proteinases. Two mechanisms have been proposed, the promoted-water pathway and nucleophile pathway [11]. Fig. 3C and 3F show the promoted-water pathway for ADAMTS-5. First, the zinc-coordinated water loses one hydrogen atom to Glu411 and the nucleophilic oxygen of water attacks the scissile carbonyl bond, leading to the tetrahedral intermediate (as the arrows show in Fig. 3C and 3F). In this state, zinc links to the substrate carbonyl oxygen instead of the oxygen of water. Then, as the arrows indicate, the peptide bond is cleaved and the N-terminal portion of the substrate is lost. The remaining C-terminal portion of the substrate forms an enzyme product complex. Finally, the product will be released from the enzyme, which can start the next catalytic cycle.
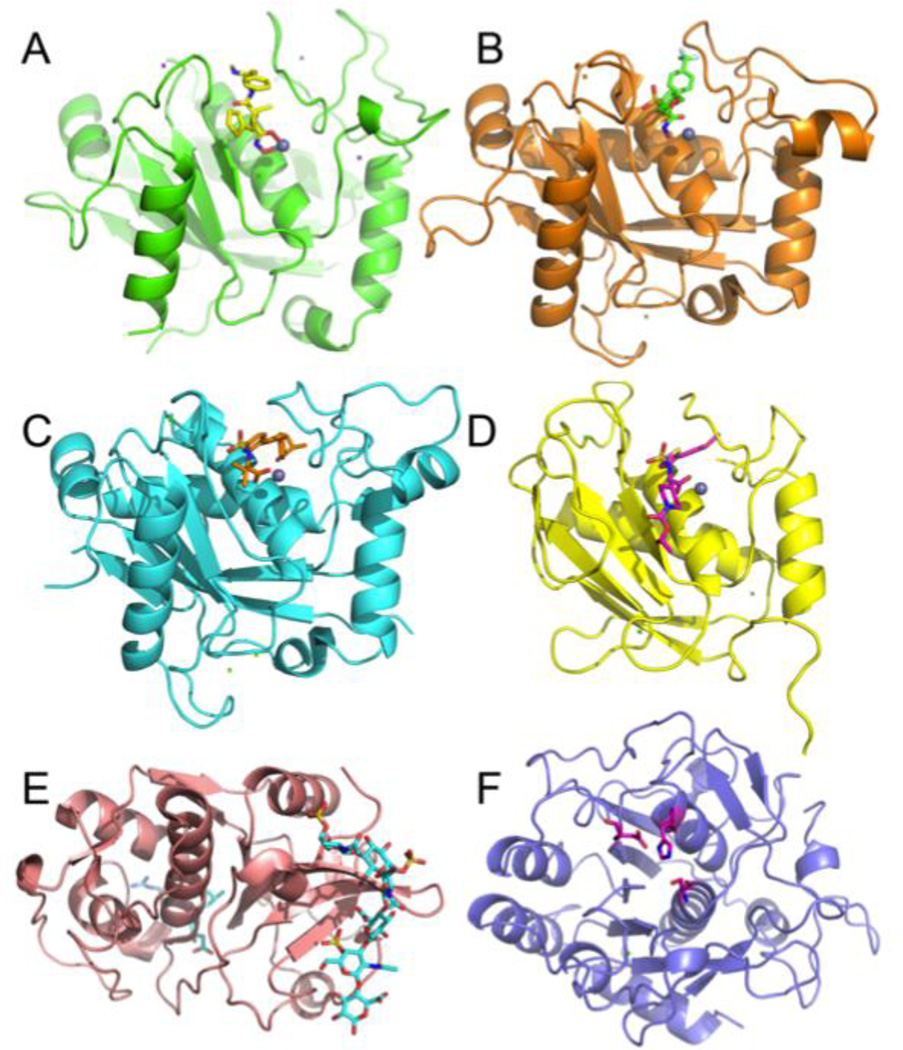
3. Active Site Structures
Many structures of the catalytic domain of the above proteases have been elucidated, except for PACE4 (Fig. 4). The size of the catalytic domains of ADAM-8, ADAMTS-4, ADAMTS-5, and catK are similar because of their similar sequence length. For MMP-13, the catalytic domain is smaller than the other proteases. Based on a homology model, PACE4 has the largest catalytic domain due to the greater number of amino acids that comprise it. Secondary structures and patterns of ADAM-8, ADAMTS-4, and ADAMTS-5 are similar (Fig. 4A–C), unlike MMP-13 (Fig. 4D), which has a different structural pattern. However, the active sites of these four metalloproteinases have considerable similarity, as they employ the same mechanism of peptide hydrolysis (Fig. 3). ADAM-8, ADAMTS-4, and ADAMTS-5 all have an α-helix, which forms the base of the active site. There is also an α-helix and several loops located at the right-hand side of the ligand. MMP-13 lacks the α-helix. As for catK and PACE4, the active sites are very different. These differences are expected as they are different classes of proteinases. Although ADAM-8, ADAMTS-4, ADAMTS-5, and MMP-13 share similar tertiary structures, the active site pockets have different properties in terms of size, shape, hydrophobicity and electrostatic potential (data not shown). These different properties determine the preference for different compounds (ligands) [12–14]. Thus, there is an opportunity to design potent and, more importantly, selective inhibitors against each of these proteases, even if they are closely related. Of course, it must be taken into consideration that proteins are not totally rigid; on the contrary, they can take different conformations to accommodate different ligands [13]. That is the reason why one compound can bind to several target proteins, and also why the development of selective inhibitors targeting only one member within a family is challenging.
Figure 4. 3D crystal structures of the catalytic domains of ADAMTS-4, ADAMTS-5, ADAM-8, MMP-13, Cathepsin K and PACE-4.
Proteins are displayed as ribbons, ligands and zinc ions are represented as sticks and gray spheres, respectively. The model of PACE4 is built using SWISS-MODEL [98]. PACE4A-I was chosen as the target sequence and the crystal structure of furin (PDB code: 1P8J) [99] was used to model PACE4. A-F display the structures of ADAM-8, ADAMTS-5, ADAMTS-4, MMP-13, cathepsin K and PACE4A-I, respectively. The catalytic triad residues of PACE4A-I are shown as sticks. The PDB codes used were 4DD8 (ADAM-8) [100], 3C9E (Cathepsin K) [101], 3ELM (MMP-13) [12], 2RJP (ADAMTS-4) [102], 3B8Z (ADAMTS-5) [103]. The graphs were prepared using PyMOL [104].
Mouse Models Confirm the Importance of Proteases in OA
The mouse degradome is larger than the human degradome, particularly in proteases related to immunological and reproductive functions, and is missing some key enzymes such as MMP-1 [15]. Despite this, mouse models of OA are invaluable for target validation, largely due to the availability of knockout (KO) mice [16]. For the purposes of this review, we focused on GeMMs and expression studies performed in surgical and spontaneous models of murine OA, since these are the models most commonly utilized (for review of the models, see [17]).
1. Validation in Genetically Engineered Mouse Models (GeMMs)
Surgical Models
The majority of protease KO mice have been tested in surgical models (Table 1). OA triggered by destabilization of the medial meniscus (DMM), in particular, provides an opportunity for long-term follow-up due to the slow progression of structural changes in the joint [18]. Inhibition of cartilage degradation remains the main criterion for concluding whether or not particular KO mice are protected from OA, but increasingly subchondral bone changes are included in analyses. The role of synovial change in these models is under active investigation. Of the 8 proteases and endogenous inhibitors tested, Timp2 [19] and Mmp9 [20, 16] deficient mice are more susceptible to OA. The loss of Timp2 promotes vascular invasion of the periarticular region prior to the development of OA changes, suggesting that increased angiogenesis may drive OA progression [19]. It was postulated that MMP-9 plays a protective role in OA, due its known anti-inflammatory functions, including its ability to degrade IL-1β [16]. The lack of Adamts4 [21], Mmp3 [16], Mmp12 [16], or Mmp17 [22] does not influence OA progression. MMP-17 (also known as MT4-MMP) was tested because it may be involved in activating ADAMTS-4 [23]. It is interesting to note that although Mmp17 null mice showed no protection in the DMM model, they were protected from glycosaminoglycn (GAG) loss into the synovial fluid after intra-articular injection of IL-1β, suggesting that MMP-17 may play a role in joint destruction in an inflammatory situation [22]. Only three KO strains, Adamts5, Mmp13, and catK (Ctsk) null mice, are protected against OA development, although 100% protection against cartilage degeneration was never reported.
