Abstract
Background:
Mucinous cysts are lesions with malignant potential. Their management is stil difficult. Ethanol lavage under EUS can be used and could be a good alternative treatment. We report a bi-center experience of ethanol lavage in mucinous cysts of the pancreas.
Patients and methods:
A total of 13 patients in 2 tertiary centers (7 men, 6 women, mean age=68.5 years) underwent ethanol lavage for mucinous cysts under endoscopic ultrasound (EUS) from 2001 to 2010. One of the patients had 2 cysts treated during the same procedure. One patient underwent a second procedure of ethanol lavage. Mucinous cyst diagnosis required: (1) EUS showing cystic lesion without nodule and without communication with pancreatic branch duct. Six cysts were located in the isthmus of the pancreas, 3 in the head, 3 in the body, and 2 in the tail. The mean size was 24 mm (11-50); and (2) Intra-cystic ACE level >400 UI/l and/or histologic proof. Diagnosis of mucinous cyst was obtained using ACE levels in 5 cases, histology in 8 cases, and both in 1 case.
Results:
No complication was reported. Complete responses were observed in 11 cases (85%), with no responses in 2 cases (15%). Mean follow-up was 26 months (4-118 months). Contact was lost with 1 patient. No recurrence was noticed in patients with complete responses.
Conclusion:
This study confirms the feasibility and effectiveness of a loco-regional treatment under EUS for pancreatic cysts. The good ratio of response is probably explained by the lack of septa and the small size of the cysts. The follow-up is still short and needs to be increased. Nethertheless loco-regional treatment of pancreatic cysts lesions under EUS should form a part of the management of pancreatic lesions.
Keywords: endoscopic ultrasound, mucinous cyst, ethanol lavage, therapeutic endoscopic ultrasound
Introduction
Mucinous pancreatic cysts are considered as premalignant lesions. Their malignant potential is reported in the first surgical series.1,2,3 The detection frequency of these diseases increases with the accuracy of imaging techniques.4 Given the widespread use of cross-sectional imaging modalities for various indications, pancreatic cysts (including mucinous cysts) are now detected in nearly 20% of abdominal imaging,5 with the majority discovered incidentally and subsequently identified as benign via abdominal imaging.6 The standard treatment is major and morbid surgery (normally whipple surgery). Enucleation can also be used as a loco-regional surgical treatment; however, this method entails significant risks of morbidity and mortality.7,8
The use of ethanol lavage under echo-endoscopy (EUS) as an alternative treatment for mucinous cysts has been described by two teams.9,10,11,12,13,14,15
In this study, we report a two-center experience of ethanol lavage in pancreatic cystic lesions.
Patients and methods
A total of 13 patients (7 men, 6 women; mean age of 68.5 years) enrolled in two centers underwent EUS for mutinous cysts from 2001 to 2010. One patient had two cysts treated during the same procedure; thus, a total of 14 cysts were treated.
The criteria for the diagnosis of mucinous cysts were: (1) EUS showing cystic lesions without a nodule and with no communication with the pancreatic branch duct. A total of 6 cysts were located in the pancreatic isthmus, 3 in the head, 3 in the body, and 2 in the tail. The mean cyst size was 24 mm (11 to 50 mm); and (2) Intracystic ACE level >400 UI/l and/or histologic proof.
Diagnosis of the mucinous cyst was performed via ACE level determination in 5 cases, histological examination in 8 cases, and both in 1 case.
All patients underwent a CT scan prior to treatment.
Six cysts were asymptomatic, whereas seven were discovered in patients with non-specific abdominal pain. No patient had a history of pancreatitis.
