Abstract
Paraganglioma is a rare tumor that should be included in the differential diagnosis of retroperitoneal tumors. Endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) has emerged as an effective tool in the diagnosis of these lesions. A 37-year-old female patient with a history of microcytic anemia underwent EUS-FNA and was diagnosed with a neuroendocrine tumor by histopathological and immunohistochemical analysis. The tumor was surgically removed, and the final diagnosis was paraganglioma. This case report emphasizes the importance of EUS in the evaluation of this type of lesion.
Keywords: paraganglioma, neuroendocrine tumor, pancreas, endoscopic ultrasound, fine needle aspiration, immunohistochemstry
INTRODUCTION
Paraganglioma is a rare tumor derived from the chromaffin cells of a sympathetic ganglia. It should always be included in the differential diagnosis of retroperitoneal tumors.1 The diagnosis is made by histopathology and confirmed by immunohistochemistry.
Endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) has emerged as an effective tool in the diagnosis of lesions located into the retroperitonium.2 Even though EUS-FNA should not be done in functional paragangliomas, it is uncertain if FNA can trigger the secretion of catecholamines in non-funcional tumors. The authors present a rare case of an uneventful EUS-FNA diagnosis of such a tumor.
CASE REPORT
A 37-years-old female with a history of microcytic anemia presented at the Santa Casa University General Hospital. She was asymptomatic and there were no alterations in laboratorial tests and physical examination, except for a lesion in the palate, which was later diagnosed as a adenocarcinoma. During the staging of this lesion, the abdomen computed tomography (CT) showed a tumor measuring 4.8 cm × 3.2 cm × 4.3 cm localized in the retroperitoneal region between the vena cava, pancreas head and duodenum. EUS revealed a hipoechogenic, heterogeneous lesion, measuring 3.5 cm × 3.5 cm localized in the pancreatic region, between the vena cava and aorta and next to the superior mesenteric vein. Its invasion could not be rulled out (Fig. 1). The suspected diagnosis was of a retroperitoneum metastasis. EUS-FNA was then performed with a 22-G needle. The histopathological analysis demonstrated malignant cells and immunohistochemical analysis was positive for chromogranin and sinaptophisin, diagnosing neuroendocrine tumor (Fig. 2). After further team discussion, a decision was made to surgically remove the tumor (Fig. 3). The patient was advised for a duodenum pancreatectomy and the final diagnosis was a paraganglioma.
Figure 1.

Endoscopic ultrasound: hipoechogenic lesion in the pancreatic region.
Figure 2.
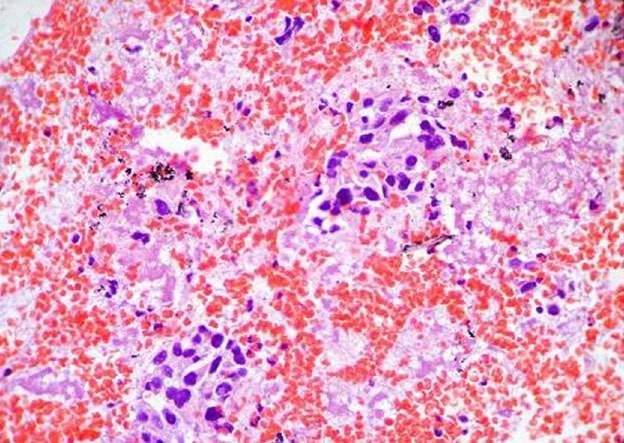
Immunohistochemical compatible with neuroendocrine tumor.
Figure 3.

Ressected lesion.
DISCUSSION
Paragangliomas are rare neuroendocrine tumors most commonly found in the abdomen (84%). About 30% to 50% are malignant.3 The functional ones represent 36% to 60% of all paragangliomas and secrete norepinephrine and normetanephrine. Such patients may be present with severe hypertension, although there are reports of patients with normal blood pressure.3
The preoperative diagnosis is difficult to obtain, especially in non-functional cases, as demonstrated in this case. Functional cases are easier to diagnose because urinary catecholamines are elevated.4,5
Even though imaging studies are helpful, diagnosis of paragangliomas can be safely done only with careful histologic and immunohistochemical evaluation of stains of chromogranin A and S100 protein.4 Recent studies have showed that the diagnosis may be unanticipated by EUS, with anedoctal reports regarding such cases.6
The present case was not different and the diagnosis of paraganglioma was not expected, since the patient had an adenocarcinoma under investigation, had no symptoms related to the first and the EUS appearance was unusual for a neuroendocrine tumour.
The EUS-FNA allows preoperative diagnosis with material for histological analysis. If the patient has symptoms consistent with a pheochromocytoma or a cystic mass of uncertain etiology, it is advisable to assay a 24-hour urine collection for catecholamines, metanephrines, and vanillylmandelic acid before needle puncturing of the lesion.7
Clinical signs should raise a suspicion of paraganglioma, in which case, needle puncture is contraindicated and appropriate imaging and biochemical studies should be obtained. Although EUS-FNA is contraindicated, assessment of anatomically adjacent structures by EUS may provide useful information before surgical resection.2 In the present case, the main diferential diagnosis was a metastatic lesion. Nonetheless, EUS-FNA was performed uneventfully and this most unusual diagnosis was possible.
REFERENCES
- 1.Rha SE, Byun JY, Jung SE, et al. Neurogenic tumors in the abdomen: tumor types and imaging characteristics. Radiographics. 2003;23:29–43. doi: 10.1148/rg.231025050. [DOI] [PubMed] [Google Scholar]
- 2.Kubota K, Kato S, Mawatari H, et al. Risk endoscopic ultrasonography-guided fine-needle aspiration for asymptomatic retroperitoneal tumors. Digest Endosc. 2010;22:144–6. doi: 10.1111/j.1443-1661.2010.00939.x. [DOI] [PubMed] [Google Scholar]
- 3.Yang JH, Bae SJ, Park S, et al. Bilateral pheochromocytoma associated with paraganglioma and papillary thyroid carcinoma: report of an unusual case. Endocr J. 2007;54:227–31. doi: 10.1507/endocrj.k06-068. [DOI] [PubMed] [Google Scholar]
- 4.Ohkawara T, Naruse H, Takeda H, et al. Primary paraganglioma of the head of pancreas: contribution of combinatorial image analyses to the diagnosis of disease. Intern Med. 2005;44:1195–6. doi: 10.2169/internalmedicine.44.1195. [DOI] [PubMed] [Google Scholar]
- 5.Sahdev A, Sohaib A, Monson JP, et al. CT and MR imaging of unusual locations of extra-adrenal paragangliomas (pheochromcytomas) Eur Radiol. 2005;15:85–92. doi: 10.1007/s00330-004-2412-3. [DOI] [PubMed] [Google Scholar]
- 6.Akdamar MK, Eltoum I, Eloubeidi MA. Retroperitoneal paraganglioma: EUS appearance and risk associated with EUS-guided FNA. Gastrointstinal. Endosc. 2004;60:1018–21. doi: 10.1016/s0016-5107(04)02218-7. [DOI] [PubMed] [Google Scholar]
- 7.Baguet JP, Hammer L, Tremel F, et al. Metastatic phaeochromocytoma: risks of diagnostic needle puncture and treatment by arterial embolisation. J Hum Hypertens. 2001;15:209–11. doi: 10.1038/sj.jhh.1001151. [DOI] [PubMed] [Google Scholar]