Table 1.
Surgical Murine Models of Osteoarthritis
| KO/TG | STRAIN OF MICE |
MODEL | TIME POINT POST SURGERY |
TISSUES STUDIED |
FINDINGS | REF |
|---|---|---|---|---|---|---|
| Adamts4 ko (aggrecanase 1) | 129SvEv-Brd | destabilization of the medial meniscus (DMM) surgery | 4, 8 weeks | cartilage |
|
Glasson 2004 |
| Adamts5 ko (aggrecanase 2) | 129SvEv-Brd | DMM | 4 weeks, 8 weeks, 6 months | cartilage, subchondral bone |
|
Glasson 2005; Botter 2009 |
| Adamts4/5 double ko | 129SvEv-Brd | DMM | 8 weeks, 6 months | cartilage |
|
Majumdar 2007 |
| aggrecan-knockin (Chloe, MMP resistant) | C57BL/6 | DMM | 4, 8 weeks | cartilage |
|
Little 2005, Little 2007 |
| aggrecan-knockin (Jaffa, ADAMTS resistant) | C57BL/6 | DMM | 4, 8 weeks | cartilage |
|
Little 2007 |
| Timp2 ko | C57BL/6J | destabilized by partial resection of the medial meniscus | 1, 4 months | bone, vasculature, cartilage |
|
Mi 2012 |
| Mmp3 ko (Str1 ko) | C57BL10 | DMM | 8 weeks | cartilage |
|
Glasson 2007 |
| Mmp9 ko | FVB/N | DMM | 8 weeks | cartilage |
|
Glasson 2005 ORS; Glasson 2007 |
| Mmp12 ko | C57BL/6 | DMM | 8 weeks | cartilage |
|
Glasson 2007 |
| Mmp13 ko | FVBN | DMM | 4, 8 weeks | cartilage, bone |
|
Little 2009 |
| Mmp13Col2ER | C57BL/6j | transection of medial collateral ligament and partial removal of the medial meniscus | 8, 12, 16 weeks | cartilage |
|
Wang 2013 |
| Mmp13 overexpressing | FVB/N | DMM | 4, 8 weeks | cartilage, synovium |
|
Glasson 2007 |
| Mmp17 ko (MT4MMP ko) | C57BL6 | DMM | 8 weeks | cartilage |
|
Clements 2011 |
| Ctsk ko | 129SVJ-C57BL/6J | ACLT | 16 weeks | cartilage, bone |
|
Hayami 2012 |
| 129/SV × C57BL/6 | partial resection of the medial meniscus and transection of the MCL and ACL | 8 weeks | cartilage, bone |
|
Kozawa 2012 |
Histological scores were assigned to four quadrants (medial tibial plateau, medial femoral condyle, lateral tibial plateau, and lateral femoral condyle) of the left and right knee joints at all sectioned levels to obtain a summed OA score for the whole knee joint, or for the medial and lateral tibial plateau separately
Adamts5 null mice are protected from aggrecan loss and cartilage degradation after instability induced by DMM surgery [24]. Protection from cartilage degradation and subchondral bone remodeling has been demonstrated as far out as six months after DMM, but these mice were not protected from osteophyte development [25, 24]. Adamts4/5 null mice show similar protection against cartilage degeneration as Adamts5 null mice [26]. Two transgenic mouse strains have also been developed in order to compare the roles of MMP and ADAMTS cleavage in the interglobular domain (IGD) of aggrecan. Chloe mice are resistant to cleavage by MMPs at the Asn341-Phe342 site [27], while Jaffa mice are resistant to ADAMTS cleavage at the Glu373-Ala374 site [28]. In the DMM model, Chloe mice developed OA similar to WT mice, while Jaffa mice showed similar protection from cartilage degradation as Adamts5 null mice [24, 28]. This suggests that blocking ADAMTS-mediated cleavage in the aggrecan IGD alone is sufficient for protecting against cartilage erosion.
Mmp13 null mice were not protected from aggrecan loss after DMM, but in spite of this, they suffered significantly less cartilage damage up to 8 weeks following surgery [29]. These mice actually developed localized proteoglycan depletion on the femoral side, but this did not result in increased structural damage. On the contrary, cartilage structure was preserved in Mmp13 KO mice, demonstrating the importance of collagen cleavage to the loss of cartilage tissue in OA [29]. Similarly, cartilage-specific Mmp13-deficient mice were protected against cartilage degeneration in a different joint instability model up to 16 weeks post surgery [30]. These were Mmp13 null crossed with Col2CreER transgenic mice, Mmp13Col2ER, and it may be worth noting that the Col2a1-Cre mouse also alters gene expression in synovial fibroblasts and not just in chondrocytes [31]. Conversely, DMM in Mmp13 overexpressing mice resulted in accelerated cartilage degradation [16], further confirming the crucial role of this protease in OA. A variety of transcription factors (NF-κB, HIF2α, Ihh, Runx2, ELF3, C/EBPβ, and AP-1) have been implicated in the regulation of MMP-13, but it is not yet understood how each of these factors participates in OA pathogenesis [32, 5, 33]. HIF2α deficient mice (Epas1+/−) and Runx2+/− mice are protected against cartilage degradation [34] and osteophyte formation in joint instability models [35, 36]. These studies reinforce the importance of MMP-13 in the pathogenesis of OA, but the factors regulating its transcription do not likely themselves represent viable drug targets due to their widespread biological activities.
Ctsk null mice develop osteopetrosis, with higher bone mineral content and higher bone volume by two months of age [37]. By 25 weeks of age, these increases were still apparent in the tibial metaphysis, but the subchondral bone appeared to be unaffected [38]. In two different models, Ctsk null mice were protected against cartilage degradation and subchondral bone changes up to 16 weeks after surgery, although osteophytosis was not significantly reduced [39, 38]. Eight weeks after partial medial menisectomy, wild-type mice expressed catK in chondrocytes and synovium [38]. Ctsk null mice showed a hint of protection against osteophyte formation, but this was not analyzed for statistical significance [38].
Spontaneous OA
Mice are susceptible to naturally occurring OA of the knee joints to varying degrees depending on background strain [40]. Slowly progressive natural OA in C57Bl/6 mice has been studied in some detail [41, 42]. In analyses of articular cartilage integrity, chondrocyte cell death, and subchondral bone up to 23 months of age, the joint changes were comparable to those seen 5.5 months after DMM surgery, but with lower incidence and development of osteophytes [41].
Among the transgenic mice studied for progression of spontaneous OA, mice deficient in Adam15 [43], Mmp2 [44], or Mmp14 [45] develop more rapid osteoarthritis compared to WT mice (Table 2). Mmp3 null mice show similar development of OA as WT (B10.RIII) mice by one year of age, but by two years, they have significantly less cartilage degeneration; there was no significant difference in fibrosis or in synovial infiltration [46]. Remarkably, there is no report in the literature yet on susceptibility of Adamts4, Adamts5, or Mmp13 null mice to spontaneous OA, so it is not possible to compare the relative protection to that in the Mmp3 null mice. In addition, Ctsk null mice have only been evaluated out to 25 weeks of age, which is not long enough for spontaneous OA to develop in the matched WT mice [38]. There are, however, data that confirm indirectly the key roles of these proteases: mice that lack TIMP-3, an endogenous inhibitor of ADAMTS-4/5 and MMP-13, develop earlier proteoglycan loss during the aging process [47]. In mice overexpressing hMmp13, OA developed more rapidly [48], although another group could not repeat these results [16]. Ctsk overexpressing mice were found to develop progressive synovitis with age, resulting in synovial hyperplasia, fibrosis, and joint destruction [49].