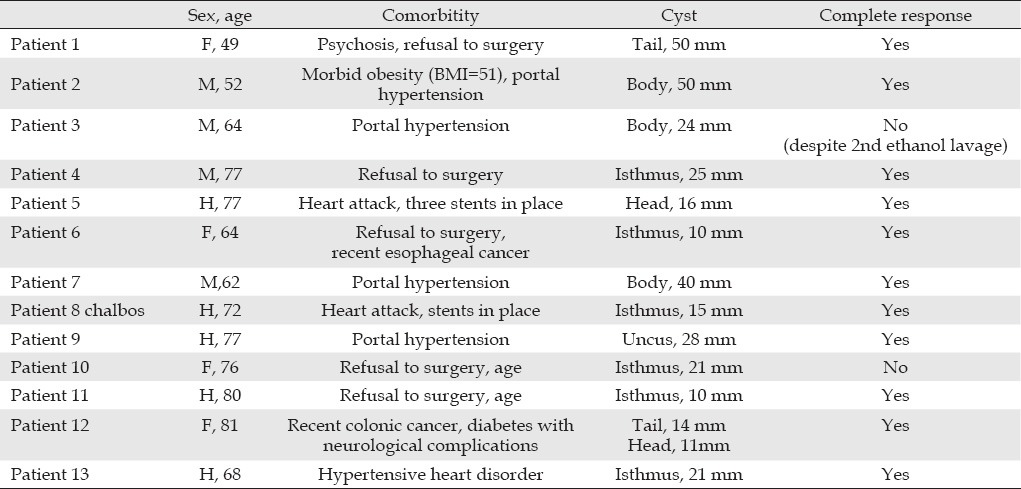
Patients exhibited contraindications for surgery and/or had refused surgery. The contraindications were portal hypertension, congestive cardiac failure, hypertensive heart disease, and recent colonic cancer (Table 1). The method of treatment was decided after a multidisciplinary discussion.
Table 1.
Case details
Treatment was via intracystic ethanol lavage (99%) under a general anesthetic. After fluid cyst aspiration, ethanol lavage was performed using a volume that is equivalent to half the fluid extracted from the cyst. Ethanol was reaspirated after a certain latency time (Pentax® EG38UT, Hitachi®, and Cook Medical®). At the end of the procedure, Lipiodol® was injected in six patients. Lipiodol® was used as an earmark because of its fibrotic effect on the cyst wall.
A follow-up examination was performed via computed tomography (CT) scan and EUS when necessary. The CT scan was conducted after six months and then annually afterward.
Results
Complication
No clinical complication was observed.
Response
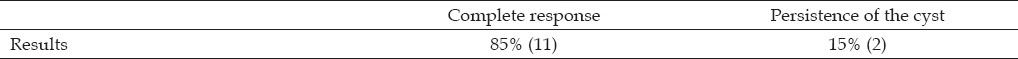
A complete response was defined as the absence of an observable pancreatic cyst in the CT scan during checkup. If the cyst persisted even at a reduced size, the treatment was considered a failure.
A complete response was observed in 11 cases (85%), whereas 2 cases (15%) showed no response (Table 2).
Table 2.
Result of treatment
Follow-up
The mean follow-up period was 26 months (4 to 118 months). Contact was lost with one patient. One patient underwent a second round of ethanol lavage because of a lack of response; however, the procedure did not succeed.
No recurrence was observed in patients with complete response.
Discussion
Epidemiology and standard management
Mucinous cysts were first described by Compagno et al.16. The natural history of this type of cyst is not well known, but degeneration is involved.1,2,3 In 2004, Kosmahl et al.17 estimated that the percentage of mucinous pancreatic cysts ranged from 7% to 40%. In the Japanese autopsy series,18,19 the prevalence of pancreatic cysts, including mucinous and serous cysts, intraductal papillary mucinous neoplasm of the pancreas (IMPT), and other uncommon types of cysts, was 25%. Thus, the theoretical frequency of mucinous cysts in the population is approximately 2% to 4%, which is a significant value.
The standard management of these cysts is surgery, which has a mortality rate of 1% to 5%, as well as a high morbidity rate of 25% to 40%.20,21,22 For small-sized lesions, a close follow-up is usually sufficient.23 The frequency of detection of cystic lesions at younger ages has increased because of the wider use of radiological imaging. The lifelong monitoring of these lesions is probably burdensome for patients, both psychologically and financially.24
Thus, ethanol lavage, which has a lower morbidity rate, is proposed as an alternative treatment for mucinous cysts.