Table 2.
Murine Models of Spontaneous Osteoarthritis
| KO/TG | STRAIN OF MICE |
MODEL | TIME POINT | TISSUES STUDIED |
FINDINGS | REF |
|---|---|---|---|---|---|---|
| aggrecan-knockin (Jaffa, ADAMTS resistant) | C57BL/6 | aging | 12 months old | cartilage, bone |
|
Little 2007 |
| Adam15 ko (metargidin) | 129/SvJ | aging | 3-, 6-, 12–14-months old | cartilage, bone, synovium, meniscus, tendons, ligaments |
|
Bohm 2005 |
| Timp3 ko | C57BL/6 | aging | 4 weeks to 24 months old | cartilage, meniscus |
|
Sahebjam 2007 |
| Mmp2 ko | C57BL/6J | aging | up to 6 months old | cartilage, bone |
|
Mosig 2007 |
| Mmp3 ko (Str1) ko | B10.RIII | aging | 1, 2 years old | cartilage, bone, synovium |
|
Blom 2007 |
| Mmp13 overexpressing | FVB/N | aging | 5 months old | cartilage, synovium |
|
Neuhold 2001 |
| Mmp13 overexpressing | FVB/N | aging | 20 weeks old | cartilage |
|
Glasson 2007 |
| Mmp14 ko (MT1-MMP) ko | Swiss Black mice | aging | up to day 40 | joints |
|
Holmbeck 1999 |
| Ctsk overexpressing | FVB/N | aging | 7, 12 months old | cartilage, synovium |
|
Morko 2005 |
Other models
The roles of some of these enzymes have been studied in models of acute inflammation. Adamts5 null mice are protected from cartilage proteoglycan loss, but not from synovitis, in the acute phase of the inflammatory antigen-induced arthritis (AIA) model (day 3) [50]. Jaffa mice also demonstrate early protection from cartilage proteoglycan loss in the AIA model (days 1–5), but by day 7, they develop cartilage erosion similar to Chloe and WT mice with extensive proteoglycan loss in all genotypes. Between days 7 and 28, however, Jaffa mice show an ability to initiate proteoglycan restoration, resulting in significantly lower cartilage erosion scores [28]. Together with the results from the DMM model, these findings offer a compelling reason to believe that blocking aggrecanolysis in the IGD domain may be beneficial throughout the pathogenesis of OA; it may slow down progressive cartilage erosion and may also offer a chance at repair.
Adamts5 null mice are protected from proteoglycan loss and development of fibrosis on the surfaces of the knee joint tissues in a model of joint deterioration induced by intra-articular injection of TGF-β1 and treadmill running [51], suggesting that ADAMTS-5 may also play a role in fibrosis.
The remaining proteases in the proposed scheme, PACE4, ADAM8, and HtrA1, provide compelling justification for testing their roles in OA pathogenesis using GeMM. These experiments, however, are not yet in the public domain. Transgenic mice overexpressing a catalytically inactive mutant of Adam8 develop significantly less bone resorption, inflammation, and cartilage degradation in the collagen-induced arthritis model, compared to WT mice [52]. HtrA1 has been postulated to participate in degradation of the pericellular matrix in response to biomechanical stress, which exposes the receptor tyrosine kinase DDR2 to its ligand, native CII, and triggers release of MMP-13 [53]. This may be a mechanism by which Ddr2+/− mice show attenuated progression of OA after DMM surgery [54]. Data in Htra1-deficient mice are not available.
2. Murine Expression Data
The year 2012 witnessed the publication of several microarray expression studies in murine OA models [55–57]. In one study, expression patterns in articular cartilage of aging STR/Ort mice, which are spontaneously susceptible to OA-like changes [57], revealed that many of the proteases that are thought to play roles in human OA were upregulated in STR/Ort articular cartilage, amongst them many of those listed in Fig 1. The authors combined data from OA mice at 18 and 40 weeks of age and showed that the following protease-related genes were significantly upregulated when compared with non-OA samples: Adam8, Adamts1, Adamts4, Ctsk, Htra1, Mmp2, Mmp3, Mmp13, Mmp14, Timp1, Timp2, and Timp3 - thus largely confirming the networks that were dissected through years of research in isolated cartilage from several species including human OA. Additional upregulated protease genes included Capn6 (Calpain-6), Dpp7 (dipeptidylpeptidase 7), Mmp19, and Prss23 (protease serine 23); and a few were downregulated, including Dpep1 (dipeptidase 1), and Gzma (granzyme A).
A second microarray study [56] analyzed gene expression in whole knee joint samples, comparing samples taken 8 weeks post DMM, where surgery had been performed in young mice (12 weeks of age) or in 12-month old mice, which develop a more severe disease. Fewer significant changes in protease-related genes were reported, but Htra1, Mmp2, Mmp3, and Timp1 were upregulated in both young and old mice; Pcsk5, which encodes the proprotein convertase PC5/6A, was upregulated in old mice, but not in young mice.
Finally, another study analyzed samples taken from whole knee joint extracts 6 hours and 4 weeks post DMM [55]. Six hours after surgery, the following protease-related genes were upregulated compared to sham mice: Timp1, Mmp3, Adamts1, Adamts4, Mmp19, and Adamts5. Timp1 and Mmp3 were still increased 4 weeks post DMM. Follow-up qRT-PCR studies showed that Adamts5 and Mmp3, 6 h after surgery, were up in cartilage but not in meniscus or in bone. In addition, joint immobilization by sciatic neurectomy, which inhibited movement in the operated limb and protected against development of OA, abrogated the responses of selected genes, including Adamts5, Adamts1 and Adamts4, in whole knee extracts six hours post surgery.
These expression studies in diverse murine models confirm that proteases are tightly regulated throughout all stages of OA (as early as 6 hours after surgery and up to 40 weeks in ageing STR/ort mice). Studies like this will enable researchers to dissect the roles of proteases over time and evaluate differences with age, and in different tissues. It is possible that protease expression in other tissues contributes to OA pathogenesis. In this respect, an interesting study exploring the effect of high-fat diet (HFD) on 8-wk-old male B6 mice found a highly variable obesity when these genetically identical mice were fed a HFD [58]. Micro-array and RT-PCR analysis of adipose tissues revealed that one of the genes overexpressed in the high compared to the low weight-gainers was Adamts5. In independent studies, it was shown that the “high-gainer” mice developed more Safranin-O staining loss than the “low-gainer” mice fed a HFD [59]. This indicates that induction of ADAMTS-5 in other tissues (outside the joint?) may contribute to OA development. To our knowledge, obesity-induced OA has not been tested in Adamts5 null mice.
3. Proof of Concept Studies with Selective Inhibitors
To date, studies in GeMMs have narrowed protease targets down to three enzymes that are critical for development of overall joint damage in OA: ADAMTS-5, MMP-13, and catK.
In vivo studies with selective small molecule inhibitors targeting these proteases have been performed in various animal models, but in general, the information is quite limited, especially for ADAMTS-5. Wyeth’s ADAMTS-4/5 inhibitor was shown to protect against cartilage degeneration and changes in weight-bearing in the rat medial meniscal tear model [60], but no mouse data are available for this compound. Phase 1 clinical trials have been completed and revealed no safety issues (NCT00427687, NCT00454298) (www.clinicaltrials.gov). As a promising alternative approach to small molecule inhibition, GlaxoSmithKline recently reported a neutralizing anti-ADAMTS-5 antibody [61]. When administered prophylactically to mice over 8 weeks post DMM, the antibody was shown to protect against joint damage [62, 61]. In addition, the antibody was shown to fully penetrate mouse cartilage when administered intraperitoneally to mice six weeks post DMM surgery [62]. Therapeutic efficacy of the antibody on established OA was not reported.
MMP inhibitor development has been hindered by non-specificity and resulting musculoskeletal syndrome (MSS) [63]. Studies of more selective inhibitors targeting MMP-13 have not reported these issues, and they appear to offer protection from cartilage loss in a variety of different species [64–67], and to prevent pain behaviors in rats [64, 68]. In a recent study using a murine joint instability model, an MMP-13 inhibitor was able to slow down cartilage loss, when administered at the time of surgery, up to 12 weeks follow-up [30]. Again, therapeutic protocols have not yet been reported, and no MMP-13 inhibitor has reached clinical trial to date.
Studies with catK inhibitors in OA models in species other than mice have shown beneficial effects, not only on structural progression of disease [69, 39], but also on joint pain in long-term spontaneous OA in Dunkin-Hartley guinea pigs [70]. Novartis has recently completed three phase 2 clinical trials testing balicatib (AAE581), a catK inhibitor, for safety and efficacy in osteoporosis [71] and in knee OA (NCT00170911, NCT00100607, and NCT00371670). Patients with painful knee OA (KL Grade 3) were tested in a 12-month placebo-controlled trial to evaluate safety, tolerability, and disease modifying efficacy of daily oral treatment. Results from this study have not been posted to date.
Conclusions And Future Challenges
GeMMs have been used for protease gain-of-function and loss-of-function experiments, but inhibitor studies have largely been performed in other species. Murine models, the DMM model in particular, offer the advantage that they are slowly progressive and thus enable exploring therapeutic efficacy at different stages during OA progression. Testing compounds targeting ADAMTS-5, MMP-13, and catK in these models will provide insight into their therapeutic efficacy on established OA. Time-course experiments may inform us whether there is an optimal window of opportunity for pharmacological modulation, and if and when there is a point of no return.
Structural damage to the joint is essentially what defines OA, but what matters to the patient are the symptoms that accompany this joint failure, most notably pain. It remains to be seen whether halting structural progression will be accompanied by alleviating pain. Approaches to model OA pain in mice are being developed [72] and may offer a tremendous opportunity to address this major gap in our understanding of OA as a complex disease entity. It was recently shown that Adamts-5 deficient mice are protected from mechanical allodynia after DMM surgery [73]. This may simply be a consequence of the fact that they are protected from developing OA in this model, but may also reflect a direct role for ADAMTS-5 in the nervous system. Adamts5 is expressed in dorsal root ganglia in adult mice [74]. Over the last decade, proteases, particularly MMPs, have been implicated increasingly in mediating inflammation due to their ability to cleave cytokines, chemokines, and receptors, in addition to degrading ECM [75]. It is recognized that generating pain requires interaction between the immune and nervous systems (reviewed in [76]). Therefore, it seems likely that MMPs and other proteases may participate in the development and maintenance of pain. A polymorphism in the gene encoding PACE4 (PCSK6) was strongly associated with protection against pain in knee OA in a multi-cohort study [77] and Pcsk6 null mice were protected against pain in a battery of tests [77]. Since PACE4 is also the main activator of the pro-aggrecanases in human OA cartilage [78], this might suggest that there are indeed common pathways for structural progression and pain mechanisms in OA.
A putative role for proteases in mouse models of OA pain has not yet been studied, but proteases may constitute a promising area for addressing the intersection between structural damage and pain.
Acknowledgments
Rachel E. Miller is supported by an Arthritis Foundation Post-Doctoral Fellowship. Anne-Marie Malfait is supported by Grant R01AR060364 from the National Institutes of Health/National Institute of Arthritis and Musculoskeletal and Skin Diseases. The funding agencies had no role in the preparation of this manuscript.
The articles cited in this review were selected from the authors’ personal libraries of articles and from PubMed searches using the keywords “osteoarthritis,” “proteases,” “inhibitors,” and “animal models.” Selections were made on the basis of the expert opinions of the authors. Searches were performed through December 2012.
Footnotes
Compliance with Ethics Guidelines
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
Anne-Marie Malfait and Micky D. Tortorella were previously employed by Pfizer. Anne-Marie Malfait is an associate editor of Osteoarthritis and Cartilage (Elsevier).
Rachel E. Miller and Yongzhi Lu declare that they have no conflict of interest.
References
- 1.Lopez-Otin C, Overall CM. Protease degradomics: a new challenge for proteomics. Nat Rev Mol Cell Biol. 2002;3(7):509–519. doi: 10.1038/nrm858. [DOI] [PubMed] [Google Scholar]
- 2.Lopez-Otin C, Bond JS. Proteases: multifunctional enzymes in life and disease. J Biol Chem. 2008;283(45):30433–30437. doi: 10.1074/jbc.R800035200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Drag M, Salvesen GS. Emerging principles in protease-based drug discovery. Nat Rev Drug Discov. 2010;9(9):690–701. doi: 10.1038/nrd3053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Loeser RF, Goldring SR, Scanzello CR, Goldring MB. Osteoarthritis: a disease of the joint as an organ. Arthritis Rheum. 2012;64(6):1697–1707. doi: 10.1002/art.34453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Troeberg L, Nagase H. Proteases involved in cartilage matrix degradation in osteoarthritis. Biochim Biophys Acta. 2012;1824(1):133–145. doi: 10.1016/j.bbapap.2011.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Milner JM, Rowan AD, Elliott SF, Cawston TE. Inhibition of furin-like enzymes blocks interleukin-1alpha/oncostatin M-stimulated cartilage degradation. Arthritis Rheum. 2003;48(4):1057–1066. doi: 10.1002/art.10873. [DOI] [PubMed] [Google Scholar]
- 7.Sondergaard BC, Henriksen K, Wulf H, Oestergaard S, Schurigt U, Brauer R, et al. Relative contribution of matrix metalloprotease and cysteine protease activities to cytokine-stimulated articular cartilage degradation. Osteoarthritis Cartilage. 2006;14(8):738–748. doi: 10.1016/j.joca.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 8.Milner JM, Patel A, Rowan AD. Emerging roles of serine proteinases in tissue turnover in arthritis. Arthritis Rheum. 2008;58(12):3644–3656. doi: 10.1002/art.24046. [DOI] [PubMed] [Google Scholar]
- 9.Le Graverand-Gastineau MP. Disease modifying osteoarthritis drugs: facing development challenges and choosing molecular targets. Curr Drug Targets. 2010;11(5):528–535. doi: 10.2174/138945010791011893. [DOI] [PubMed] [Google Scholar]
- 10. Little CB, Fosang AJ. Is cartilage matrix breakdown an appropriate therapeutic target in osteoarthritis--insights from studies of aggrecan and collagen proteolysis? Curr Drug Targets. 2010;11(5):561–575. doi: 10.2174/138945010791011956. Provides a good discussion on the relationship between cartilage structural integrity and pathology in other tissues in the OA joint.