Accuracy of the diagnosis
A mucinous cyst is composed of epithelial cells that produce mucin with ovarian stroma.16 It is primarily detected in women aged 40 to 50 years (sex ratio=20). In 90% of cases, the mucinous cyst is located in the head or tail of the pancreas. Its unilocular characteristic does not allow differentiation from unilocular serous cysts or small-sized IMPT, as determined via imaging.25 Cytological examination via EUS-fine needle aspiration (FNA) offers an accuracy of less than 50%. The determination of intracystic tumor marker levels has an accuracy of 70% to 80%.26 The presence of mucin allows differentiation between mucinous cysts and serous
cysts.27
In our series, diagnosis was based on the endoscopic examination of unilocular cysts combined with histological examination and determination of intracystic CEA levels. The high percentage of the affected people reported in literature was remarkable. This finding can be explained by a bias in our study, wherein the patients showed a heavy comorbidity, which is more common among men. Nevertheless, the diagnosis of these cysts remains difficult, and diagnostic errors cannot be ruled out.
Previous alcoholization and other complications
The destruction of tissues or cyst lesions was described in rabbits in 1991.28 Ethanol injection was performed for liver, thyroid, parathyroid, prostatic, and pulmonary lesions, as well as for a post-traumatic cyst of the spleen.29,30,31,32,33,36 Two percutaneous alcohol injections for pancreatic cysts were reported.37 Under EUS, alcoholization of a gastric tumor as well as liver metastasis was detected in humans,38,39 whereas alcoholization of normal pancreatic tissues was observed in pigs.40 Gan et al.9 described the ethanol lavage of pancreatic cysts in humans. They performed ethanol lavage on 25 patients, with a prospective follow-up of one year. The same team also compared ethanol lavage versus saline intracystic infusion in 42 patients.12 Our series confirms the feasibility of their technique, which has a duration that is equivalent to that of a fine-needle aspiration procedure.
No patients suffered pancreatitis, a complication described in pigs.40,41 However, amylasemia or imaging was not conducted after the lavage. Systematic blood tests would probably show biological pancreatitis.
An evaluation prior to treatment is important to ensure the correct diagnosis of mucinous cysts. In addition, communication of the cyst with pancreatic branch ducts must be determined to eliminate IMPT. Magnetic resonance imaging (MRI) should also be conducted. In our diagnosis, only EUS was performed. Indeed, alcohol injection of IMPT is not likely to have the same consequences as mucinous cyst treatment. Nevertheless, in the series by Di Maio et al.10, 13 patients with possible IMPT underwent ethanol lavage without serious complications.
Response evaluation
The evaluation of tumoral response remains problematic. Our main criterion in this study was the disappearance of the cysts in the CT scan; this criterion is similar to that of Brugge's team. However, the histological response seems impossible to be evaluated without surgery.
In addition, the risk of degeneration over time is not evaluated well. The evaluation of the efficiency of ethanol lavage would take 5 to 10 years,42 which is the estimated duration of mucinous cyst degeneration. Thus, the median follow-up in our series (26 months) is still too short. However, the low complication rate and the imaging response encourage the use of ethanol lavage as an alternative to morbid surgery in cases of surgical contraindications. Therefore, ethanol lavage warrants its place in the management of pancreatic cystic lesions.
Results (Table 3)
Table 3.
Literature for Ethanol lavage of mucinous cysts of the pancreas
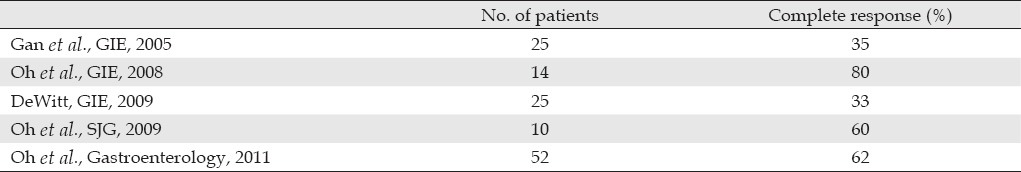
Our results show a higher response ratio than those of previous studies by Gan et al.9 and DeWitt et al.12 Both teams conducted their studies on 25 patients (a larger sample base compared with that of our study), with both obtaining a ratio of 33%. However, nine patients who underwent surgery had a complete histological response. Our results are similar to those of Oh et al. (60%),13 who recently published their results on 52 patients.15 The response in their series was 62%, and the mean cyst size was 31.8 mm. On the other hand, the mean size of the cysts in our series was 24 mm. The smaller size in our series explains our more promising results. The size is a predictive factor of resolution in the series of Oh et al.14 Thus, the lack of septa could explain the increased response; however, they did not describe this lack of response in their report. Furthermore, we obtained a better response to mucinous cysts than to indeterminate cysts.