- 11.Wu S, Zhang C, Xu D, Guo H. Catalysis of carboxypeptidase A: promoted-water versus nucleophilic pathways. J Phys Chem B. 2010;114(28):9259–9267. doi: 10.1021/jp101448j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Monovich LG, Tommasi RA, Fujimoto RA, Blancuzzi V, Clark K, Cornell WD, et al. Discovery of potent, selective, and orally active carboxylic acid based inhibitors of matrix metalloproteinase-13. J Med Chem. 2009;52(11):3523–3538. doi: 10.1021/jm801394m. [DOI] [PubMed] [Google Scholar]
- 13. Shieh HS, Tomasselli AG, Mathis KJ, Schnute ME, Woodard SS, Caspers N, et al. Structure analysis reveals the flexibility of the ADAMTS-5 active site. Protein Sci. 2011;20(4):735–744. doi: 10.1002/pro.606. First demonstration that the active site of ADAMTS-5 can undergo an induced conformational change by a small molecule may enable the design of inhibitors with improved potency and selectivity profiles.
- 14.Tortorella MD, Tomasselli AG, Mathis KJ, Schnute ME, Woodard SS, Munie G, et al. Structural and inhibition analysis reveals the mechanism of selectivity of a series of aggrecanase inhibitors. J Biol Chem. 2009;284(36):24185–24191. doi: 10.1074/jbc.M109.029116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Puente XS, Sanchez LM, Overall CM, Lopez-Otin C. Human and mouse proteases: a comparative genomic approach. Nat Rev Genet. 2003;4(7):544–558. doi: 10.1038/nrg1111. [DOI] [PubMed] [Google Scholar]
- 16.Glasson SS. In vivo osteoarthritis target validation utilizing genetically-modified mice. Curr Drug Targets. 2007;8(2):367–376. doi: 10.2174/138945007779940061. [DOI] [PubMed] [Google Scholar]
- 17.Little CB, Smith MM. Animal Models of Osteoarthritis. Curr Rheumatol Rev. 2008;4(3):175–182. [Google Scholar]
- 18.Glasson SS, Blanchet TJ, Morris EA. The surgical destabilization of the medial meniscus (DMM) model of osteoarthritis in the 129/SvEv mouse. Osteoarthritis Cartilage. 2007;15(9):1061–1069. doi: 10.1016/j.joca.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 19.Mi M, Shi S, Li T, Holz J, Lee YJ, Sheu TJ, et al. TIMP2 deficient mice develop accelerated osteoarthritis via promotion of angiogenesis upon destabilization of the medial meniscus. Biochem Biophys Res Commun. 2012;423(2):366–372. doi: 10.1016/j.bbrc.2012.05.132. [DOI] [PubMed] [Google Scholar]
- 20.Glasson S, Blanchet T, Morris EA. Less Severe OA is Observed in IL-1b KO Mice and More Severe OA is Observed in MMP-9 and MK2 KO Mice in a Surgical Model of OA. ORS 51st Annual Meeting; Feb 20–23; Washington, DC. 2005. p. 0251. [Google Scholar]
- 21.Glasson SS, Askew R, Sheppard B, Carito BA, Blanchet T, Ma HL, et al. Characterization of and osteoarthritis susceptibility in ADAMTS-4-knockout mice. Arthritis Rheum. 2004;50(8):2547–2558. doi: 10.1002/art.20558. [DOI] [PubMed] [Google Scholar]
- 22.Clements KM, Flannelly JK, Tart J, Brockbank SM, Wardale J, Freeth J, et al. Matrix metalloproteinase 17 is necessary for cartilage aggrecan degradation in an inflammatory environment. Ann Rheum Dis. 2011;70(4):683–689. doi: 10.1136/ard.2010.130757. [DOI] [PubMed] [Google Scholar]
- 23.Gao G, Plaas A, Thompson VP, Jin S, Zuo F, Sandy JD. ADAMTS4 (aggrecanase-1) activation on the cell surface involves C-terminal cleavage by glycosylphosphatidyl inositol-anchored membrane type 4-matrix metalloproteinase and binding of the activated proteinase to chondroitin sulfate and heparan sulfate on syndecan-1. J Biol Chem. 2004;279(11):10042–10051. doi: 10.1074/jbc.M312100200. [DOI] [PubMed] [Google Scholar]
- 24.Glasson SS, Askew R, Sheppard B, Carito B, Blanchet T, Ma HL, et al. Deletion of active ADAMTS5 prevents cartilage degradation in a murine model of osteoarthritis. Nature. 2005;434(7033):644–648. doi: 10.1038/nature03369. [DOI] [PubMed] [Google Scholar]
- 25.Botter SM, Glasson SS, Hopkins B, Clockaerts S, Weinans H, van Leeuwen JP, et al. ADAMTS5−/− mice have less subchondral bone changes after induction of osteoarthritis through surgical instability: implications for a link between cartilage and subchondral bone changes. Osteoarthritis Cartilage. 2009;17(5):636–645. doi: 10.1016/j.joca.2008.09.018. [DOI] [PubMed] [Google Scholar]
- 26.Majumdar MK, Askew R, Schelling S, Stedman N, Blanchet T, Hopkins B, et al. Doubleknockout of ADAMTS-4 and ADAMTS-5 in mice results in physiologically normal animals and prevents the progression of osteoarthritis. Arthritis Rheum. 2007;56(11):3670–3674. doi: 10.1002/art.23027. [DOI] [PubMed] [Google Scholar]
- 27.Little CB, Meeker CT, Hembry RM, Sims NA, Lawlor KE, Golub SB, et al. Matrix metalloproteinases are not essential for aggrecan turnover during normal skeletal growth and development. Mol Cell Biol. 2005;25(8):3388–3399. doi: 10.1128/MCB.25.8.3388-3399.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Little CB, Meeker CT, Golub SB, Lawlor KE, Farmer PJ, Smith SM, et al. Blocking aggrecanase cleavage in the aggrecan interglobular domain abrogates cartilage erosion and promotes cartilage repair. J Clin Invest. 2007;117(6):1627–1636. doi: 10.1172/JCI30765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Little CB, Barai A, Burkhardt D, Smith SM, Fosang AJ, Werb Z, et al. Matrix metalloproteinase 13-deficient mice are resistant to osteoarthritic cartilage erosion but not chondrocyte hypertrophy or osteophyte development. Arthritis Rheum. 2009;60(12):3723–3733. doi: 10.1002/art.25002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang M, Sampson ER, Jin H, Li J, Ke QH, Im HJ, et al. MMP13 is a Critical Target Gene During the Progression of Osteoarthritis. Arthritis Res Ther. 2013 doi: 10.1186/ar4133. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fosang AJ, Golub SB, East CJ, Rogerson FM. Abundant LacZ activity in the absence of Cre expression in the normal and inflamed synovium of adult Col2a1-Cre; ROSA26RLacZ) reporter mice. Osteoarthritis Cartilage. doi: 10.1016/j.joca.2012.11.013. In press. [DOI] [PubMed] [Google Scholar]
- 32.Goldring MB, Otero M, Plumb DA, Dragomir C, Favero M, El Hachem K, et al. Roles of inflammatory and anabolic cytokines in cartilage metabolism: signals and multiple effectors converge upon MMP-13 regulation in osteoarthritis. Eur Cell Mater. 2011;21:202–220. doi: 10.22203/ecm.v021a16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Husa M, Liu-Bryan R, Terkeltaub R. Shifting HIFs in osteoarthritis. Nat Med. 2010;16(6):641–644. doi: 10.1038/nm0610-641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang S, Kim J, Ryu JH, Oh H, Chun CH, Kim BJ, et al. Hypoxia-inducible factor-2alpha is a catabolic regulator of osteoarthritic cartilage destruction. Nat Med. 2010;16(6):687–693. doi: 10.1038/nm.2153. [DOI] [PubMed] [Google Scholar]
- 35.Saito T, Fukai A, Mabuchi A, Ikeda T, Yano F, Ohba S, et al. Transcriptional regulation of endochondral ossification by HIF-2alpha during skeletal growth and osteoarthritis development. Nat Med. 2010;16(6):678–686. doi: 10.1038/nm.2146. [DOI] [PubMed] [Google Scholar]
- 36.Kamekura S, Kawasaki Y, Hoshi K, Shimoaka T, Chikuda H, Maruyama Z, et al. Contribution of runt-related transcription factor 2 to the pathogenesis of osteoarthritis in mice after induction of knee joint instability. Arthritis Rheum. 2006;54(8):2462–2470. doi: 10.1002/art.22041. [DOI] [PubMed] [Google Scholar]
- 37.Gowen M, Lazner F, Dodds R, Kapadia R, Feild J, Tavaria M, et al. Cathepsin K knockout mice develop osteopetrosis due to a deficit in matrix degradation but not demineralization. J Bone Miner Res. 1999;14(10):1654–1663. doi: 10.1359/jbmr.1999.14.10.1654. [DOI] [PubMed] [Google Scholar]
- 38. Kozawa E, Nishida Y, Cheng XW, Urakawa H, Arai E, Futamura N, et al. Osteoarthritic change is delayed in a Ctsk-knockout mouse model of osteoarthritis. Arthritis Rheum. 2012;64(2):454–464. doi: 10.1002/art.33398. First report on protection against osteoarthritis-like changes after destabilization of the knee in Ctsk-null mice (with 39).
- 39. Hayami T, Zhuo Y, Wesolowski GA, Pickarski M, Duong le T. Inhibition of cathepsin K reduces cartilage degeneration in the anterior cruciate ligament transection rabbit and murine models of osteoarthritis. Bone. 2012;50(6):1250–1259. doi: 10.1016/j.bone.2012.03.025. First report on reduced osteoarthritis after ACL transection in mice that lack cathepsin K also describes an 8-week experiment with a CatK inhibitor in a rabbit ACL transection model.
- 40.Bendele AM. Animal models of osteoarthritis. J Musculoskelet Neuronal Interact. 2001;1(4):363–376. [PubMed] [Google Scholar]
- 41.McNulty MA, Loeser RF, Davey C, Callahan MF, Ferguson CM, Carlson CS. Histopathology of naturally occurring and surgically induced osteoarthritis in mice. Osteoarthritis Cartilage. 2012;20(8):949–956. doi: 10.1016/j.joca.2012.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.van der Kraan PM, Stoop R, Meijers TH, Poole AR, van den Berg WB. Expression of type × collagen in young and old C57Bl/6 and Balb/c mice. Relation with articular cartilage degeneration. Osteoarthritis Cartilage. 2001;9(2):92–100. doi: 10.1053/joca.2000.0364. [DOI] [PubMed] [Google Scholar]
- 43.Bohm BB, Aigner T, Roy B, Brodie TA, Blobel CP, Burkhardt H. Homeostatic effects of the metalloproteinase disintegrin ADAM15 in degenerative cartilage remodeling. Arthritis Rheum. 2005;52(4):1100–1109. doi: 10.1002/art.20974. [DOI] [PubMed] [Google Scholar]
- 44.Mosig RA, Dowling O, DiFeo A, Ramirez MC, Parker IC, Abe E, et al. Loss of MMP-2 disrupts skeletal and craniofacial development and results in decreased bone mineralization, joint erosion and defects in osteoblast and osteoclast growth. Hum Mol Genet. 2007;16(9):1113–1123. doi: 10.1093/hmg/ddm060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Holmbeck K, Bianco P, Caterina J, Yamada S, Kromer M, Kuznetsov SA, et al. MT1-MMP-deficient mice develop dwarfism, osteopenia, arthritis, and connective tissue disease due to inadequate collagen turnover. Cell. 1999;99(1):81–92. doi: 10.1016/s0092-8674(00)80064-1. [DOI] [PubMed] [Google Scholar]
- 46.Blom AB, van Lent PL, Libregts S, Holthuysen AE, van der Kraan PM, van Rooijen N, et al. Crucial role of macrophages in matrix metalloproteinase-mediated cartilage destruction during experimental osteoarthritis: involvement of matrix metalloproteinase 3. Arthritis Rheum. 2007;56(1):147–157. doi: 10.1002/art.22337. [DOI] [PubMed] [Google Scholar]
- 47.Sahebjam S, Khokha R, Mort JS. Increased collagen and aggrecan degradation with age in the joints of Timp3(−/−) mice. Arthritis Rheum. 2007;56(3):905–909. doi: 10.1002/art.22427. [DOI] [PubMed] [Google Scholar]
- 48.Neuhold LA, Killar L, Zhao W, Sung ML, Warner L, Kulik J, et al. Postnatal expression in hyaline cartilage of constitutively active human collagenase-3 (MMP-13) induces osteoarthritis in mice. J Clin Invest. 2001;107(1):35–44. doi: 10.1172/JCI10564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Morko J, Kiviranta R, Joronen K, Saamanen AM, Vuorio E, Salminen-Mankonen H. Spontaneous development of synovitis and cartilage degeneration in transgenic mice overexpressing cathepsin K. Arthritis Rheum. 2005;52(12):3713–3717. doi: 10.1002/art.21423. [DOI] [PubMed] [Google Scholar]
- 50.Stanton H, Rogerson FM, East CJ, Golub SB, Lawlor KE, Meeker CT, et al. ADAMTS5 is the major aggrecanase in mouse cartilage in vivo and in vitro. Nature. 2005;434(7033):648–652. doi: 10.1038/nature03417. [DOI] [PubMed] [Google Scholar]
- 51.Li J, Anemaet W, Diaz MA, Buchanan S, Tortorella M, Malfait AM, et al. Knockout of ADAMTS5 does not eliminate cartilage aggrecanase activity but abrogates joint fibrosis and promotes cartilage aggrecan deposition in murine osteoarthritis models. J Orthop Res. 2011;29(4):516–522. doi: 10.1002/jor.21215. [DOI] [PubMed] [Google Scholar]
- 52.Zack MD, Melton MA, Stock JL, Storer CE, Barve RA, Minnerly JC, et al. Reduced incidence and severity of experimental autoimmune arthritis in mice expressing catalytically inactive A disintegrin and metalloproteinase 8 (ADAM8) Clin Exp Immunol. 2009;158(2):246–256. doi: 10.1111/j.1365-2249.2009.04009.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Xu L, Polur I, Servais JM, Hsieh S, Lee PL, Goldring MB, et al. Intact pericellular matrix of articular cartilage is required for unactivated discoidin domain receptor 2 in the mouse model. Am J Pathol. 2011;179(3):1338–1346. doi: 10.1016/j.ajpath.2011.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Xu L, Servais J, Polur I, Kim D, Lee PL, Chung K, et al. Attenuation of osteoarthritis progression by reduction of discoidin domain receptor 2 in mice. Arthritis Rheum. 2010;62(9):2736–2744. doi: 10.1002/art.27582. Based on studies in Ddr2−/− mice, the authors propose a chain of molecular events that underlies the process of articular cartilage degeneration, eventually leading to the development of OA.
- 55. Burleigh A, Chanalaris A, Gardiner MD, Driscoll C, Boruc O, Saklatvala J, et al. Joint immobilization prevents murine osteoarthritis and reveals the highly mechanosensitive nature of protease expression in vivo. Arthritis Rheum. 2012;64(7):2278–2288. doi: 10.1002/art.34420. Expression studies in the DMM model reveal a rapid induction of genes encoding proteases, including aggrecanases. It is also shown that some genes, including Adamts5, are mechanosensitive.