All patients, except for one, underwent only one session of ethanol lavage. With the patient who underwent a second round of ethanol lavage, the increase in efficiency that has been described for a repeat procedure was not observed.10
Aside from ethanol lavage, Oh et al.13 also used paclitexel injection in their studies. As previously mentioned, the results of our study are similar to those of Oh et al.13 As a whole, these similar complete response ratios suggest that the best treatment for mucinous cysts has yet to be defined. Perhaps, with continuous developments and improvements in the techniques, other pancreatic lesions could be ablated.
Conclusions
The management of pancreatic cysts remains difficult. A locoregional treatment (ethanol lavage in our series) is one possible method of management. The current results show that this treatment is feasible, has no complications, shows good response, and prevents the immediate recurrence of cysts. These results corroborate the of previous studies. Small mucinous cysts can be effectively treated with the proposed method. Nevertheless, this loco-regional treatment requires further improvement, and a long follow-up is necessary. The development of new techniques is also warranted.
References
- 1.Zamboni G, Scarpa A, Bogina G, et al. Mucinous cystic tumors of the pancreas: clinicopathological features, prognosis, and relationship to other mucinous cystic tumors. Am J Surg Pathol. 1999;23:410–22. doi: 10.1097/00000478-199904000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Warshaw AL, Compton CC, Lewandrowski K, et al. Cystic tumors of the pancreas. New clinical, radiologic, and pathologic observations in 67 patients. Ann Surg. 1990;212:432–43. doi: 10.1097/00000658-199010000-00006. discussion 444-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Le Borgne J, de Calan L, Partensky C. Cystadenomas and cystadenocarcinomas of the pancreas: a multiinstitutional retrospective study of 398 cases. French Surgical Association. Ann Surg. 1999;230:152–61. doi: 10.1097/00000658-199908000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carlos Fernandez-del castillo, Javier Targaroma, Sarh Thayer. Incidental pancreatic cysts : clinicopathologic characteristics and comparison with symptomatic patients. Arch Surg. 2003;138:427–34. doi: 10.1001/archsurg.138.4.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brugge WR. Cystic lesions of the pancreas: a surprisingly common finding. ASGE Clinical Updates. 2006;13:1–4. [Google Scholar]
- 6.Walsh RM, Vogt DP, Henderson JM, et al. Natural history of indetermi- nate pancreatic cysts. Surgery. 2005;138:665–70. doi: 10.1016/j.surg.2005.07.019. discussion 70-1. [DOI] [PubMed] [Google Scholar]
- 7.Turrini O, Schmidt CM, Pitt HA, et al. Side-branch intra-ductal papillary mucinous neoplasms of the pancreatic head/uncinate: resection or enucleation. HPB (Oxford) 2011;13:126–31. doi: 10.1111/j.1477-2574.2010.00256.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Talamini MA, Moesinger R, Yeo CJ, et al. Cystadenoma of the pancreas: is enucleation an adequate operation? Ann Surg. 1998;227:896–903. doi: 10.1097/00000658-199806000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gan SI, Thompson CC, Lauwers GY, et al. Ethanol lavage of pancreatic cystic lesions: initial pilot study. Gastrointest Endosc. 2005;61:746–52. doi: 10.1016/s0016-5107(05)00320-2. [DOI] [PubMed] [Google Scholar]
- 10.DiMaio CJ, DeWitt JM, Brugge WR. Ablation of pancretic cystic lesions. The use of multiple endoscopic ultrasond-guided ethanol lavage sessins. Pancreas. 2011;40:664–8. doi: 10.1097/MPA.0b013e3182128d06. [DOI] [PubMed] [Google Scholar]
- 11.DeWitt J, DiMaio CJ, Brugge WR. Long term follow-up of pancreatic cyst that resolve radiologically after EUS-guided ethanol ablation. Gastrointest Endosc. 2010;72:862–6. doi: 10.1016/j.gie.2010.02.039. [DOI] [PubMed] [Google Scholar]
- 12.DeWitt J, McGreevy K, Schmidt CM, et al. EUS-guided ethanol versus saline solution lavage for pancreatic cysts: a randomized, double-blind study. Gastrointest Endosc. 2009;70:710–23. doi: 10.1016/j.gie.2009.03.1173. [DOI] [PubMed] [Google Scholar]
- 13.Oh HC, Seo DW, Lee TY, et al. New treatment for cystic tumors of the pancreas: EUS-guided ethanol lavage with paclitaxel injection. Gastrointest Endosc. 2008;67:636–42. doi: 10.1016/j.gie.2007.09.038. [DOI] [PubMed] [Google Scholar]
- 14.Oh HC, Seo DW, Kim SC, et al. Septated cystic tumors of the pancreas: is it possible to threat them by endoscopic ultrasonography-guided intervention? Scand J Gastroenterol. 2009;44:242–7. doi: 10.1080/00365520802495537. [DOI] [PubMed] [Google Scholar]
- 15.Oh HC, Seo DW, Song TJ, et al. Endoscopic ultrasonography-guided ethanol lavage with paclitaxel injection treats patients with pancretics cysts. Gastroenterology. 2011;140:172–9. doi: 10.1053/j.gastro.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 16.Compagno J, Oertel JE. Mucinous cystic neoplasms of the pancreas with overt and latent malignancy (cystadenocarcinoma and cystadenoma). A clinicopathologic study of 41 cases. Am J Clin Pathol. 1978;69:573–80. doi: 10.1093/ajcp/69.6.573. [DOI] [PubMed] [Google Scholar]
- 17.Kosmahl M, Pauser U, Peters K, et al. Cystic neoplasms of the pancreas and tumor-like lesions with cystic features: a review of 418 cases and a classification proposal. Virchows Arch. 2004;445:168–78. doi: 10.1007/s00428-004-1043-z. [DOI] [PubMed] [Google Scholar]
- 18.Kimura W, Nagai H, Kururuda A, et al. Analysis of small cystic lesions of the pancreas. Int J Pancreat. 1995;18:197–206. doi: 10.1007/BF02784942. [DOI] [PubMed] [Google Scholar]
- 19.Kimura W, Morikane K, Esaki Y, et al. Histologic and biologic patterns of microscopic pancreatic ductal adenocarcinomas detected incidentally at autopsy. Cancer. 1998;82:1839–49. doi: 10.1002/(sici)1097-0142(19980515)82:10<1839::aid-cncr5>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 20.Spinelli KS, Fromwiller TE, Daniel RA, et al. Cystic pancreatic neoplasm: oservate or oprerate. Ann Surg. 2004;239:651–7. doi: 10.1097/01.sla.0000124299.57430.ce. discussion 657-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sauvanet A, Dousset B, Proye C, et al. Pancreatic enucleation: limits of an attractive procedure. Pancreatology. 2003;124:A425. [Google Scholar]
- 22.Nemes R, Curca T, Paraliov T, et al. Cystic tumors of the pancreas. Considerations upon 34 operated cases. Rom J Gastroenterol. 2001;96:3295–300. [PubMed] [Google Scholar]
- 23.Handrich SJ, Hough DM, Fletcher JG, et al. The natural history of the incidentally discovered small simple pancreatic cyst: long-term fol- low-up and clinical implications. AJR Am J Roentgenol. 2005;184:20–3. doi: 10.2214/ajr.184.1.01840020. [DOI] [PubMed] [Google Scholar]
- 24.Spinelli KS, Fromwiller TE, Daniel RA, et al. Cystic pancreatic neoplasms: observe or operate. Ann Surg. 2004;239:651–7. doi: 10.1097/01.sla.0000124299.57430.ce. discussion 7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goh BK, Tan YM, Yap WM, et al. Pancreatic serous oligocystic adenomas: clinicopathologic features and a comparison with serous microcystic adenomas and mucinous cystic neoplasms. World J Surg. 2006;30:1553–9. doi: 10.1007/s00268-005-0749-7. [DOI] [PubMed] [Google Scholar]
- 26.Van der Waaij LA, van Dullemen HM, Porte RJ. Cyst fluid analysis in the differential diagnosis of pancreatic cystic lesions: a pooled analysis. Gastrointest Endosc. 2005;62:383–9. doi: 10.1016/s0016-5107(05)01581-6. [DOI] [PubMed] [Google Scholar]