- 56.Loeser RF, Olex AL, McNulty MA, Carlson CS, Callahan MF, Ferguson CM, et al. Microarray analysis reveals age-related differences in gene expression during the development of osteoarthritis in mice. Arthritis Rheum. 2012;64(3):705–717. doi: 10.1002/art.33388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Poulet B, Ulici V, Stone TC, Pead M, Gburcik V, Constantinou E, et al. Time-series transcriptional profiling yields new perspectives on susceptibility to murine osteoarthritis. Arthritis Rheum. 2012;64(10):3256–3266. doi: 10.1002/art.34572. [DOI] [PubMed] [Google Scholar]
- 58.Koza RA, Nikonova L, Hogan J, Rim JS, Mendoza T, Faulk C, et al. Changes in gene expression foreshadow diet-induced obesity in genetically identical mice. PLoS Genet. 2006;2(5):e81. doi: 10.1371/journal.pgen.0020081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Griffin TM, Fermor B, Huebner JL, Kraus VB, Rodriguiz RM, Wetsel WC, et al. Diet-induced obesity differentially regulates behavioral, biomechanical, and molecular risk factors for osteoarthritis in mice. Arthritis Res Ther. 2010;12(4):R130. doi: 10.1186/ar3068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Glasson S, Bendele A, Sum PE, Tam S, Tejada J, Rivera-Bermudez M, et al. Selective Aggrecanase Inhibition is Disease Modifying and Pain Alleviating in a Rat Meniscal Tear Model of Osteoarthritis. OARSI Annual Meeting; Montreal, Canada: Osteoarthritis Cartilage. 2009. p. S56. [Google Scholar]
- 61.Larkin J. Linking an ADAMTS5-specific Therapeutic Monoclonal Antibody to a Sensitive Biochemical Marker of Target Engagement and Activity for Potential Application as a Companion Diagnostic. OARSI Annual Meeting; April 26–29; Barcelona, Spain: Osteoarthritis Cartilage. 2012. p. S290. [Google Scholar]
- 62.Burden M, Hamblin P, Larkin J, White J, inventors; Glaxo Group Limited. Burden M, Hamblin P, Larkin J, White J, assignees. patent WO 2011/002968 A2. Polypeptides and Method of Treatment. 2010
- 63.Krzeski P, Buckland-Wright C, Balint G, Cline GA, Stoner K, Lyon R, et al. Development of musculoskeletal toxicity without clear benefit after administration of PG-116800, a matrix metalloproteinase inhibitor, to patients with knee osteoarthritis: a randomized, 12-month, double-blind, placebo-controlled study. Arthritis Res Ther. 2007;9(5):R109. doi: 10.1186/ar2315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Baragi VM, Becher G, Bendele AM, Biesinger R, Bluhm H, Boer J, et al. A new class of potent matrix metalloproteinase 13 inhibitors for potential treatment of osteoarthritis: Evidence of histologic and clinical efficacy without musculoskeletal toxicity in rat models. Arthritis Rheum. 2009;60(7):2008–2018. doi: 10.1002/art.24629. [DOI] [PubMed] [Google Scholar]
- 65.Johnson AR, Pavlovsky AG, Ortwine DF, Prior F, Man CF, Bornemeier DA, et al. Discovery and characterization of a novel inhibitor of matrix metalloprotease-13 that reduces cartilage damage in vivo without joint fibroplasia side effects. J Biol Chem. 2007;282(38):27781–27791. doi: 10.1074/jbc.M703286200. [DOI] [PubMed] [Google Scholar]
- 66.Jungel A, Ospelt C, Lesch M, Thiel M, Sunyer T, Schorr O, et al. Effect of the oral application of a highly selective MMP-13 inhibitor in three different animal models of rheumatoid arthritis. Ann Rheum Dis. 2010;69(5):898–902. doi: 10.1136/ard.2008.106021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Settle S, Vickery L, Nemirovskiy O, Vidmar T, Bendele A, Messing D, et al. Cartilage degradation biomarkers predict efficacy of a novel, highly selective matrix metalloproteinase 13 inhibitor in a dog model of osteoarthritis: confirmation by multivariate analysis that modulation of type II collagen and aggrecan degradation peptides parallels pathologic changes. Arthritis Rheum. 2010;62(10):3006–3015. doi: 10.1002/art.27596. Demonstrates chondroprotective effects of a potent and highly selective MMP-13 inhibitor in a canine OA model. Biomarkers of cartilage degradation are also evaluated.
- 68.Black RA, Gabel C, Lively S, Toteva M, Fan P, Tocker J, et al. MMP-13 Inhibitors Reduce Nociception in a Rat Model of Osteoarthritis. OARSI Annual Meeting; Brussels, Belgium: Osteoarthritis Cartilage. 2010. p. S25. [Google Scholar]
- 69.Connor JR, LePage C, Swift BA, Yamashita D, Bendele AM, Maul D, et al. Protective effects of a cathepsin K inhibitor, SB-553484, in the canine partial medial meniscectomy model of osteoarthritis. Osteoarthritis Cartilage. 2009;17(9):1236–1243. doi: 10.1016/j.joca.2009.03.015. [DOI] [PubMed] [Google Scholar]
- 70.McDougall JJ, Schuelert N, Bowyer J. Cathepsin K inhibition reduces CTXII levels and joint pain in the guinea pig model of spontaneous osteoarthritis. Osteoarthritis Cartilage. 2010;18(10):1355–1357. doi: 10.1016/j.joca.2010.07.014. [DOI] [PubMed] [Google Scholar]
- 71.Chappard D, Libouban H, Mindeholm L, Basle MF, Legrand E, Audran M. The cathepsin K inhibitor AAE581 induces morphological changes in osteoclasts of treated patients. Microsc Res Tech. 2010;73(7):726–732. doi: 10.1002/jemt.20813. [DOI] [PubMed] [Google Scholar]
- 72.Malfait AM. Modelling pain in post-traumatic osteoarthritis of the knee. Pain. 2012;153(2):257–258. doi: 10.1016/j.pain.2011.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Malfait AM, Ritchie J, Gil AS, Austin JS, Hartke J, Qin W, et al. ADAMTS-5 deficient mice do not develop mechanical allodynia associated with osteoarthritis following medial meniscal destabilization. Osteoarthritis Cartilage. 2010;18(4):572–580. doi: 10.1016/j.joca.2009.11.013. [DOI] [PubMed] [Google Scholar]
- 74.McCulloch DR, Le Goff C, Bhatt S, Dixon LJ, Sandy JD, Apte SS. Adamts5, the gene encoding a proteoglycan-degrading metalloprotease, is expressed by specific cell lineages during mouse embryonic development and in adult tissues. Gene Expr Patterns. 2009;9(5):314–323. doi: 10.1016/j.gep.2009.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Parks WC, Wilson CL, Lopez-Boado YS. Matrix metalloproteinases as modulators of inflammation and innate immunity. Nat Rev Immunol. 2004;4(8):617–629. doi: 10.1038/nri1418. [DOI] [PubMed] [Google Scholar]
- 76.Scholz J, Woolf CJ. The neuropathic pain triad: neurons, immune cells and glia. Nat Neurosci. 2007;10(11):1361–1368. doi: 10.1038/nn1992. [DOI] [PubMed] [Google Scholar]