- 27.Centeno BA. Cystic lesions. In: Centeno BA, Pitman MB, editors. Fine needle aspiration biopsy of the pancreas. Boston: Butterworth, Heinemann; 1999. pp. 53–108. [Google Scholar]
- 28.Kurohiji T, Yamashita Y, Kimitsuki H, et al. An experimental study of ethanol injection on VX2 liver cancer. Gan to Kagaku Ryoho. 1991;18:1908–11. [PubMed] [Google Scholar]
- 29.Larssen TB, Jensen DK, Viste A, et al. Single-session alcohol sclerotherapy in symptomatic begnin hepatic cyst. Long term results Acta radiol. 1999;40:636–8. doi: 10.3109/02841859909175601. [DOI] [PubMed] [Google Scholar]
- 30.Giovannini M, Seitz JF. Ultrasoun guided per cutaneaous alcohol injection of small liver metastasis: results in 40 patients. Cancer. 1994;73:294–7. doi: 10.1002/1097-0142(19940115)73:2<294::aid-cncr2820730210>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 31.Giovannini M, Seitz JF. Treatment of hepatic malignant tumors with percutaneous echo-guided injection of absolute alcohol and 5FU-folinic acid-ultrafluid lipiodol combination. Preliminary results in 17 patients. Gastroenterol Clin Biol. 1992;16:488–9. [PubMed] [Google Scholar]
- 32.Giovannini M, Seitz JF. Percutaneous echo-guided alcoholization in hepatic tumors. Gastroenterol Clin Biol. 1992;16:126–30. [PubMed] [Google Scholar]
- 33.Bennedbaek FN, Hegedus L. Treatment of recurrent thyroid cysts with ethanol: a randomized double-blind controlled trial. J Clin Endocrinol Metab. 2003;88:5773–7. doi: 10.1210/jc.2003-031000. [DOI] [PubMed] [Google Scholar]
- 34.Fletcher S, Kanagasundaram NS, Rayner HC, et al. Assesment of ultrasound guided percutaneous ethanol injection and parathyroidectomy in patients with tertiary hyperparathyropidism. Nephrol Dial Transplant. 1998;13:3111–7. doi: 10.1093/ndt/13.12.3111. [DOI] [PubMed] [Google Scholar]
- 35.Plante MK, Gross AL, Kliment J, et al. Intraprostatic ethanol chemoablation via transmural and transperineal injection. BJU. 2003;91:94–8. doi: 10.1046/j.1464-410x.2003.04011.x. [DOI] [PubMed] [Google Scholar]
- 36.Suzuki K, Morivama N, Yokose T, et al. Preliminary study of percutaneous alcohol injection into the lung. JPN J Cancer Res. 1998;89:89–95. doi: 10.1111/j.1349-7006.1998.tb00484.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yamamoto S, Miyake I, Takatori K, et al. Percutaneous ethanol injection for unresectable pancreatic cancer- report of 2 cases. Gan to Kagaku Ryoho. 1998;25:1969–71. [PubMed] [Google Scholar]
- 38.Gunter E, Lingenfelser T, Eitelbach F, et al. EUS-guided ethanol injection for treatment of a GI stromal tumor. Gastrointest Endosc. 2003;57:113–5. doi: 10.1067/mge.2003.39. [DOI] [PubMed] [Google Scholar]
- 39.Barclay RL, Perez-Miranda M, Giovannini M. EUS-guided treatement of a solid hepatic metastasis. Gastrointest Endosc. 2002;55:266–70. doi: 10.1067/mge.2002.120784. [DOI] [PubMed] [Google Scholar]
- 40.Aslanian H, Salem RR, Marginean C, et al. EUS-guided ethanol injection of normal porcine pancreas: a pilot study. Gastrointest Endosc. 2005;62:723–7. doi: 10.1016/j.gie.2005.06.048. [DOI] [PubMed] [Google Scholar]
- 41.Matthes K, Mino-Kenudson M, Sahani DV, et al. Concentration-dependant ablation of pancreatic tissue by EUS-guided ethanol injection. Gastrointest Endosc. 2007;65:272–7. doi: 10.1016/j.gie.2006.04.043. [DOI] [PubMed] [Google Scholar]
- 42.Zamboni G, Scarpa A, Bogina G, et al. Mucinous cystic tumors of the pancreas: clinicopathological features, prognosis, and relationship to other mucinous cystic tumors. Am J Surg Pathol. 1999;23:410–22. doi: 10.1097/00000478-199904000-00005. [DOI] [PubMed] [Google Scholar]