- 77.Malfait AM, Seymour AB, Gao F, Tortorella MD, Le Graverand-Gastineau MP, Wood LS, et al. A role for PACE4 in osteoarthritis pain: evidence from human genetic association and null mutant phenotype. Ann Rheum Dis. 2012;71(6):1042–1048. doi: 10.1136/annrheumdis-2011-200300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Malfait AM, Arner EC, Song RH, Alston JT, Markosyan S, Staten N, et al. Proprotein convertase activation of aggrecanases in cartilage in situ. Arch Biochem Biophys. 2008;478(1):43–51. doi: 10.1016/j.abb.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 79.Mitchell PG, Magna HA, Reeves LM, Lopresti-Morrow LL, Yocum SA, Rosner PJ, et al. Cloning, expression, and type II collagenolytic activity of matrix metalloproteinase-13 from human osteoarthritic cartilage. J Clin Invest. 1996;97(3):761–768. doi: 10.1172/JCI118475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Song RH, Tortorella MD, Malfait AM, Alston JT, Yang Z, Arner EC, et al. Aggrecan degradation in human articular cartilage explants is mediated by both ADAMTS-4 and ADAMTS-5. Arthritis Rheum. 2007;56(2):575–585. doi: 10.1002/art.22334. [DOI] [PubMed] [Google Scholar]
- 81.Heinegard D. Proteoglycans and more--from molecules to biology. Int J Exp Pathol. 2009;90(6):575–586. doi: 10.1111/j.1365-2613.2009.00695.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wang P, Tortorella M, England K, Malfait AM, Thomas G, Arner EC, et al. Proprotein convertase furin interacts with and cleaves pro-ADAMTS4 (Aggrecanase-1) in the trans-Golgi network. J Biol Chem. 2004;279(15):15434–15440. doi: 10.1074/jbc.M312797200. [DOI] [PubMed] [Google Scholar]
- 83.Tortorella MD, Arner EC, Hills R, Gormley J, Fok K, Pegg L, et al. ADAMTS-4 (aggrecanase-1): N-terminal activation mechanisms. Arch Biochem Biophys. 2005;444(1):34–44. doi: 10.1016/j.abb.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 84.Longpre JM, McCulloch DR, Koo BH, Alexander JP, Apte SS, Leduc R. Characterization of proADAMTS5 processing by proprotein convertases. Int J Biochem Cell Biol. 2009;41(5):1116–1126. doi: 10.1016/j.biocel.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 85.Knauper V, Lopez-Otin C, Smith B, Knight G, Murphy G. Biochemical characterization of human collagenase-3. J Biol Chem. 1996;271(3):1544–1550. doi: 10.1074/jbc.271.3.1544. [DOI] [PubMed] [Google Scholar]
- 86.Kashiwagi M, Tortorella M, Nagase H, Brew K. TIMP-3 is a potent inhibitor of aggrecanase 1 (ADAM-TS4) and aggrecanase 2 (ADAM-TS5) J Biol Chem. 2001;276(16):12501–12504. doi: 10.1074/jbc.C000848200. [DOI] [PubMed] [Google Scholar]
- 87.Kafienah W, Bromme D, Buttle DJ, Croucher LJ, Hollander AP. Human cathepsin K cleaves native type I and II collagens at the N-terminal end of the triple helix. Biochem J. 1998;331(Pt 3):727–732. doi: 10.1042/bj3310727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hou WS, Li Z, Buttner FH, Bartnik E, Bromme D. Cleavage site specificity of cathepsin K toward cartilage proteoglycans and protease complex formation. Biol Chem. 2003;384(6):891–897. doi: 10.1515/BC.2003.100. [DOI] [PubMed] [Google Scholar]
- 89.Zack MD, Malfait AM, Skepner AP, Yates MP, Griggs DW, Hall T, et al. ADAM-8 isolated from human osteoarthritic chondrocytes cleaves fibronectin at Ala(271) Arthritis Rheum. 2009;60(9):2704–2713. doi: 10.1002/art.24753. [DOI] [PubMed] [Google Scholar]
- 90.Grau S, Richards PJ, Kerr B, Hughes C, Caterson B, Williams AS, et al. The role of human HtrA1 in arthritic disease. J Biol Chem. 2006;281(10):6124–6129. doi: 10.1074/jbc.M500361200. [DOI] [PubMed] [Google Scholar]
- 91.Xie DL, Hui F, Meyers R, Homandberg GA. Cartilage chondrolysis by fibronectin fragments is associated with release of several proteinases: stromelysin plays a major role in chondrolysis. Arch Biochem Biophys. 1994;311(2):205–212. doi: 10.1006/abbi.1994.1228. [DOI] [PubMed] [Google Scholar]
- 92.Homandberg GA, Wen C, Hui F. Cartilage damaging activities of fibronectin fragments derived from cartilage and synovial fluid. Osteoarthritis Cartilage. 1998;6(4):231–244. doi: 10.1053/joca.1998.0116. [DOI] [PubMed] [Google Scholar]
- 93.Stanton H, Ung L, Fosang AJ. The 45 kDa collagen-binding fragment of fibronectin induces matrix metalloproteinase-13 synthesis by chondrocytes and aggrecan degradation by aggrecanases. Biochem J. 2002;364(Pt 1):181–190. doi: 10.1042/bj3640181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Tsuchiya A, Yano M, Tocharus J, Kojima H, Fukumoto M, Kawaichi M, et al. Expression of mouse HtrA1 serine protease in normal bone and cartilage and its upregulation in joint cartilage damaged by experimental arthritis. Bone. 2005;37(3):323–336. doi: 10.1016/j.bone.2005.03.015. [DOI] [PubMed] [Google Scholar]
- 95.Chamberland A, Wang E, Jones AR, Collins-Racie LA, LaVallie ER, Huang Y, et al. Identification of a novel HtrA1-susceptible cleavage site in human aggrecan: evidence for the involvement of HtrA1 in aggrecan proteolysis in vivo. J Biol Chem. 2009;284(40):27352–27359. doi: 10.1074/jbc.M109.037051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Tortorella M, Tomasselli A, Song L, TenBrink R, Anglin C, Malfait AM. Healthy minds, healthy joints: Defining a novel role for BACE1 in cartilage erosion. OARSI annual meeting; Brussels, Belgium: Osteoarthritis Cartilage. 2010. p. S120. [Google Scholar]
- 97.Ren J, Wen L, Gao X, Jin C, Xue Y, Yao X. DOG 1.0: illustrator of protein domain structures. Cell Res. 2009;19(2):271–273. doi: 10.1038/cr.2009.6. [DOI] [PubMed] [Google Scholar]
- 98.Arnold K, Bordoli L, Kopp J, Schwede T. The SWISS-MODEL workspace: a web-based environment for protein structure homology modelling. Bioinformatics. 2006;22(2):195–201. doi: 10.1093/bioinformatics/bti770. [DOI] [PubMed] [Google Scholar]
- 99.Henrich S, Cameron A, Bourenkov GP, Kiefersauer R, Huber R, Lindberg I, et al. The crystal structure of the proprotein processing proteinase furin explains its stringent specificity. Nat Struct Biol. 2003;10(7):520–526. doi: 10.1038/nsb941. [DOI] [PubMed] [Google Scholar]
- 100.Hall T, Shieh HS, Day JE, Caspers N, Chrencik JE, Williams JM, et al. Structure of human ADAM-8 catalytic domain complexed with batimastat. Acta Crystallogr Sect F Struct Biol Cryst Commun. 2012;68(Pt 6):616–621. doi: 10.1107/S1744309112015618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Li Z, Kienetz M, Cherney MM, James MN, Bromme D. The crystal and molecular structures of a cathepsin K:chondroitin sulfate complex. J Mol Biol. 2008;383(1):78–91. doi: 10.1016/j.jmb.2008.07.038. [DOI] [PubMed] [Google Scholar]
- 102.Mosyak L, Georgiadis K, Shane T, Svenson K, Hebert T, McDonagh T, et al. Crystal structures of the two major aggrecan degrading enzymes, ADAMTS4 and ADAMTS5. Protein Sci. 2008;17(1):16–21. doi: 10.1110/ps.073287008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Shieh HS, Mathis KJ, Williams JM, Hills RL, Wiese JF, Benson TE, et al. High resolution crystal structure of the catalytic domain of ADAMTS-5 (aggrecanase-2) J Biol Chem. 2008;283(3):1501–1507. doi: 10.1074/jbc.M705879200. [DOI] [PubMed] [Google Scholar]
- 104.DeLano WL. The PyMOL Molecular Graphics System. 1.3r1 ed. New York: Schrodinger, LLC; 2010. [Google Scholar]